Abstract
Background
Nonalcoholic fatty liver disease (NAFLD) is becoming a global health problem. Bisphenol A (BPA), one of most widely used environmental chemicals, is suspected to be a contributor to the development NAFLD. This study was performed to examine the relationship between human BPA levels and risk of NAFLD.
Methods
The data (n = 3476 adults: 1474 men and 2002 women) used in this study were obtained from the Korean National Environmental Health Survey III (2015-2017). BPA levels were measured in urine samples. NAFLD was defined using hepatic steatosis index after exclusion of other causes of hepatic diseases.
Results
There was a significant linear relationship between the elevated urinary BPA concentrations and risk of NAFLD. In a univariate analysis, odds ratio (OR) of the highest quartile of urinary BPA level was 1.47 [95% confidence interval (CI) 1.11-1.94] compared to the lowest quartile. After adjusted with covariates, the ORs for NAFLD in the third and fourth quartiles were 1.31 [95% CI 1.03-1.67] and 1.32 [95% CI 1.03–1.70], respectively.
Conclusions
Urinary BPA levels are positively associated with the risk of NAFLD in adults. Further experimental studies are needed to understand the molecular mechanisms of BPA on NAFLD prevalence.
Keywords: Bisphenol A, Hepatic steatosis index, Nonalcoholic fatty liver disease, Korean adults, Korean national environmental health survey
Introduction
Nonalcoholic fatty liver (NAFLD) characterized by a fat accumulation of more than 5% in the liver without excessive alcohol use, viral hepatitis, and other liver diseases [1]. It encompassed a wide range of conditions from nonalcoholic fatty liver to more severe form, nonalcoholic steatohepatitis [2]. It is expected to be a primary cause of hepatocellular carcinoma and end-stage liver disease in the next few decades [3, 4]. The prevalence of NAFLD has been on the rise over recent decades and is estimated to be 25.24%, with 24.13% in the United States of America (USA) and 27.37% in Asia [5]. Although Western dietary consumption and inactive lifestyle contributed to the increasing rate of NAFLD [6], environmental chemicals which are frequently used in everyday material, can be the risk factor for NAFLD [7, 8].
Bisphenol A (BPA), one of the most widely used chemicals, consisted of two phenol rings attached by a methyl bridge, with two methyl groups [9]. It is utilized in the production of polycarbonate plastic and epoxy resin that are widely used in various applications including food packaging, beverage bottle, baby bottle, and paint [9, 10]. Because of the broad application, human can be exposed to BPA in their daily life and BPA is detected in over 90% of the humans [11, 12].
BPA is known to have estrogenic property by binding to the estrogenic receptors [9]. Many studies have reported the harmful health effects of BPA, including cancer, reproductive and development system, and neurological disorders [9, 13, 14]. Recently, epidemiological studies suggested the association between internal BPA levels and the risk of obesity and metabolic disorders, including insulin resistance, type 2 diabetes mellitus, and hyperlipidemia [15–17]. It might be due to the upregulation of lipogenic enzymes and transcription factors such as liver X receptor, the sterol regulatory element binding protein-1c, and the carbohydrate responsive element binding protein [18] and the elevation of oxidative stress [19]. BPA is associated with the weight gain, fat accumulation, and insulin resistance, thereby increasing the risk of NAFLD.
Previously, patients with histological diagnosis of NAFLD showed higher BPA levels in urine compared to the healthy subjects [7]. The positive association also showed between urinary BPA levels and NAFLD in USA population [20]. Nevertheless, the study from the USA included multiethnic populations; the majority of the race was non-Hispanic white [20]. Race/ethnicity and lifestyle could affect the NAFLD prevalence [1, 21]; however, the relationship between Asians and the risk of NAFLD prevalence has not been studied.
Therefore, this study was performed to evaluate the association between the urinary level of BPA and risk of NAFLD in Korean adults.
Materials and methods
Study population
This research data was taken from the Korean National Environmental Health Survey (KoNEHS) III (2015-2017). KoNEHS is conducted every 3 years from 2009 to understand the exposure levels of environmental chemicals, examine influential factors, and continuously investigate the factors of spatiotemporal distribution and changes in the Korean population. The third stage of KoNEHS was stratified into regional administrative and coastal regions and then classified based on the age, sex, and geographical regions socio-economic status. A total of 233 sampling units were randomly selected. After that, 15 households were selected using the systemic extraction method, and about 15 people were surveyed in each sample area [22].
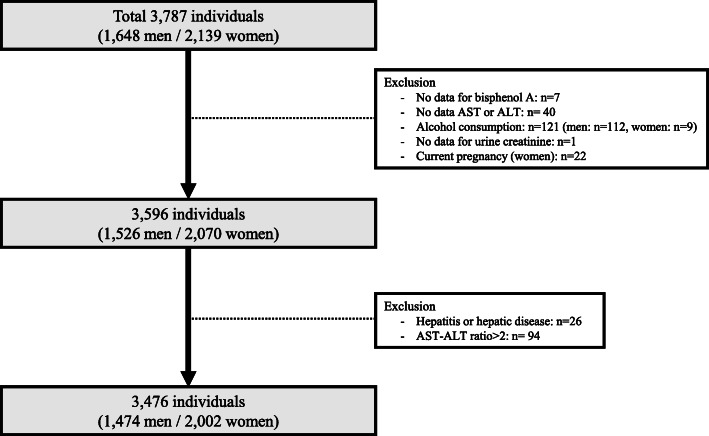
A total number of 3787 individuals (1648 men and 2139 women) with an age of ≥ 18 years underwent the questionnaires, anthropometric measurements, and collected urine and blood to analyze the levels of environmental chemicals. Three hundred eleven were excluded because of missing data for urinary BPA levels (n = 7), one of alanine aminotransferase (ALT) or aspartate aminotransferase (AST) levels (n = 40), and urine creatinine level (n = 1); those with significant alcohol consumption (n = 121; who consumed alcohol 3 times more than a week and 7-9 cups per time in men (n = 112) and who consumed alcohol 3 times more than a week and 5-6 cups per time in women (n = 19)); those with current pregnant women (n = 22); those with hepatitis or hepatic disease (n = 26); and those with AST/ALT ratio > 2 (n = 94). Finally, 3476 participants (1474 men and 2002 women) were included in this analysis (Fig. 1).
