Abstract
Daily rhythms of behavior and neurophysiology are integral to the circadian clocks of all animals. Examples of circadian clock regulation in the human brain include daily rhythms in sleep-wake, cognitive function, olfactory sensitivity, and risk for ischemic stroke, all of which overlap with symptoms displayed by many COVID-19 patients. Motivated by the relatively unexplored, yet pervasive, overlap between circadian functions and COVID-19 neurological symptoms, this perspective piece uses daily variations in the sense of smell and the timing of sleep and wakefulness as illustrative examples. We propose that time-stamping clinical data and testing may expand and refine diagnosis and treatment of COVID-19.
Keywords: COVID-19, circadian, olfaction, sleep, neurological
What’s the problem?
Since December 2019, the identification of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) as the cause of the COVID-19 pandemic has been accompanied by the description of many symptoms of infection. Among these are dysfunction in olfactory sensitivity, elevated stroke risk, altered sleep timing and changes in mental status (Spinato et al., 2020; Varatharaj et al., 2020; Wang et al., 2020), all of which are neurobiological functions regulated by the circadian clock. In addition, various neurological conditions persist or develop during the recovery phase of the disease leading to reports of a growing number of so-called Long COVID-19 Syndrome patients (Lambert and Survivor Corps, 2020). Although the symptoms of these patients are varied, they include difficulty sleeping, joint pain, neuropathies, dizziness, flashes of light in vision, Guillain-Barré syndrome, loss and altered smell perception, confusion, memory problems, sadness, and anxiety—all of which also intersect clock regulated functions. These observations raise the questions of “how does the circadian clock interact with the neurologically rooted symptoms of COVID-19?” and “can this be used for either diagnosis or therapy?”
COVID-19 pathology may depend on, or interfere with, daily rhythms. Impaired sleep-wake may reflect damage to the circadian system (e.g., pacemakers in the brain such as the hypothalamic suprachiasmatic nucleus [SCN], or in peripheral tissues such as the olfactory epithelium). Irregular daily rhythms could result from either direct local viral infection or indirect cytokine storms or strokes. For viral infection, adherence molecules and the virus must be present. The genes encoding proteins involved in entry of SARS-CoV-2 into cells (e.g., ACE2, NPR1, Furin, TMPRSS2) (Bilinska et al., 2020; Cantuti-Castelvetri et al., 2020) are broadly expressed in many tissues including the brain in baboons (Mure et al., 2018). However, SARS-CoV-2 typically does not penetrate the central nervous system (Mahalaxmi et al., 2021; Politi et al., 2020; Zhang, Huo et al., 2020; Solomon et al., 2020; Laurendon et al., 2020). Whether there are daily rhythms in ACE2 abundance or binding, or other steps necessary for infection, has not been investigated. The extremely rare cases that have identified virus in the brain likely reflect disruption of the blood-brain-barrier. One provocative report found that among all patients who died from COVID-19 over 42 days in Hamburg, Germany, over half had detectable SARS-CoV-2 in their brains (Matschke et al., 2020).
Pezzini and Padovani (2020) note, however, that neurological symptoms likely arise as a function of the massive inflammation that comes with pulmonary and/or systemic disease or due to chronic inflammation that can occur during the long recovery phase of COVID-19. As the disease progresses, a patient subset develops symptoms akin to autoimmune encephalitis and astrogliosis (Andalib et al., 2021). In addition, the presence of a variety of autoimmune antibodies has been reported in recovering patients (Woodruff et al., 2020), indicating a breakdown of self-tolerance that is characteristic of autoimmune disorders. We thus conclude that damage to the circadian system, if it occurs, results from indirect consequences of COVID-19.
A number of excellent reviews in this journal (Sengupta et al., 2021; Kronfeld-Schor et al., 2021; Haspel et al., 2021) and elsewhere (Baig, 2020; Paterson et al., 2020; Ray and Reddy, 2020; Asadi-Pooya and Simani, 2020; Varatharaj et al., 2020) provide important explorations of what we now know about the neurobiology of COVID-19, including daily and seasonal variations in neuroimmune function, both in the intensive care unit and in the environment, which can affect SARS-CoV-2 infectivity and mortality. In this perspective paper, our goal is to shed light on how clock regulated neuropathology of COVID-19 could be evaluated, quantified, and used diagnostically. Chronobiology benefits from the power of quantification and these methods have not as yet been applied in the context of this disease. Here, we address the potential value of olfactory testing that is meaningfully tied to circadian phase as a diagnostic for COVID-19 and we discuss how sleep timing could be used to understand the ways in which the circadian clock may be affected by the disease. We conclude with recommendations that incorporate chronobiological principles to augment diagnosis and treatment of COVID-19 and support translational chronobiology.
Case 1. Clock Regulation at the Point of Infection: Altered Olfaction in COVID-19 Patients
The most recent large-scale systematic meta-analysis of the literature assessing olfactory dysfunction in COVID-19 has revealed that the pooled prevalence estimate of smell loss is 77% when assessed through objective measurements (Hannum et al., 2020). Notably, objective olfactory tests can identify 82% of otherwise asymptomatic SARS-CoV-2 carriers and are much more sensitive to SARS-CoV-2 infection than is self-report (i.e., up to 83% vs. 15%; Gözen et al., 2021; Bhattacharjee et al., 2020).
