Abstract
Background:
Although research demonstrates that autistic children are at risk of poor sleep quality, very little is known about sleep quality and its impact on quality of life in autistic adults. We investigated the relationships between sleep quality, perceived stress, and quality of life for autistic adults.
Method:
Data were prospectively collected from both autistic adults (N=40) and non-autistic adults (N=24). Sleep Quality was measured using the Pittsburgh Sleep Quality Index, Perceived Stress was measured using the Perceived Stress Scale, and Quality of Life was measured using the Brief Version of the World Health Organization Quality of Life Scale. We ran OLS regression models to examine the association between study group, perceived stress, sleep quality, and quality of life. We tested for main effects of study group (i.e., autistic or non-autistic), sleep quality, and perceived stress, adjusting for demographic characteristics. Then, we tested the interaction between study group and sleep quality. Finally, we tested a three-way interaction between group, sleep quality, and perceived stress.
Results:
Autistic adults reported worse sleep quality compared to non-autistic adults. Poorer sleep quality was significantly associated with lower quality of life for all participants in the study. Findings from the three-way interaction indicated that higher perceived stress further exacerbated the relationship between poorer sleep quality and lower quality of life for autistic adults.
Conclusions:
These findings suggest that interventions that target both sleep quality and stress could effectively improve quality of life for autistic adults.
Keywords: ASD, Asperger’s, sleep disorders, sleep problems, stress, intervention
Introduction
Humans spend about a third of their lives sleeping, and sleep plays a key role in maintaining health and wellbeing throughout life. The unfavorable consequences of sleep loss are well-documented. Poor sleep quality has been associated with decreased psychological well-being, including poorer mood, cognitive failures, lost work productivity, and lower relationship satisfaction (Steptoe et al., 2008). In addition to psychosocial consequences, research indicates that lack of sleep can have adverse effects on the cardiovascular, immunological, and endocrinological systems (Okun, 2011). More specifically, sleep can dysregulate immune and endocrine pathways which put individuals at increased risk of inflammatory mediated diseases such as cardiovascular disease, diabetes, metabolic syndrome, and depression (Okun, 2011). Better understanding sleep quality in populations with documented sleep problems is important because sleep is foundational to health and well-being.
Sleep problems in autistic people are highly prevalent and may be associated with increased physical and mental health problems (Richdale & Schreck, 2009). A number of studies report high rates of sleep problems in autistic children compared to typically developing peers (Souders et al., 2009). Though sleep is less studied in autistic adults, research has begun to indicate that these problems persist into adulthood (Goldman et al., 2017; Schreck & Richdale, 2020). Further, autistic adults have a higher risk of all major psychiatric disorders including anxiety and depression, and other medical conditions including obesity, diabetes, and immune conditions (Croen et al., 2015; Hollocks et al., 2019; Steensel et al., 2011; Whitney et al., 2018). Premature mortality is markedly increased in autistic adults, partially resulting from increased medical and psychiatric morbidity (Hirvikoski et al., 2016). Poor physical and mental health in autistic people is linked to lower quality of life (Bishop-Fitzpatrick et al., 2016), and sleep may contribute to both increased physical morbidity and decreased quality of life.
Sleep Quality in Autistic Children
Sleep problems are one of the major concerns consistently reported by parents of autistic children (Richdale, 1999). Previous studies have found that parent reports of sleep problems of their autistic children range from 50% to 80%, compared to 9% to 50% in non-autistic comparison groups (Allik et al., 2006; Couturier et al., 2005; Malow et al., 2006; Polimeni et al., 2005). Objective sleep measures such as polysomnography and actigraphy support these subjectively reported symptoms of poor sleep in autistic children (Richdale & Schreck, 2009)
Several biopsychosocial factors—including biological abnormalities in circadian rhythm and melatonin—are associated with sleep problems in autistic children. Several studies indicate that low melatonin levels are common in autistic children (Kulman et al., 2000; Tordjman et al., 2005). Furthermore, Bourgeron (2007) found that clock gene mutations, which play a central role in regulation of circadian rhythms, coupled with abnormal decreases in melatonin levels in autistic children are associated with abnormal circadian rhythm, including sleep/wake rhythm. These factors may be linked to the high levels of insomnia seen in autistic children. This link has important implications for quality of life in autistic children as insomnia has been associated with psychological health in both the typically developing and autistic populations, including anxiety, depression, and hypersensitivity to touch (Nadeau et al., 2014; Richdale & Schreck, 2009; Tzischinsky et al., 2018; Uren et al., 2019). These biological processes underlying sleep problems in autistic children are likely to affect sleep throughout life.
