Abstract
Introduction
To evaluate effects of Ocufolin on retinal microvasculature in mild non-proliferative diabetic retinopathy patients who carried methylenetetrahydrofolate reductase (MTHFR) polymorphisms (DR+MTHFRP).
Research design and methods
This is a prospective cohort study. Eight DR+MTHFRP (administrated Ocufolin for 6 months) and 15 normal controls (NCs) were recruited. MTHFR polymorphisms were subtyped as normal, C677T, or A1298C. Best-corrected visual acuity (BCVA) was evaluated. Retinal vessel density (VD) and microstructure were evaluated by optical coherence tomography angiography.
Results
BCVA and vascular indices of DR+MTHFRP at baseline were worse than those of NC and improved. Compared with baseline, DR+MTHFRP had significantly improved BCVA during follow-up period (p<0.05). VD of superficial vascular plexus was increased at 4 months (p=0.012), while VD of retinal vascular network did not change (p>0.05). Carriers of A1298C and C677T showed statistically significant increase in VD at all layers by 6 months, while carriers of C677T alone showed no significant change and carriers of A1298C alone showed decreased density from 4 months to 6 months. Microstructure did not change during the follow-up period.
Conclusion
A 6-month intake of Ocufolin is capable of reversing structural changes of microangiopathy in mild non-proliferative DR+MTHFRP. This suggests a novel way to address these impairments prior to catastrophic vision loss.
Keywords: diabetes mellitus, type 2, retina
Significance of this study.
What is already known about this subject?
Retinal vessel density and the thickness of the retinal nerve fiber layer in patients with mild diabetic retinopathy (DR) were significantly reduced compared with normal non-diabetic controls. Methylenetetrahydrofolate reductase (MTHFR) folate polymorphisms may lead to the accelerated progression of retinopathy in patients with diabetes.
What are the new findings?
A 6-month intake of Ocufolin can reverse microvascular damage and improve best-corrected visual acuity in mild non-proliferative DR+MTHFRP.
Ocufolin has potentially beneficial effects for DR+MTHFRP patients with impaired homocysteine metabolism.
How might these results change the focus of research or clinical practice?
The present study shines a light on further treatment options for loss of vision and DR using Ocufolin.
Introduction
Diabetic retinopathy (DR), microangiopathy, is the main cause of blindness in working-age adults globally.1 In DR, a progression of injuries to the endothelium impairs hemodynamics and perfusion: loss of pericytes, roughening of the vessel wall, turbulence, proliferation of endothelial cells, and thickening of the basement membrane, which may be monitored with optical coherence tomography angiography (OCTA).2–7 These are followed by capillary leakage, hemorrhage, capillary network dropout, and retinal ischemia, causing neovascularization in a continuum of deterioration.2–4 8 9 Ultimately, this results in neuronal degeneration and atrophy with permanent loss of vision.2 3 9 Our previous studies have reported that reduction of retinal tissue perfusion is a reliable marker for early DR.4 It has been shown that retinal vessel density and the thickness of the retinal nerve fiber layer in patients with mild DR were significantly reduced compared with normal non-diabetic controls.10
Methylenetetrahydrofolate reductase, MTHFR, is an enzyme that facilitates the remethylation of folate, contributing to the conversion of homocysteine, Hcy, to methionine.11 12 Reduced function polymorphisms of MTHFR are common in the general population (50% or more) and are found with similar frequency in DR patients.12 The most common MTHFR polymorphisms are of the nucleotides 677 (C677T) and 1298 (A1298C), which are associated with reduced enzyme activity responsible for methyl group production.12 The resultant deficiency of available methyl groups causes increased plasma Hcy levels, hypertension, and impaired DNA methylation.13–17 Hcy is a sulfur-containing intermediate metabolite between cysteine and methionine.16 Both elevated serum Hcy and intravitreal Hcy injection have been shown to increase microvascular damage and retinal atrophy.11 16 18
Diabetes and homocysteine metabolism are impacted by both nutritional deficiencies and common MTHFR genetic polymorphisms, which further impair vitamin–mineral uptake and metabolism. The elderly and patients with DR frequently have deficiencies of crucial vitamins, minerals, and related compounds, which cause elevation of Hcy, inflammation, oxidative stress, with loss of vascular density and tissue perfusion. This self-iterative multiple metabolic hit results in vascular morphometric changes, capillary injury, and ischemia.11 19–24
Thus, Hcy, inflammation, and oxidative stress are potential therapeutic targets in DR.18 19 21–24 Patients with MTHFR polymorphisms are at increased risk for more severe diabetic microangiopathy.12 Reduction of oxidative stress and Hcy in the mitochondria and cell membranes of diabetic patients can reasonably be expected to reduce ischemia and end-organ damage of the visual system.16 19 25 The C677T variant is the most studied polymorphism, but the A1298C variant is not harmless. It is associated with decreased HDL, pregnancy loss and infertility.26–28 A study of pulmonary embolism found that the compound heterozygous state, C677T+A1298C, was more liable to pulmonary embolus.29 A study of Tunisian patients with type 2 diabetes and MTHFR variants demonstrated that C677T+A1298C had the greatest risk for DR and complications.12
It has been demonstrated that MTHFR folate polymorphisms may lead to the accelerated progression of retinopathy in patients with diabetes.12 Accumulating evidence indicates that elevated serum Hcy induces endothelial injury. This causes a cascade of hypertension, decreased retinal blood flow, ischemia, and retinal cell death.16–18 This in turn compromises the blood–retinal and blood–brain barriers.30 31 A better understanding of MTHFR gene polymorphisms and their impact on vasculature may improve treatment strategies for DR.15 17 25 32 33 33
Food supplementation with vitamins, minerals, and nutraceuticals is a safe, inexpensive, and simple way to address the underlying risk factors and drivers of DR, specifically hyperhomocysteinemia, hypertension, inflammation, and increased oxidative stress.13 17 19 23 25 34 Targeting homocysteine and oxidative stress has been shown to improve conjunctival perfusion, retinal electrophysiology, and retinal threshold sensitivity.23 35 Also, it is documented to decrease capillary cell apoptosis and macular edema.23 36 It remains untested how medical therapy targeting Hcy or MTHFR polymorphism status affects retinal microvascular density.