Unlike most upper respiratory tract infections where olfactory loss is due to obstructive interference, olfactory deficiency with COVID-19 appears to be sensorineural, and dysfunction is in the olfactory epithelium and/or afferent brain pathways. Nasal inhalation of the SARS-CoV-2 virus is a primary route of infection, allowing the virus to make contact with the olfactory epithelium, which contains three main cell types: olfactory sensory neurons through which odorants are detected, basal cells which comprise stem and progenitor cells that produce new olfactory sensory neurons, and sustentacular cells that play a support role for the olfactory sensory neurons. Basal and sustentacular cells in the olfactory epithelium have a high expression of the angiotensin-converting enzyme 2 (ACE2) receptor that has been shown to be necessary for the spike protein of SARS-CoV-2 to enter a cell (Bilinska et al., 2020; Lechien, Radulesco, et al., 2021; Sungnak et al., 2020). Disruption of the basal and especially sustentacular cells by SARS-CoV-2, which then causes inflammation and damage to the olfactory sensory neurons, appears to be the cause of olfactory perturbations in COVID-19 (Brann et al., 2020; Whitcroft and Hummel, 2020).
Penetration of SARS-CoV-2 into the basal and sustentacular cells can also impair the normal neurogenesis of olfactory sensory neurons (Goncalves and Goldstein, 2016), and this may explain the variability seen in the length of time to recover olfactory function following COVID-19 infection (Lee et al., 2020). Although most people experience full olfactory recovery within 1 to 3 weeks after the virus has cleared, a proportion of patients report unremitting olfactory dysfunction (de Melo et al., 2021; Li et al., 2020; Otte et al., 2020).
The Centers for Disease Control and Prevention (CDC) lists “new loss of smell” as an early warning symptom of COVID-19. More importantly, recent studies have now shown that olfactory loss is the best predictor of SARS-CoV-2 infection; indeed, it is potentially superior to other symptoms that the CDC and the World Health Organization (WHO) have determined to be relevant such as fever, cough, headache, and fatigue (Gerkin et al., 2021). Not only is smell loss an early symptom of COVID-19 (Klopfenstein et al., 2020; Levinson et al., 2020; Salje et al., 2020), olfactory dysfunction has been shown to precede positive polymerase chain reaction (PCR) findings by a median of 2 days (Weiss et al., 2020). Given that to date over 185 million people worldwide have been infected with SARS-CoV-2, daily assessment of olfactory function has enormous public health potential. It is also important to note that olfactory dysfunction is more prevalent in mild (86% of mild cases) than in severe manifestations of COVID-19 (Lechien, Chiesa-Estomba, et al., 2021); given that individuals with mild illness may be more likely to mingle and thus transmit illness, it is crucial that olfactory dysfunction be recognized as a means to curb disease transmission. To this end, Pierron et al. (2020) found that, in France, sudden smell loss was a better predictor of critical care and hospital overload from COVID-19 patients than governmentally issued indicators of COVID-19 infection.
Beyond smell loss per se, Weiss et al. (2020) found that parosmia—qualitatively altered olfactory perception where an odor is detected but is perceived unusually and typically as unpleasant—was the first symptom reported in a third of the positive cases where smell dysfunction occurred. Germane to the neurological significance of olfaction in COVID-19, the same study found that all COVID-19 positive individuals who indicated olfactory dysfunction also self-reported neurological symptoms such as headache, dizziness, or fatigue; a small subset of whom experienced prolonged neurological symptoms (≥ 20 days after receiving a positive test). Thus, in addition to decreased olfactory sensitivity, parosmia should be assessed as an early warning symptom of COVID-19, and olfactory impairment in general may be a signal for subsequent neurological involvement (Asadi-Pooya and Simani, 2020; Mahalaxmi et al., 2021; Politi et al., 2020; Zubair et al., 2020).
As loss of smell is recognized as a cardinal indicator of COVID-19, a number of objective smell tests have been developed and at least one smell test has been approved for in-home purposes (e.g., ANOSMIC™). As these tests grow in usage, we recommend that measurements of smell sensitivity take circadian phase into account.
Odor detection depends on factors including the odorant and concentration being tested, age, sex, and various other individual difference characteristics (for review see Herz, 2016). In humans, olfactory sensitivity has also been shown to be affected by circadian phase, which when mapped on to time of day, indicates peak sensitivity in the afternoon-evening, and lowest sensitivity in the early morning (Figure 1; Herz et al., 2018). The time of peak sensitivity has been shown to be genotype specific in mice, worms, and flies (Granados-Fuentes et al., 2006; Krishnan et al., 1999; Olmedo et al., 2012) and likely depends on factors such as age, sex, and lighting history that influence chronotype. Diurnal variation in olfactory sensitivity has also been explored in humans (Nordin et al., 2003; Lötsch et al., 1997) but definitive findings are lacking. Future research examining diurnal variability in olfactory function would be a valuable addition to what is currently known about olfactory fluctuations and circadian phase. Nevertheless, as circadian phase has been shown to influence olfactory sensitivity (Herz et al., 2018), we argue that smell tests for assessment of COVID-19 should take circadian phase into account. No studies to date have done so, and we propose several questions concerning circadian influences in olfaction and COVID-19 to aid future research, clinical practice, and public health.
