Abstract
Background:
Osteochondral lesion of the talus (OLT) may be caused by osteochondritis dissecans, osteochondral fractures, avascular necrosis, or focal arthritic changes. For certain focal cartilage defects, bone marrow stimulation (BMS) has been a widely used technique to restore a fibrocartilage substitute overlying the defect. There are various postoperative weightbearing protocols for this procedure, with no single gold standard method.
Purpose:
To retrospectively review the outcomes of patients undergoing ankle arthroscopy with concomitant BMS to determine outcomes based on postoperative weightbearing status.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
We retrospectively reviewed the records of patients who underwent ankle arthroscopy with BMS for OLTs between 2015 and 2018. Patients were placed into 2 cohorts based on postoperative immobilization status: the nonweightbearing (NWB) group and the weightbearing-as-tolerated (WBAT) group. Patient characteristics obtained included age, sex, comorbidities, and etiology of talar pathology. Outcomes included the pain visual analog scale (VAS), range of motion (ROM), complications, time to first weightbearing, and the method and length of immobilization. Patients who were lost to follow-up before 30 days were excluded. The chi-square test was used to compare categorical variables between cohorts, and the t test was used for continuous variables.
Results:
A total of 69 patients met the inclusion criteria for this study, 18 in the WBAT group and 51 in the NWB group. The mean lesion size was 9.48 × 9.21 mm (range, 3-15 mm × 2-20 mm) for the NWB group and 9.36 × 9.72 mm (range, 5-14 mm × 6-20 mm) for the WBAT group (P > .05). The VAS scores improved from 4.40 to 0.67 for the WBAT group and from 6.33 to 2.55 for the NWB group, with the difference in final values reaching statistical significance (P = .0002). Postoperative ROM was not significantly different between the groups. There were 4 repeat operations within the NWB cohort.
Conclusion:
The surgical management of OLTs can be challenging, and the postoperative weightbearing protocol can be an extra obstacle for the patient to navigate. We found no difference in pain, ROM, or complications when allowing immediate, full WBAT.
Keywords: weightbearing, ankle arthroscopy, talus, bone marrow stimulation
Osteochondral lesion of the talus (OLT) is a term used to describe abnormal lesions of the talus that may be caused by osteochondritis dissecans, osteochondral fractures, avascular necrosis, and focal arthritic changes. Differentiating the exact cause of individual OLTs can be difficult, and determining the appropriate surgical treatment may also be a challenge, which depends on one’s training and comfort level with surgical management. For focal cartilage defects with minimal to no subchondral loss, microfracture or other bone marrow stimulation (BMS) techniques have been widely used to stimulate the restoration of a hyaline-like fibrocartilage substitute overlying the defect. Numerous studies have shown microfracture to produce excellent clinical outcomes with years of lasting patient satisfaction.3,6,17 As with many other surgical procedures, weightbearing status after microfracture for OLT is often an imprecise decision and can vary by provider.
While many surgeons believe a period of nonweightbearing (NWB) will help facilitate the restorative process and stabilize the post-drilling clot, there is minimal basic science and clinical evidence to support this theory. Because of this uncertainty, postoperative rehabilitation protocols can range from immediate weightbearing as tolerated (WBAT) to a 6- to 8-week period of NWB or restricted/partial weightbearing (PWB).8,20 Restrictions on patients’ weightbearing are not completely innocuous; however, as they may prove difficult for patients’ overall mobility, resulting in decreased quality of life and potential loss of work, they relegate the patients to the usage of assistive devices that may lead to adverse events.2 Additionally, the unique bony architecture of the ankle confers an added level of stability not seen in other joints that may allow for more aggressive postoperative weightbearing considerations.1,16,18,19
To our knowledge, the effects of NWB versus early weightbearing (EWB) in the ankle after microfracture/BMS have not been fully elucidated. The purpose of this study was to retrospectively review the outcomes of patients undergoing ankle arthroscopy and microfracture/BMS to determine whether there was any difference in outcomes in those managed with postoperative EWB versus delayed weightbearing. We hypothesized that the 2 cohorts would have similar postoperative visual analog scale (VAS) scores and range of motion (ROM) measurements, without a difference in complications.
