Abstract
Objective
This systematic review aimed in assessing the effects of different weaning protocols in people with neuromuscular disease (NMD) receiving invasive mechanical ventilation, identifying which protocol is the best and how different protocols can affect weaning outcome success, duration of weaning, intensive care unit (ICU) and hospital stay and mortality.
Design
Systematic review.
Data sources
Electronic databases (MEDLINE, EMBASE, Web of Science and Scopus) were searched from January 2009 to August 2020.
Eligibility criteria for selecting studies
Randomised controlled trials (RCTs) and non-RCT that evaluated patients with NMD (adults and children from 5 years old) in the weaning process managed with a protocol (pressure support ventilation; synchronised intermittent mandatory ventilation; continuous positive airway pressure; ‘T’ piece).
Primary outcome
Weaning success.
Secondary outcomes
Weaning duration, ICU stay, hospital stay, ICU mortality, complications (pneumothorax, ventilation-associated pneumonia).
Data extraction and synthesis
Two review authors assessed the titles and the abstracts for inclusion and reviewed the full texts independently.
Results
We found no studies that fulfilled the inclusion criteria.
Conclusions
The absence of studies about different weaning protocols for patients with NMD does not allow concluding the superiority of any specific weaning protocol for patients with NMD or determining the impact of different types of protocols on other outcomes. The result of this review encourages further studies.
PROSPERO registration number
CRD42019117393.
Keywords: neuromuscular disease, respiratory medicine (see thoracic medicine), intensive & critical care
Strengths and limitations of this study.
The review highlighted the lack of specific protocols for mechanical ventilation weaning in patients with neuromuscular disease.
Observational and retrospective studies are the most common for patients with neuromuscular disease on ventilator weaning.
After the search, it was not possible to determine the most interesting and efficient weaning protocol for this population.
Non-invasive ventilation is described as a promising resource for patients with neuromuscular disease after mechanical ventilation.
Introduction
Neuromuscular disease (NMD) can be defined as a chronic and progressive disease, which may present with different clinical characteristics, in which its pattern is based on the location where the injury occurs in a motor unit.1 2 NMDs are characterised by progressive muscular impairment, with difficulty in ambulation, swallowing and ventilation, with progressive reduction of vital capacity and increased work of breathing.3 These changes lead to the development of acute and chronic respiratory failure, which is an important cause of prolonged ventilatory dependence,4 5 associated with increased healthcare costs.6
Three main components may contribute to respiratory failure and the need for mechanical ventilation in these patients: (1) inspiratory muscle weakness; (2) expiratory muscle weakness and (3) upper airway compromise.7–9 The patients with NMD experience this respiratory impairment, in general, by a large proportion of motor units that innervate the respiratory muscles affected.2
The majority of critically ill patients admitted to intensive care unit (ICU) require ventilatory support for acute or chronic respiratory failure,3 specially the NMD ones.8 10–12 In addition, the pattern of neuromuscular abnormalities associated with critical illness, defined as ICU-acquired weakness, can lead to prolonged mechanical ventilation, a longer hospital stay and increased ventilation.4
The emergence of respiratory symptoms, with progressive hypercapnia, can lead to death from respiratory failure.3 7 Long-term invasive or non-invasive mechanical ventilation is the main intervention for people who present with acute respiratory acidosis; progressive decline in vital capacity (<10–15 mL/kg); or progressive decline in maximal inspiratory pressure (<20–30 cm H2O).3 8 13
Weaning from mechanical ventilation is the process of transition to spontaneous ventilation.14 In people with NMD, conventional weaning is generally not possible.15 Weaning difficulty may occur in different populations, such as older people with prolonged ICU hospitalisation, people with chronic respiratory diseases or NMD.16 Therefore, the decision to progress to extubation is more challenging in this group of people with advanced respiratory muscle weakness, and this can lead to a need for tracheostomy and prolonged mechanical ventilation.4
The weaning process may be conducted in different protocols such as the following:
‘T’ piece: in which the patient receives only supplemental oxygen through a T-shaped tube connected to an endotracheal tube (orotracheal or tracheostomy).14
Continuous positive airway pressure (CPAP): the weaning protocol involves using a continuous pressure, equal to the previous positive end-expiratory pressure level used before.14
Pressure support: the use of progressive lower levels of inspiratory pressure support until it reaches 5–8 cm H2O.14 This protocol is the most used and described one.