Fig. 1.
Study population in the present study obtained from the Korean National Environmental Health Survey III (2015-2017)
Data collection and diagnosis
Demographic and lifestyle characteristics, including age, sex, drinking and smoking status, physical activity, monthly household income, education level, marriage, and medication taking were surveyed through face-to-face interviews. Based on their response, some variables were categorized as follows: education (less than high school graduate, high school graduate, and college graduate or higher), smoking (never, former, and current), physical activity levels (no, moderate, and vigorous), monthly household income (< 2, 2-3, 3-5, and > 5 million Korean won), and marital status (single, married, and divorced/separated). Drinking status was reclassified as never, former, and current according to the questionnaires: did not drink at all (never), had a drinking experience but did not drink at all in the last year (former), and had a drinking experience and drink more than once a week (current).
Participants with diagnosis of hepatitis or hepatic steatosis and who were presently under treatment or taking drugs were regarded as one that has the hepatic disease. Hypertension was defined by self-reporting a history of hypertension or taking antihypertensive medications. Diabetes mellitus (DM) was defined by self-reporting a history of DM or taking anti-diabetic medications. Hyperlipidemia was defined as a self-reported history of hyperlipidemia, use of anti-hyperlipidemic medication, high-density lipoprotein cholesterol ≤ 40 mg/dL, and triglyceride (TG) ≥ 240. Body mass index (BMI) was calculated as the body weight (kg) divided by height squared (m2).
Urinary bisphenol A concentrations
Spot urine samples were collected from participants and stored at 0-4 °C immediately, and subsequently frozen at −20 °C according to the guideline of National Institute of Environmental Research [23]. Urinary BPA were measured using ultra-performance liquid chromatography-mass spectrometry (Xevo TQ-S, Waters, Milford, MA, USA) [24]. Values below the detection limit were divided by the square root of 2.
Laboratory evaluations
Blood samples were collected from participants at the same time with the urine samples. The samples were centrifuged at 3500 rpm to separate the serum, and stored at 0-4 °C. The separated serum was aliquoted and frozen at −20 °C according to the guideline of National Institute of Environmental Research [23]. AST, ALT, and gamma-glutamyl transpeptidase (γ-GTP) were measured in serum samples [25]. The reference values were AST < 34U/L., ALT 10 - 49U/L, and γ-GTP < 73 U/L for men and γ-GTP < 38 U/L for women.
NAFLD evaluations
The hepatic steatosis index (HSI) is an efficient non-invasive biomarker for NAFLD [26]. The variables in the HSI formula were levels of ALT, AST, BMI, sex, and presence of DM. Subjects were categorized into NAFLD and non-NAFLD using the published cut-off value of 36.
Since elevated AST, ALT, and γ-GTP were also used for NAFLD assessment [27–29], we defined abnormal AST, ALT, and γ-GTP based on the reference value.
Statistical analysis
The average and standard error (continuous variables), and frequency (categorical variables) were provided in non-NAFLD and NAFLD based on the hepatic steatosis index score. Sample weights were included in order to reconstruct the data at the level of the entire population of Korea. The log transformation was performed because the distribution of urinary BPA concentrations was skewed to the right. BPA concentrations were categorized into quartiles based on the weighted sample distribution. The weighted mean (continuous variables) and weighted frequencies (categorical variables) in general characteristics were described by the BPA quartiles. The general characteristics were compared using the t test and an analysis of variance (continuous variable) or χ2 test (categorical variables).
A multivariate logistic regression analysis was performed to evaluate the relationship between urinary BPA levels and NAFLD. Covariates of age, sex, drinking, smoking, physical activity, monthly household income, education, marriage, and urine creatinine were included in the regression model. Because BMI is used in the HSI formula, it is not included in multivariate analysis as an independent variable to avoid collinearity. In this formula, 2 points was added in female to adjust the lower BMI in women compared to men. Also, because DM was an independent risk factor of NAFLD, 2 point was added in the subject with DM [26]. Thus, sex and DM were used as independent variables in multivariate analysis. Data analyses were performed using STATA (version 16.0 StataCorp LP College Station, TX, USA). P values < 0.05 were considered significant.
Results
General characteristics of study population
The general characteristic of samples was shown in Tables 1 and 2. Respondents were divided into two categories, non-NAFLD and NAFLD, based on the HSI (Table 1). Of 3476 participants, 2561 (73.68%) had HSI value under 36, and 915 (26.32%) had HSI value over 36 or higher. The mean age was 52.67 years old in non-NAFLD and 53.78 years old in NAFLD. Drinking status, physical activity, monthly income, education, and marital status was significantly different between non-NAFLD and NAFLD group (p = 0.018, p = 0.005, p = 0.037, p < 0.001, and p = 0.043, respectively). Participants in the NAFLD group had significantly higher levels in AST, ALT, γ-GTP, and BMI (all p < 0.001).
Table 1.