Methods
After institutional review board approval, we conducted a retrospective review of all patients who underwent anterior ankle arthroscopy with microfracture/BMS for OLTs between the years 2015-2018. This was an analysis at a single academic institution, with all surgeries being performed by 5 fellowship-trained, orthopaedic foot and ankle surgeons (including S.B.A. and A.A.) utilizing similar surgical technique. All cases with concomitant procedures that necessitated a period of immobilization were excluded to avoid confounders and potential bias. Patients who did not meet the minimum follow-up period of 30 days were also excluded. There were no exclusions by age. The included patients were placed into 2 cohorts based on the postoperative weightbearing status: NWB in the splint group and the WBAT group. These protocols were chosen by preference of the attending surgeon, and no surgeon switched protocols over the study period. Patients who underwent PWB were excluded because of the potential confounding effect.
Surgical Procedures and Postoperative Rehabilitation
The surgical technique employed was similar across all surgeons included in this study. The patient was placed in the supine position with a bump under the ipsilateral hip. The joint was distended with injection of 10 to 15 mL saline anteromedially. Based on the surgeon’s preference, noninvasive ankle traction was used in some cases. An anteromedial incision was made just medial to the anterior tibial tendon. Once the skin was incised, a small mosquito was placed into the incision and joint and distracted to create a portal. Next, the blunt trocar was placed into the anteromedial portal and the 2.7-mm/30° arthroscope was placed. Under visualization, a spinal needle was placed in the anterolateral aspect of the ankle. This would be where the portal would be placed. Once this was in position, the spinal needle was removed, and a blade was used to make the anterolateral portal. The skin was incised only, care was taken to avoid the superficial peroneal nerve. Next, a mosquito was placed into the anterolateral incision through the capsule into the joint and distracted. A 2.5-mm or 3.5-mm shaver was then placed into the ankle joint. From this point, the amount of debridement and synovectomy differed among the surgeons.
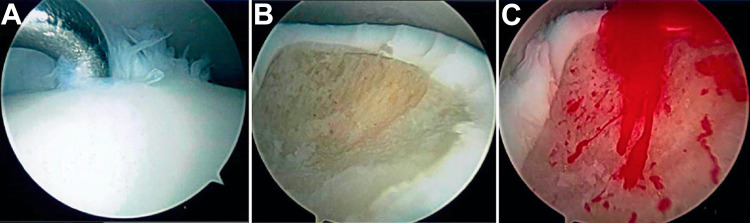
Next, a diagnostic arthroscopy was performed in an order specific to each surgeon but included evaluation of the gutters and the medial, central, and lateral talar dome of the talus as well as the ligamentous structures of the ankle. When a defect was encountered, generally, debridement was performed from the ipsilateral portal to the defect while viewing with the arthroscope from the opposite side. The lesion was debrided using a shaver and curette to create a stable base and measured using the end of a probe with a known length for reference. Next, depending on the attending surgeon’s preference, either a 90° awl was placed in the anteromedial portal and holes were placed into the subchondral bone or a curette was used to remove a thin layer of the subchondral bone. The lesion before and after BMS can be seen in Figure 1. Bleeding was seen emanating from the bone after removal of the lesion, loose bone, and BMS. Instruments were removed, and portals were then closed with a No. 3-0 nylon (Ethicon) interrupted suture. The sutures were removed at 2 weeks postoperatively.
Figure 1.
(A) The medial talar osteochondral lesion viewed from (B) the anterolateral portal after (C) debridement after bone marrow stimulation.
In the WBAT cohort, soft dressings were applied, and a walking boot was placed. The patient was able to remove the dressing at 3 days postoperatively and to shower, but no immersion in water was allowed until 2 weeks postoperatively. The patient was instructed to begin physical therapy (PT) with active and passive ROM at 3 days with local modalities for swelling control. The boot was to be worn at all times when outside the home but could be removed at home and at night. The boot was discontinued at 2 weeks postoperatively. PT from weeks 2 to 6 included the progression of ROM and strengthening as tolerated, with discharge to full activities as tolerated at 6 weeks postoperatively.
In the NWB group, a short leg splint was placed at the time of surgery and worn until the 2-week follow-up. At that time, the splint and sutures were removed, and the patient was transitioned into a cast for an additional 4 weeks. The patient remained NWB for the entirety of the 6 weeks. After this time, the patient was put into a controlled ankle motion boot and transitioned to gradual WBAT, with boot removal for the NWB ankle ROM. The boot was removed after 6 weeks, and the patient began formal PT for the ankle ROM, strengthening, and return to sport progression.