Sleep Quality in Autistic Adults
Research has begun to support the notion that these sleep problems continue into adulthood (Ballester et al., 2018; Goldman et al., 2017). According to a 2015 study (Baker & Richdale), problems related to sleep, in particular insomnia, continue into adulthood for those with autism spectrum disorder. The 36 autistic participants in this study experienced significantly more sleep disturbances, longer sleep onset latencies, and poorer sleep efficiency (Baker & Richdale, 2015). A recent longitudinal study (Deserno et al., 2019) spanning across two years and focusing on multiple potential predictors of quality of life, found that sleep problems are a strong correlate of quality of life in autistic adults. Another recent study provides additional evidence that suggests that sleep quality impact quality of life: Lawson and colleagues found that among autistic and non-autistic adults (aged 15–80), depression symptoms, psychological well-being, sleep quality, and autonomic symptoms are all significant correlates of quality of life (Lawson et al., 2020). Their findings demonstrate that lower sleep quality is associated with reduced physical quality of life for both groups. Their findings suggest that interventions targeting depression and insomnia symptomatology could improve overall well-being in autistic adults (Lawson et al., 2020). With this in mind, our study sought to build on this emerging body of research that identifies sleep quality as a strong correlate of quality of life and determines whether stress may exacerbate this relationship.
Quality of Life and Perceived Stress in Autistic Adults
Recent research consistently suggests that quality of life in autistic adults in relatively poor (Ayres et al., 2018; Hong et al., 2016; Kamp-Becker et al., 2010; Khanna et al., 2014) and may be particularly poor for autistic adults with worsened physical and mental health (Bishop-Fitzpatrick et al., 2016; Schreck, 2021). A recent study found that sleep problems are correlated with quality of life in autistic adults (Deserno et al., 2019). This study used a large longitudinal database that covered the entire adult lifespan and included measures of autism-specific characteristics, co-occurring conditions, aspects of daily functioning, and demographics (Deserno et al., 2019). Our use of a non-autistic adult control group as a comparison serves to further test these findings and assess the unique needs of autistic adults.
Stress is also a contributing factor to quality of life in autistic adults. An association between perceived stress and quality of life in autistic and non-autistic populations is well-established (Bishop-Fitzpatrick et al., 2018; Hirvikoski & Blomqvist, 2014; Hong et al., 2016). Further, in the non-autistic population, research has demonstrated an association between perceived stress, sleep quality, and quality of life (LeBlanc et al., 2007). Considering if this relationship were also true for autistic adults would be highly valuable in better understanding predictors and developing interventions to improve quality of life. Therefore, moderation analysis could be used to test this combined effect of sleep quality and perceived stress on quality of life of autistic adults.
Aims and Purpose
The overall purpose of this study was to expand upon previous work that documents the association between perceived stress and quality of life in autistic adults and to further examine the contribution of sleep quality to quality of life. We aimed to evaluate the direct and indirect effect of sleep quality on perceived stress and quality of life. We also aimed in exploratory analyses to examine whether being autistic moderates the impact of stress and sleep quality on quality of life using exploratory analyses. Based on previous research, we first hypothesized that sleep quality would be worse in autistic adults compared to non-autistic adults. Additionally, we hypothesized that there would be a significant, positive association between sleep quality and quality of life in both groups. Findings have the potential to inform interventions directed at improving quality of life and sleep quality in autistic adults.
Methods
Participants
Data were prospectively collected from 40 autistic adults who were enrolled in an active comparative effectiveness study of two psychosocial interventions for autistic adults [reference removed for blind review]. All participants who were enrolled in this clinical trial were sent informational letters about the study, and the first 40 to respond who met the eligibility criteria were enrolled. Eligibility criteria included satisfying expert clinical opinion and research criteria for autism spectrum disorder based on the Autism Diagnostic Observation Schedule (Lord et al., 2000) or the Autism Diagnostic Interview-R (Lord, Rutter, & Le Couteur, 1994); age 18–55 years; and intelligent quotient (IQ) ≥ 80 as assessed by the Wechsler Abbreviated Scale of Intelligence (Wechsler, 2008).
An additional cohort of 24 non-autistic adults who were matched to the autistic group on age, biological sex, and race were also recruited. These participants had no current psychiatric disability, as confirmed through the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders (First et al., 2002) and had no other major medical disorders. This comparison group was recruited through a database of participants who had served as non-autistic volunteers in previous autism studies.
This study was approved as part of a larger intervention study by the [university name removed for blind review] Institutional Review Board, and all data collected were dealt with confidentially and complied with the policies and procedures governing research set forth by the University. All participants provided written informed consent prior to enrollment. Data were collected in 2014 and 2015 from autistic participants at different timepoints of the larger comparative effectiveness study. There was no significant association between treatment exposure our dependent variable (quality of life). Thus, we did not covary for treatment exposure in analyses (described below).