Successful weaning is defined as the ability to maintain spontaneous ventilation without the need for reintubation and invasive mechanical ventilation for 48 hours after extubation.14 For patients with NMD, due to the difficulty of weaning, it may be also defined as the absence of a need for tracheostomy and mechanical ventilation for 5 days after extubation.4
Postweaning monitoring should observe whether two of the following findings are present: respiratory acidosis (pH <7.35; PaCO2 >45 mm Hg); SpO2 (peripheral oxygen saturation) <90% or PaO2 (partial pressure of oxygen in arterial blood) <60 mm Hg with FiO2 (fraction of inspired oxygen) >50%; RR (respiratory rate) >35 rpm; decreased level of consciousness, restlessness or excessive sweating; or signs suggestive of respiratory muscle fatigue, such as the use of accessory muscles or paradoxical movement of the abdomen, in order to determinate the need to re-establish mechanical ventilation again.4 14
Weaning failure from invasive ventilation is frequent in people with NMD due to muscle weakness and gradual hypercapnia.4 In this way, non-invasive ventilation, even after weaning failure, is an option. Furthermore, a future weaning can be conducted when and if clinically possible.4 16 Although this whole process significantly increases health costs with this patient population.
Objectives
The aim of this systematic review was to assess the effects of different weaning protocols in people with NMD receiving invasive mechanical ventilation. Our secondary aim was to assess how the different protocols affect weaning success, duration of weaning, duration of stay in the ICU, duration of hospital stay, ICU mortality and also to assess adverse effects.
Methods
The review authors followed the Cochrane Handbook for Systematic Reviews of Interventions17 and the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) Statement.18 The protocol for the systematic review was previously published on BMJ Open.19
Eligibility criteria for inclusion
Population
Adults (above 16 years old) and children (from 5 to 16 years old) with a clinical diagnosis of an NMD (muscular dystrophy of any origin including Duchenne muscular dystrophy, amyotrophic lateral sclerosis (ALS), congenital myasthenia, myasthenia gravis, congenital myopathy, spinal muscular atrophy, Guillian-Barré Syndrome, severe inherited neuropathies, metabolic myopathies (Pompe disease), inflammatory myopathies and mitochondrial diseases) of any gender.
All patients ventilated for at least 48 hours with orotracheal tube or tracheostomy because of acute respiratory failure, and considered by physicians to be ready for weaning according to clinical criteria and weaning parameters. No patients with other respiratory or cardiovascular clinical diagnosis associated were considered, nor patients with mixed NMD diagnosis.
Intervention
The intervention assessed was the process of weaning from mechanical ventilation in people with NMD using a protocol with criteria for deciding if the patient is ready for extubation with 30 min to 2 hours spontaneous breathing trial (SBT) at the end point of the protocol. The following protocols were considered for inclusion:
Pressure support ventilation, with gradual reduction of the support pressure.
Synchronised intermittent mandatory ventilation, with gradual reduction of respiratory rate and support pressure.
CPAP, with gradual reduction of applied pressure.
‘T’ piece, with progressive increase of spontaneous ventilation time.
Comparison
Any comparison between the different protocols was considered. If the studies classified the weaning based on the outcomes: simple (successful after first attempt of SBT); difficult (requiring up to three attempts or less than 7 days to reach success; prolonged (requiring more than 7 days to reach success), comparisons would also be considered.
Outcomes
Primary outcome
Weaning success, defined as the ability to maintain spontaneous ventilation without the need for reintubation and invasive mechanical ventilation for 48 hours after extubation.14
Secondary outcomes
Duration of weaning in patients with acute and prolonged mechanical ventilation—defined as the time between the weaning protocol initiation and the moment of extubation.