Outcome Measures and Statistical Analysis
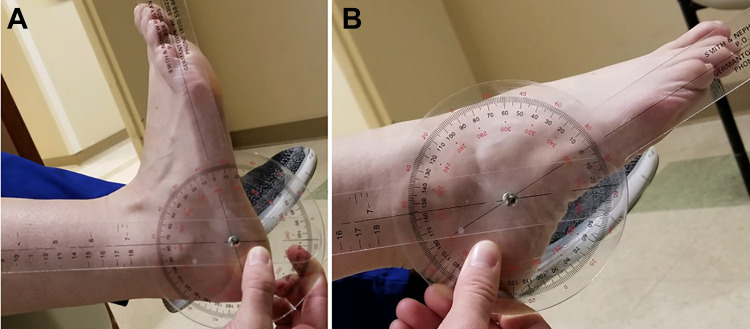
Patient characteristics and outcomes were reviewed and included preoperative and postoperative data points. Patient characteristics included age, sex, comorbidities, and etiology of talar pathology. Outcomes included the VAS for pain (0-10 [worst pain]), ROM, complications, time to first weightbearing, and the method and length of immobilization. ROM measurements were performed by the provider in the clinic using a manual goniometer with the knee at 90° (Figure 2).
Figure 2.
Example of range-of-motion measurements: (A) dorsiflexion and (B) plantarflexion.
Statistical measures were used to compare the cohorts, with chi-square test used for categorical variables and the t test for continuous variables. A post hoc power analysis was performed and showed the study to be properly powered to determine any changes in VAS scores. Statistical analyses were performed using MedCalc for Windows Version 15.0 (MedCalc Software). The level of significance was set at P < .05.
Results
A total of 275 patients underwent ankle arthroscopy between 2015 and 2018. Of these patients,195 were excluded for having additional confounding procedures, 6 inadequate follow-up time, and 5 PWB status. Ultimately, 69 patients were included: 51 patients in the NWB group and 18 in the WBAT group. Outcome measures for all patients were obtained at the final follow-up.
Complete demographics and lesion characteristics can be found in Tables 1 and 2. The mean age was 34.56 years (range, 14-70 years) for the WBAT group and 39.71 years (range, 13-73 years) for the NWB group. The mean follow-up for the WBAT group was 406 days (range, 37-1177 d) and 568 (range, 32-1771 d) in the NWB group. The mean lesion size for the NWB group was 9.48 × 9.21 mm (range, 3-15 mm × 2-20 mm) and 9.36 × 9.72 mm (range, 5-14 mm × 6-20 mm) for the WBAT cohort. These variables were not significantly different between the 2 groups.
TABLE 1.
Characteristics of the Study Groupsa
| WBAT (n = 18) | NWB (n = 51) | P Value | |
|---|---|---|---|
| Sex, male/female | 11/7 | 24/27 | |
| Age, y | 34.56 ± 18.91 | 39.71 ± 14.54 | .24 |
| Race | |||
| White | 14 | 36 | |
| Black | 1 | 9 | |
| Asian | 0 | 1 | |
| Other | 3 | 5 | |
| Smoker | |||
| Current | 2 | 7 | |
| Never | 15 | 34 | |
| Former | 1 | 8 | |
| Not answered | 2 | ||
| Laterality, right/left | 9/9 | 23/28 | |
| Weight, kg | 88.53 ± 30.94 | 89.49 ± 27.01 | .90 |
| Height, cm | 170.23 ± 23.52 | 168.95 ± 26.44 | .86 |
aData are presented as mean ± SD or No. NWB, nonweightbearing; WBAT, weightbearing as tolerated.
TABLE 2.
Location and Sizes of OLTa
| WBAT (n = 18) | NWB (n = 51) | |
|---|---|---|
| Location, n | ||
| Medial | 7 | 29 |
| Lateral | 7 | 15 |
| Medial and lateral | 2 | 4 |
| Posterior | 1 | 1 |
| Medial and central | 0 | 1 |
| Not recorded | 1 | 1 |
| Size, mm, mean (range)b | 9.36 × 9.72 (5-14 × 6-20) |
9.48 × 9.21 (3-15 × 2-20) |
aNWB, nonweightbearing; OLT, osteochondral lesion of the talus; WBAT, weightbearing as tolerated.
bNonsignificant differences between groups (P ≥ .05).
Complete outcome results can be found in Table 3. The VAS pain scores improved for the WBAT group from 4.40 to 0.67 and from 6.33 to 2.55 for the NWB group. The postoperative VAS scores were significantly lower for the WBAT compared with the NWB group (P = .0002). Postoperative ROM measurements for plantarflexion and dorsiflexion were not significantly different between the groups. A multiple regression analysis was performed for all independent variables, which were each nonpredictive for postoperative VAS scores. Within the NWB cohort, 4 patients required reoperation for continued pain, with 3 undergoing repeat arthroscopy and the fourth undergoing syndesmotic fusion and fibular osteotomy. There were no additional nonoperative complications in the NWB group. No operative or nonoperative complications were encountered in the WBAT cohort.