Power Analysis and Sample Size
Estimates of sample size requirements for the proposed study were calculated using standard procedures (Cohen, 1988), assuming that the criterion for statistical significance is set at alpha = .05 and for statistical power (1-beta) = .80. Previous studies have identified a large effect size for the association between perceived stress and quality of life (Hong et al., 2016; Bishop-Fitzpatrick et al., 2018) and sleep and quality of life (Lawson et al., 2020) in autistic adults. Sample size was thus set to detect a large effect size (d = .80). All power analyses were conducted a priori using with G*Power 3.1 (Faul et al., 2007). Our sample size allows us to detect a large effect (d = .80) for the difference in perceived stress and sleep quality between autistic adults and non-autistic adults, as well as a large effect for the relationship between stress and sleep quality, and quality of life (f2 = .35, R2 = .35).
Measures
Independent Variable: Sleep Quality.
Sleep quality was measured using the Pittsburgh Sleep Quality Index (PSQI), which is a self-rated questionnaire that measures sleep quality over seven areas of sleep. It measures quality and patterns of sleep in adults. It differentiates “poor” from “good” sleep by measuring seven domains: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction. Questions include: “When have you usually gone to bed?”; “How long has it taken you to fall asleep at night?”; “During the past month, how often have you had trouble staying awake while driving, eating meals, or engaging in social activity?”; and “During the past month, how much of a problem has it been for you to keep up enthusiasm to get things done?” In order to conserve power, we used a composite score of overall sleep quality (Buysse et al., 1988) rather than domain scores in all analyses. The PSQI has strong internal consistency with a Cronbach’s alpha of 0.83 in the general population and 0.68 in autistic adults (Baker & Richdale, 2015). Reliability of the composite score in this sample was α = 0.68, suggesting that internal consistency remains adequate for autistic adults who self-report their sleep quality.
Independent Variable: Perceived Stress.
Perceived stress was measured using the Perceived Stress Scale (PSS), which consists of 10 items that are rated on a 5-point Likert scale where higher scores are indicative of greater perceived stress. Questions include: “In the last month, how often have you been upset because of something that happened unexpectedly?”; “How often have you felt things were going your way?”; and “How often have you found that you could not cope with all the things that you had to do?” This is a highly reliable scale with a Cronbach’s alpha of 0.91 in the general population (Cohen & Janicki-Deverts, 2012), and 0.76 in adults with mixed-IQ (Hong et al., 2016). Reliability in this sample was α = 0.90.
Dependent Variable: Quality of Life.
Quality of Life was measured using the Brief version of the World Health Organization Quality of Life Scale (WHOQOL-BREF). The WHOQOL-BREF measures subjective quality of life in the domains of physical health, psychological health, social relationships, and environment. The scale contains 26 items which are measured on a 5-point scale, with higher scores indicating better quality of life. Similar to previous autism research that utilizes the WHOQOL-BREF, we used scale scores for our analyses (possible range= 0–100; Hong et al., 2016; Bishop-Fitzpatrick et al., 2018). Examples of questions include: “To what extent do you feel that physical pain prevents you from doing what you need to do?”; “Do you have energy for everyday life?”; “How satisfied are you with your personal relationships?”; and “How satisfied are you with your access to health services?” This is a highly reliable scale with a Cronbach’s alpha of 0.93 in the general population and 0.71 in autistic adults (Hong et al., 2016). Reliability in this sample was α = 0.94.
Demographic Variables.
Sex, race, and employment status were self-reported and recorded on the day of data collection. We used dummy coding to separate responses to these independent variables: sex, race, employment and diagnosis. Sex is male (1) or female (0), race is white (1) or racial minority (0), employment is employed (1) or unemployed (0), and diagnosis is autism diagnosis (1) or none (0). The racial minority category includes participants that identified as African American or Black (N=7), Asian (N=2), Hispanic (N=1), Hispanic or Latino (N=2), Multiple (African American and White) (N=1), and Multiple (N=1). We did not include a measure of autism severity in our analyses because autism severity data were not collected for non-autistic participants.
Interaction Terms.
We included three separate interaction terms in the third exploratory model to further understand the relationships among our variables. The first two-way interaction variable (Autism X Sleep Quality) tests the interaction effect between group and sleep quality. The next two-way interaction variable (Autism X Stress) tests the interaction effect between group and stress. Finally, we created a three-way interaction variable between diagnosis, sleep quality, and perceived stress to further assess the relationship among the three, and its prediction of quality of life. The beta estimate provides a centered and standardized coefficient for each term in the regression analysis.
Analyses
We conducted preliminary analyses to ensure that parametric tests were appropriate. These data conformed to the assumptions of homoscedasticity and the residuals were normally distributed. One participant scored higher than others on the quality of life measure. However, this participant’s response was not highly leveraged, in that it did not unduly influence the regression analysis results, and this score was kept in the data. Missing data were estimated at the time of analysis using the expectation-maximization (EM) algorithm, which results in less biased parameter estimates than mean or regression imputation (Schafer & Graham, 2002).