Figure 1.
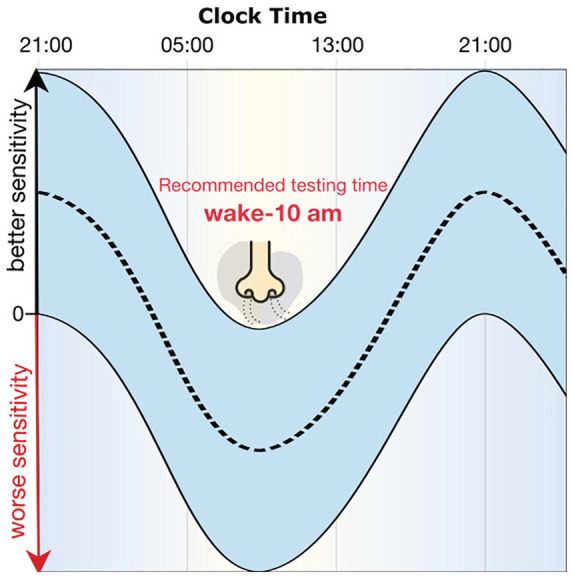
Predicted circadian function for olfactory sensitivity and recommendations for testing time. The dashed line represents the sample average cosinor function for olfactory sensitivity; the blue area represents the 95% confidence interval estimated using a multilevel cosinor model. Lowest olfactory acuity occurs between approximately 0200 and 1000 h. We therefore recommend that testing smell function occur between waking and 1000 h to be most sensitive to capturing mild perturbations in smell function early in COVID-19 infection (modified from Herz et al., 2018). Note that the circadian range described here was obtained from a limited sample of adolescents and ethnicity was not assessed. As circadian phase is known to change with age (Duffy and Czeisler, 2002; Roenneberg et al., 2004) and can vary with ethnicity (Malone et al., 2016), the specific window of circadian phase indicated here may not be fully generalizable.
First, does initial olfactory dysfunction correlate with the circadian phase of olfactory sensitivity—for example, being more pronounced when sensitivity is lowest—and can this be used to distinguish COVID-19 positive from negative cases? The Weiss et al. (2020) study instructed individuals to, as much as possible, conduct in-home smell testing that involved sniffing peanut butter (or jam if a nut allergy was present), at the same time of day without specifying morning or evening. However, we suggest that it would be best to assess olfactory function early in the day when sensitivity is at its lowest (before 1000 h) given that initial changes in odor perception may be mild and could be obscured by heightened sensitivity later in the day (Figure 1). If the test were performed in the evening (when sensitivity typically is highest), it might delay detection of changes in olfactory sensitivity and mitigate curtailing transmission through an olfactory diagnostic.
In the future, it will also be important to consider differences in olfactory sensitivity as a function of time of day, age, sex, and lighting history. For example, it may be the case that due to circadian dysregulation in COVID-19, olfactory sensitivity remains flat and thus comparing sensitivity changes (or lack thereof) over the day may help distinguish COVID-19 positive from negative cases. Another intriguing question is whether time of day regulates when the SARS-CoV-2 virus is most likely to be shed from the nose, an observation that would have major consequences for social mobility. Relatedly, could the timing of viral shedding be related in any meaningful way to changes in olfactory perception? These questions now need to be addressed by real-world, stringent experimentation.
Case 2. Clock Regulation as Part of COVID-19 Pathology: The Sleep-Wake Cycle as a Marker for Clock Regulated Function
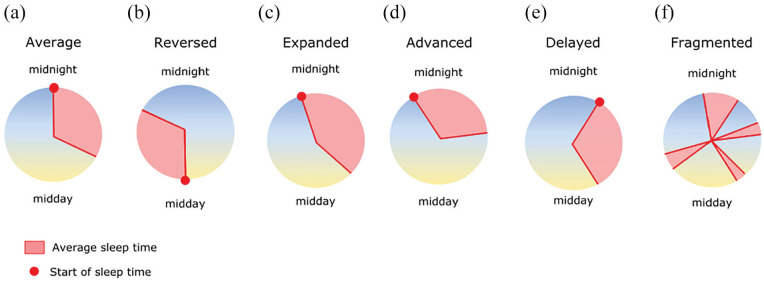
Sleep occupies about a third of our lifetime. The timing of the sleep-wake cycle (Figure 2) is one of the most salient features of the circadian clock in humans and is easily measured. The preferred timing of sleep and waking (chronotype) is a characteristic of the individual, controlled primarily by genes, light, and age (Jones et al., 2019; Roenneberg et al., 2004, 2007; Ptáček et al., 2007). In a robustly and stably synchronized individual, it is an indicator of the entrained phase of thousands of internal parameters. Disruption of sleep timing via regular use of an alarm clock or long-term shift work has consequences thought to reflect a desynchronization phenomenon (Roenneberg and Merrow, 2016). The impact of chronic social jetlag/shift-work includes increased risk of elevated body mass index (Roenneberg et al., 2012), higher incidence of cancers (Wegrzyn et al., 2017), and poorer work and cognitive performance (Devore et al., 2013; Yong et al., 2016). If COVID-19 were to disrupt sleep systematically, this symptom on its own would be expected to be detrimental to health and well-being.
Figure 2.
