People with type 2 diabetes mellitus (T2DM) face challenging self-management regimens to improve their glycemia, weight, and cholesterol and to decrease morbidity and mortality as well as high costs of care.1 Optimal diabetes management requires balancing HbA1c, frequency of hypoglycemia and reducing glucose variability (GV), which limits the ability of people with diabetes to reach HbA1c target goals without excessive hypoglycemia.2 Blood glucose and lifestyle digital monitoring with live coaching can provide real-time patient-centric support for people with T2DM.3,4 However, among many available diabetes apps, there is limited evidence that digital self-monitoring integrated with coaching can achieve clinical and self-reported outcomes.5 The purpose of our study was to investigate combined impact of a digital therapeutic platform and access to a live Certified Diabetes Care and Education Specialist (CDCES) on diabetes outcomes for individuals with T2DM, validating the platform-based data with clinical and self-reported measures. We hypothesized improvement in HbA1c, self-reported weight and glucose control satisfaction at 3-month follow-up. Further, reduction in platform-based GV would be associated with improvement in outcome measures.
In this study (ClinicalTrials.gov: NCT04057248), 12 participants (75% male; Age 55.4 ± 9.9) with baseline HbA1c >8.5% were provided with Dario digital therapeutic platform (connected blood glucose meter, test strips, mobile app and access to live CDCES). At both study enrollment and completion, participants completed blood testing and a satisfaction report. During 3-month intervention, participants tracked their blood glucose levels through the app and were routinely contacted by CDCES. Clinical outcomes and self-reported data before and after intervention were compared. Further, the time trajectory of the GV (users’ SDs) was evaluated. Critically, we tested the moderating effect of improvement in clinical and self-reported outcomes on platform-based GV trajectory. The statistical analysis was adjusted for the small sample size.
Wilcoxon signed-rank test with 10,000 Monte-Carlo simulations showed significant improvement in HbA1c (8.2 ± 1.4% vs 10.2 ± 1.6%, P < .001), FBG (171.1 ± 67.6 mg/dL vs 210.1 ± 82.6 mg/dL, P = .038), HDL (45.42 ± 12.92 vs. 42.37 ± 11.90, P = .029), BMI (32.23 ± 5.88 vs 35.78 ± 5.95, P = .024)) and self-reported evaluation in weight (2.92 ± 0.90 vs 2.42 ± 0.51, P = .034) and glucose control satisfaction (3.83 ± 1.03 vs 2.50 ± 0.67, P = .008) on 1 (very dissatisfied) − 5 (very satisfied). Single-case analysis with linear mixed model6 revealed a significant decrease in patients’ GV over the 3-month period (B = −1.00 [−1.87, −0.12], t = −2.42, Rsvg2 = 0.10, P = .027, Figure 1).
Figure 1.
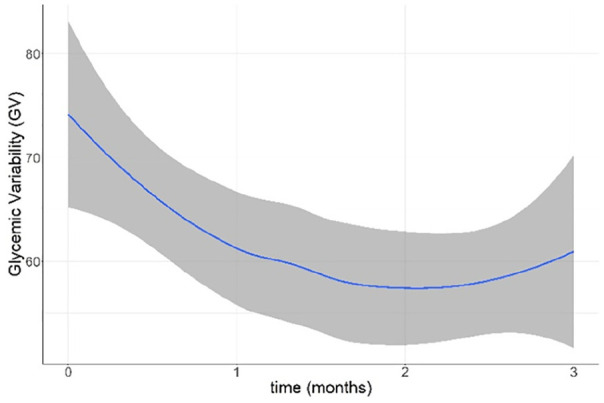
Locally weighted smoothed trajectory of the monthly average GV with 95% confidence intervals (the dark grey area surrounding the curve).
In addition, interaction analysis revealed a steeper GV reduction for participants who showed greater improvement in FBG (B = −2.32[−4.13, −0.52], t = −2.52, P = .013), BMI (B = −2.02[−4.01, −0.03], t = −1.99, P = .049), HDL (B = −2.00[−3.71, −0.28], t = −2.28, P = .025), self-reported weight (B = −2.14[−4.88, −0.41], t = −2.43, P = .017) and glucose control satisfaction (B = −2.17[−3.88, −0.46], t = −2.49, P = .014). Finally, weekly engagement with CDCES predicted reduction of participants’ GV during the following week (B = −5.56[−11.20, −0.35], t = −2.24, Rsvg2 = 0.07, P = .027).
Our findings suggest that a diabetes digital platform with real-time feedback and access to coaching improved diabetes outcome measures such as HbA1c with a reduction in GV. Importantly, we provide clinical validation for digital self-monitoring to deliver personalized care for patients with T2DM. Future research should replicate our findings using a larger sample.
Acknowledgments
None
Footnotes
Abbreviations: BMI, body mass index; CDCES, certified diabetes care and education specialist; FBG, fasting blood glucose; GV, glycemic variability; HDL, high-density lipoprotein; SD, standard deviation; T2DM, type 2 diabetes mellitus.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Yifat Fundoiano-Hershcovitz, Eitan Feniger and Sharon Dar are full time employees of Dario Health, Marilyn Ritholz is a member in Dario Health Scientific advisory board and Pavel Goldstein has received a consulting fee to assist with analyses but otherwise has no conflicts of interest.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded by Dario Health.
ORCID iD: Yifat Fundoiano-Hershcovitz  https://orcid.org/0000-0002-8526-0252
https://orcid.org/0000-0002-8526-0252
References
- 1.Amante DJ, Harlan DM, Lemon SC, et al. Evaluation of a diabetes remote monitoring program facilitated by connected glucose meters for patients with poorly controlled type 2 diabetes: randomized crossover trial. JMIR Diabetes. 2021;6:e25574. doi: 10.2196/25574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kovatchev B, Cobelli C.Glucose variability: timing, risk analysis, and relationship to hypoglycemia in diabetes. Diabetes Care. 2016;39:502-510. doi: 10.2337/dc15-2035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chrvala CA, Sherr D, Lipman RD.Diabetes self-management education for adults with type 2 diabetes mellitus: a systematic review of the effect on glycemic control. Patient Educ Couns. 2016;99:926-943. doi: 10.1016/j.pec.2015.11.003 [DOI] [PubMed] [Google Scholar]
- 4.Fundoiano-Hershcovitz Y, Hirsch A, Dar S, Feniger E, Goldstein P.Role of digital engagement in diabetes care beyond measurement: retrospective cohort study. JMIR Diabetes. 2021;6:e24030. doi: 10.2196/24030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kumar S, Moseson H, Uppal J, Juusola JL.A diabetes mobile app with in-app coaching from a Certified Diabetes Educator reduces A1C for individuals with type 2 diabetes. Diabetes Educ. 2018;44:226-236. doi: 10.1177/0145721718765650 [DOI] [PubMed] [Google Scholar]
- 6.Krasny-Pacini A, Evans J.Single-case experimental designs to assess intervention effectiveness in rehabilitation: a practical guide. Ann Phys Rehabil Med. 2018;61:164-179. doi: 10.1016/j.rehab.2017.12.002 [DOI] [PubMed] [Google Scholar]