Duration of ICU stay in patients with acute and prolonged mechanical ventilation—defined as the time between ICU admission and ICU discharge.
Duration of hospital stay in patients with acute and prolonged mechanical ventilation—defined as the time between hospital admission and hospital discharge.
ICU mortality rate in patients with acute and prolonged mechanical ventilation—defined as the mortality rate during ICU stay.
Incidence of pneumothorax during mechanical ventilation period.
Incidence of ventilation associated pneumonia.
Study designs
To ensure this evidence synthesis is based on the highest quality of evidence, we only considered including randomised controlled trials (RCTs) and non-RCTs (experimental study with participants subjected to some type of intervention or control group, and with the same outcome of interest measured). There were no restrictions to language in the studies selection.
Search method
Electronic databases were searched from 1 January 2009 up to 31 August 2020: Cochrane Neuromuscular Specialised Register (The Cochrane Library, current issues), MEDLINE, EMBASE, Web of Science and Scopus. We also searched the US National Institutes of Health Clinical Trials Registry, ClinicalTrials. gov (ClinicalTrials. gov) and the WHO International Clinical Trials Registry Portal (apps. who. int/ trialsearch/). Predating 2009 were deemed to be irrelevant to the current experiences of mechanical ventilation weaning for NMD due to considerable changes in these patients management over recent decades.
Search terms included were: ‘neuromuscular disease’ or all other terms compatible with clinical diagnoses of these types of diseases, such as ‘muscular dystrophy’, ‘Duchenne muscular dystrophy’, ‘amyotrophic lateral sclerosis’, ‘congenital myasthenia’, ‘myasthenia gravis’, ‘congenital myopathy’, ‘spinal muscular atrophy’, ‘Guillian Barré Syndrome’, ‘severe inherited neuropathies’, ‘metabolic myopathies’, ‘Pompe disease’, ‘inflammatory myopathies’ and ‘mitochondrial diseases’ combined with ‘mechanical ventilation’ or ‘artificial respiration’ or ‘mechanical ventilation weaning’ or ‘ventilator weaning’ or ‘respirator weaning’ and all the combination between them. The search strategy is available as an online supplemental file 1.
bmjopen-2020-047449supp001.pdf (63.8KB, pdf)
Study selection
Two review authors (SCGBN and IL) performed the search. Two review authors (SCGBN and RT-C) assessed the titles and the abstracts for inclusion independently and induplicate. When the full text was assessed for eligibility criteria, it was performed independently as well, and the authors had an excellent agreement of 99.5%. The disagreements were resolved through consultation of a third review author (IL).
Patient and public involvement
In the present systematic review, there was no involvement of patients or public. The paper proposed to use results previously authorised and published by other authors, without there being any need for patient or public involvement. The research question was developed based on the questions raised by other authors, most of the time according to the clinical difficult and necessity of improving the weaning protocols for this population. The results presented are available in the publication for patients with NMD and public in general.
Results
After searching scrutinously all the databases proposed from January 2009 to August 2020 no studies fulfilled the inclusion criteria regarding different weaning protocols on patients with NMD receiving mechanical ventilation for respiratory failure. A flow chart shows the detailed process of selection (figure 1).
Figure 1.