A catalog of aberrations concerning the timing of sleep. Red area indicates sleep time with the red circle showing the sleep start time for each condition. (a) Average sleep time for many people (Roenneberg et al., 2004). (b) A precisely reversed sleep-wake cycle relative to normal. This pattern has been reported rarely and often anecdotally. (c) With illnesses that are accompanied by fever, sleep duration often expands. Here, the timing of sleep symmetrically expands around the normal sleep time shown in (a). (d, e) Sleep timing can shift to an earlier or later phase. This would occur if the light-dark environment drastically and predictably were changed. (f) Sleep can become unconsolidated and fragmented (here, the indication of sleep onset is omitted due to multiple sleep episodes). Note that sleep timing is neither routinely documented in clinical practice nor in most surveys of sleep characteristics.
The sleep symptoms reported in acutely ill COVID-19 patients are several, but surprisingly understudied compared with studies on sleep disruptions of the general population during this pandemic. For example, one patient from an Egyptian hospital developed insomnia and restless leg syndrome (Tony et al., 2020), which resolved as the infection improved. Unfortunately, the reported data lacked quantification. In a survey of 43 patients with neurological symptoms during COVID-19 infection, a reversed sleep-wake cycle (Figure 2) was observed in two of them (Paterson et al., 2020). This extreme version of chronotype, reversal of the sleep-wake cycle, is rarely reported with respect to any illness. An example of reversed entrained phase was documented in a clock-less mutant fungal strain (Merrow et al., 1999). Mutant mice lacking the receptor for vasoactive intestinal peptide showed daily onsets of activity about 8 h earlier than wild-type mice. Interestingly, a protocol putting animals under tremendous metabolic strain (working for food) can lead to a reversed chronotype, accompanied by an extremely low core body temperature (Hut et al., 2011). Based on these data, we note that it is possible that due to the physiological stress of COVID-19, the reported symptoms in Paterson et al. (2020) could also describe conversion to an extreme early or late chronotype.
Figure 2 shows the set of possible changes in sleep that might be listed as sleep disturbance. There is no doubt that, for humans, sleeping in antiphase relative to conventional times constitutes a severe disruption of normal life. In the report of reversed chronotype in COVID-19 by Paterson et al. (2020), one of the two cases of antiphase sleep timing resolved at the time the paper was written. Thus, in this case, resolution of COVID-19 (and accompanying physiological duress) led to resolution of inverted sleep schedules.
Moving from a case report to an epidemiological scale study, Deng et al. (2021) performed a meta-analysis on the literature reporting depression, anxiety, and sleep disturbance in COVID-19 patients. They concluded that sleep disturbance was present in 34% of COVID-19 patients (n = 5153 from 31 studies). The patients were surveyed with the Pittsburgh Sleep Quality Index (PSQI), which asks about sleep quality, and the Insomnia Severity Index (ISI), which assesses insomnia. Thus, their study included sleep quality, sleep interruptions, and insomnia, but failed to sample sleep timing.
In long-COVID patients, sleep-related symptoms are reported at high frequency. A meta-analysis revealed that 52% of patients suffering from long-COVID report fatigue and that this is the most frequently reported symptom overall (Cares-Marambio et al., 2021). Lambert et al. (2020) found that sleeping more than usual was noted by up to 16% of respondents and difficulty sleeping was indicated by up to 50%. In Lambert et al. (2020), which surveyed thousands of patients recovering from COVID-19, fatigue was the most common complaint (similar to most other studies collecting long-COVID symptoms). Arguably, if one wished to identify a quantitative measure with which to study neurological impairment in COVID-19, the sleep-wake cycle is one that provides a robust quantitative measure, and its disturbance is widespread in these patients. The availability of qualitative versus quantitative information is a key issue. There is much of the former and little of the latter, a problem not limited to the reporting of COVID-19 symptomology.
We propose that objective measures of sleep can be recorded using a wrist-worn actimeter from patients who remain at least moderately active. These measures would include the timing and duration of sleep and the amount of activity within a sleep bout. Although actigraphy is not the gold standard for sleep assessment, it is easy to implement and would be sufficient for detecting changes in sleep timing that would reveal disruptions of the circadian clock. A study by Marino et al. (2013) compared actigraphy with polysomnography (simultaneous measurement of multiple parameters associated with sleep such as electroencephalogram, eye movements, muscle activity, and heart rate) in insomnia patients, and found accuracy of over 90% at the level of the individual. As we have no a priori reason to expect insomnia in long-COVID patients, and as we think that insomnia is more difficult to detect than shifts in (consolidated) sleep timing, we expect that actigraphy would be useful for assessing sleep changes ocurring with COVID-19 (see Figure 2). In the absence of actigraphy, self-reporting with questionnaires or commercially available sleep apps (e.g., SleepScore™) can be used for understanding sleep timing.
Catergorisation of the sleep timing characteristics of acutely ill COVID-19 patients as well as long-haul COVID sufferers may give insight into basic circadian biology and sleep, based on correlations with stochastic brain injuries and neuropathology that occur in a subset of those infected. Likewise, circulating cytokines known to affect sleep and the circadian clock (Cermakian et al., 2013; Besedovsky et al., 2019) could be monitored in COVID-19 to better understand how acute inflammation changes the timing of sleep.