We first used one way ANOVAs to test group differences in perceived stress, sleep quality, and quality of life and Pearson’s correlation coefficients to test the bivariate associations between perceived stress, sleep quality, and quality of life. Then, using OLS regression, we examined the relationship between sleep quality and quality of life. Demographic characteristics were entered into the second model in order to account for their impact on quality of life, along with sleep quality and perceived stress to test for their main effects. Next, exploratory analyses tested the impact of the interaction between sleep quality and group on quality of life. Finally, we tested our exploratory three-way interaction between sleep quality, perceived stress, and group. Standardized regression coefficients (β) were also generated as an effect size metric to assess the strength of these associations (Nieminen et al., 2013). Finally, to conserve power, we conducted post-hoc multiple pairwise correlational comparisons between quality of life and the seven sleep quality domains in our sample of autistic adults. All analyses were conducted using STATA version 15.1.
Results
Preliminary Analyses
Demographic characteristics of autistic and non-autistic adults are presented in Table 1. Most participants were male, white, and in their mid-twenties. Autistic and non-autistic adults did not differ significantly with regard to sex, race, or age, suggesting that group matching was successful. Of the autistic adults in our sample, less than half were employed. As expected, this differed significantly from the non-autistic adults. Ultimately, employment status was not included in regression analyses as it did not influence the results.
Table 1.
Demographic Characteristics of Participants
| Variables | Autistic Adults (N=40) | Non-Autistic Adults (N=24) | p† |
|---|---|---|---|
|
| |||
| Age | 24.2 (6.95) | 25 (3.68) | 0.605 |
| Male | 36 (90) | 20 (83.33) | 0.443 |
| White | 33 (82.50) | 16 (66.67) | 0.153 |
| Employed | 19 (47.50) | 20 (83.33) | 0.004 |
| Full-scale IQ* | 106.53 (15.33) | 110.375 (14.94) | 0.33 |
Note. M = mean, SD = standard deviation, N = number
independent t-test, two-tailed, for significant differences between autistic adults or non-autistic adults
Based on the Wechsler Adult Intelligence Scale-Revised.
Group Differences in Sleep Quality, Perceived Stress, and Quality of Life
Differences between autistic and non-autistic adults across independent and dependent variables, as well as correlations between these variables, are presented in Table 2. Autistic adults had significantly poorer sleep quality [F(1, 62) = 18.52, p < 0.001], higher perceived stress [F(1, 62) = 12.53, p < 0.001], and lower quality of life [F(1, 62) = 19.94, p < 0.001] compared to non-autistic adults. Correlational analyses revealed statistically significant associations between perceived stress, sleep quality, and quality of life for autistic adults versus non-autistic adults. Autistic adults reported worse composite sleep quality, greater perceived stress, and lower quality of life than non-autistic adults. The size of these differences were large (Cohen, 1988), with Cohen’s d = 0.93 for sleep quality, Cohen’s d = 1.12 for perceived stress, and Cohen’s d = 1.15 for quality of life.
Table 2.
Group Differences in Perceived Stress, Sleep Quality, and Quality of Life
| Group Differences Mean (SD) | F | d | Correlation Coefficients | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Autistic Adults | Non-Autistic Adults | Autistic Adults | Non-Autistic Adults | |||||
|
| ||||||||
| Variable | 1. | 2. | 1. | 2. | ||||
| 1. Perceived Stress | 23.15 (3.36) | 19.5 (3.15) | 18.52*** | 1.12 | -- | -- | ||
| 2. Sleep Quality | 6.21 (3.11) | 3.5 (2.73) | 12.53*** | 0.93 | 0.4146** | -- | 0.0757 | -- |
| 3. Quality of Life | 59.06 (11.93) | 73.03 (12.41) | 19.94*** | 1.15 | −0.386* | −3249* | −0.3515 | −0.6631 |
Note. SD = standard deviation; d = Co’en’s d
p < .05
p < .01
p < .001
Prediction of Quality of Life based on Diagnosis, Perceived Stress and Sleep Quality
There was a significant main effect of sleep quality on quality of life for all participants in the study, B = −1.447, β = −0.339, p < 0.01, when controlling for diagnosis, age, sex, full scale IQ, and perceived stress. As expected, based on previous research, there was a significant main effect of having an autism diagnosis and perceived stress on quality of life in the bivariate and full models. Results of these regression models are displayed in Table 3.
Table 3.