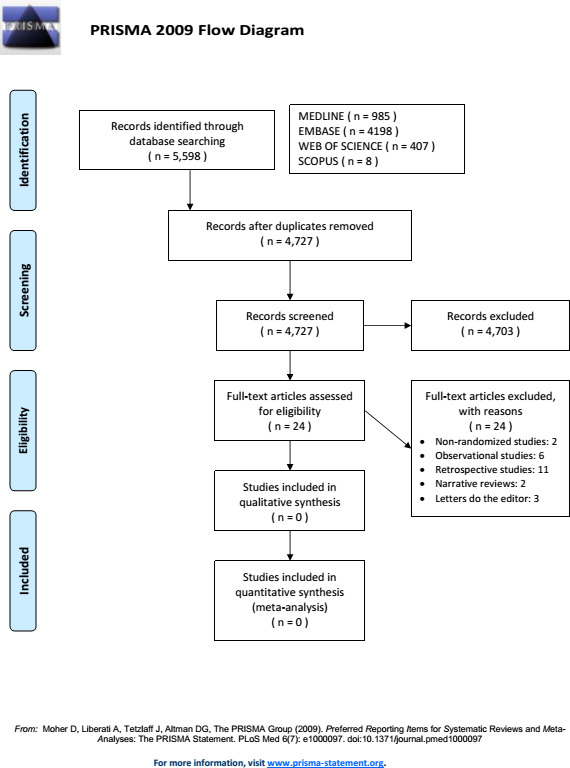
Flow chart showing publication selection.18. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Although 24 studies were selected to full-text reading, none met the eligibility criteria. The excluded publications comprised 2 non-randmomised studies,20 21 6 observational studies,22–27 11 retrospective studies,4 12 16 28–35 2 narrative reviews36 37 and 3 letters to the editor.38–40 The non-randomised studies were not included as eligible despite having a control group, because they did not compare different weaning protocols. In both cases, patients with NMD were submitted to pressure support weaning protocol and the outcomes measured were different from those included in the methods. These two articles are presented in the Discussion section below due to relevant information.
Discussion
We found no high-quality evidence either for or against any of the weaning protocols proposed (pressure support ventilation (PSV), synchronised intermittent mandatory ventilation (SIMV), continuous positive airway pressure (CPAP), or ‘T’ piece) in patients with NMD under mechanical ventilation.
Sun et al20 investigated patients with myasthenia gravis crisis who were hospitalised and needed invasive mechanical ventilation. All the patients were submitted to ventilatory weaning with a gradual reduction in support pressure as protocol, up to values that allowed the SBT in this ventilatory mode. In addition to the SBT, the analysis of the Rapid and Shallow Breathing Index (RSBI) and the fraction of diaphragm thickening fraction (DTF) by bedside ultrasound were also performed. The patients were divided into a successful weaning group and a weaning failure group. Of the 37 patients evaluated, with 63 evaluation measures taken, the characteristics of the groups were similar at the beginning of the SBT. Between 50 and 60 min from the beginning of the SBT, the authors reported that there was a statistically significant increase in the RSBI compared with the initial 5 min (80.41×57.29, p=0.029), as well as a reduction in the DTF (24.46×61.89, p=0.000) in the weaning failure group (n=30). These variables were not observed in the successful weaning group (n=33). The findings of this study allow us to deduce that the weaning protocol using pressure support, as well as the analysis of the RSBI and/or the DTF during SBT, can be a predictive value for the success or failure of weaning.
Vianello et al,21 on the other hand, studied patients diagnosed with NMD and who were admitted to ICUs requiring ventilatory support. In their inclusion criteria, there were patients who remained on mechanical ventilation (MV) for >48 hours and who underwent a weaning protocol with a gradual reduction in support pressure. The authors compare the use of non-invasive ventilation (NIV) immediately after extubation associated with mechanically assisted cough versus a control group of patients with NMD who received standard medical therapy, without the interventions mentioned, after extubation. All patients underwent an SBT in PSV mode with PS<8 cm H2O and were considered able to be extubated when they showed no signs of intolerance. The results described demonstrate, despite the absence of difference in the mortality outcome, that the need for reintubation (30% × 100% − p=0.002) and tracheostomy (30% × 90% − p=0.01) was significantly greater in the group that received standard medical therapy, although all patients were considered ready for extubation by the protocol using the ventilatory pressure support mode.21
The decision about the ideal time to extubate these patients and wean them from ventilatory support is much harder for the patients that deal with respiratory muscle weakness and chronic ventilatory failure, increasing repeated extubation fails and tracheotomies rates.4
In the retrospective studies group with patients with NMD, it was described that early extubation (<6 hours) after a thymectomy in myasthenia gravis crisis was related to a lower reintubation rate, lower postoperative pulmonary infection and shorter duration of ICU stay compared with late extubation (>6 hours).33 Another interesting factor associated with prolonged mechanical ventilation and tracheostomy prolonged need in these patients is neurogenic dysphagia.34 And non-invasive ventilation was highlighted as a feasible intervention to be used after weaning failure with survival improvement and lower reintubation rate,4 as well as instead of invasive mechanical ventilation and future weaning, where no mortality difference was noted.35