Despite a growing literature on the modulation of viral infection by sleep or the circadian clock (Edgar et al., 2016; Scheiermann et al., 2018; Sengupta et al., 2019), we do not know if improved sleep is protective against SARS-CoV-2. This has prompted many reviews speculating on the potential for chronobiotics such as melatonin (Zhang, Wang et al., 2020; Anderson and Reiter, 2020) as adjuvant therapy. A recent retrospective analysis using available data from nearly 27,000 individuals in a COVID-19 registry found melatonin usage associated with a small (28%) reduced risk of a positive COVID-19 test after adjusting for potential confounds such as age, sex, and various comorbidities (Zhou et al., 2020). However, whether the frequency or dosage of melatonin administration affects COVID-19 infection was not investigated. It will be intriguing to learn the outcomes of several ongoing clinical trials testing melatonin supplementation as a COVID-19 therapy (Acuña-Castroviejo et al., 2020; García et al., 2020).
The extent of sleep disruption with illness—not limited to COVID-19—is likely vastly underreported as there is no standard and routine protocol for documentation in clinical environments. Given that subjective reports of sleep timing are easy to perform and that these methods have been highly successful in yielding insights into circadian biology, sleep assessment in patients would yield valuable dividends. If such effects are implemented rapidly, COVID-19 is a unique opportunity to demonstrate proof of principle.
Conclusion
We have identified several questions regarding COVID-19 and circadian functions in the nervous system. If clinical and/or at-home smell testing methods become routine, will the time of testing be an important variable in detecting the infection early and reliably? Will changes in daily olfactory performance be diagnostic for viral shedding, or the resolution of neurological symptoms following elimination of the virus? Does the timing of sleep change with this illness and does this correlate with symptoms? Does sleep or sleep timing contribute to the high incidence of fatigue reported in long-COVID sufferes? We have suggested simple measures (e.g., smell testing, actigraphy) that can be used to gather quantitative data reflecting time of day. The pervasive circadian rhythmicity of neurophysiology and behavior places chronobiology in a unique position to probe the connection between COVID-19 pathology and neurological damage. As has been suggested for other illnesses, interventions that support the circadian clock may eventually contribute to prevention and treatment of COVID-19.
Acknowledgments
We thank Prof. Kathryn Roecklein and Prof. Dr. Elizabeth Coulthard for discussions at the early stage of this work. We also acknowledge the Workshop “Chronobiology of COVID-19” (https://careconferences.org) as the coalescence point for the concepts discussed here.
Footnotes
Conflict of Interest Statement: The author(s) have no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
ORCID iD: Martha Merrow  https://orcid.org/0000-0002-8688-2360
https://orcid.org/0000-0002-8688-2360
References
- Acuña-Castroviejo D, Escames G, Figueira JC, Oliva P, Borobia AM, Acuña-Fernández C. (2020) Clinical trial to test the efficacy of melatonin in COVID-19. J Pineal Res 69:e12683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andalib S, Biller J, di Napoli M, Moghimi N, McCullough LD, Rubinos CA, O’Hana Nobleza C, Azarpazhooh MR, Catanese L, Elicer I, et al. (2021) Peripheral nervous system manifestations associated with COVID-19. Curr Neurol Neurosci Rep 21:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson G, Reiter RJ. (2020) Melatonin: roles in influenza, covid-19, and other viral infections. Rev Med Virol 30:e2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asadi-Pooya AA, Simani L. (2020) Central nervous system manifestations of COVID-19: a systematic review. J Neurol Sci 413:116832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baig AM. (2020) Neurological manifestations in COVID-19 caused by SARS-CoV-2. CNS Neurosci Ther 26:499-501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Besedovsky L, Lange T, Haack M. (2019) The sleep-immune crosstalk in health and disease. Physiol Rev 99:1325-1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhattacharjee AS, Joshi SV, Naik S, Sangle S, Abraham NM. (2020) Quantitative assessment of olfactory dysfunction accurately detects asymptomatic COVID-19 carriers. EClinicalMedicine 28:100575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilinska K, Jakubowska P, von Bartheld CS, Butowt R. (2020) Expression of the SARS-CoV-2 entry proteins, ACE2 and TMPRSS2, in cells of the olfactory epithelium: identification of cell types and trends with age. ACS Chem Neurosci 11:1555-1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brann DH, Tsukahara T, Weinreb C, Lipovsek M, van den Berge K, Gong B, Chance R, Macaulay IC, Chou HJ, Fletcher RB, et al. (2020) Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia. Sci Adv 6:eabc5801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantuti-Castelvetri L, Ojha R, Pedro LD, Djannatian M, Franz J, Kuivanen S, van der Meer F, Kallio K, Kaya T, Anastasina M, et