Unstandardized and Standardized Coefficients from the Regression of Quality of Life on Sleep Quality, Stress, and Selected Independent Variables
| Predictor Variables | Bivariate Model | Full Model | ||
|---|---|---|---|---|
|
| ||||
| B (SE) | β | B (SE) | β | |
|
| ||||
| Autism Diagnosis | −13.96*** (3.127) | −1.01 | −6.103 (3.291) | −0.442 |
| Age (in years) | −0.170 (.235) | −0.073 | ||
| Sex (ref: women) | ||||
| Men | −4.714 (4.170) | −0.114 | ||
| Full Scale IQ | 0.110 (.0923) | 0.121 | ||
| Perceived Stress | −0.911* (.438) | −0.245 | ||
| Sleep Quality | −1.447** (.483) | −0.339 | ||
| Constant | 73.03*** (2.47) | 91.88*** (12.99) | ||
| Observations | 64 | 64 | ||
SE: Standard error of the regression coefficient
β: Standardized beta
p<0.05
p<0.01
p<0.001
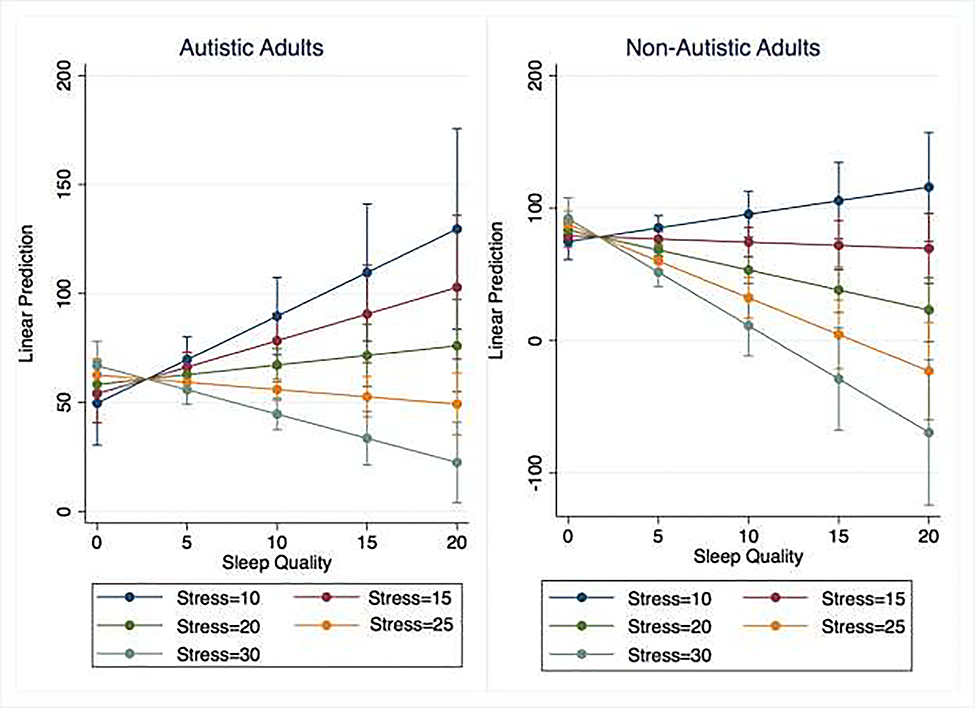
Prediction of Quality of Life based on the Interactions between Diagnosis, Perceived Stress and Sleep Quality
We found no significant interaction effect between group and perceived stress, nor between group and sleep quality on quality of life. These findings demonstrate there is no combined significant association between diagnosis (autism vs. not) and sleep quality and diagnosis and perceived stress on quality of life despite autistic adults reporting both worse composite sleep quality and higher levels of perceived stress. However, we did find a statistically significant three-way interaction effect among autism diagnosis, perceived stress, and sleep quality on quality of life, B = −3.11, β = −0.144, p < 0.01. Interaction models are displayed in Table 4 and presented graphically in Figure 1. The use of a three-way interaction in our moderated regression analysis tested the combined effect of our three independent variables on quality of life. The three-way interaction demonstrates that the interaction between sleep quality and perceived stress is different depending on group. The relationship shown among sleep quality, perceived stress, and quality of life depends on having an autism diagnosis. This demonstrates a significant moderation effect as the interaction between sleep quality and perceived stress and its association with quality of life is not the same for the autistic group and the non-autistic group. Compared to the non-autistic group, autistic adults with high perceived stress and poor sleep quality have statistically significant worse quality of life.
Table 4.
Unstandardized and Standardized Coefficients from the Regression of Quality of Life on the Interactions between Diagnosis, Sleep Quality and Perceived Stress
| Predictor Variables | Interaction Model | Three-way Interaction Model | ||
|---|---|---|---|---|
|
| ||||
| B (SE) | β | B (SE) | β | |
|
| ||||
| Autism Diagnosis | −15.45 (18.82) | −0.301 | −24.95*** (3.318) | −0.487 |
| Age (in years) | −0.195 (.231) | −0.083 | −0.175 (.209) | −0.061 |
| Sex (ref: women) | ||||
| Men | −3.575 (4.133) | −0.259 | −3.720 (3.728) | −0.342 |
| Full Scale IQ | 0.0842 (.0934) | 0.0925 | 0.0350 (.0843) | 0.112 |
| Perceived Stress | −1.085 (.707) | −0.292 | 0.861 (.6 3) | −0.201 |
| Sleep Quality | −2.774** (.807) | −0.650 | 7.111** (2.427) | −0.248 |
| Autism X Sleep Quality | 2.017 (1.007) | 0.473 | ||
| Autism X Stress | 0.0369 (.906) | 0.009 | ||
| Autism X Sleep Quality X Stress | −0.311** (.0938) | −0.144 | ||
| Constant | 102.5*** (18.89) | 3.v 19 | 1 69.82*** (15.38) | 0.643 |
| Observations | 64 | 64 | ||
SE: Standard error of the regression coefficient
β: Standardized beta
p < 0.05
p < 0.01
p < 0.001
Figure 1. Adjusted Predictions of Quality of Life with 95% Confidence Intervals.