The observational prospective studies without control group showed that non-invasive ventilation initiated after spontaneous breathing cycles for Guillain-Barré Syndrom patients under MV is a potential therapeutic strategy.23 And the study that observed the comparison between different five weaning predictors described that the Timed Inspiratory Effort index had a better performance than the others (integrative weaning index, non-invasive tension-time index, maximum inspiratory pressure and breathing frequency/tidal volume—RSBI).25
Two prospective studies with different groups, that were not included because they did not evaluate weaning protocols, attempted to compare prognostic factors of weaning in patients with ALS24 and the ability to prevent atelectasis after extubation with respiratory physiotherapy.27 In the first, it was observed that tracheostomy and use of MV was associated with longer survival, compared with patients who were not directly submitted to invasive MV. The worst prognosis was related to older patients and to the time of respiratory symptoms onset.24 The other study demonstrated, with randomised groups, that a postextubation chest physiotherapy protocol decreased the incidence of atelectasis in paediatric patients with NMD.27
According to the other studies observed during the search, weaning has been studied and applied to this population in the types of protocols. But the results are not satisfactory for any of them, with high failure rates in the process anyway.
The search for the best way to promote weaning from mechanical ventilation for the population of patients with NMD has led professionals and researchers to focus on the use of NIV as a way of progressing and continuing weaning from MV.4 21 23 This type of approach is justified by the absence of studies with an appropriate methodology that identify a better way to conduct weaning in these patients. The combination of NIV with invasive MV has led to a reduction in reintubation rates, despite the increase in the number of patients dependent on this therapy.4 21 41 This observation was also described even for prolonged MV patients with NMD.23
Although NIV has been described as an excellent alternative for weaning in patients who fail in the conventional conditions for evaluating weaning36 (protocols proposed for analysis) it seems to be more efficient when installed immediately after MV removal and not after the appearance respiratory failure, when it would be, especially for patients with NMD, associated with a greater probability of failure and the need to return to invasive MV.4
Xu et al26 observed, in a series of cases of infantile and juvenile patients with Pompe disease, that after conducting weaning in CPAP or PSV, the use of NIV immediately after extubation led to an improvement in respiratory muscle strength, with better respiratory conditions after extubation. However, the result reported by the authors reinforces that the conventional assessment on weaning does not seem to be sufficient for patients with NMD.
Another important consideration is that respiratory failure in patients with NMD is due to impaired respiratory muscle strength and bulbar dysfunction. Traditional methods of assessing the progression of weaning and extubation have important limitations in determining these changes. Craig et al23 even conditioned the removal of MV and placement in NIV for progression of the weaning to conventional parameters of spontaneous breathing conditions and also to safe bulbar function.
Lack of evidence of effectiveness, like in this case, is not evidence that the interventions are ineffective, simply means that there were no papers that met the criteria of methodological quality to be evaluated.
Implications for practice
We found no relevant evidence, so we cannot make any recommendations about better weaning protocols for patients with NMD. The guidelines about ventilatory support management for patients with NMD should be more explicit and clear about the basis of the recommendations regarding weaning protocols.
Implications for research
Given the high incidence of patients with NMD requiring mechanical ventilation for acute or chronic respiratory failure,10 11 there is a lot of space for RCTs, with high methodological rigour to better define the best weaning protocol in this population to ensure better outcomes, mainly in the weaning success.
Conclusion
The absence of studies presenting the proposed inclusion criteria does not allow concluding the superiority of any specific weaning protocol for patients with NMD or determining the impact of different types of protocols on other outcomes such as duration of mechanical ventilation and weaning, duration of ICU or hospital stay, mortality or complications.
The result of this review encourages other authors and researchers to develop specific research and with an adequate methodology in order to seek better answers on weaning protocols in this population.