Ocufolin (Global Healthcare Focus, Montgomery, Alabama, USA) is a medical food containing l-methylfolate, which improves circulation leading to decreased tissue ischemia in patients with compromising MTHFR mutations.37 A complete description of the components of Ocufolin has been listed in table 1. Schmidl et al38 reported that a 3-month intake of a single Ocufolin capsule daily could significantly reduce Hcy in patients with diabetes while increasing retinal blood flow. Recently, a case series report showed photographic improvement of DR after long-term administration of Ocufolin.39 Conjunctival microcirculation has also been reported to improve after the administration of three capsules daily of Ocufolin.35 The ingredients of Ocufolin have been reported previously.35 The goal of this study was to explore the potential beneficial effects of Ocufolin on retinal microvascular density in mild DR patients with MTHFR polymorphisms.
Table 1.
Components in one capsule of Ocufolin
| Ingredient | Amount |
| L-methylfolate | 900 µg |
| Vitamin C (ascorbic acid) | 33.3 mg |
| Vitamin D (as cholecalciferol) | 1500 IU |
| Vitamin E natural complex (as alpha, beta, gamma, and delta tocopherols) | 7.5 IU |
| Vitamin B1 (as thiamine hydrochloride) | 1.5 mg |
| Vitamin B2 (riboflavin) | 10 mg |
| Vitamin B6 (as pyridoxal 5′-phosphate) | 3 mg |
| Vitamin B12 (as methylcobalamin) | 500 µg |
| Pantothenic acid (as calcium-D-pantothenate) | 5 mg |
| Zinc (as zinc oxide) | 26.6 mg |
| Selenium (as L-selenomethionine) | 20 µg |
| Copper (as cupric oxide) | 0.667 µg |
| N-acetyl cysteine | 180 mg |
| Lutein | 3.35 mg |
| Zeaxanthin | 700 µg |
Methods
Study design, setting, and population
This is a prospective cohort study. Sixteen eyes of eight patients and 15 eyes of gender-matched and age-matched normal controls (NCs) were included in the study. All the subjects were recruited from the Bascom Palmer Eye Institute, University of Miami Miller School of Medicine between August 2017 and January 2020 and underwent a complete ophthalmic examination. DR was diagnosed by a retina specialist (JHT) based on American Diabetes Association criteria and the American Academy of Ophthalmology Retina/Vitreous Panel.40 41 MTHFR polymorphisms were screened in 27 patients with mild DR. Mild DR patients with the presence of the MTHFR reduced function polymorphisms A1298C and/or C677T were eligible for this study. Patients with other retinal vascular diseases, cloudy corneas, and crystalline lens, glaucoma, and other systemic diseases were excluded. Genetic testing was performed by the MyGenetx Laboratory (Franklin, Tennessee, USA).
Written informed consent was obtained from all subjects. Demographics of the study population were obtained.
To evaluate the effect of Ocufolin, each DR+MTHFRP patient was given Ocufolin orally as per the following: one capsule with breakfast for the first week, two capsules with breakfast for the second week, and then three capsules for the rest of the 6 months (6M). Ocufolin intake was confirmed when patients came back at 4 months (4M) (second visit) and 6M (final visit). Best-corrected visual acuity (BCVA), logarithm of the Minimum Angle of Resolution (logMAR), vital measurements including systolic blood pressure (SBP), diastolic blood pressure (DBP), mean artery pressure (MAP), and heart rate (HR), and Mini-Mental Status examination (MMSE) were evaluated.
Measurements of retinal microvascular density
Retinal angiography was captured using the Optovue OCTA device, which is a spectral-domain OCTA system and operates at a scan speed of 70 000 A-scans per second. A raster scan with 304 (A-scan)×304 (B-scan) was used to capture an area of 3×3 mm centered on the fovea. The vessel densities of superficial vascular plexus (SVP), deep vascular plexus (DVP), and total retinal vascular network (RVN) were analysed using 3×3 mm angiography scans.