al. (2020) Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity. Science 370:856-860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cares-Marambio K, Montenegro-Jiménez Y, Torres-Castro R, Vera-Uribe R, Torralba Y, Alsina-Restoy X, Vasconcello-Castillo L, Vilaró J. (2021) Prevalence of potential respiratory symptoms in survivors of hospital admission after coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis. Chron Respir Dis 18: 1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cermakian N, Lange T, Golombek D, Sarkar D, Nakao A, Shibata S, Mazzoccoli G. (2013) Crosstalk between the circadian clock circuitry and the immune system. Chronobiol Int 30:870-888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Melo GD, Lazarini F, Levallois S, Hautefort C, Michel V, Larrous F, Verillaud B, Aparicio C, Wagner S, Gheusi G, et al. (2021) COVID-19-related anosmia is associated with viral persistence and inflammation in human olfactory epithelium and brain infection in hamsters. Sci Transl Med 13:eabf8396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng J, Zhou F, Hou W, Silver Z, Wong CY, Chang O, Huang E, Zuo QK. (2021) The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann N Y Acad Sci 1486:90-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devore EE, Grodstein F, Schernhammer ES. (2013) Shift work and cognition in the nurses’ health study. Am J Epidemiol 178:1296-1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy JF, Czeisler CA. (2002) Age-related change in the relationship between circadian period, circadian phase, and diurnal preference in humans. Neurosci Lett 318:117-120. [DOI] [PubMed] [Google Scholar]
- Edgar RS, Stangherlin A, Nagy AD, Nicoll MP, Efstathiou S, O’Neill JS, Reddy AB. (2016) Cell autonomous regulation of herpes and influenza virus infection by the circadian clock. Proc Natl Acad Sci USA 113:10085-10090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García IG, García IG, Rodriguez-Rubio M, Rodriguez-Rubio M, Mariblanca AR, Mariblanca AR, de Soto LM, de Soto LM, García LD, García LD, et al. (2020) A randomized multicenter clinical trial to evaluate the efficacy of melatonin in the prophylaxis of SARS-CoV-2 infection in high-risk contacts (MeCOVID Trial): a structured summary of a study protocol for a randomised controlled trial. Trials 21:466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerkin RC, Ohla K, Veldhuizen MG, Joseph PV, Kelly CE, Bakke AJ, Steele KE, Farruggia MC, Pellegrino R, Pepino MY, et al. (2021) Recent smell loss is the best predictor of COVID-19 among individuals with recent respiratory symptoms. Chem Senses 46:bjaa081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goncalves S, Goldstein BJ. (2016) Pathophysiology of olfactory disorders and potential treatment strategies. Curr Otorhinolaryngol Rep 4:115-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gözen ED, Aliyeva C, Tevetoğlu F, Karaali R, Balkan İİ, Yener HM, Özdoğan HA. (2021) Evaluation of olfactory function with objective tests in COVID-19-positive patients: a cross-sectional study. Ear Nose Throat J 100:169S-173S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granados-Fuentes D, Tseng A, Herzog ED. (2006) A circadian clock in the olfactory bulb controls olfactory responsivity. J Neurosci 26:12219-12225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannum ME, Ramirez VA, Lipson SJ, Herriman RD, Toskala AK, Lin C, Joseph PV, Reed DR. (2020) Objective sensory testing methods reveal a higher prevalence of olfactory loss in COVID-19-positive patients compared to subjective methods: a systematic review and meta-analysis. Chem Senses 45:865-874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haspel J, Kim M, Zee P, Schwarzmeier T, Montagnese S, Panda S, Albani A, Merrow M. (2021) A timely call to arms: COVID-19, the circadian clock, and critical care. J Biol Rhythms 36:55-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herz RS. (2016) The role of odor-evoked memory in psychological and physiological health. Brain Sci 6:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herz RS, Reen E, van Barker DH, Hilditch CJ, Bartz AL, Carskadon MA. (2018) The influence of circadian timing on olfactory sensitivity. Chem Senses 43:45-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hut RA, Pilorz V, Boerema AS, Strijkstra AM, Daan S. (2011) Working for food shifts nocturnal mouse activity into the day. PLoS ONE 6:e17527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones SE, Lane JM, Wood AR, van Hees VT, Tyrrell J, Beaumont RN, Jeffries AR, Dashti HS, Hillsdon M, Ruth KS, et al. (2019) Genome-wide association analyses of chronotype in 697,828 individuals provides insights into circadian rhythms. Nat Commun 10:343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klopfenstein T, Kadiane-Oussou NJ, Toko L, Royer P-Y, Lepiller Q, Gendrin V, Zayet S. (2020) Features of anosmia in COVID-19. Med Mal Infect 50:436-439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan B, Dryer SE, Hardin PE. (1999) Circadian rhythms in olfactory responses of Drosophila melanogaster. Nature 400:375-378. [DOI] [PubMed] [Google Scholar]