TABLE 3.
Results of Outcome Measuresa
| WBAT (n = 18) | NWB (n = 51) | P Value | |
|---|---|---|---|
| Follow-up, d, mean (range) | 406 (37-1177) | 568 (32-1771) | .21 |
| Length of immobilization, d | 0 | 30.75 ± 17.87 | |
| Preoperative | |||
| VAS pain | 4.40 ± 1.52 | 6.33 ± 2.50 | .0031 |
| ROM dorsiflexion, deg | 15.59 ± 6.59 | 13.02 ± 7.25 | .19 |
| ROM plantarflexion, deg | 44.12 ± 11.21 | 45.47 ± 8.72 | .62 |
| Postoperative | |||
| VAS pain | 0.67 ± 0.82 | 2.55 ± 1.92 | .0002 |
| ROM dorsiflexion, deg | 16.92 ± 5.96 | 14.62 ± 7.20 | .23 |
| ROM plantarflexion, deg | 43.93 ± 8.81 | 43.65 ± 10.91 | .92 |
| Repeat operations, n | 0 | 4 | |
| Nonoperative complications, n | 0 | 0 |
aData are presented as mean ± SD unless otherwise indicated. Bolded P values indicate statistically significant differences between groups (P < .05). NWB, nonweightbearing; ROM, range of motion; VAS, visual analog scale; WBAT, weightbearing as tolerated.
Discussion
The most significant findings of this study are that immediate WBAT after microfracture of OLT appears to be a safe, effective postoperative weightbearing protocol. Patients who were made to immediately WBAT were found to have a significantly lower postoperative VAS score, averaging under 1, with no repeat operations or nonoperative complications. Alternatively, the NWB group had a mean postoperative VAS pain score of 2.55 with 4 repeat procedures, despite similar preoperative lesion sizes among the 2 cohorts.
Arthroscopic microfracture is an effective treatment for OLT lesions under 2 cm in size. The stimulation of fibrocartilage is thought to provide a primary benefit of filling in the osteochondral defect and preventing pain and disability by improving the mechanics of the joint. Based on the underlying mechanism of repair, conservative postoperative protocols have traditionally been followed to protect the new fibrocartilage and promote further healing.4 In cases in which microfracture sites have been revisited arthroscopically, there is evidence that the natural borders of the lesion confer a protective environment for the new cartilage from the loading forces of weightbearing and thus do not require restrictions.9 Literature detailing earlier weightbearing protocols for OLT microfracture has reported successful outcomes, which is supported by the postoperative pain ratings and lack of increased complications found in this study.12 Similarly, the question of weightbearing after microfracture in the knee has been explored and the outcomes found to be equivocal in the available literature. Marder et al13 found that small, full-thickness femoral condyle defects treated with microfracture did just as well with WBAT, with no continuous passive motion, when compared with a group that was NWB and utilized early continuous passive motion as determined by patient-reported outcomes. A recent literature review corroborates these findings in the knee, suggesting that weightbearing restrictions do not have an effect on outcomes in the microfracture of the tibiofemoral or patellofemoral lesions, although the minimal level 1 evidence is a noted limitation.9 However, despite the similarities in both pathology and microfracture technique between the talus and the ankle, a direct comparison between the 2 joints should not be made.
The ability to allow EWB, specifically in the ankle, is based on the bony architecture, which confers a stability not seen in other joints and is less reliant on soft tissue constraints.1,16,18,19 Specifically, regarding OLT microfractures, studies by Lee et al11 and Deal et al4 compared early mobilization at 2 weeks and late mobilization at 6 weeks, each showing comparable outcomes years after the procedures in both the VAS and the American Orthopedic Foot & Ankle Society scores.4,11 One study that did examine immediate WBAT postoperatively in 58 patients showed a decrease in the VAS from 7.31 to 0.95 postoperatively, with just the use of a figure-of-8 brace, but did not have a weight restricted cohort to compare directly against.12 The primary difference between our study and those in the literature is the inclusion of a direct comparison of NWB cohorts against which the outcomes measures can be directly compared. These findings suggest that the least restrictive weightbearing status, allowing patients to self-regulate by comfort, may not compromise clinical outcomes and would allow patients to avoid some of the complications that can stem from restrictions. In fact, our study suggests that patients experience a greater degree of pain relief when able to ambulate right away, which may be due to a variety of underlying causes. Despite these potential benefits, it is important to note that this study did not perform a formal magnetic resonance imaging (MRI) analysis of the repaired tissue and therefore cannot comment on the quality of the repair tissue.