Note: Higher scores on the PSQI indicate worse sleep quality (0–20 on the x-axis). Higher scores on the PSS indicate worse levels of perceived stress (10–30 in the key). Higher scores on the WHOQOL, indicate higher quality of life.
In Figure 1, higher scores on the PSQI indicate worse sleep quality (0–20 on the x-axis). Similarly, higher scores on the PSS indicate worse levels of perceived stress (10–30 in the key). Higher scores on the WHOQOL, however, indicate higher quality of life. The plot compares the combined associations between stress and sleep quality on predictions of quality of life for autistic adults vs non-autistic adults. The findings displayed in the plot indicate that stress and sleep quality have a significant combined effect on quality of life for both autistic adults and non-autistic adults. The figure demonstrates a similar pattern for all participants in that high levels of stress and poor sleep quality are associated with worse quality of life. However, quality of life is worse for autistic adults as a result of high stress and poor sleep. Autistic adults with the highest stress levels (stress=30) and worst sleep quality (sleep quality=20), have worse quality of life than non-autistic adults with similar stress levels and sleep quality.
Sleep Quality Domains and Quality of Life Domains
We conducted post-hoc exploratory analyses of the relationships between quality of life and the seven sleep quality domains in our sample of autistic adults (N=40). These results are displayed in Table 5. These analyses measure the strength and direction of associations between each subscale domain and quality of life. Results in our sample of autistic adults indicate that sleep duration has the strongest negative association with quality of life such that autistic adults with decreased sleep duration had worse quality of life. Sleep duration was measured in number of hours of sleep obtained per night, with decreased sleep duration any time less than seven hours.
Table 5.
Post-Hoc Multiple Pairwise Correlational Comparisons of Sleep Quality Components and Quality of Life for Autistic Adults
| Variables | Quality of Life |
|---|---|
|
| |
| Sleep Duration | −0.4575* |
| Sleep Disturbance | −0.2269 |
| Sleep Latency | −0.1047 |
| Daytime Dysfunction due to Sleepiness | −0.0516 |
| Sleep Efficiency | −0.1036 |
| Overall Sleep Quality | 0.1374 |
| Sleep Medication Use | −0.3388* |
p<0.05
Discussion
This study examined the relationship among sleep quality, perceived stress, and quality of life for autistic adults. An association between sleep quality and quality of life in the typically developing population is well-documented, with poor sleep contributing to worsened quality of life, as well as decreased physical and mental health (Liu et al, 2018; Okun, 2011; Steptoe et al., 2008). Research has consistently suggested that both sleep quality and quality of life are poor in autistic people, yet whether these factors contribute to one another has needed further analysis. Therefore, we hypothesized that autistic adults would have worse sleep quality than non-autistic adults, and that there would be a similar negative association between sleep quality and quality of life for autistic adults as has been identified in non-autistic adults in previous research.
Our findings indicate that autistic adults do experience significantly worse sleep quality compared to non-autistic adults, and that this difference is moderate to large. This builds on the emerging body of research indicating that autistic adults are at risk of a range of physical health challenges, including sleep problems (Goldman et al., 2017; Lawson et al., 2020). It also suggests that sleep problems that are well-documented among autistic children do continue into adulthood.
Further, through use of our standardized regression coefficients as effect size indices (Nieminen et al., 2013), our models demonstrate a large effect in the relationships between autism diagnosis and quality of life, as well as sleep quality and quality of life. Our findings demonstrate a statistically significant association between sleep quality on quality of life for all participants in the study. Findings of our exploratory interaction analyses do not demonstrate a combined significant association between autism diagnosis and sleep quality on quality of life, despite the fact sleep quality was much poorer in the autistic group. Sleep quality is worse in autistic adults; however, poor sleep is negatively associated with quality of life for everyone, not necessarily more so in autistic adults. Our post-hoc analyses do indicate, however, that a specific sleep quality domain, sleep duration, is negatively associated with quality of life for autistic adults. Autistic adults’ ability to sleep for an appropriate duration may specifically and uniquely affect their quality of life. With findings demonstrating that our autistic group has worse quality of life and poorer sleep, our study tested the relationships among sleep quality, perceived stress, and quality of life. We found that perceived stress and sleep quality do have a significant, combined association with quality of life for autistic adults. Quality of life for autistic adults with poor sleep quality and high levels of stress is worse than for non-autistic adults with similarly poor sleep and stress.