Supplementary Material
Acknowledgments
The authors thank the anonymous reviewers that contributed constructively to the manuscript. We would also like to thank the members of PneumoCardioVascular Lab/HUOL and Laboratório de Inovação Tecnológica em Reabilitação from Universidade de Federal do Rio Grande do Norte in Brazil for their contribution in researches with neuromuscular disease patients.
Footnotes
Twitter: @vanessaresqueti
Contributors: Data curation: SCGBN and RT-C. Formal analysis: SCGBN and RT-C. Methodology: SCGBN, RT-C and IL. Resources: VRR and GAFF. Writing-original draft: SCGBN, RT-C and GAFF. Writing-review and editing: SCGBN, RT-C, IL, VRR and GAFF. No additional data available.
Funding: The study received financial support from the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) (https://www.gov.br/cases/pt-br), PGCI CAPES 054/2014 - 23038.007514/2014-78. GAFF received a grant from CNPq (https://www.cnpq.br) number 312876/2018-1, and VRR received a grant from CNPq (https://www.cnpq.br) number 315580/2018-6.
Disclaimer: The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Since this study does not involve human participants, ethical approval was not applicable.
References
- 1.Anziska Y, Sternberg A. Exercise in neuromuscular disease. Muscle Nerve 2013;48:3–20. 10.1002/mus.23771 [DOI] [PubMed] [Google Scholar]
- 2.Rezania K, Goldenberg FD, White S. Neuromuscular disorders and acute respiratory failure: diagnosis and management. Neurol Clin 2012;30:161–85. 10.1016/j.ncl.2011.09.010 [DOI] [PubMed] [Google Scholar]
- 3.Ambrosino N, Carpenè N, Gherardi M. Chronic respiratory care for neuromuscular diseases in adults. Eur Respir J 2009;34:444–51. 10.1183/09031936.00182208 [DOI] [PubMed] [Google Scholar]
- 4.Kim SM, Kang S-W, Choi Y-C, et al. Successful extubation after weaning failure by noninvasive ventilation in patients with neuromuscular disease: case series. Ann Rehabil Med 2017;41:450–5. 10.5535/arm.2017.41.3.450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cabrera Serrano M, Rabinstein AA. Causes and outcomes of acute neuromuscular respiratory failure. Arch Neurol 2010;67:1089–94. 10.1001/archneurol.2010.207 [DOI] [PubMed] [Google Scholar]
- 6.Busl KM, Ouyang B, Boland TA, et al. Prolonged mechanical ventilation is associated with pulmonary complications, increased length of stay, and unfavorable discharge destination among patients with subdural hematoma. J Neurosurg Anesthesiol 2015;27:31–6. 10.1097/ANA.0000000000000085 [DOI] [PubMed] [Google Scholar]
- 7.Benditt JO, Boitano LJ. Pulmonary issues in patients with chronic neuromuscular disease. Am J Respir Crit Care Med 2013;187:1046–55. 10.1164/rccm.201210-1804CI [DOI] [PubMed] [Google Scholar]
- 8.Racca F, Vianello A, Mongini T, et al. Practical approach to respiratory emergencies in neurological diseases. Neurol Sci 2020;41:497–508. 10.1007/s10072-019-04163-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vassilakopoulos T, Petrof BJ. Ventilator-induced diaphragmatic dysfunction. Am J Respir Crit Care Med 2004;169:336–41. 10.1164/rccm.200304-489CP [DOI] [PubMed] [Google Scholar]