General characteristics of study participants according to hepatic steatosis index score
| Total (n = 3476) | non-NAFLD (n = 2561) | NAFLD (n = 915) | p value | |
|---|---|---|---|---|
| Age, year | 52.96 ± 0.25 | 52.67 ± 0.29 | 53.78 ± 0.46 | 0.090 |
| Gender (%, men) | 1474 (42.41) | 1070 (41.78) | 404 (44.15) | 0.213 |
| BMI, kg/m2 | 24.61 ± 0.05 | 23.23 ± 0.04 | 28.47±0.10 | < 0.001 |
| Drinking status, n (%) | 0.018 | |||
| Never | 715 (20.57) | 502 (19.60) | 213 (23.28) | |
| Former | 439 (12.63) | 314 (12.26) | 125 (13.66) | |
| Current | 2322 (66.80) | 1745 (68.14) | 577 (63.06) | |
| Smoking status, n (%) | 0.727 | |||
| Never | 2278 (65.54) | 1667 (65.48) | 602 (65.68) | |
| Former | 679 (19.53) | 507 (19.80) | 172 (18.80) | |
| Current | 519 (14.93) | 377 (14.72) | 142 (15.52) | |
| Physical activity, n (%) | 0.005 | |||
| No | 1888 (54.32) | 1350 (52.71) | 538 (58.80) | |
| Moderate | 274 (7.88) | 205 (8.00) | 69 (7.54) | |
| Vigorous | 1314 (37.80) | 1006 (39.28) | 308 (33.66) | |
| Monthly household income, n (%) | 0.037 | |||
| < 2 million Korean Won | 1308 (37.63) | 944 (36.86) | 364 (39.78) | |
| 2-3 million Korean Won | 733 (21.09) | 523 (20.42) | 210 (22.95) | |
| 3-5 million Korean Won | 873 (25.12) | 662 (25.93) | 209 (22.84) | |
| > 5 million Korean Won | 562 (16.17) | 430 (16.79) | 132 (14.43) | |
| Education, n (%) | < 0.001 | |||
| < High school | 1172 (33.72) | 800 (31.24) | 372 (40.66) | |
| High school | 1220 (35.10) | 941 (36.74) | 279 (30.49) | |
| College or higher | 10.84 (31.19) | 820 (32.02) | 264 (28.85) | |
| Marital status, n (%) | 0.043 | |||
| Single | 397 (11.42) | 310 (12.10) | 87 (9.51) | |
| Married | 2681 (77.13) | 1971 (76.96) | 710 (77.60) | |
| Divorced or separated | 398 (11.45) | 280 (10.93) | 118 (12.90) | |
| AST | 25.97 ± 0.17 | 24.95 ± 0.18 | 28.84 ± 0.41 | < 0.001 |
| ALT | 24.86 ± 0.26 | 20.82 ± 0.18 | 36.17 ± 0.74 | < 0.001 |
| γ-GTP | 29.78 ± 0.57 | 26.00 ± 0.61 | 40.36 ± 1.29 | < 0.001 |
| Comorbidity, n (%) | ||||
| Hypertension | 798 (22.96) | 474 (18.51) | 324 (35.41) | < 0.001 |
| Diabetes mellitus | 309 (8.89) | 146 (5.70) | 163 (17.81) | < 0.001 |
| Hyperlipidemia | 1211 (34.84) | 734 (28.66) | 477 (52.13) | < 0.001 |
NAFLD nonalcoholic fatty liver disease, BMI body mass index, AST aspartate aminotransferase, ALT alanine aminotransferase, γ-GTP gamma-glutamyl transpeptidase
Table 2.
General characteristics of study participants according to urinary bisphenol A concentrations
| Quartile 1 (n = 888) | Quartile 2 (n = 880) | Quartile 3 (n = 860) | Quartile 4 (n = 848) | P value | |
|---|---|---|---|---|---|
| Age (year) | 47.60 ± 0.96 | 47.23 ± 0.93 | 47.08 ± 0.88 | 45.82 ± 0.74 | 0.135 |
| Gender (%, men) | 43.98 ± 1.87 | 45.03 ± 1.83 | 50.84 ± 2.24 | 56.02 ± 1.91 | < 0.001 |
| BMI (kg/m2) | 23.87 ± 0.14 | 24.17 ± 0.16 | 24.61 ± 0.19 | 24.73 ± 0.17 | < 0.001 |
| Drinking status (%) | 0.056 | ||||
| Never | 17.13 ± 1.80 | 17.37 ± 1.73 | 14.72 ± 1.51 | 13.71 ± 1.46 | |
| Former | 11.64 ± 1.34 | 12.83 ± 1.59 | 10.27 ± 1.59 | 10.91 ± 1.38 | |
| Current | 71.21 ± 2.08 | 69.77 ± 2.11 | 75.00 ± 1.95 | 75.37 ± 1.98 | |
| Smoking status (%) | < 0.001 | ||||
| Never | 70.06 ± 1.71 | 65.52 ± 1.91 | 59.79 ± 2.53 | 58.71 ± 2.42 | |
| Former | 16.16 ± 1.51 | 18.49 ± 1.67 | 20.25 ± 1.80 | 18.24 ± 1.83 | |
| Current | 13.77 ± 1.76 | 15.97 ± 2.09 | 20.24 ± 1.82 | 23.03 ± 2.10 | |
| Physical activity (%) | 0.099 | ||||
| No | 52.75 ± 2.34 | 54.60 ± 2.46 | 54.01 ± 2.34 | 60.38 ± 2.05 | |
| Moderate | 9.68 ± 1.42 | 6.44 ± 1.07 | 7.71 ± 1.19 | 5.79 ± 0.96 | |
| Vigorous | 37.56 ± 2.61 | 38.95 ± 2.42 | 38.27 ± 2.16 | 33.82 ± 2.15 | |
| Monthly household income (%) | 0.943 | ||||