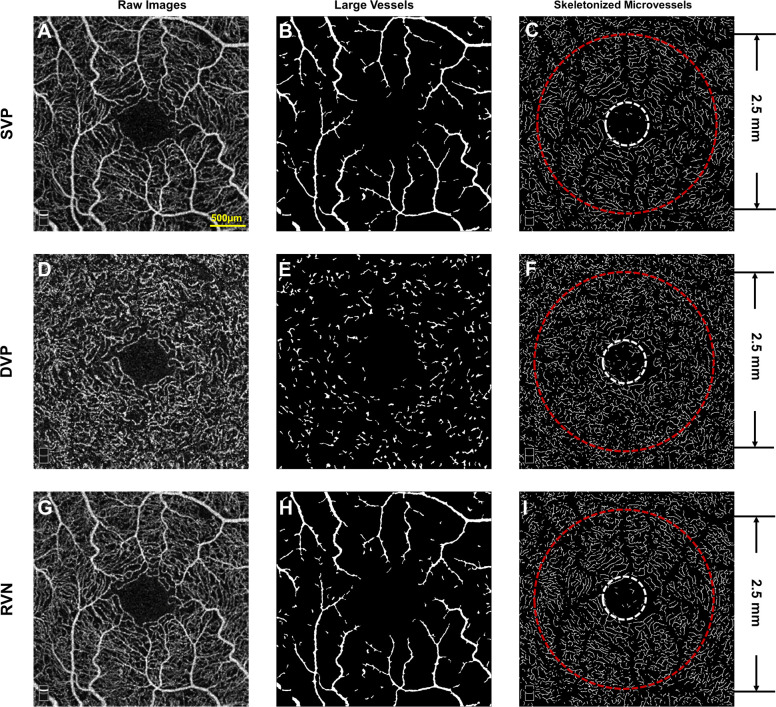
The SVP, DVP, and RVN were segmented from the structures immediately above and below using a custom MATLAB (MathWorks, Natick, Massachusetts, USA) software program. As in previous studies,4 20 a series of imaging processes, including inversion, equalization, projection, and background noise removal, were used to generate binary images. After removing the large vessels (a diameter of ≥25 µm), the remaining microvessels were analyzed. The microvessels within the annulus (0.6–2.5 mm in diameter) were calculated and compared after excluding the foveal avascular zone (FAZ, a diameter of 0.6 mm circle centered on the fovea). Retinal vessel densities (VDs) of three retinal segments, SVP (VDs), DVP (vascular plexus (VDd)), RVN (retinal vascular network (VDr)), were calculated as fractal dimensions (Dbox) within a 2.5 mm diameter circle centered on the fovea (Benoit Pro 2.0, TruSoft International, St. Petersburg, Florida, USA) (figure 1). Representative en face images of the retinal microvascular network in a patient with DR+MTHFR given Ocufolin at baseline, 4M, and 6M are shown in figure 2.
Figure 1.
Segmentation of optical coherence tomography angiography images. The SVP (A), DVP (D), and RVN (G) in a field of view of 3×3 mm were acquired using optical coherence tomography angiography (OCTA) from a patient with DR+MTHFRP. Vessels ≥25 µm (B, E, and H) were extracted. The remaining vessels were defined as microvessels. After processing, the skeletonised microvascular networks (C, F, and I) were used to calculate vessel density using fractal analysis. DR+MTHFRP, mild diabetic retinopathy patients with methylenetetrahydrofolate reductase polymorphisms; DVP, deep vascular plexus; SVP, superficial vascular plexus; RVN, retinal vascular network.
Figure 2.
Representative optical coherence tomography angiography en face images. The images of the retinal microvascular network in a patient with DR+MTHFRP at baseline (A, B, and C) at 4 months (D, E, and F) and 6M (G, H, I) are shown. The vessel density of the microvascular networks in the SVP and RVN at 4 months and 6 months appears higher than that at baseline. However, the densities in DVP were statistically unchanged at the baseline, 4 months, and 6 months. The vessel density expressed as box-counting (Dbox) was listed in each column. DR+MTHFRP, mild diabetic retinopathy patients with methylenetetrahydrofolate reductase polymorphisms; Dbox, fractal dimension; DVP, deep vascular plexus; RVN, retinal vascular network; SVP, superficial vascular plexus.
A commercially available retinal segmentation software program (Orion, Voxeleron, Pleasanton, California, USA) was employed to analyze the dataset of the 6×6 mm scans to yield six intraretinal layers, including the retinal nerve fiber layer (RNFL), ganglion cell-inner plexiform layer (GCIPL), inner nuclear layer (INL), outer plexiform layer (OPL), outer nuclear layer (ONL), and photoreceptor layer (PR) (figure 3).
Figure 3.
Cross-sectional retinal and segmented topographic thickness maps of intraretinal layers. Using the Optovue OCTA device, the retina of a normal control was imaged (A). Six layers of the intraretinal layers were segmented (B). Seven boundaries defined these six intraretinal layers and created six topographic maps (with a diameter of 6 mm) (C). GCIPL, ganglion cell-inner plexiform layer; INL, inner nuclear layer; OCTA, optical coherence tomography angiography; ONL, outer nuclear layer; OPL, outer plexiform layer; PR, retinal photoreceptor; RNFL, retinal nerve fiber layer. Bar=500 µm.
Statistical analysis
IBM SPSS Statistics for Windows (V.25.0, IBM) was used to analyze the data. The measurements of microvascular density were analysed using a generalizsed estimating equation model. Pearson correlation coefficients were used to evaluate the linear correlations among changes of these variables, including BCVA and vascular metrics. Statistical significance was considered as p<0.05.
Results
Study population and baseline clinical characteristics
Sixteen eyes of eight patients with DR+MTHFRP and 15 eyes of 15 NC subjects were imaged. The majority of patients were male (n=6) with well-controlled hypertension (n=5). The mean HbA1c in DR+MTHFRP patients was 7.6%±0.9% (range 6.9–8.1). The mean diabetic duration was 15±7 years (range 5–25). Four patients carried C677T mutation. Two patients carried the A1298C mutation, and two patients carried both C677T/A1298C (compound heterozygous mutations) (table 2).
Table 2.
Demographics and comorbidities of the patient population (n=8)
| Demographics | |
| Age (years), mean (SD) (range) | 58 (7) (47–67) |
| Gender, male, n (%) | 6 (75) |
| Race | |
| White, n (%) | 6 (75) |
| Ethnicity | |
| Hispanic, n (%) | 4 (50) |
| Smoking | |
| Former, n (%) | 1 (12.5) |
| Current, n (%) | 1 (12.5) |
| Durations of diabetes (years), mean (SD) (range) | 15 (7) (5–25) |
| Comorbidities, n (%) | |
| Obesity | 5 (62.5) |
| Hypertension | 5 (62.5) |
| Heart disease | 2 (25) |
| Hypercholesterolemia | 3 (37.5) |
| (HbA1C) (%), mean, SD (range) | 6.9 (0.8) (5.7–8.1) |
| Hcy ((μmol/L), mean, SD (range) | 12.2 (4.2) (6.8–18.2) |
| MTHFR mutations | C677T/A1298C |
HbA1C, hemoglobin A1C; MTHFR, methylenetetrahydrofolate reductase.