- Kronfeld-Schor N, Stevenson TJ, Nickbakhsh S, Schernhammer ES, Dopico XC, Dayan T, Martinez M, Helm B. (2021) Drivers of infectious disease seasonality: potential implications for COVID-19. J Biol Rhythms 36:35-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert NJ. and Survivor Corps (2020) COVID-19 “Long Hauler” symptoms survey report. Indiana University School of Medicine. www.survivorcorps.com
- Laurendon T, Radulesco T, Mugnier J, Gérault M, Chagnaud C, El Ahmadi AA, Varoquaux A. (2020) Bilateral transient olfactory bulb edema during COVID-19-related anosmia. Neurology 95:224-225. [DOI] [PubMed] [Google Scholar]
- Lechien JR, Chiesa-Estomba CM, Beckers E, Mustin V, Ducarme M, Journe F, Marchant A, Jouffe L, Barillari MR, Cammaroto G, et al. (2021) Prevalence and 6-month recovery of olfactory dysfunction: a multicentre study of 1363 COVID-19 patients. J Intern Med: 1-11. doi: 10.1111/joim.13209. [DOI] [PubMed] [Google Scholar]
- Lechien JR, Radulesco T, Calvo-Henriquez C, Chiesa-Estomba CM, Hans S, Barillari MR, Cammaroto G, Descamps G, Hsieh J, Vaira L, et al. (2021) ACE2 & TMPRSS2 expressions in head & neck tissues: a systematic review. Head Neck Pathol 15:225-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y, Min P, Lee S, Kim SW. (2020) Prevalence and duration of acute loss of smell or taste in COVID-19 patients. J Korean Med Sci 35:e174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinson R, Elbaz M, Ben-Ami R, Shasha D, Levinson T, Choshen G, Petrov K, Gadoth A, Paran Y. (2020) Time course of anosmia and dysgeusia in patients with mild SARS-CoV-2 infection. Infect Diseases 52:600-602. [DOI] [PubMed] [Google Scholar]
- Li J, Long X, Zhu C, Wang H, Wang T, Lin Z, Xiong N. (2020) Olfactory dysfunction in recovered coronavirus disease 2019 (COVID-19) patients. Mov Disord 35:1100-1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lötsch J, Nordin S, Hummel T, Murphy C, Kobal G. (1997) Chronobiology of nasal chemosensitivity: do odor or trigeminal pain thresholds follow a circadian rhythm? Chem Senses 22:593-598. [DOI] [PubMed] [Google Scholar]
- Mahalaxmi I, Kaavya J, Mohana Devi S, Balachandar V. (2021) COVID-19 and olfactory dysfunction: a possible associative approach towards neurodegenerative diseases. J Cell Physiol 236:763-770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malone SK, Patterson F, Lu Y, Lozano A, Hanlon A. (2016) Ethnic differences in sleep duration and morning-evening type in a population sample. Chronobiol Int 33:10-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marino M, Li Y, Rueschman MN, Winkelman JW, Ellenbogen JM, Solet JM, Dulin H, Berkman LF, Buxton OM. (2013) Measuring sleep: accuracy, sensitivity, and specificity of wrist actigraphy compared to polysomnography. Sleep 36:1747-1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matschke J, Lütgehetmann M, Hagel C, Sperhake JP, Schröder AS, Edler C, Mushumba H, Fitzek A, Allweiss L, Dandri M, et al. (2020) Neuropathology of patients with COVID-19 in Germany: a post-mortem case series. Lancet Neurol 19:919-929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrow M, Brunner M, Roenneberg T. (1999) Assignment of circadian function for the Neurospora clock gene frequency. Nature 399:584-586. [DOI] [PubMed] [Google Scholar]
- Mure LS, Le HD, Benegiamo G, Chang MW, Rios L, Jillani N, Ngotho M, Kariuki T, Dkhissi-Benyahya O, Cooper HM, et al. (2018) Diurnal transcriptome atlas of a primate across major neural and peripheral tissues. Science 359:eaao0318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordin S, Lötsch J, Murphy C, Hummel T, Kobal G. (2003) Circadian rhythm and desensitization in chemosensory event-related potentials in response to odorous and painful stimuli. Psychophysiology 40:612-619. [DOI] [PubMed] [Google Scholar]
- Olmedo M, O’Neill JS, Edgar RS, Valekunja UK, Reddy AB, Merrow M. (2012) Circadian regulation of olfaction and an evolutionarily conserved, nontranscriptional marker in Caenorhabditis elegans. Proc Natl Acad Sci USA 109:20479-20484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otte MS, Klussmann JP, Luers JC. (2020) Persisting olfactory dysfunction in patients after recovering from COVID-19. J Infect 81:e58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paterson RW, Brown RL, Benjamin L, Nortley R, Wiethoff S, Bharucha T, Jayaseelan DL, Kumar G, Raftopoulos RE, Zambreanu L, et al. (2020) The emerging spectrum of COVID-19 neurology: clinical, radiological and laboratory findings. Brain 143:3104-3120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pezzini A, Padovani A. (2020) Lifting the mask on neurological manifestations of COVID-19. Nat Rev Neurol 16:636-644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierron D, Pereda-Loth V, Mantel M, Moranges M, Bignon E, Alva O, Kabous J, Heiske M, Pacalon J, David R, et al. (2020) Smell and taste changes are early indicators of the COVID-19 pandemic and political decision effectiveness. Nat Commun 11:5152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Politi LS, Salsano E, Grimaldi M. (2020) Magnetic resonance imaging alteration of the brain in a patient with coronavirus disease 2019 (COVID-19) and anosmia. JAMA Neurol 77:1028-1029. [DOI] [PubMed] [Google Scholar]
- Ptáček LJ, Jones CR, Fu Y-H. (2007) Novel insights from genetic and molecular characterization of the human clock. Cold Spring Harb Symp Quant Biol 72:273-277. [DOI] [PubMed] [Google Scholar]