| < 2 million Korean Won | 28.53 ± 2.63 | 27.09 ± 2.42 | 25.90 ± 1.89 | 28.94 ± 2.66 | |
| 2-3 million Korean Won | 19.55 ± 2.32 | 25.18 ± 2.14 | 22.59 ± 2.14 | 20.34 ± 1.97 | |
| 3-5 million Korean Won | 30.38 ± 2.72 | 25.97 ± 2.53 | 30.14 ± 2.19 | 29.79 ± 2.72 | |
| > 5 million Korean Won | 21.52 ± 2.64 | 21.75 ± 2.34 | 21.35 ± 2.33 | 20.91 ± 2.14 | |
| Education (%) | 0.996 | ||||
| < High school | 22.41 ± 2.26 | 20.30 ± 1.90 | 21.73 ± 1.92 | 20.25 ± 1.82 | |
| High school | 35.01 ± 2.13 | 38.62 ± 2.07 | 38.93 ± 2.64 | 38.25 ± 2.32 | |
| College and more | 42.56 ± 2.71 | 41.07 ± 2.21 | 39.33 ± 2.66 | 41.49 ± 2.53 | |
| Marital status (%) | 0.797 | ||||
| Single | 21.02 ± 2.29 | 21.65 ± 2.18 | 20.27 ± 2.25 | 22.42 ± 2.14 | |
| Married | 71.13 ± 2.35 | 69.49 ± 2.39 | 71.26 ± 2.33 | 69.69 ± 2.23 | |
| Divorced or separated | 7.84 ± 1.16 | 8.85 ± 1.26 | 8.45 ± 1.32 | 7.87 ± 1.13 | |
| AST | 25.57 ± 0.35 | 24.79 ± 0.32 | 25.90 ± 0.82 | 25.42 ± 0.45 | 0.048 |
| ALT | 24.70 ± 0.62 | 24.09 ± 0.67 | 25.91 ± 1.19 | 26.26 ± 0.72 | 0.729 |
| γ-GTP | 28.18 ± 1.25 | 28.49 ± 1.25 | 32.20 ± 1.88 | 32.57 ± 1.87 | 0.015 |
| Comorbidity (%) | |||||
| Hypertension | 16.78 ± 1.21 | 17.06 ± 1.62 | 17.29 ± 1.40 | 14.40 ± 1.54 | 0.257 |
| Diabetes mellitus | 6.44 ± 0.98 | 4.65 ± 0.63 | 6.02 ± 1.13 | 7.39 ± 1.10 | 0.359 |
| Hyperlipidemia | 27.92 ± 2.11 | 30.54 ± 2.00 | 31.41 ± 2.56 | 34.44 ± 2.12 | 0.025 |
BMI body mass index, AST aspartate aminotransferase, ALT alanine aminotransferase, γ-GTP, gamma-glutamyl transpeptidase. Data were shown as the weighted mean or frequency ± standard errors as appropriated
Table 2 indicated the general characteristics of study participants according to urinary BPA concentration. BPA concentrations were log-transformed because of the skewness. The transformed BPA level was classified into quartiles based on the weighted sample distribution. The range of BPA concentration (μg/L) is shown as follows: min-0.50 in the first quartile, 0.50-1.26 in the second quartile, 1.26-2.67 in the third quartile, and 2.67-max in the fourth quartile. Gender, BMI, smoking status, AST, γ-GTP, and hyperlipidemia were found to be statistically significant among the levels of BPA (p < 0.001, p < 0.001, p < 0.001, p = 0.048, p = 0.015, and p = 0.025, respectively).
Distribution of urinary BPA concentrations
The urinary BPA levels were shown in Table 3 between the non-NAFLD group and NAFLD group. The geometric mean (GM) concentration of BPA in NAFLD group (2.56 μg/L) was significantly higher than in non-NAFLD group (2.24 μg/L) (p = 0.001). The 25th, 50th, and 75th levels of urinary BPA were 0.48 μg/L, 1.21 μg/L, and 2.56 μg/L in non-NAFLD group, and 0.57 μg/L, 1.52 μg/L, and 2.96 μg/L in NAFLD group.
Table 3.
Distributions of urinary bisphenol A levels (BPA, μg/L) in the study population
| BPA conc. (μg/L) | Total | non-NAFLD | NAFLD | P value |
|---|---|---|---|---|
| GM (GSE) | 2.32 (0.07) | 2.24 (0.08) | 2.56 (0.15) | 0.001 |
| Percentile | ||||
| Min | 0.05 | 0.05 | 0.05 | |
| 25th | 0.5 | 0.48 | 0.57 | |
| 50th | 1.26 | 1.21 | 1.52 | |
| 75th | 2.66 | 2.56 | 2.96 | |
| Max | 111.31 | 111.31 | 86.78 |
NAFLD nonalcoholic fatty liver disease, GM geometric mean, GSE geometric standard error
Prevalence of NAFLD and abnormal ALT, AST, and γ-GTP according to urinary BPA levels
The number of NAFLD based on HSI, and abnormal ALT, AST, and γ-GTP were presented in Table 4. The prevalence of NAFLD based on HSI and abnormal ALT were increased in accordance with the increase of urinary BPA concentrations (p = 0.002 and p = 0.023, respectively). However, there were no significant relationships between the number of abnormal AST and γ-GTP with urinary BPA levels.
Table 4.