While seemingly innocuous in young, healthy patients, weightbearing restrictions can result in a significant burden on others, making the decision on the extent and duration of immobilization critical. Common complications from immobilization range in severity but include loss of muscle strength and endurance; increased stiffness and pain in the immobilized joint; loss of cardiovascular endurance from decreased activity; and an increased risk for more severe complications, such as decreased cardiac reserve, orthostatic hypotension, and venous thromboembolism.5 Even after short-term immobilization, it can take months to recover the losses in ROM and strength, which can lead to additional costs related to loss of work and therapy.7,15 While the data in our study did not reach statistical significance, there was a trend toward improved postoperative ROM in the WBAT group compared with the NWB group at the final follow-up. On a practical note, research has also shown that patients often do not comply with prescribed weightbearing precautions, despite clear instructions.14 There are also drawbacks with the assistive devices necessary to maintain a partial or NWB status. While crutches or scooters allow for the weight to be redistributed to the contralateral side, they can require excessive strength, balance, and metabolic demands that could result in injury even in younger patients.2,10 If patients are unable to effectively utilize these devices, they may opt to be more sedentary. For these reasons, it should be the goal to provide patients with the least restrictive weightbearing status possible that does not compromise their outcome.
The primary limitation of this study is the retrospective nature of the design and the relatively small number of cases included, despite being the largest study of its kind to our knowledge. There was also no formal randomization to the cohorts, and patient allocation was purely based on who presented to each attending clinic preoperatively through various scheduling arms. While many patients had long-term follow-ups, there were also a few included who had relatively a short-term follow-up of just over 4 weeks, which was standard for patients doing well in the practice of one of the attending surgeons. There were also no patient-reported outcome scores, second-look arthroscopy on a significant number of the cases, or MRI analysis of repair tissue quality, which prevented the analysis of these important factors. Despite the limitations, we believe that these findings warrant further investigation with a formal randomized controlled trial or simply further consideration of postoperative weightbearing status by the provider.
Conclusion
The surgical management of OLTs can be challenging, and the postoperative weightbearing protocol can be an extra obstacle for the patient to navigate. We found no difference in the VAS, ROM, or complications when allowing immediate, full WBAT as well as using removable immobilization, as compared with a variety of other protocols at early follow-up. In fact, there was a trend toward lower pain scores in the immediate full weightbearing group. Although the follow-up was short term in this study, the early outcomes suggest equivalency when allowing immediate weightbearing and removable immobilization after ankle arthroscopy and talar microfracture.
Footnotes
Final revision submitted February 22, 2021; accepted March 2, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: N.L.G. has received hospitality payments from Smith & Nephew. B.L. has received grant support from DJO and Zimmer Biomet; education payments from Smith & Nephew; and hospitality payments from Wright Medical. S.A.A. has received education payments from Terumo BCT; consulting fees from 4WEB, Conventus, Embody, Exactech, MedShape, Ortho Solutions, Orthofix, RTI Surgical, Sonoma Orthopedics, Stryker, and Trimed; nonconsulting fees from 4WEB, Arthrex, Medline, and Terumo BCT; honoraria from In2Bones; and hospitality payments from Wright Medical and has stock/stock options in Tyber Medical. A.A. has received consulting fees from Arthrex and Bioventus; nonconsulting fees and royalties from Arthrex; and hospitality payments from Lima USA. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Duke Health Institutional Review Board (protocol ID: Pro00092763).
