Abstract
Background:
During the COVID-19 pandemic, telemedicine use rapidly and dramatically increased for management of diabetes mellitus. It is unknown whether access to telemedicine care has been equitable during this time. This study aimed to identify patient-level factors associated with adoption of telemedicine for subspecialty diabetes care during the pandemic.
Methods:
We conducted an explanatory sequential mixed-methods study using data from a single academic medical center. We used multivariate logistic regression to explore associations between telemedicine use and demographic factors for patients receiving subspecialty diabetes care between March 19 and June 30, 2020. We then surveyed a sample of patients who received in-person care to understand why these patients did not use telemedicine.
Results:
Among 1292 patients who received subspecialty diabetes care during the study period, those over age 65 were less likely to use telemedicine (OR: 0.34, 95% CI: 0.22-0.52, P < .001), as were patients with a primary language other than English (OR: 0.53, 95% CI: 0.31-0.91, P = .02), and patients with public insurance (OR: 0.64, 95% CI: 0.49-0.84, P = .001). Perceived quality of care and technological barriers were the most common reasons cited for choosing in-person care during the pandemic.
Conclusions:
Our findings suggest that, amidst the COVID-19 pandemic, there have been disparities in telemedicine use by age, language, and insurance for patients with diabetes mellitus. We anticipate telemedicine will continue to be an important care modality for chronic conditions in the years ahead. Significant work must therefore be done to ensure that telemedicine services do not introduce or widen population health disparities.
Keywords: COVID-19, diabetes mellitus, health disparities, telemedicine
Introduction
Since the start of the COVID-19 pandemic, telemedicine use has rapidly and dramatically increased for management of a variety of chronic conditions,1 raising important questions about whether access to telemedicine care has been equitable or may be contributing to health disparities.2,3 Management of diabetes mellitus is particularly well-suited to telemedicine because treatment decisions rely primarily on patient-generated health data (PGHD) and a health-coaching approach to behavior management.4 Although PGHD from traditional fingerstick glucose meters and insulin pumps can only be accessed and shared from a computer with internet access, many newer glucose meters, continuous glucose monitors, insulin pumps, and “smart” insulin pens can facilitate data-sharing via Bluetooth connectivity and cellular networks. This functionality is highly relevant because recent survey data from the Pew Research Center reveal that the majority of Americans in every age category and racial/ethnic group now own a smartphone, including those in the least privileged education and income brackets, and those living in rural areas.5 Furthermore, 15%-20% of Americans (and a higher percentage of young adults) are “smartphone dependent,” meaning they do not have broadband internet access at home.5
At the beginning of the COVID-19 pandemic, diabetes practices across the United States adopted telemedicine at a breathless pace in order to facilitate recommended social distancing while continuing to deliver needed care. The process of adoption varied by practice site, with some moving to entirely remote care and others offering a mix of in-person and telemedicine modalities. At University of California, Davis (UC Davis), an academic medical center in northern California, both telemedicine and in-person care were offered during the pandemic. After a statewide shelter-in-place order was issued on March 19, 2020, diabetes patients with scheduled appointments in endocrinology were proactively contacted to offer telemedicine care in lieu of an in-person visit. As a result, telemedicine encounters expanded from only 1% of subspecialty diabetes visits to greater than 50% of subspecialty diabetes visits during the three months before and after the shelter-in-place order. Patients who were unable or disinclined to participate in telemedicine were offered in-person care or telephone visits.
To explore this shift in telemedicine use for diabetes care, we conducted an explanatory sequential mixed-methods study that included an observational retrospective analysis and a patient survey with open-ended questions. The observational analysis compared patients who experienced only in-person or telephone visits versus those who utilized telemedicine for subspecialty diabetes care at UC Davis after the shelter-in-place order to identify key differences that might indicate disparities in telemedicine access. We then surveyed patients who opted for in-person care to better understand individual or system-level barriers to telemedicine use in this population. We hypothesized that demographic characteristics would be associated with uptake of telemedicine for diabetes care during the shelter-in-place order.