Prevalence of NAFLD and abnormal ALT, AST, and γ-GTP activities according to urinary bisphenol A levels
| Quartile 1 (n = 888) | Quartile 2 (n = 880) | Quartile 3 (n = 860) | Quartile 4 (n = 848) | P value | ||
|---|---|---|---|---|---|---|
| NAFLD | Actual number | 201 | 214 | 242 | 258 | 0.002 |
| Weighted frequency (95% CI) | 21.83 (18.42-25.68) | 22.14 (18.88-25.78) | 25.55 (21.64-29.90) | 29.18 (25.48-33.19) | ||
| Abnormal ALT | Actual number | 83 | 88 | 87 | 102 | 0.023 |
| Weighted frequency (95% CI) | 10.41 (8.22-13.11) | 12.27 (9.36-15.93) | 11.25 (8.80-14.27) | 15.34 (12.53-18.66) | ||
| Abnormal AST | Actual number | 110 | 82 | 91 | 10 | 0.872 |
| Weighted frequency (95% CI) | 12.24 (9.62-15.45) | 7.59 (5.67-10.09) | 9.99 (8.03-12.35) | 11.77 (9.45-14.58) | ||
| Abnormal γ-GTP | Actual number | 104 | 89 | 99 | 95 | 0.844 |
| Weighted frequency (95% CI) | 10.86 (8.54-13.72) | 9.29 (6.97-12.29) | 12.05 (9.42-15.29) | 10.31 (8.06-13.09) | ||
NAFLD nonalcoholic fatty liver disease, AST aspartate aminotransferase, ALT alanine aminotransferase, γ-GTP gamma-glutamyl transpeptidase
The association between urinary BPA concentrations and NAFLD prevalence
Odds ratio (OR) and 95% CI for NAFLD based on HSI according to BPA levels were presented in Table 5. A logistic regression was conducted based on the BPA quartile, using the first quantile as the reference group.
Table 5.
Multivariate analysis for NAFLD according to urinary bisphenol A levels
| Crude | Model 1 | Model 2 | Model 3 | |||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | |
| Quartile 1 | 1 | 0.002* | 1 | 0.035* | 1 | 0.003* | 1 | 0.010* |
| Quartile 2 | 1.01 (0.74-1.39) | 0.913 | 1.00 (0.73-1.37) | 0.955 | 1.09 (0.87-1.36) | 0.435 | 1.08 (0.85-1.36) | 0.510 |
| Quartile 3 | 1.22 (0.89-1.68) | 0.203 | 1.16 (0.84-1.58) | 0.346 | 1.28 (1.02-1.60) | 0.032 | 1.31 (1.03-1.67) | 0.025 |
| Quartile 4 | 1.47 (1.11-1.94) | 0.006 | 1.31 (0.99-1.75) | 0.058 | 1.37 (1.08-1.73) | 0.007 | 1.32 (1.03-1.70) | 0.026 |
NAFLD nonalcoholic fatty liver disease, OR odds ratio, CI confidence interval
*p values were shown the test of trend of odds
Crude: Hepatic steatosis index, bisphenol A
Model 1: Crude + age, gender, creatinine
Model 2: Model 1 + smoking, drinking, exercise, marital status, education, income
Model 3: Model 2 + hypertension, diabetes mellitus, hyperlipidemia
In a crude model, the fourth quartile showed a significantly higher OR of HSI (1.47 [95% CI 1.11-1.94]). When adjusting age, gender and urine creatinine (model 1), OR in the fourth quartile was 1.31 (95% CI 0.99-1.75). Hence, there was no significant association.
With an additional adjustment of the socio-economic values (model 2), the third and fourth quartiles showed higher ORs of NAFLD by HSI compared to the first quartile (1.28 [95% CI 1.02-1.60] and 1.37 [95% CI 1.08-1.73], respectively).
Further adjusting comorbidities such as hypertension, DM, and hyperlipidemia (model 3), ORs in the third and fourth quartiles were higher than in reference group (1.31 [95% CI 1.03-1.67] and 1.32 [95% CI 1.03-1.70] respectively).
Results of trend tests for the correlation between NAFLD and BPA were p < 0.05 regardless of adjustments (crude, model 1, model 2, and model 3).
Discussion
This study was conducted to evaluate the association between urinary BPA level and NAFLD base on HSI score in the Korean population. The higher risk of NAFLD according to HSI was significantly associated with higher urinary BPA concentration. Exposure of BPA presented by urine BPA level linearly correlated with NAFLD occurrence in both unadjusted and adjusted models.
BPA is widely used in the synthesis of consumer products, including food and beverage containers, baby bottle, and dental sealants [9, 10]. Human are exposed to BPA through oral administration, inhalation and dermal absorption [30]. Once BPA enters to body, it binds to glucuronic acid and converts to BPA glucuronide in the liver and gut [9], and the BPA glucuronides are primarily excreted through urine [31]. Although some prospective studies used in both urine and blood samples to measure BPA levels [7, 32], urine samples were used to demonstrate the BPA exposure in population based studies because of the relatively ease to collect the biological samples compared to the blood.
BPA has been suggested that the positive relationship with obesity and metabolic disease in healthy adults [15, 16, 33]. Obesity is well-known factor in liver abnormalities, including NAFLD [34] that is characterized by an increase of hepatic TG content with or without inflammation and fibrosis [1, 2]. Recent epidemiologic studies have showed an association between urinary BPA levels and the risk of NAFLD [7, 20]. It seems that BPA could promote lipid accumulation in the liver as well as obesity.
Experimental studies have suggested the underlying mechanism for the hepatic lipid accumulation due to BPA exposure. BPA-treated mice showed the increase of lipid accumulation in the liver through the activation of lipogenic enzymes, including acetyl-CoA carboxylase, fatty acid synthase, stearoyl-CoA desaturase-1, and sterol regulatory element binding factor 1 [18, 35]. In addition, the elevation of inflammation might be closely associated with the appearance and progression of liver disease [7, 19, 36]. Thus, BPA could induce hepatic steatosis through modulated by de novo lipogenesis and inflammation.