- 10.Luo F, Annane D, Orlikowski D, et al. Invasive versus non-invasive ventilation for acute respiratory failure in neuromuscular disease and chest wall disorders. Cochrane Database Syst Rev 2017;12:CD008380. 10.1002/14651858.CD008380.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schoser B, Fong E, Geberhiwot T, et al. Maximum inspiratory pressure as a clinically meaningful trial endpoint for neuromuscular diseases: a comprehensive review of the literature. Orphanet J Rare Dis 2017;12:52. 10.1186/s13023-017-0598-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Windisch W, Dellweg D, Geiseler J. Prolonged weaning from mechanical ventilation: results from specialized weaning centers - a registry-based study from the WeanNet Initiative. Dtsch Arztebl Int 2020;117:197–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chevrolet JC, Deléamont P. Repeated vital capacity measurements as predictive parameters for mechanical ventilation need and weaning success in the Guillain-Barré syndrome. Am Rev Respir Dis 1991;144:814–8. 10.1164/ajrccm/144.4.814 [DOI] [PubMed] [Google Scholar]
- 14.Zein H, Baratloo A, Negida A. Ventilator weaning and spontaneous breathing trials; an educational review. Emerg 2016;4:65–71. [PMC free article] [PubMed] [Google Scholar]
- 15.Fan E, Cheek F, Chlan L, et al. An official American thoracic Society clinical practice guideline: the diagnosis of intensive care unit-acquired weakness in adults. Am J Respir Crit Care Med 2014;190:1437–46. 10.1164/rccm.201411-2011ST [DOI] [PubMed] [Google Scholar]
- 16.Tsara V, Moisiadis N, Antoniadou M, et al. Characteristics and outcome of patients with difficult weaning from mechanical ventilation: an 18 years' experience of a respiratory intermediate unit attached to a pulmonary department. Hippokratia 2015;19:37–40. [PMC free article] [PubMed] [Google Scholar]
- 17.Higgins JPT, Green S, The Cochrane Collaboration . Cochrane Handbook for systematic reviews of interventions. version 5.1.0, 1011. Available: www.cochrane-handbook.org
- 18.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006–12. 10.1016/j.jclinepi.2009.06.005 [DOI] [PubMed] [Google Scholar]
- 19.Bernardes Neto SCG, Torres R, Lima Íllia, et al. Weaning from mechanical ventilation in people with neuromuscular disease: protocol for a systematic review. BMJ Open 2019;9:e029890. 10.1136/bmjopen-2019-029890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sun Q, Shan F, Dong H, et al. [Predictive value of ultrasonic diaphragm thickening fraction on successful weaning for patients with myasthenia gravis crisis]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 2017;29:619–23. 10.3760/cma.j.issn.2095-4352.2017.07.009 [DOI] [PubMed] [Google Scholar]
- 21.Vianello A, Arcaro G, Braccioni F, et al. Prevention of extubation failure in high-risk patients with neuromuscular disease. J Crit Care 2011;26:517–24. 10.1016/j.jcrc.2010.12.008 [DOI] [PubMed] [Google Scholar]
- 22.Onders RP, Khansarinia S, Weiser T, et al. Multicenter analysis of diaphragm pacing in tetraplegics with cardiac pacemakers: positive implications for ventilator weaning in intensive care units. Surgery 2010;148:893–8. 10.1016/j.surg.2010.07.008 [DOI] [PubMed] [Google Scholar]
- 23.Craig VJ, Ford V, Chakrabarti B. Non-invasive ventilation in the weaning of patients with acute Guillain barre syndrome requiring invasive ventilation. Am. J. Respir. Crit. Care Med 2017;195. [Google Scholar]
- 24.Hayashi N, Atsuta N, Yokoi D, et al. Prognosis of amyotrophic lateral sclerosis patients undergoing tracheostomy invasive ventilation therapy in Japan. J Neurol Neurosurg Psychiatry 2020;91:285–90. 10.1136/jnnp-2019-322213 [DOI] [PubMed] [Google Scholar]
- 25.de Souza LC, Guimarães FS, Lugon JR. The timed inspiratory effort: a promising index of mechanical ventilation weaning for patients with neurologic or neuromuscular diseases. Respir Care 2015;60:231–8. 10.4187/respcare.03393 [DOI] [PubMed] [Google Scholar]