Findings suggest that the interaction between sleep quality, perceived stress, and quality of life seen in the general population also applies to autistic adults. Findings also help us to better understand the modifiable correlates of quality of life for autistic adults and develop and/or adapt interventions accordingly. Although our analyses were correlational and did not test causal mechanisms, further research should investigate whether sleep problems are causally linked to worse quality of life and health problems in autistic people, providing a possible avenue for intervention. Further, research should examine the association between diagnosed sleep disorders and illness morbidity in large, representative samples of autistic adults.
Limitations
Findings should be interpreted within the context of this study’s limitations. Our sample was relatively small and only powered to detect large effects. Small sample sizes increase the likelihood of a Type II error which can skew results and/or over or underestimate effect size. We also chose to only conduct post-hoc analyses on sleep quality domains and quality of life in order to conserve power; thus results of post-hoc analyses should be interpreted as preliminary and exploratory. A lack of statistical significance in our study may be a result of our small sample size, rather than a lack of effect. Similarly, a statistically significant result may represent a Type II error. Further, the sample is a relatively limited sample that is homogenous in terms of race, ethnicity, and IQ; thus, results are not generalizable to the entire population of autistic adults. Future research should include larger, population-level samples of autistic and non-autistic adults to ensure generalizability of findings. Additionally, our use of self-report measures could have potentially resulted in self-report bias. Finally, data are cross-sectional, therefore this study demonstrates correlational rather than causal relationships as mentioned prior. Despite these limitations, our findings contribute to a growing body of literature on sleep quality and its correlates in autistic adults.
Implications
The findings of this study suggest that interventions that teach generalizable skills to assist autistic adults in lowering their stress and sleeping better may help to improve their quality of life. Sleep quality interventions might involve behavioral interventions, educational programming, or pharmacological treatment. These interventions could potentially lead to better clinical outcomes, including decreased risk of physical and mental health problems. Furthermore, they have the potential to improve quality of life, overall well-being, and life expectancy for the growing population of autistic adults. Our findings also suggest that autistic adults should be evaluated for undiagnosed sleep disorders and poor sleep quality. Developing and adapting appropriate treatment options for sleep disorders in autistic adults should be prioritized in future research.
Highlights.
Autistic adults report worse sleep quality compared to non-autistic adults
Poor sleep quality is associated with lower quality of life for autistic and non-autistic adults
Quality of life for autistic adults with poor sleep quality and high levels of stress is worse than for non-autistic adults with similarly poor sleep and stress
Interventions that teach generalizable skills to assist autistic adults in lowering their stress and sleeping better may help to improve their quality of life
Acknowledgments
This study was supported by grants from the National Institutes Health (MH-85851, MH-95783, RR-24154, HD-55748; U54HD090256; UL1TR002373; KL2TR002374; KL2TR000428); Autism Speaks (5703 and 8568); Department of Defense (AR100344); and Pennsylvania Department of Health.
Footnotes
Conflict of Interest
The authors declare no conficts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allik H, Larsson J-O, & Smedje H (2006). Health-related quality of life in parents of school-age children with Asperger syndrome or high-functioning autism. Health and Quality of Life Outcomes, 4(1), 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders: DSM-5 (5th edition). [Google Scholar]
- Ayres M, Parr JR, Rodgers J, Mason D, Avery L, & Flynn D (2018). A systematic review of quality of life of adults on the autism spectrum. Autism: The International Journal of Research and Practice, 22(7), 774–783. [DOI] [PubMed] [Google Scholar]
- Baker EK, & Richdale AL (2015). Sleep patterns in adults with a diagnosis of high-functioning autism spectrum disorder. Sleep, 38(11), 1765–1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballester P, Martínez MJ, Javaloyes A, Inda M.-d.-M., Fernández N, Gázquez P, Aguilar V, Pérez A, Hernández L, Richdale AL, & Peiró AM (2019). Sleep problems in adults with autism spectrum disorder and intellectual disability. Autism Research, 12(1), 66–79. [DOI] [PubMed] [Google Scholar]