Methods
Telemedicine has been defined broadly by the Institute of Medicine as “the use of electronic information and communications technologies to provide and support health care when distance separates the participants.”6 In this manuscript, we use the term telemedicine to refer specifically to the delivery of medical care via real-time video encounters between patients and their health care providers. These telemedicine visits maintain traditional visit structure but are conducted virtually using internet-based video applications on patients’ smartphones or personal computers.
Observational Study
Participants and setting
All UC Davis patients who completed a visit with an endocrinologist for a diagnosis of type 1 or type 2 diabetes mellitus (ICD10 of E10.* or E11.*) from the beginning of the shelter-in-place order on March 19, 2020 through June 30, 2020 were included in the observational study. Because we were interested in the characteristics of those who did not successfully utilize video-based telemedicine, we grouped telephone encounters with in-person encounters; this categorization is supported by recently published studies that suggest that patients receiving telephone care during the pandemic differ significantly from those receiving video care.7,8
Data elements and collection
Demographic data on all eligible patients, including sex, age, race/ethnicity, insurance status, primary language, and zip code, were abstracted from the UC Davis electronic health record (EHR). We also abstracted visit dates and whether the visit was completed using telemedicine. To assess rural residence, we matched patient zip code to the Federal Office of Rural Health Policy (FORHP) list of eligible zip codes.9 We also matched patient zip code to Census Bureau income statistics to determine the median household income associated with the patient’s zip code. We then divided our study population into patients who had any telemedicine visits for diabetes care during the study period, and patients who had none.
Statistical analysis
We fit a multivariate logistic regression model to calculate the adjusted odds of telemedicine use and corresponding 95% confidence intervals. We examined the association of telemedicine use with age, sex, race/ethnicity, urban/rural residence, primary language, public/private insurance, median household income associated with patient zip code, and diabetes type. We used interaction terms to examine effect modification by age, sex, urban/rural residence, language, insurance, race, and median income; interaction terms were excluded from the final model if they were not significant at the P = .05 level. We reported two-tailed tests of significance at the P < .05 level. All statistical analyses were performed using Stata software, version 16.1.10
Survey
Participants and setting
To gain further insight into why some patients chose an in-person visit compared with a telemedicine visit, we conducted surveys by phone with adult patients and parents of pediatric patients who were seen in-person at an endocrinology specialty clinic for a diagnosis of diabetes mellitus during the study period. We excluded new patients (who were not uniformly offered telemedicine during this time), patients with additional non-diabetes endocrine diagnoses such as thyroid cancer or hypopituitarism (which might require an in-person encounter), and patients for whom the provider had noted in the EHR that an in-person appointment was needed. For the survey component, we also excluded patients seen at satellite clinic locations, because the standardization of processes for patient outreach and rescheduling was less certain at these sites, and we hoped to engage survey participants who were specifically offered telemedicine visits but chose to receive in-person care.
Survey questions and procedures
We generated a random sample of 80 eligible patients from the EHR and attempted up to six total phone calls to each, including on evenings. Participants first provided verbal consent, and then were asked if they were offered telemedicine for their recent diabetes visit. If they answered no to this screening question, the survey was ended. Otherwise, they were asked: (1) Why did you choose to come in-person for this visit instead of using telemedicine? and (2) Would you be likely to use a video visit in the future for diabetes care if it was offered? All phone interviews were conducted by one trained researcher to minimize variation. Reasons were recorded briefly by the surveyor in one to six words and were subsequently categorized by the research team. Survey data were recorded anonymously and were not connected to EHR data.
General
All aspects of this study were approved by the UC Davis Institutional Review Board.