- Ray S, Reddy AB. (2020) COVID-19 management in light of the circadian clock. Nat Rev Mol Cell Biol 21:494-495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roenneberg T, Allebrandt KV, Merrow M, Vetter C. (2012) Social jetlag and obesity. Curr Biol 22:939-943. [DOI] [PubMed] [Google Scholar]
- Roenneberg T, Merrow M. (2016) The circadian clock and human health. Curr Biol 26:R432-R443. [DOI] [PubMed] [Google Scholar]
- Roenneberg T, Kuehnle T, Pramstaller PP, Ricken J, Havel M, Guth A, Merrow M. (2004) A marker for the end of adolescence. Curr Biol 14:R1038-R1039. [DOI] [PubMed] [Google Scholar]
- Roenneberg T, Kumar CJ, Merrow M. (2007) The human circadian clock entrains to sun time. Curr Biol 17:R44-R45. [DOI] [PubMed] [Google Scholar]
- Salje H, Kiem CT, Lefrancq N, Courtejoie N, Bosetti P, Paireau J, Andronico A, Hozé N, Richet J, Dubost CL, et al. (2020) Estimating the burden of SARS-CoV-2 in France. Science 369:208-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheiermann C, Gibbs J, Ince L, Loudon A. (2018) Clocking in to immunity. Nat Rev Immunol 18:423-437. [DOI] [PubMed] [Google Scholar]
- Sengupta S, Ince L, Sartor F, Borrmann H, Zhuang X, Naik A, Curtis A, McKeating JA. (2021) Clocks, viruses, and immunity: lessons for the COVID-19 pandemic. J Biol Rhythms 36:23-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sengupta S, Tang SY, Devine JC, Anderson ST, Nayak S, Zhang SL, Valenzuela A, Fisher DG, Grant GR, López CB, et al. (2019) Circadian control of lung inflammation in influenza infection. Nat Commun 10:4107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon IH, Normandin E, Bhattacharyya S, Mukerji SS, Keller K, Ali AS, Adams G, Hornick JL, Padera RF, Sabeti P. (2020) Neuropathological features of covid-19. N Engl J Med 383:989-992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinato G, Fabbris C, Polesel J, Cazzador D, Borsetto D, Hopkins C, Boscolo-Rizzo P. (2020) Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection. JAMA 323:2089-2091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sungnak W, Huang N, Bécavin C, Berg M, Queen R, Litvinukova M, Talavera-López C, Maatz H, Reichart D, Sampaziotis F, et al. (2020) SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat Med 26:681-687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tony AA, Tony EA, Ali SB, Ezzeldin AM, Mahmoud AA. (2020) COVID-19-associated sleep disorders: a case report. Neurobiol Sleep Circadian Rhythms 9:100057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varatharaj A, Thomas N, Ellul MA, Davies NWS, Pollak TA, Tenorio EL, Sultan M, Easton A, Breen G, Zandi M, et al. (2020) Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiatry 7:875-882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S, Zhang Y, Ding W, Meng Y, Hu H, Liu Z, Zeng X, Wang M. (2020) Psychological distress and sleep problems when people are under interpersonal isolation during an epidemic: a nationwide multicenter cross-sectional study. Eur Psychiatry 63:e77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wegrzyn LR, Tamimi RM, Rosner BA, Brown SB, Stevens RG, Eliassen AH, Laden F, Willett WC, Hankinson SE, Schernhammer ES. (2017) Rotating night-shift work and the risk of breast cancer in the nurses’ health studies. Am J Epidemiol 186:532-540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss JJ, Attuquayefio TN, White EB, Li F, Herz RS, White TL, Campbell M, Geng B, Datta R, Wyllie AL, et al. (2020) Tracking smell loss to identify healthcare workers with SARS-CoV-2 infection. MedRxiv. doi: 10.1101/2020.09.07.20188813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitcroft KL, Hummel T. (2020) Olfactory dysfunction in COVID-19: diagnosis and management. JAMA 323:2512-2514. [DOI] [PubMed] [Google Scholar]
- Woodruff MC, Ramonell RP, Lee E-H, Sanz I. (2020) Clinically identifiable autoreactivity is common in severe SARS-CoV-2 infection. MedRxiv. doi: 10.1101/2020.10.21.20216192. [DOI] [Google Scholar]
- Yong M, Fischer D, Germann C, Lang S, Vetter C, Oberlinner C. (2016) Are chronotype, social jetlag and sleep duration associated with health measured by Work Ability Index? Chronobiol Int 33:721-729. [DOI] [PubMed] [Google Scholar]
- Zhang BZ, Chu H, Han S, Shuai H, Deng J, Hu YF, Gong H, Lee AC, Zou Z, Yau T, et al. (2020) SARS-CoV-2 infects human neural progenitor cells and brain organoids. Cell Res 30:928-931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang R, Wang X, Ni L, Di X, Ma B, Niu S, Liu C, Reiter RJ. (2020) COVID-19: melatonin as a potential adjuvant treatment. Life Sci 250:117716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Y, Hou Y, Shen J, Mehra R, Kallianpur A, Culver DA, Gack MU, Farha S, Zein J, Comhair S, et al. (2020) A network medicine approach to investigation and population-based validation of disease manifestations and drug repurposing for COVID-19. PLoS Biol 18:e3000970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zubair AS, McAlpine LS, Gardin T, Farhadian S, Kuruvilla DE, Spudich S. (2020) Neuropathogenesis and neurologic manifestations of the coronaviruses in the age of coronavirus disease 2019: a review. JAMA Neurol 77:1018-1027. [DOI] [PMC free article] [PubMed] [Google Scholar]