- 26.Xu L, Ba H, Pei Y, et al. Comprehensive approach to weaning in difficult-to-wean infantile and juvenile-onset glycogen-storage disease type II patients: a case series. Ital J Pediatr 2019;45:106. 10.1186/s13052-019-0692-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bilan N, Poorshiri B. The role of chest physiotherapy in prevention of postextubation atelectasis in pediatric patients with neuromuscular diseases. Iran J Child Neurol 2013;7:21–4. [PMC free article] [PubMed] [Google Scholar]
- 28.Ponfick M, Wiederer R, Bösl K, et al. The influence of weaning duration on rehabilitative outcome in early neurological rehabilitation. NeuroRehabilitation 2014;34:493–8. 10.3233/NRE-141066 [DOI] [PubMed] [Google Scholar]
- 29.Bach JR, Sinquee DM, Saporito LR, et al. Efficacy of mechanical insufflation-exsufflation in extubating unweanable subjects with restrictive pulmonary disorders. Respir Care 2015;60:477–83. 10.4187/respcare.03584 [DOI] [PubMed] [Google Scholar]
- 30.Liptzin DR, Connell EA, Marable J. Ready or not? Weaning chronic ventilation and decannulation in a pediatric ventilator care program. Am J Respir Crit Care Med 2015;191:825–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Parker R, Sunderland G, Ford V, et al. S85 Initiation of long-term non-invasive ventilation enables successful weaning from prolonged mechanical ventilation. Thorax 2013;68:A45.2–6. 10.1136/thoraxjnl-2013-204457.92 [DOI] [Google Scholar]
- 32.Feng X-wei, Zhou X-ming, Qu W-xiu, et al. [Retrospective analysis of related factors for patients with weaning difficulties in medical intensive care unit]. Zhonghua Yi Xue Za Zhi 2011;91:2688–91. [PubMed] [Google Scholar]
- 33.Chen L, Xie W, Zheng D, et al. Early extubation after thymectomy is good for the patients with myasthenia gravis.. Neurol Sci 2019;40:2125–32. 10.1007/s10072-019-03941-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schröder JB, Marian T, Muhle P, et al. Intubation, tracheostomy, and decannulation in patients with Guillain-Barré-syndrome-does dysphagia matter? Muscle Nerve 2019;59:194–200. 10.1002/mus.26377 [DOI] [PubMed] [Google Scholar]
- 35.Chadwick R, Nadig V, Oscroft NS, et al. Weaning from prolonged invasive ventilation in motor neuron disease: analysis of outcomes and survival. J Neurol Neurosurg Psychiatry 2011;82:643–5. 10.1136/jnnp.2009.193631 [DOI] [PubMed] [Google Scholar]
- 36.Gonzalez-Bermejo J, Morelot-Panzini C, Similowski T, et al. Particularités du sevrage de la ventilation mécanique chez les patients atteints de maladie neuromusculaire - Weaning of mechanical ventilation in neuromuscular diseases. Réanimation 2009;18:576–81. [Google Scholar]
- 37.Pohl M. Weaning from prolonged mechanical ventilation in early neurological and neurosurgical rehabilitation (ENNR). Beatmungsentwöhnung in der neurologisch-neurochirurgischen Frührehabilitation 2016;22:187–91. [Google Scholar]
- 38.Racca F, Del Sorbo L, Capello EC, et al. Neuromuscular patients as candidates for non invasive ventilation during the weaning process. Minerva Anestesiol 2012;78:391. [PubMed] [Google Scholar]
- 39.Vianello A, Arcaro G, Braccioni F. Preventive non-invasive ventilation is indicated for neuromuscular disease patients after extubation. Minerva Anestesiol 2012;78:390. [PubMed] [Google Scholar]
- 40.Cheng G, Bach JR. Continuous critical care and long-term noninvasive ventilatory support for patients with neuromuscular disease. Chest 2009;135:246–7. 10.1378/chest.08-1895 [DOI] [PubMed] [Google Scholar]
- 41.Bach JR, Gonçalves MR, Hamdani I, et al. Extubation of patients with neuromuscular weakness: a new management paradigm. Chest 2010;137:1033–9. 10.1378/chest.09-2144 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-047449supp001.pdf (63.8KB, pdf)
Data Availability Statement
No data are available.