Results
Observational Study
A total of 1292 adult and pediatric patients were seen for diabetes care with a UC Davis endocrinologist between March 19 and June 30, 2020. Of these patients, 552 completed at least one telemedicine visit and the remaining 740 received in-person or telephone care only. Telemedicine, in-person, and telephone visits were conducted by 17 endocrinologists during the study period. Table 1 shows demographic characteristics of the sample. Most patients receiving subspecialty diabetes care lived in urban areas (87.2%), spoke English as their primary language (93.0%), and had public insurance (68.8%). Patients seen for type 2 diabetes made up 57.2% of our study population, and the remaining 42.8% were seen for type 1 diabetes.
Table 1.
Study Population.
| All patients N (%) |
In-person or telephone care
only N (%) |
Telemedicine care N (%) | |
|---|---|---|---|
| Age | |||
| 1-24 | 360 (28.2) | 171 (23.3) | 189 (34.7) |
| 25-49 | 155 (12.1) | 64 (8.7) | 91 (16.7) |
| 50-65 | 308 (24.1) | 170 (23.2) | 138 (25.4) |
| >65 | 455 (35.6) | 329 (44.8) | 126 (23.2) |
| Diabetes type | |||
| Type 1 | 553 (42.8) | 271 (36.6) | 282 (51.1) |
| Type 2 | 739 (57.2) | 469 (63.4) | 270 (48.9) |
| Sex | |||
| Male | 613 (47.5) | 350 (47.3) | 263 (47.6) |
| Female | 679 (52.6) | 390 (52.7) | 289 (52.4) |
| Urban/rural residence | |||
| Urban | 1,127 (87.2) | 652 (88.1) | 475(86.1) |
| Rural | 165 (12.8) | 88 (11.9) | 77 (14.0) |
| Language | |||
| English | 1,201 (93.0) | 671 (90.7) | 530 (96.0) |
| Language other than English | 91 (7.0) | 69 (9.3) | 22 (4.0) |
| Insurance | |||
| Private | 403 (31.2) | 177 (23.9) | 226 (40.9) |
| Public | 889 (68.8) | 563 (76.1) | 326 (59.1) |
| Median annual household income | |||
| $50 000 or less | 353 (27.3) | 201 (27.2) | 152 (27.5) |
| $50 001-60 000 | 337 (26.1) | 203 (27.4) | 134 (24.3) |
| $60 001-$80 000 | 403 (31.2) | 217 (29.3) | 186 (33.7) |
| >$80 000 | 199 (15.4) | 119 (16.1) | 80 (14.5) |
| Race/ethnicity | |||
| White | 735 (56.9) | 406 (54.9) | 329 (59.6) |
| Black | 135 (10.5) | 75 (10.1) | 60 (10.9) |
| Hispanic | 192 (14.9) | 115 (15.5) | 77 (14.0) |
| Asian | 132 (10.2) | 84 (11.4) | 48 (8.7) |
| Native American, Native Hawaiian, or Alaska Native | 29 (2.2) | 19 (2.6) | 10 (1.8) |
| Other or unknown | 69 (5.3) | 41 (5.5) | 28 (5.1) |
| Total N | 1292 | 740 | 552 |
Table 2 shows the results of our logistic regression for telemedicine use. Older age was associated with significantly lower odds of telemedicine use. The odds of using telemedicine was 0.62 for those aged 50–65 (95% CI: 0.41–0.93, P = .02) and dropped to 0.34 for those over age 65 (95% CI: 0.22-0.52, P < .001). Speaking a language other than English was also associated with lower odds of telemedicine use (OR: 0.53, 95% CI: 0.31-0.91, P = .02). In addition, patients with public insurance were significantly less likely than those with private insurance to use telemedicine (OR: 0.64, 95% CI: 0.49-0.84, P = .001). We found no association between telemedicine use and sex, type of diabetes, urban/rural residence, race/ethnicity, or neighborhood median household income.
Table 2.