Effect of Ocufolin in DR+MTHFRP patients
Clinical parameters (BCVA)
Significant progressive improvement of BCVA was observed at 4M and 6M in all patients receiving Ocufolin compared with baseline values. At 6M, BCVA approached but did not reach that of non-diabetic NC (all p<0.05; figure 4). The average BCVA (LogMAR) at baseline, 4M, and 6M is 0.14±0.08, 0.10±0.09, and 0.09±0.09, respectively. Table 3 shows the BCVA Snellen and logMAR values for each patient at baseline, 4 months, and 6 months.
Figure 4.
Changes of BCVA (logMAR) in DR+MTHFRP at baseline, 4M, and 6M. The effect of Ocufolin on BCVA (logMAR) was significant. BCVA at 4M and 6M significantly and progressively improved compared with baseline acuity. It did not reach that of the non-diabetic NC by the end of the study. It is unknown if a longer study would show further improvement. BCVA, best-corrected visual acuity; DR+MTHFRP, mild diabetic retinopathy patients with methylenetetrahydrofolate reductase polymorphisms; logMAR, logarithm of the Minimum Angle of Resolution; 4M, 4 months; 6M, 6 months; NC, non-diabetic normal controls.
Table 3.
Changes of BCVA in each patient during follow-up periods
| No. | Baseline (logMAR) | 4M (logMAR) | 6M (logMAR) | |||
| OD | OS | OD | OS | OD | OS | |
| 1 | 20/40 (0.3) | 20/30 (0.18) | 20/25 (0.1) | 20/30 (0.18) | 20/20 (0) | 20/30 (0.18) |
| 2 | 20/25 (0.1) | 20/30 (0.18) | 20/25 (0.1) | 20/30 (0.18) | 20/20 (0) | 20/40 (0.3) |
| 3 | 20/25 (0.1) | 20/20 (0) | 20/25 (0.1) | 20/20 (0) | 20/20 (0) | 20/20 (0) |
| 4 | 20/25 (0.1) | 20/25 (0.1) | 20/20 (0) | 20/20 (0) | 20/20 (0) | 20/20 (0) |
| 5 | 20/30 (0.18) | 20/30 (0.18) | 20/25 (0.1) | 20/20 (0) | 20/25 (0.1) | 20/25 (0.1) |
| 6 | 20/25 (0.1) | 20/25 (0.1) | 20/30 (0.18) | 20/25 (0.1) | 20/25 (0.1) | 20/25 (0.1) |
| 7 | 20/25 (0.1) | 20/25 (0.1) | 20/25 (0.1) | 20/25 (0.1) | 20/30 (0.18) | 20/25 (0.1) |
| 8 | 20/40 (0.3) | 20/25 (0.1) | 20/40 (0.3) | 20/20 (0) | 20/25 (0.1) | 20/25 (0.1) |
BCVA, best-corrected visual acuity; logMAR, logarithm of the Minimum Angle of Resolution; 4M, 4 months; 6M, 6 months; OD, right eye; OS, left eye.
Systemic parameters
Systemic markers (SBP, DBP, MAP, and MMSE) remained stable without significant changes during the Ocufolin trial.
Vascular densities of all polymorphisms taken together
Vessel density was measured in patients with DR+MTHFRP at baseline, 4M, and 6M, and in NC groups. Compared with baseline, the vessel density of superficial vascular plexus (VDs) statistically significantly increased at 4M (Dbox 1.785 at 4M; Dbox 1.768 at baseline: p=0.012). At 6M, VDs trended toward an increase from baseline (Dbox 1.781 at 6M, Dbox 1.768 at baseline) but was slightly lower than at 4 months.
Vascular density of the deep VDd and the VDr at 4M and 6M were above untreated baseline, trending upward but not reaching statistical significance during this treatment period. (Dbox for VDd: baseline: 1.791, 4M: 1.794, 6M: 1.792. Dbox for VDr: baseline: 1.785, 4M: 1.791, 6M: 1.789.)
VDr, VDs, and VDd, in DR+MTHFRP patients, although trending upward, remained significantly lower than non-diabetic NCs at all studied intervals (all p<0.05).
Tissue volumes of intraretinal layers
At 4M and 6M, the thickness of the OPL was significantly reduced compared with Baseline values in the DR+MTHFRP group receiving Ocufolin: 0.84 mm3 at baseline and 0.80 mm3 (p=0.027, figure 5D) at 4M and 6M. No significant changes were found in the intraretinal thicknesses of RNFL (A), GCIPL (B), INL (C), ONL (E), and PR (F) during the Ocufolin intake period between the DR+MTHFRP and NC groups (all p>0.05, figure 5). Additionally, table 4 provided the changes of six retinal layers in each patient during follow-up periods.
Figure 5.
Tissue volumes of intraretinal layers. No significant changes were found on the intraretinal thicknesses of RNFL (A), GCIPL (B), INL (C), ONL (E), and PR (F) during the Ocufolin intake period between the D+PM and NC groups (all p>0.05). There were no significant differences in the intraretinal thicknesses in between except OPL(D) at 4M and 6M (p=0.027). D+PM, mild diabetic retinopathy patients with methylenetetra-hydrofolate reductase polymorphisms; GCIPL, ganglion cell-inner plexiform layer; INL, inner nuclear layer; 4M, 4 months; 6M, 6 months; NC, normal control; ONL, outer nuclear layer; OPL, outer plexiform layer; PR, retinal photoreceptor layer; RNFL, retinal nerve fiber layer.
Table 4.