References
- 1.Anderson DD, Tochigi Y, Rudert MJ, Vaseenon T, Brown TD, Amendola A. Effect of implantation accuracy on ankle contact mechanics with a metallic focal resurfacing implant. J Bone Joint Surg Am. 2010;92(6):1490–1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bateni H, Maki BE. Assistive devices for balance and mobility: benefits, demands, and adverse consequences. Arch Phys Med Rehabil. 2005;86(1):134–145. [DOI] [PubMed] [Google Scholar]
- 3.Choi SW, Lee GW, Lee KB. Arthroscopic microfracture for osteochondral lesions of the talus: functional outcomes at a mean of 6.7 years in 165 consecutive ankles. Am J Sports Med. 2020;48(1):153–158. [DOI] [PubMed] [Google Scholar]
- 4.Deal JB, Patzkowski JC, Groth AT, et al. Early vs delayed weightbearing after microfracture of osteochondral lesions of the talus: a prospective randomized trial. Foot Ankle Orthop. 2019;4(2):2473011419838832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dittmer DK, Teasell R. Complications of immobilization and bed rest, part I: musculoskeletal and cardiovascular complications. Can Fam Physician. 1993;39:1428–1437. [PMC free article] [PubMed] [Google Scholar]
- 6.Donnenwerth MP, Roukis TS. Outcome of arthroscopic debridement and microfracture as the primary treatment for osteochondral lesions of the talar dome. Arthroscopy. 2012;28(12):1902–1907. [DOI] [PubMed] [Google Scholar]
- 7.Grosset J-F, Onambele-Pearson G. Effect of foot and ankle immobilization on leg and thigh muscles’ volume and morphology: a case study using magnetic resonance imaging. Anat Rec. 2008;291(12):1673–1683. [DOI] [PubMed] [Google Scholar]
- 8.Hurst JM, Steadman JR, O’Brien L, Rodkey WG, Briggs KK. Rehabilitation following microfracture for chondral injury in the knee. Clin Sports Med. 2010;29(2):257–265, viii. [DOI] [PubMed] [Google Scholar]
- 9.Jain D, Belay ES, Anderson JA, Garrett WE, Lau BC. Are weightbearing restrictions required after microfracture for isolated chondral lesions of the knee? A review of the basic science and clinical literature. Sports Health. 2021;13(2):111–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lai Y-F, Lin P-C, Chen C-H, Chen J-L, Hsu H-T. Current status and changes in pain and activities of daily living in elderly patients with osteoarthritis before and after unilateral total knee replacement surgery. J Clin Med. 2019;8(2):221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee DH, Lee KB, Jung ST, Seon JK, Kim MS, Sung IH. Comparison of early versus delayed weightbearing outcomes after microfracture for small to midsized osteochondral lesions of the talus. Am J Sports Med. 2012;40(9):2023–2028. [DOI] [PubMed] [Google Scholar]
- 12.Li S, Li H, Liu Y, Qu F, Wang J, Liu C. Clinical outcomes of early weight-bearing after arthroscopic microfracture during the treatment of osteochondral lesions of the talus. Chin Med J (Engl). 2014;127(13):2470–2474. [PubMed] [Google Scholar]
- 13.Marder RA, Hopkins G, Jr, Timmerman LA. Arthroscopic microfracture of chondral defects of the knee: a comparison of two postoperative treatments. Arthroscopy. 2005;21(2):152–158. [DOI] [PubMed] [Google Scholar]
- 14.Polat G, Karademir G, Akalan E, Aşık M, Erdil M. Patient compliance with touchdown weight bearing after microfracture treatment of talar osteochondral lesions. J Orthop Surg Res. 2017;12(1):46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shaffer MA, Okereke E, Esterhai JL, Jr, et al. Effects of immobilization on plantar-flexion torque, fatigue resistance, and functional ability following an ankle fracture. Phys Ther. 2000;80(8):769–780. [PubMed] [Google Scholar]
- 16.Stormont DM, Morrey BF, An KN, Cass JR. Stability of the loaded ankle; relation between articular restraint and primary and secondary static restraints. Am J Sports Med. 1985;13(5):295–300. [DOI] [PubMed] [Google Scholar]
- 17.Takao M, Ochi M, Naito K, Uchio Y, Kono T, Oae K. Arthroscopic drilling for chondral, subchondral, and combined chondral-subchondral lesions of the talar dome. Arthroscopy. 2003;19(5):524–530. [DOI] [PubMed] [Google Scholar]
- 18.Tochigi Y, Rudert MJ, Amendola A, Brown TD, Saltzman CL. Tensile engagement of the peri-ankle ligaments in stance phase. Foot Ankle Int. 2005;26(12):1067–1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tochigi Y, Rudert MJ, Saltzman CL, Amendola A, Brown TD. Contribution of articular surface geometry to ankle stabilization. J Bone Joint Surg Am. 2006;88(12):2704–2713. [DOI] [PubMed] [Google Scholar]
- 20.van Eekeren IC, Reilingh ML, van Dijk CN. Rehabilitation and return-to-sports activity after debridement and bone marrow stimulation of osteochondral talar defects. Sports Med. 2012;42(10):857–870. [DOI] [PubMed] [Google Scholar]