Previously, BPA levels in urine and blood in NAFLD patients was significantly higher than healthy subjects [7]. In US population based study, the positive association also showed between urinary BPA concentrations and the prevalence of NAFLD [20]. Similar with the previous studies, higher levels of urinary BPA were associated with NAFLD prevalence in Korean adults. Although BPA is metabolized and excreted over 90% within 24 h after administration [37], most people can be exposed to BPA through their life. In addition, internal BPA levels can vary depending on the lifestyle, diet, and living environment [38]. Thus, further study is needed on whether the reduction of BPA exposure can decrease the incidence of NAFLD.
In addition, the prevalence of abnormal ALT was increased according to increase of BPA levels, but not in AST and γ-GTP. Similar with our result, serum ALT levels was relatively higher in NAFLD patients than healthy people [28, 39]. Because the increase of hepatic lipid accumulation can induce the toxic effects on hepatocytes [40], NAFLD may induce the elevation of liver enzymes, including ALT, AST, and GGT. It seems that exposure to BPA might increase the risk of liver damages.
To the best of our knowledge, this is the first study to establish the association between urinary BPA level and NAFLD prevalence in the Korean population. In addition, because study was performed from the data that can represent the national population, these results could generalize to the population. However, there remains some limitation. First, HSI score is used to define NAFLD. Liver biopsy and abdominal ultrasound might be more appropriate to find liver steatosis. However, those are not feasible in population based large-scale study because of the invasiveness and cost issue. HSI is a noninvasive tool to predict the presence of NAFLD using anthropometric and laboratory parameters, including BMI, AST, and ALT [26]. HSI score with < 36 or > 36 had 93.1% sensitivity to rule-out the absence of NAFLD and 92.4% specificity to detect the presence of NAFLD. Nevertheless, there is still a problem with classification errors, because 30 ≤ HSI ≤ 36 was considered as the non-NAFLD group. However, it is inevitable to statistical analysis. Second, the amount of alcohol consumption (g/day) could not estimate because KoNEHS offered the drinking times in the last month and the number of glass per times. In this study, men who consumed alcohol 3 times more than a week and 7-9 glasses per time, and women who consumed alcohol 3 times more than a week and 5-6 glasses per time were defined as heavy drinker by referring to previous study [41]. Third, it could not evaluate the causal relationship between urinary BPA level and NAFLD because of a cross-sectional analysis. Additional studies are needed to determine the contribution of BPA on NAFLD prevalence. Fourth, BPA levels were measured using spot urine samples. After administration, most of BPA is eliminated within 24 h via urine [37]; thus, temporal variation of BPA levels in subjects can be raised. Nevertheless, KoNEHS randomly collected the spot urine sample from a large population according to the survey guideline [23]. It may reflect the average BPA levels in population.
In conclusion, the result of this study based on a representative Korean population indicated that there is positive association between urine BPA concentration reflecting BPA exposure and risk of increasing NAFLD. As BPA has been observed to be associated with an increased prevalence of NAFLD, it would be desirable to reduce BPA exposure.
Acknowledgements
This study used data from the Korean National Environmental Health Survey (KoNEHS) Cycle 3 which was conducted by Ministry of Environment, National Institute of Environmental Research.
Authors’ contributions
Conceptualization, Y.Y.J.; Methodology, A.S.J. and O.S.; Software, Y.Y.J.; Formal analysis, O.S., P.K.J., K.T.H., and Y.Y.J.; Writing—original draft preparation, A.S.J. and Y.E.J.; Writing—review and editing, H.Y.P. and Y.Y.J. The authors read and approved the final manuscript.
Funding
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-2021R1I1A3046386).
Availability of data and materials
Our investigation was based on KoNEHS cycle 3 (2015–2017), which was approved by the institutional review board of the National Institute of Environmental Research in Korea (NIER-2016-BR-003-01, NIER-2016-BR-003-03). All participants provided written informed consent. The data presented in this study are available on request from the corresponding author. In this case, the researcher receives data that does not include identifiable IDs and/or regional code variables in combination with personal information and other data.
Declarations
Ethics approval and consent to participate
Ethical review and approval were waived for this study, due to use existing information/data, documents, and records.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sang Joon An and Eun-Jung Yang contributed equally to this work.
Contributor Information
Sang Joon An, Email: neuroan@cku.ac.kr.
Eun-Jung Yang, Email: enyang7@yuhs.ac.
Subin Oh, Email: rosette731@gmail.com.
Kyong Jin Park, Email: kyongjin99@gmail.com.
Taehyen Kim, Email: starkim3@naver.com.
Yeon-pyo Hong, Email: hyp026@cau.ac.kr.
Yun-Jung Yang, Email: yangyj@ish.ac.kr.