Adjusted Odds of Telemedicine Care.
| Odds ratio | 95% CI | P value | |
|---|---|---|---|
| Age | |||
| 1-24 | Ref | ||
| 25-49 | 1.09 | 0.70-1.45 | .67 |
| 50-65 | 0.62 | 0.41-0.93 | .02 |
| >65 | 0.34 | 0.22-0.52 | <.001 |
| Diabetes type | |||
| Type 1 | Ref | ||
| Type 2 | 1.09 | 0.78-1.54 | .61 |
| Sex | |||
| Male | Ref | ||
| Female | 1.02 | 0.80-1.28 | .90 |
| Urban/rural residence | |||
| Urban | Ref | ||
| Rural | 1.00 | 0.70-1.45 | .99 |
| Language | |||
| English | Ref | ||
| Language other than English | 0.53 | 0.31-0.91 | .02 |
| Insurance | |||
| Private | Ref | ||
| Public | 0.64 | 0.49-0.84 | .001 |
| Median household income | |||
| $50 000 or less | Ref | ||
| $50 001-$60 000 | 1.10 | 0.79-1.54 | .56 |
| $60 001-$80 000 | 1.35 | 0.98-1.85 | .06 |
| >$80 000 | 0.92 | 0.63-1.36 | .67 |
| Race/ethnicity | |||
| White | Ref | ||
| Black | 1.10 | 0.74-1.65 | .64 |
| Hispanic | 0.81 | 0.56-1.15 | .24 |
| Asian | 0.87 | 0.57-1.32 | .52 |
| Native American, Native Hawaiian, or Alaska Native | 0.65 | 0.28-1.52 | .32 |
| Other or unknown | 0.82 | 0.48-1.40 | .47 |
Survey
Out of 80 patients randomly selected for the survey, 56 agreed to participate. Only one patient declined to participate; the remaining 23 were not able to be reached by phone after six attempts. Three of the 56 patients who agreed to participate reported that they were not offered a telemedicine visit for diabetes care during the study period. The remaining 53 respondents (15 parents and 38 adult patients) completed the open-ended survey questions. Parents of pediatric patients had a higher response rate (94.1%) than adult patients (63.5%).
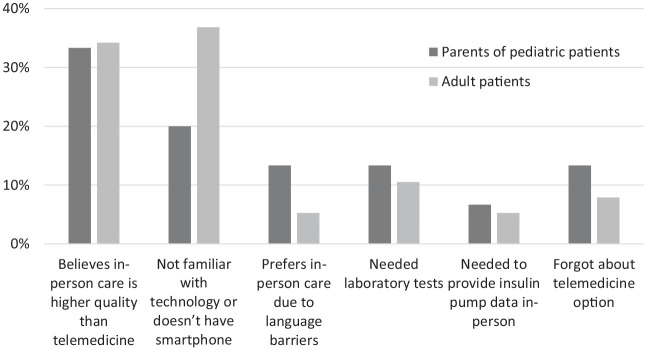
Figure 1 shows the reasons given by these 53 respondents for choosing an in-person visit instead of a telemedicine visit for diabetes management. Overall, the most cited reasons among both adult patients and caretakers of pediatric patients were a belief that in-person care is higher quality than telemedicine and a lack of familiarity with technology or lack of smartphone access. Being unfamiliar with the technology required or not having a smartphone was the primary barrier cited by 36.8% of adult patients and 20% of parents of pediatric patients. The perception that in-person care is of higher quality than telemedicine care was cited by 34.2% of adult patients and 33.3% of parents of pediatric patients. Other reasons provided included language barriers (5.2% of adult patients, 13.3% of parents), needing lab tests (10.5% of adults, 13.3% of parents), needing to provide insulin pump data in-person (5.3% of adult patients, 6.7% of parents), and forgetting to change the appointment or forgetting that the appointment was supposed to be a video visit (7.9% of adult patients, 13.3% of parents). Most respondents who were parents of pediatric patients (53.3%) said that they would use a telemedicine visit for their child’s diabetes care if they were offered one in the future. In contrast, the majority of adult patient respondents (81.6%) reported that they likely would not use telemedicine for diabetes care in the future.
Figure 1.