Changes of six introretinal layers in each patient during follow-up periods
| No. | Eye | RNFL | GCIPL | INL | OPL | ONL | PR | ||||||||||||
| Ba | 4M | 6M | Ba | 4M | 6M | Ba | 4M | 6M | Ba | 4M | 6M | Ba | 4M | 6M | Ba | 4M | 6M | ||
| 1 | OD | 1.30 | 1.36 | 1.29 | 2.00 | 1.91 | 2.05 | 0.90 | 0.88 | 0.82 | 0.85 | 0.74 | 0.81 | 2.01 | 2.18 | 2.05 | 1.37 | 1.39 | 1.32 |
| OS | 1.30 | 1.30 | 1.27 | 2.03 | 1.96 | 2.10 | 0.87 | 0.89 | 0.87 | 0.82 | 0.80 | 0.79 | 2.07 | 2.15 | 2.11 | 1.33 | 1.40 | 1.30 | |
| 2 | OD | 1.19 | 1.20 | 1.21 | 1.92 | 1.97 | 1.91 | 0.89 | 0.82 | 0.86 | 0.66 | 0.68 | 0.60 | 1.97 | 1.96 | 2.00 | 1.22 | 1.21 | 1.21 |
| OS | 1.44 | 1.37 | 1.43 | 2.19 | 2.14 | 2.13 | 0.82 | 0.81 | 0.82 | 0.98 | 0.94 | 0.90 | 1.78 | 1.80 | 1.81 | 1.32 | 1.34 | 1.33 | |
| 3 | OD | 1.13 | 1.17 | 1.05 | 2.13 | 2.13 | 2.22 | 1.05 | 1.06 | 1.08 | 0.73 | 0.88 | 0.70 | 2.35 | 2.23 | 2.39 | 1.21 | 1.37 | 1.22 |
| OS | 1.09 | 1.15 | 1.15 | 2.10 | 2.02 | 2.05 | 0.99 | 1.01 | 1.06 | 0.72 | 0.81 | 0.78 | 2.29 | 2.26 | 2.30 | 1.24 | 1.31 | 1.29 | |
| 4 | OD | 1.03 | 0.99 | 0.97 | 1.95 | 1.92 | 1.85 | 0.87 | 0.88 | 0.95 | 0.76 | 0.85 | 0.70 | 1.95 | 1.95 | 2.15 | 1.23 | 1.26 | 1.21 |
| OS | 1.16 | 1.04 | 1.05 | 1.89 | 1.99 | 1.89 | 0.93 | 0.93 | 0.92 | 0.63 | 0.62 | 0.73 | 2.06 | 2.11 | 2.02 | 1.15 | 1.12 | 1.25 | |
| 5 | OD | 1.19 | 1.10 | 1.08 | 1.96 | 2.05 | 2.07 | 0.81 | 1.15 | 1.13 | 0.82 | 0.76 | 0.83 | 2.08 | 2.21 | 2.11 | 1.34 | 1.27 | 1.33 |
| OS | 1.18 | 1.04 | 1.07 | 2.13 | 1.77 | 1.77 | 1.02 | 0.92 | 0.91 | 0.76 | 0.75 | 0.71 | 2.24 | 2.13 | 2.18 | 1.34 | 1.33 | 1.30 | |
| 6 | OD | 0.85 | 0.94 | 0.92 | 1.85 | 1.77 | 1.89 | 0.76 | 0.72 | 0.64 | 0.80 | 0.84 | 0.86 | 1.68 | 1.68 | 1.71 | 1.12 | 1.14 | 1.16 |
| OS | 0.95 | 0.90 | 0.89 | 1.79 | 1.84 | 1.86 | 0.77 | 0.79 | 0.80 | 0.83 | 0.86 | 0.85 | 1.66 | 1.76 | 1.76 | 1.16 | 1.19 | 1.18 | |
| 7 | OD | 1.16 | 1.20 | 1.18 | 1.98 | 2.06 | 2.06 | 0.98 | 0.85 | 0.76 | 0.64 | 1.01 | 0.86 | 2.16 | 1.81 | 1.86 | 1.21 | 1.32 | 1.31 |
| OS | 1.16 | 1.14 | 1.12 | 2.02 | 2.05 | 2.02 | 0.85 | 0.89 | 0.92 | 0.68 | 0.72 | 0.71 | 2.01 | 2.00 | 2.00 | 1.19 | 1.21 | 1.21 | |
| 8 | OD | 1.27 | 1.20 | 1.36 | 2.06 | 2.20 | 2.14 | 0.88 | 0.84 | 0.85 | 1.03 | 1.13 | 0.97 | 1.85 | 1.76 | 1.79 | 1.47 | 1.32 | 1.32 |
| OS | 1.42 | 1.36 | 1.34 | 2.15 | 2.20 | 2.18 | 0.89 | 0.86 | 0.88 | 0.83 | 1.00 | 1.01 | 1.93 | 1.78 | 1.83 | 1.26 | 1.31 | 1.32 | |
Ba, baseline; GCIPL, ganglion cell-inner plexiform layer; INL, inner nuclear layer; 4M, 4 months; 6M, 6 months; OD, right eye; ONL, outer nuclear layer; OPL, outer plexiform layer; OS, left eye; PR, retinal photoreceptor layer; RNFL, retinal nerve fiber layer.
Effects of Ocufolin on retinal vascular density according to MTHFR polymorphism
Varying effects of different MTHFR genotypes on retinal microvasculature were noted during the Ocufolin administration trial (figure 5). At 4M C677T and combined C667T+A1298C, patients had an upward trend of overall vascular density (VDs, VDd, and VDr). For both A1298C and C677T+A1298C, VDs and VDr increased at 4M were statistically significant. For C677T+A1298C alone, the increase over DR baseline was statistically significant in all layers at 4M and 6M. The single polymorphism A1298C showed a decrease in density of all segmented layers at 6M compared with 4M (figure 6).