References
- 1.Perumpail BJ, Khan MA, Yoo ER, Cholankeril G, Kim D, Ahmed A. Clinical epidemiology and disease burden of nonalcoholic fatty liver disease. World J Gastroenterol. 2017;23(47):8263–8276. doi: 10.3748/wjg.v23.i47.8263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002;346(16):1221–1231. doi: 10.1056/NEJMra011775. [DOI] [PubMed] [Google Scholar]
- 3.Thandra KC, Barsouk A, Saginala K, Aluru JS, Rawla P, Barsouk A. Epidemiology of non-alcoholic fatty liver disease and risk of hepatocellular carcinoma progression. Clin Exp Hepatol. 2020;6(4):289–294. doi: 10.5114/ceh.2020.102153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anstee QM, Marietti M, Hardy T, Henry L, Eslam Met al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol 2018;15(1):11-20. doi:10.1038/nrgastro.2017.109. [DOI] [PubMed]
- 5.Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 6.Fan JG, Kim SU, Wong VW. New trends on obesity and NAFLD in Asia. J Hepatol. 2017;67(4):862–873. doi: 10.1016/j.jhep.2017.06.003. [DOI] [PubMed] [Google Scholar]
- 7.Dallio M, Masarone M, Errico S, Gravina AG, Nicolucci C, Di Sarno R, et al. Role of bisphenol A as environmental factor in the promotion of non-alcoholic fatty liver disease: in vitro and clinical study. Aliment Pharmacol Ther. 2018;47(6):826–837. doi: 10.1111/apt.14499. [DOI] [PubMed] [Google Scholar]
- 8.Foulds CE, Trevino LS, York B, Walker CL. Endocrine-disrupting chemicals and fatty liver disease. Nat Rev Endocrinol. 2017;13(8):445–457. doi: 10.1038/nrendo.2017.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.NTP. National Toxicology Program . NTP-CERHR monograph on the potential human reproductive and developmental effects of bisphenol A. 2008. pp. 1–64. [PubMed] [Google Scholar]
- 10.Corrales J, Kristofco LA, Steele WB, Yates BS, Breed CS, Williams ES, et al. Global assessment of bisphenol A in the environment: review and analysis of its occurrence and bioaccumulation. Dose-Response. 2015;13(3):1559325815598308. doi: 10.1177/1559325815598308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Calafat AM, Kuklenyik Z, Reidy JA, Caudill SP, Ekong J, Needham LL. Urinary concentrations of bisphenol A and 4-nonylphenol in a human reference population. Environ Health Perspect. 2005;113(4):391–395. doi: 10.1289/ehp.7534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim K, Park H, Yang W, Lee JH. Urinary concentrations of bisphenol A and triclosan and associations with demographic factors in the Korean population. Environ Res. 2011;111(8):1280–1285. doi: 10.1016/j.envres.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 13.Itoh K, Yaoi T, Fushiki S. Bisphenol A, an endocrine-disrupting chemical, and brain development. Neuropathology. 2012;32(4):447–457. doi: 10.1111/j.1440-1789.2011.01287.x. [DOI] [PubMed] [Google Scholar]
- 14.Kabir ER, Rahman MS, Rahman I. A review on endocrine disruptors and their possible impacts on human health. Environ Toxicol Pharmacol. 2015;40(1):241–258. doi: 10.1016/j.etap.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 15.Lee I, Park YJ, Kim MJ, Kim S, Choi S, Park J, et al. Associations of urinary concentrations of phthalate metabolites, bisphenol A, and parabens with obesity and diabetes mellitus in a Korean adult population: Korean National Environmental Health Survey (KoNEHS) 2015-2017. Environ Int. 2021;146:106227. doi: 10.1016/j.envint.2020.106227. [DOI] [PubMed] [Google Scholar]
- 16.Wang T, Li M, Chen B, Xu M, Xu Y, Huang Y, et al. Urinary bisphenol A (BPA) concentration associates with obesity and insulin resistance. J Clin Endocrinol Metab. 2012;97(2):E223–E227. doi: 10.1210/jc.2011-1989. [DOI] [PubMed] [Google Scholar]
- 17.Stahlhut RW, Myers JP, Taylor JA, Nadal A, Dyer JA, Vom Saal FS. Experimental BPA exposure and glucose-stimulated insulin response in adult men and women. J Endocr Soc. 2018;2(10):1173–1187. doi: 10.1210/js.2018-00151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marmugi A, Ducheix S, Lasserre F, Polizzi A, Paris A, Priymenko N, et al. Low doses of bisphenol A induce gene expression related to lipid synthesis and trigger triglyceride accumulation in adult mouse liver. Hepatology. 2012;55(2):395–407. doi: 10.1002/hep.24685. [DOI] [PubMed] [Google Scholar]
- 19.Huc L, Lemarie A, Gueraud F, Helies-Toussaint C. Low concentrations of bisphenol A induce lipid accumulation mediated by the production of reactive oxygen species in the mitochondria of HepG2 cells. Toxicol in Vitro. 2012;26(5):709–717. doi: 10.1016/j.tiv.2012.03.017. [DOI] [PubMed] [Google Scholar]
- 20.Kim D, Yoo ER, Li AA, Cholankeril G, Tighe SP, Kim W, et al. Elevated urinary bisphenol A levels are associated with non-alcoholic fatty liver disease among adults in the United States. Liver Int. 2019;39(7):1335–1342. doi: 10.1111/liv.14110. [DOI] [PubMed] [Google Scholar]
- 21.Mitra S, De A, Chowdhury A. Epidemiology of non-alcoholic and alcoholic fatty liver diseases. Transl Gastroenterol Hepatol. 2020;5:16. doi: 10.21037/tgh.2019.09.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Korean National Institute of environmental research . Guidelines for using raw materials for Korean National Environmental Health Survey - the second stage ('15-'17) Incheon: Korean National Institute Of Environmental Research; 2019. [Google Scholar]
- 23.Korean national Institute of Environmental Research . 3rd basic National Environmental Health Survey Guideline for Management of Biological Samples (revised) 2019. [Google Scholar]
- 24.Korean National Institute of Environmental Research. Analysis manual of environmental hazardous substances in biological samples (organic compounds). Guidelines for using raw materials for Korean National Environmental Health Survey - the third stage ('15-'17). Incheon: Korean National Institute Of Environmental Research; 2018.