Reasons given for choosing in-person diabetes care during COVID-19 pandemic (N = 53).
Discussion
This study at an academic medical center in northern California found that older adults, patients with public insurance, and those with a primary language other than English were less likely to adopt telemedicine for subspecialty diabetes care during a statewide shelter-in-place order. Our findings have important health implications. If patients in these high-risk groups do not access care via telemedicine, their alternatives are to defer recommended visits, receive limited care by phone, or seek in-person care. The former two options run counter to published recommendations for diabetes management,11 while the last option increases the risk of contracting COVID-19 among diabetes patients who are already predisposed to greater disease-related morbidity and mortality. Our study is the first to examine disparities in telemedicine use for subspecialty diabetes care during the pandemic. However, analyses of care delivery to primary care populations during the same time frame also concluded that older adults,3,12 patients with non-English language preferences,3,12 and those with public insurance12 were less likely to receive care after widescale implementation of telemedicine, suggesting these associations are robust.
Our survey data provide insight into the reasons for these disparities in telemedicine adoption. First, many adult patients who chose to seek care in-person reported that they did so because they believe in-person care to be higher quality than care received through telemedicine. The majority of these patients also stated that they would not choose to use telemedicine for diabetes care in the future. This viewpoint appears to be more prevalent among older adults based on a recent global survey of people with type 1 diabetes, which found that the majority of respondents >65 years of age had never used and did not intend to use telemedicine for diabetes care moving forward.13 Our survey results also reveal that a lack of access to or comfort with the necessary technology for a video visit represented a primary barrier to adopting telemedicine during the pandemic. Although Pew Research Center data show that the majority of Americans of all ages now own smartphones, ownership rates are still significantly lower among individuals >65 years of age (53%) compared to those aged 50-64 years (79%) or <50 years (>90%).6 In addition, individuals from households with annual income <$30 000 (just below our state’s family-of-four income threshold to qualify for Medicaid) are less likely to own smartphones (71%) compared to those from households with annual income >$50 000 (>90%).6 Therefore, it is likely that limited access to the necessary technology played a role in reducing telemedicine adoption by older adults and those with public insurance.
It is also important to note that digital literacy can be low even among groups with high smartphone ownership,14 and particularly among non-English speakers.15 During the study period, UC Davis offered telemedicine through specific HIPAA-compliant video applications rather than allowing patients to use familiar chat applications, as advocated by some providers during the pandemic.4 The need to download and use a new video application may therefore have served as an additional barrier to telemedicine use, and may have disproportionately affected those with lower digital literacy, including individuals with a primary language besides English. In addition, early in the pandemic, interpretation services at UC Davis were more difficult to access by telemedicine than in-person. This system-level factor may have influenced providers and office staff to be less likely to offer telemedicine to non-English-speaking patients. Additionally, patients themselves may have been concerned that they could not receive effective interpretation services remotely. Indeed, our survey results revealed that these patients worried their language barriers would be more difficult to overcome during a video visit.
Interestingly, our analysis found that after adjustment for other demographic factors, patient race/ethnicity, sex, rural/urban status, and median neighborhood household income were not significantly associated with telemedicine use during the pandemic. Our review of other post-COVID-19 telemedicine analyses yields both similar and contrasting findings. A recent analysis of telemedicine child neurology encounters demonstrated no disparities in use based on sex, ethnicity, race, or income.7 However, various analyses of primary care telemedicine encounters during COVID-19 do suggest disparities by race/ethnicity3,8,12 and rurality.8 It may be that these factors in our population were strongly correlated with other covariates—such as insurance type and primary language—and thus did not demonstrate individual significance in our multivariate model, or that these factors were less influential in patient decisions when seeking subspecialty diabetes care compared to primary care. It may also be that proactive outreach from UC Davis staff to assist patients from all demographic groups in scheduling and preparing for telemedicine visits was highly successful in mitigating some disparities. UC Davis has a long history of providing care via telemedicine,16 and was able to utilize dedicated telemedicine staff in addition to clinic scheduling staff to assist with conversions of in-person to video care. Although patients with type 1 diabetes made up a greater proportion of the telemedicine cohort, diabetes type was not significantly associated with telemedicine adoption in our adjusted model due to its strong correlation with age.