Figure 6.
Dbox values by study interval and polymorphism. For all three genotypes, there was an upward trend of VDs and VDr vascular density at 4M. For both A1298C and C677T+A1298C, this reached statistical significance for VDs and VDr. Only for C677T+A1298C was the increase over the baseline density statistically significant in all layers at 4M and 6M. The single polymorphism A1298C showed a decrease in density of all segmented layers at 6M compared with 4M. 4M, 4 months; 6M, 6 months; VDd, vascular plexus; VDr, retinal vascular network; VDs, vessel densities.
Discussion
This is the first study attempted to analyze changes in visual acuity and retinal microvascular density in patients with DR+MTHFRP following administration of Ocufolin for 6 months. The key findings are the improvement of BCVA and improvement of retinal microvascular density (increased VDs, VDd, and VDr) at 4M and 6M. This suggests that Ocufolin has potentially beneficial effects for DR+MTHFRP patients with impaired Hcy metabolism. These improvements might be further extended by a longer duration of supplementation.
Ocufolin provides high doses of active forms of vitamins B1, B2, B6, L-methylfolate, and methylcobalamin and has been shown to effectively lower homocysteine in diabetics.19 25 38 Low homocysteine levels protect the blood–retina barrier.30 31 Ocufolin contains vitamin D and other antioxidants that reduce inflammation in DR eyes.21 23 It also provides n-acetylcysteine, a precursor for the potent mitochondrial antioxidant, glutathione,25 which decreases mitochondrial oxidative stress19 23 and additionally substantially lowers homocysteine.38 42
In this study, patients entered with mild or no visual impairment. After receiving Ocufolin for 6 months, eight eyes sustained improved BCVA, six eyes remained unchanged, and two eyes had decreased BCVA. Improved BCVA provides important evidence of benefit for DR patients with MTHFRP.
These changes in retinal microvascular density support the findings of a previous case series paper, which documented large-scale anatomic improvement after taking Ocufolin.39 It supports evidence of improved conjunctival perfusion previously reported in this same cohort.35 Data from Schmidl et al and data currently under review from this same cohort showed improved retinal perfusion after administration of Ocufolin.38 It is likely that improving both retinal microvascular density and retinal perfusion facilitates the improvement of vision. Further studies with larger sample sizes and placebo control should be performed to validate this conclusion. Nevertheless, the present study shines a light on further treatment options for loss of vision and DR using this medical food.
There appears to be a difference in the performance of Ocufolin between C667T and A1298C variants. C677T has been well documented to increase hypertension, homocysteine, and microangiopathy.14 17 25 33 The effects of A1298C are less well understood. A1298C is associated with decreased HDL cholesterol, miscarriage, and infertility.14 17 26–28 There is some evidence that having the C677T plus A1298C variant is associated with thromboembolism.29 Fekih-Mrissa et al12 studied 160 type 2 diabetics and found that patients having either C677T or A1298C variant were at higher risk for retinopathy than genetically normal diabetics. They found that patients with the C677T variant did not show an increase in complications, but those with A1298C did have a higher complication rate, and those having the C677T+A1298C genotype were at the highest risk for at least one complication of DR. This may support the finding that Ocufolin appeared more effective in patients who carried the A1298C variant and was clearly more effective for the C677T+A1298C genotype. The L-methylfolate component of Ocufolin is thought to offset the MTHFR reduced ability to synthesize L-methylfolate, thus lowering homocysteine and perhaps increasing HDL. This may be of therapeutic significance. A larger sample size is needed for confirmation.
Several limitations must be mentioned in this current study. First, the sample size is small, although some of the differences did reach statistical significance. Second, there was no placebo matched control, so both the patients and the investigators knew who was receiving the supplement. Third, we only evaluated the effect of Ocufolin up to 6M. The glycemic status (HbA1C) and Hcy were measured at screening, but not evaluated during baseline and follow-up visits, which may be confounding to the improvement seen in the visual acuity and the retinal vascular perfusion. Fourth, this study may make study participants more aware of their disease and may have been able to carry out additional activities to control their health, such modifying their lifestyle, modifying their diet, and improving adherence to routine treatments. We did not review these possible changes during the study, which may induce study deviation. Further studies will need to control these possible factors. Finally, this study focused on the changes in early mild DR, severe non-proliferative DR, and proliferative DR were not included. A previously published retrospective series, including moderate to severe DR patients, appeared to show anatomic improvement with longer term follow-up.39 These findings of improved microvascular density support evidence of improved perfusion of the conjunctiva previously reported in this same cohort and in the retina (data currently under review) and Schmidl et al.35 38 Future studies should measure HbA1c and Hcy at the end of the trial and include moderate to severe stages of DR, which may further enrich our knowledge on retinal microvasculature in DR, providing clinicians with new therapeutic tools.
In conclusion, the present data demonstrates that a 6-month intake of Ocufolin can reverse microvascular damage and improve BCVA in mild non-proliferative DR+MTHFRP. This may be of clinical importance since it provides a novel therapeutic strategy for patients with early DR and vision loss. Further studies are required to evaluate the long-term clinical effect of Ocufolin on different stages of DR.
Footnotes
Contributors: ZL had access to data, conducted data analysis, and wrote the manuscript. HJ contributed input to the study design, reviewed findings, and provided critical revisions to the manuscript. JHT reviewed findings and provided critical revisions. JW designed the study, oversaw study operations, and wrote and revised the manuscript. All authors have reviewed and approved this version of the manuscript. JW had full access to all the data and take full responsibility for the integrity of the data and the accuracy of the analysis.