- 25.Korean national Institute of Environmental Research . 3rd National Environmental Health Basic Survey Clinical Test Manual. 2019. [Google Scholar]
- 26.Lee JH, Kim D, Kim HJ, Lee CH, Yang JI, Kim W, et al. Hepatic steatosis index: a simple screening tool reflecting nonalcoholic fatty liver disease. Dig Liver Dis. 2010;42(7):503–508. doi: 10.1016/j.dld.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 27.Mandal A, Bhattarai B, Kafle P, Khalid M, Jonnadula SK, Lamicchane J, et al. Elevated liver enzymes in patients with type 2 diabetes mellitus and non-alcoholic fatty liver disease. Cureus. 2018;10:e3626. doi: 10.7759/cureus.3626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Martin-Rodriguez JL, Gonzalez-Cantero J, Gonzalez-Cantero A, Arrebola JP, Gonzalez-Calvin JL. Diagnostic accuracy of serum alanine aminotransferase as biomarker for nonalcoholic fatty liver disease and insulin resistance in healthy subjects, using 3T MR spectroscopy. Medicine (Baltimore) 2017;96:e6770. doi: 10.1097/MD.0000000000006770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sueyoshi S, Sawai S, Satoh M, Seimiya M, Sogawa K, Fukumura A, et al. Fractionation of gamma-glutamyltransferase in patients with nonalcoholic fatty liver disease and alcoholic liver disease. World J Hepatol. 2016;8(36):1610–1616. doi: 10.4254/wjh.v8.i36.1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ma Y, Liu H, Wu J, Yuan L, Wang Y, Du X, et al. The adverse health effects of bisphenol A and related toxicity mechanisms. Environ Res. 2019;176:108575. doi: 10.1016/j.envres.2019.108575. [DOI] [PubMed] [Google Scholar]
- 31.Volkel W, Bittner N, Dekant W. Quantitation of bisphenol A and bisphenol A glucuronide in biological samples by high performance liquid chromatography-tandem mass spectrometry. Drug Metab Dispos. 2005;33(11):1748–1757. doi: 10.1124/dmd.105.005454. [DOI] [PubMed] [Google Scholar]
- 32.Federico A, Dallio M, Gravina AG, Diano N, Errico S, Masarone M, et al. The bisphenol A induced oxidative stress in non-alcoholic fatty liver disease male patients: a clinical strategy to antagonize the progression of the disease. Int J Environ Res Public Health. 2020;17(10). 10.3390/ijerph17103369. [DOI] [PMC free article] [PubMed]
- 33.Hong SH, Sung YA, Hong YS, Ha E, Jeong K, Chung H, et al. Urinary bisphenol A is associated with insulin resistance and obesity in reproductive-aged women. Clin Endocrinol. 2017;86:506–512. doi: 10.1111/cen.13270. [DOI] [PubMed] [Google Scholar]
- 34.Sarwar R, Pierce N, Koppe S. Obesity and nonalcoholic fatty liver disease: current perspectives. Diabetes Metab Syndr Obes. 2018;11:533–542. doi: 10.2147/DMSO.S146339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Figueiredo LS, Oliveira KM, Freitas IN, Silva JA, Jr, Silva JN, Favero-Santos BC, et al. Bisphenol-a exposure worsens hepatic steatosis in ovariectomized mice fed on a high-fat diet: role of endoplasmic reticulum stress and fibrogenic pathways. Life Sci. 2020;256:118012. doi: 10.1016/j.lfs.2020.118012. [DOI] [PubMed] [Google Scholar]
- 36.Bindhumol V, Chitra KC, Mathur PP. Bisphenol A induces reactive oxygen species generation in the liver of male rats. Toxicology. 2003;188(2-3):117–124. doi: 10.1016/s0300-483x(03)00056-8. [DOI] [PubMed] [Google Scholar]
- 37.Thayer KA, Doerge DR, Hunt D, Schurman SH, Twaddle NC, Churchwell MI, et al. Pharmacokinetics of bisphenol A in humans following a single oral administration. Environ Int. 2015;83:107–115. doi: 10.1016/j.envint.2015.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.WHO/UNEP . State of the science of endocrine disrupting chemicals - 2012: an assessment of the state of the science of endocrine disruptors prepared by a group of experts for the United Nations environment Programme (UNEP) and WHO. 2013. [Google Scholar]
- 39.Arsik I, Frediani JK, Frezza D, Chen W, Ayer T, Keskinocak P, et al. Alanine aminotransferase as a monitoring biomarker in children with nonalcoholic fatty liver disease: a secondary analysis using TONIC trial data. Children (Basel). 2018;5. 10.3390/children5060064. [DOI] [PMC free article] [PubMed]
- 40.Judi L, Toukan A, Khader Y, Ajlouni K, Khatib MA. Prevalence of elevated hepatic transaminases among Jordanian patients with type 2 diabetes mellitus. Ann Saudi Med. 2010;30(1):25–32. doi: 10.4103/0256-4947.59369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kang Y, Park J, Youn K. Association between urinary phthalate metabolites and obesity in adult Korean population: Korean National Environmental Health Survey (KoNEHS), 2012–2014. Ann Occup Environ Med. 2019;31(1). 10.35371/aoem.2019.31.e23. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Our investigation was based on KoNEHS cycle 3 (2015–2017), which was approved by the institutional review board of the National Institute of Environmental Research in Korea (NIER-2016-BR-003-01, NIER-2016-BR-003-03). All participants provided written informed consent. The data presented in this study are available on request from the corresponding author. In this case, the researcher receives data that does not include identifiable IDs and/or regional code variables in combination with personal information and other data.