This study’s strengths include a large study sample and a mixed-methods approach that utilized patient survey data to complement the findings of our observational analysis. The fact that receipt of telemedicine was not randomized for our cohort would be a weakness for an interventional trial but is in fact a strength when exploring real-world uptake of telemedicine during a public health emergency. Because telemedicine was offered broadly but not exclusively during the study period at UC Davis, evaluating which patients self-selected into telemedicine versus non-telemedicine care provides important insights about how and for whom telemedicine may be a patient-centered form of health care delivery among patients with diabetes.
One limitation of our observational study is the fact that we could not control or adjust for provider-level factors that may have influenced adoption of telemedicine. Although a widescale effort was made to convert scheduled appointments from in-person to video during the study period, it is likely that opinions of providers and staff about which patients were most likely to be successful with telemedicine affected how persistent they were in attempting to convert appointments. Thus, the selection of patients into in-person and telemedicine care cohorts undoubtedly reflects provider biases in addition to patient choice. The primary limitation of the survey component for this project is potential nonresponse bias, as 30% of the sample identified for the survey component of the study did not answer the telephone and therefore were not represented in our results. Additionally, we surveyed only 56 of the 740 diabetes patients who did not adopt telemedicine during our study period. Given that this is a relatively small subset of the larger group, it is possible that reasons cited by respondents for choosing in-person care are not representative of the larger group. We approached this aspect of our study as hypothesis-generating, and believe that a larger volume, more systematic survey of patient perspectives on telemedicine would be valuable in the future. In addition, an in-depth qualitative exploration into patients’ decision-making processes around telehealth could yield rich data and provide more detailed insights about this phenomenon. Finally, we did not link survey responses with patient characteristics in our analysis, but it would be interesting in future studies to explore how survey responses correlate with demographic and clinical factors.
Conclusions
The clinical imperative and health care policies introduced by the COVID-19 pandemic have led to the swift and widespread application of telemedicine for diabetes management across the United States. With this abrupt transformation in care come important questions about whether, how, and for whom this change has been beneficial. We analyzed telemedicine use for subspecialty diabetes care at an academic medical center in northern California during a statewide shelter-in-place order. We discovered that older adults, patients with public insurance, and those requiring language interpretation services were less likely to utilize telemedicine for subspecialty diabetes care during this time. These findings suggest there is significant work to be done to improve future adoption of telemedicine for patients who would benefit, and to ensure telemedicine services neither widen existing health disparities nor create new ones.
Footnotes
Abbreviations: COVID-19, Coronavirus Disease 2019; EHR, electronic health record; FORHP, Federal Office of Rural Health Policy; HIPAA, Health Insurance Portability and Accountability Act; PGHD, patient-generated health data.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: S.H., J.R., and S.C. have no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
T.K. has received consulting fees from Eli Lilly.
A.N. has received research support from Cisco Systems, Inc; has received consulting fees from Nokia Growth Partners, Grand Rounds, Intuity Medical, Medtronic, Eli Lilly, and Roche; serves as advisor to Steady Health (received stock options); has received speaking honoraria from Academy Health and Symposia Medicus; has written for WebMD (received compensation); and is a medical advisor and cofounder of Tidepool (for which he has received no compensation).
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was funded by a research award from the Children’s Miracle Network in association with UC Davis Children’s Hospital.