Funding: This study was supported by research grants from Global Healthcare Focus LLC, NIH Center Grant P30 EY014801, NINDS 1R01NS111115-01 (JW), and a grant from the Research to Prevent Blindness (RPB). Visiting scholar activity (ZL) was supported by the Guangzhou Municipal Science and Technology Project (No. 201804010038) and the Natural Science Foundation Project of Guangdong Province (No. 2020A1515010276).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available in a public, open access repository. JW had full access to all data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study was approved by the institutional review board (IRB) of the University of Miami, Miller School of Medicine. The IRB ID is 20070492.
References
- 1.Lee R, Wong TY, Sabanayagam C. Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss. Eye Vis 2015;2:17. 10.1186/s40662-015-0026-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen Q, Ma Q, Wu C, et al. Macular vascular fractal dimension in the deep capillary layer as an early indicator of microvascular loss for retinopathy in type 2 diabetic patients. Invest Ophthalmol Vis Sci 2017;58:3785–94. 10.1167/iovs.17-21461 [DOI] [PubMed] [Google Scholar]
- 3.Kim K, Kim ES, Kim DG, et al. Progressive retinal neurodegeneration and microvascular change in diabetic retinopathy: longitudinal study using OCT angiography. Acta Diabetol 2019;56:1275–82. 10.1007/s00592-019-01395-6 [DOI] [PubMed] [Google Scholar]
- 4.Liu Z, Jiang H, Townsend JH, et al. Retinal tissue perfusion reduction best discriminates early stage diabetic retinopathy in patients with type 2 diabetes mellitus. Retina 2021;41:546–54. 10.1097/IAE.0000000000002880 [DOI] [PubMed] [Google Scholar]
- 5.Hammes H-P, Lin J, Renner O, et al. Pericytes and the pathogenesis of diabetic retinopathy. Diabetes 2002;51:3107–12. 10.2337/diabetes.51.10.3107 [DOI] [PubMed] [Google Scholar]
- 6.Burgansky-Eliash Z, Nelson DA, Bar-Tal OP, et al. Reduced retinal blood flow velocity in diabetic retinopathy. Retina 2010;30:765–73. 10.1097/IAE.0b013e3181c596c6 [DOI] [PubMed] [Google Scholar]
- 7.Shin ES, Sorenson CM, Sheibani N. Diabetes and retinal vascular dysfunction. J Ophthalmic Vis Res 2014;9:362–73. 10.4103/2008-322X.143378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bandello F, Lattanzio R, Zucchiatti I, et al. Pathophysiology and treatment of diabetic retinopathy. Acta Diabetol 2013;50:1–20. 10.1007/s00592-012-0449-3 [DOI] [PubMed] [Google Scholar]
- 9.Garner A. Histopathology of diabetic retinopathy in man. Eye 1993;7:250–3. 10.1038/eye.1993.58 [DOI] [PubMed] [Google Scholar]
- 10.Yang JY, Wang Q, Yan YN, et al. Microvascular retinal changes in pre-clinical diabetic retinopathy as detected by optical coherence tomographic angiography. Graefes Arch Clin Exp Ophthalmol 2020;258:513–20. 10.1007/s00417-019-04590-x [DOI] [PubMed] [Google Scholar]
- 11.Huang E-J, Kuo W-W, Chen Y-J, et al. Homocysteine and other biochemical parameters in type 2 diabetes mellitus with different diabetic duration or diabetic retinopathy. Clin Chim Acta 2006;366:293–8. 10.1016/j.cca.2005.10.025 [DOI] [PubMed] [Google Scholar]
- 12.Fekih-Mrissa N, Mrad M, Ibrahim H, et al. Methylenetetrahydrofolate reductase (MTHFR) (C677T and A1298C) polymorphisms and vascular complications in patients with type 2 diabetes. Can J Diabetes 2017;41:366–71. 10.1016/j.jcjd.2016.11.007 [DOI] [PubMed] [Google Scholar]
- 13.Yadav DK, Shrestha S, Lillycrop KA, et al. Vitamin B12 supplementation influences methylation of genes associated with Type 2 diabetes and its intermediate traits. Epigenomics 2018;10:71–90. 10.2217/epi-2017-0102 [DOI] [PubMed] [Google Scholar]
- 14.Fan S, Yang B, Zhi X, et al. Interactions of methylenetetrahydrofolate reductase C677T polymorphism with environmental factors on hypertension susceptibility. Int J Environ Res Public Health 2016;13:601. 10.3390/ijerph13060601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moll S, Varga EA. Homocysteine and MTHFR Mutations. Circulation 2015;132:e6–9. 10.1161/CIRCULATIONAHA.114.013311 [DOI] [PubMed] [Google Scholar]
- 16.Kowluru RA, Mohammad G, Sahajpal N. Faulty homocysteine recycling in diabetic retinopathy. Eye Vis 2020;7:4. 10.1186/s40662-019-0167-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McNulty H, Strain JJ, Hughes CF, et al. Riboflavin, MTHFR genotype and blood pressure: a personalized approach to prevention and treatment of hypertension. Mol Aspects Med 2017;53:2–9. 10.1016/j.mam.2016.10.002 [DOI] [PubMed] [Google Scholar]
- 18.Chang H-H, Lin DP-C, Chen Y-S, et al. Intravitreal homocysteine-thiolactone injection leads to the degeneration of multiple retinal cells, including photoreceptors. Mol Vis 2011;17:1946–56. [PMC free article] [PubMed] [Google Scholar]
- 19.Beltramo E, Nizheradze K, Berrone E, et al. Thiamine and benfotiamine prevent apoptosis induced by high glucose-conditioned extracellular matrix in human retinal pericytes. Diabetes Metab Res Rev 2009;25:647–56. 10.1002/dmrr.1008 [DOI] [PubMed] [Google Scholar]