Dr Crossen receives support from the National Institute for Diabetes and Digestive and Kidney Diseases, National Institutes of Health, through grant number K23DK125671. Dr. Rosenthal receives support from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, through grant number K23HD101550. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
ORCID iDs: Sarah C. Haynes  https://orcid.org/0000-0001-5399-9725
https://orcid.org/0000-0001-5399-9725
Tejaswi Kompala  https://orcid.org/0000-0002-4492-5035
https://orcid.org/0000-0002-4492-5035
Aaron Neinstein  https://orcid.org/0000-0002-9774-7180
https://orcid.org/0000-0002-9774-7180
References
- 1.The Commonwealth Fund. The impact of the COVID-19 pandemic on outpatient care: visits return to prepandemic levels, but not for all providers and patients. Published October 15, 2020. Accessed November 23, 2020. https://www.commonwealthfund.org/publications/2020/oct/impact-covid-19-pandemic-outpatient-care-visits-return-prepandemic-levels.
- 2.Nouri S, Khoong EC, Lyles CR, Karliner L.Addressing equity in telemedicine for chronic disease management during the Covid-19 pandemic. NEJM Catalyst Innovations in Care Delivery. 2020;1(3). [Google Scholar]
- 3.Katzow MW, Steinway C, Jan S.Telemedicine and health disparities during COVID-19. Pediatrics. 2020;146(2):e20201586. [DOI] [PubMed] [Google Scholar]
- 4.Crossen S, Raymond J, Neinstein A.Top 10 tips for successfully implementing a diabetes telehealth program. Diabetes Technol Ther. 2020;22(12):920-928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pew Research Center. Mobile fact sheet. Published 2019. Updated June 12, 2019. Accessed October 9, 2020. https://www.pewresearch.org/internet/fact-sheet/mobile/.
- 6.Institute of Medicine Committee on Evaluating Clinical Applications of Telemedicine. Telemedicine: A Guide to Assessing Telecommunications in Health Care. Vol. 1, Introduction and Background. Washington, DC: National Academies Press; 1996. [PubMed] [Google Scholar]
- 7.Rametta SC, Fridinger SE, Gonzalez AK, et al. Analyzing 2,589 child neurology telehealth encounters necessitated by the COVID-19 pandemic. Neurology. 2020;95:e1257-e1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pierce RP, Stevermer JJ.Disparities in use of telehealth at the onset of the COVID-19 public health emergency. J Telemed Telecare. 2020:1357633X20963893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Health Resources & Services Administration. Federal office of rural health policy eligible ZIP codes. Published 2018. Updated December, 2018 Accessed June 15, 2020. https://www.hrsa.gov/rural-health/about-us/definition/datafiles.html.
- 10.Stata Statistical Software: Release 16 [computer program]. College Station, TX: StataCorp LLC; 2019. [Google Scholar]
- 11.American Diabetes Association. Comprehensive medical evaluation and assessment of comorbidities: standards of medical care in diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S37-S47. [DOI] [PubMed] [Google Scholar]
- 12.Weber E, Miller SJ, Astha V, Janevic T, Benn E.Characteristics of telehealth users in NYC for COVID-related care during the coronavirus pandemic. J Am Med Inform Assoc. 2020;27:1949-1954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Scott SN, Fontana FY, Züger T, Laimer M, Stettler C.Use and perception of telemedicine in people with type 1 diabetes during the COVID-19 pandemic—results of a global survey. Endocrinol Diabetes Metab. 2021;4:e00180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nouri SS, Avila-Garcia P, Cemballi AG, Sarkar U, Aguilera A, Lyles CR.Assessing mobile phone digital literacy and engagement in user-centered design in a diverse, safety-net population: mixed methods study. JMIR Mhealth Uhealth. 2019;7:e14250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khoong EC, Rivadeneira NA, Hiatt RA, Sarkar U.The use of technology for communicating with clinicians or seeking health information in a multilingual urban cohort: cross-sectional survey. J Med Internet Res. 2020;22:e16951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nesbitt TS, Dharmar M, Katz-Bell J, Hartvigsen G, Marcin JP.Telehealth at UC Davis–a 20-year experience. Telemed J E Health. 2013;19:357-362. [DOI] [PubMed] [Google Scholar]