- 20.Lin Y, Jiang H, Liu Y, et al. Age-Related alterations in retinal tissue perfusion and volumetric vessel density. Invest. Ophthalmol. Vis. Sci. 2019;60:685–93. 10.1167/iovs.18-25864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lu L, Lu Q, Chen W, et al. Vitamin D3 Protects against Diabetic Retinopathy by Inhibiting High-Glucose-Induced Activation of the ROS/TXNIP/NLRP3 Inflammasome Pathway. J Diabetes Res 2018;2018:8193523 10.1155/2018/8193523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kowluru RA, Chan P-S. Oxidative stress and diabetic retinopathy. Exp Diabetes Res 2007;2007:43603 10.1155/2007/43603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kowluru RA, Zhong Q, Santos JM, et al. Beneficial effects of the nutritional supplements on the development of diabetic retinopathy. Nutr Metab 2014;11:8. 10.1186/1743-7075-11-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.ter BS, Verlaan S, Hemsworth J. Micronutrient intakes and potential inadequacies of community-dwelling older adults: a systematic review. Br J Nutr 2015;113:1195–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shi C, Wang P, Airen S, et al. Nutritional and medical food therapies for diabetic retinopathy. Eye Vis 2020;7:33. 10.1186/s40662-020-00199-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mahesh M, Cheng G, Khalighi K. Association of methylenetetrahydrofolate reductase (MTHFR) A1298C polymorphism with lower high-density lipoprotein cholesterol level. Ann Clin Lab Sci 2019;49:232–6. [PubMed] [Google Scholar]
- 27.Nair RR, Khanna A, Singh R, et al. Association of maternal and fetal MTHFR A1298C polymorphism with the risk of pregnancy loss: a study of an Indian population and a meta-analysis. Fertil Steril 2013;99:1311–8. 10.1016/j.fertnstert.2012.12.027 [DOI] [PubMed] [Google Scholar]
- 28.Shi T-L, Wu Y, Li Y, et al. The relevance of MTHFR C677T, A1298C, and MTRR A66G polymorphisms with response to male infertility in Asians: a meta-analysis. Medicine 2019;98:e14283. 10.1097/MD.0000000000014283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Basol N, Karakus N, Savas AY, et al. The importance of MTHFR C677T/A1298C combined polymorphisms in pulmonary embolism in Turkish population. Medicina 2016;52:35–40. 10.1016/j.medici.2016.01.003 [DOI] [PubMed] [Google Scholar]
- 30.Mohamed R, Sharma I, Ibrahim AS, et al. Hyperhomocysteinemia alters retinal endothelial cells barrier function and angiogenic potential via activation of oxidative stress. Sci Rep 2017;7:11952. 10.1038/s41598-017-09731-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Elsherbiny NM, Sharma I, Kira D, et al. Homocysteine induces inflammation in retina and brain. Biomolecules 2020;10:393. 10.3390/biom10030393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lei X, Zeng G, Zhang Y, et al. Association between homocysteine level and the risk of diabetic retinopathy: a systematic review and meta-analysis. Diabetol Metab Syndr 2018;10:61. 10.1186/s13098-018-0362-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Maeda M, Fujio Y, Azuma J. Mthfr gene polymorphism and diabetic retinopathy. Curr Diabetes Rev 2006;2:467–76. [DOI] [PubMed] [Google Scholar]
- 34.Maeda M, Yamamoto I, Fukuda M, et al. Mthfr gene polymorphism as a risk factor for diabetic retinopathy in type 2 diabetic patients without serum creatinine elevation. Diabetes Care 2003;26:547–8. 10.2337/diacare.26.2.547-a [DOI] [PubMed] [Google Scholar]
- 35.Liu Z, Jiang H, Townsend JH, et al. Improved conjunctival microcirculation in diabetic retinopathy patients with MTHFR polymorphisms after Ocufolin™ administration. Microvasc Res 2020;132:104066. 10.1016/j.mvr.2020.104066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smolek MK, Notaroberto NF, Jaramillo AG, et al. Intervention with vitamins in patients with nonproliferative diabetic retinopathy: a pilot study. Clin Ophthalmol 2013;7:1451–8. 10.2147/OPTH.S46718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brown C. Preservation of retinal structure and function after cilioretinal artery occlusion: a case report. Int Med Case Rep J 2016;9:29–34. 10.2147/IMCRJ.S96858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schmidl D, Howorka K, Szegedi S, et al. A pilot study to assess the effect of a three-month vitamin supplementation containing L-methylfolate on systemic homocysteine plasma concentrations and retinal blood flow in patients with diabetes. Mol Vis 2020;26:326–33. [PMC free article] [PubMed] [Google Scholar]
- 39.Wang J, Brown C, Shi C, et al. Improving diabetic and hypertensive retinopathy with a medical food containing L-methylfolate: a preliminary report. Eye Vis 2019;6:21. 10.1186/s40662-019-0147-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chamberlain JJ, Rhinehart AS, Shaefer CF, et al. Diagnosis and management of diabetes: synopsis of the 2016 American diabetes association standards of medical care in diabetes. Ann Intern Med 2016;164:542–52. 10.7326/M15-3016 [DOI] [PubMed] [Google Scholar]
- 41.Flaxel CJ, Adelman RA, Bailey ST, et al. Diabetic retinopathy preferred practice Pattern®. Ophthalmology 2020;127:P66–145. 10.1016/j.ophtha.2019.09.025 [DOI] [PubMed] [Google Scholar]
- 42.Ovrebo KK, Svardal A. The effect of glutathione modulation on the concentration of homocysteine in plasma of rats. Pharmacol Toxicol 2000;87:103–7. 10.1111/j.0901-9928.2000.870301.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available in a public, open access repository. JW had full access to all data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.