- Bishop-Fitzpatrick L, Hong J, Smith LE, Makuch RA, Greenberg JS, & Mailick MR (2016). Characterizing objective quality of life and normative outcomes in adults with autism spectrum disorder: An exploratory latent class analysis. Journal of Autism and Developmental Disorders, 46(8), 2707–2719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop-Fitzpatrick L, Mazefsky CA, & Eack SM (2018). The combined impact of social support and perceived stress on quality of life in adults with autism spectrum disorder and without intellectual disability. Autism: The International Journal of Research and Practice, 22(6), 703–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourgeron T (2007). The possible interplay of synaptic and clock genes in autism spectrum disorders. Cold Spring Harbor Symposia on Quantitative Biology, 72, 645–654. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, & Kupfer DJ (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213. [DOI] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences (2nd edition). Hillside NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Cohen S, & Janicki-Deverts D (2012). Who’s stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 2009. Journal of Applied Social Psychology, 42(6), 1320–1334. [Google Scholar]
- Couturier JL, Speechley KN, Steele M, Norman R, Stringer B, & Nicolson R (2005). Parental perception of sleep problems in children of normal intelligence with pervasive developmental disorders: Prevalence, severity, and pattern. Journal of the American Academy of Child and Adolescent Psychiatry, 44(8), 815–822. [DOI] [PubMed] [Google Scholar]
- Croen LA, Zerbo O, Qian Y, Massolo ML, Rich S, Sidney S, & Kripke C (2015). The health status of adults on the autism spectrum. Autism: The International Journal of Research and Practice, 19(7), 814–823. [DOI] [PubMed] [Google Scholar]
- Deserno MK, Borsboom D, Begeer S, Agelink van Rentergem JA, Mataw K, & Geurts HM (2019). Sleep determines quality of life in autistic adults: A longitudinal study. Autism Research: The Official Journal of the International Society for Autism Research, 12(5), 794–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [Reference removed for blind review]
- Espie CA, Emsley R, Kyle SD, Gordon C, Drake CL, Siriwardena AN, et al. (2019). Effect of digital cognitive behavioral therapy for insomnia on health, psychological well-being, and sleep-related quality of life: a randomized clinical trial. JAMA Psychiatry, 76(1), 21–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang AG, & Buchner A (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. [DOI] [PubMed] [Google Scholar]
- First M, Williams J, Spitzer R, & Gibbon M (2002). Structured clinical interview for the DSM-IV-TR Axis I Disorders, research version (patient edition). New York: Biometrics Research, New York State Psychiatric Institute. [Google Scholar]
- Goldman SE, Alder ML, Burgess HJ, Corbett BA, Hundley R, Wofford D, Fawkes DB, Wang L, Laudenslager ML, & Malow BA (2017). Characterizing sleep in adolescents and adults with autism spectrum disorders. Journal of Autism and Developmental Disorders, 47(6), 1682–1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirvikoski T, & Blomqvist M (2014). High self-perceived stress and poor coping in intellectually able adults with autism spectrum disorder. Autism: The International Journal of Research and Practice, 19(6), 752–757. [DOI] [PubMed] [Google Scholar]
- Hirvikoski T, Mittendorfer-Rutz E, Boman M, Larsson H, Lichtenstein P, & Bölte S (2016). Premature mortality in autism spectrum disorder. The British Journal of Psychiatry : The Journal of Mental Science, 208(3), 232–238. [DOI] [PubMed] [Google Scholar]
- Hollocks MJ, Lerh JW, Magiati I, Meiser-Stedman R, & Brugha TS (2019). Anxiety and depression in adults with autism spectrum disorder: a systematic review and meta-analysis. Psychological Medicine, 49(4), 559–572. [DOI] [PubMed] [Google Scholar]
- Hong J, Bishop-Fitzpatrick L, Smith LE, Greenberg JS, & Mailick MR (2016). Factors associated with subjective quality of life of adults with autism spectrum disorder: Self-report versus maternal reports. Journal of Autism and Developmental Disorders, 46(4), 1368–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamp-Becker I, Schröder J, Remschmidt H, & Bachmann CJ (2010). Health-related quality of life in adolescents and young adults with high functioning autism-spectrum disorder. GMS Psycho-Social-Medicine, 7, Doc03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khanna R, Jariwala-Parikh K, West-Strum D, & Mahabaleshwarkar R (2014). Health-related quality of life and its determinants among adults with autism. Research in Autism Spectrum Disorders, 8(3), 157–167. [Google Scholar]
- Kulman G, Lissoni P, Rovelli F, Roselli MG, Brivio F, & Sequeri P (2000). Evidence of pineal endocrine hypofunction in autistic children. Neuro Endocrinology Letters, 21(1), 31–34. [PubMed] [Google Scholar]
- Lawson LP, Richdale AL, Haschek A, Flower RL, Vartuli J, Arnold SR, & Trollor JN (2020). Cross-sectional and longitudinal predictors of quality of life in autistic individuals from adolescence to adulthood: The role of mental health and sleep quality. Autism: The International Journal of Research and Practice, 24(4), 954–967. [DOI] [PubMed] [Google Scholar]
- LeBlanc M, Beaulieu-Bonneau S, Merette C, Savard J, Ivers H, & Morin CM (2007). Psychological and health-related quality of life factors associated with insomnia in a population-based sample. Journal of Psychosomatic Research, 63(2), 157–166. [DOI] [PubMed] [Google Scholar]
- Liu F, Zhang H, Liu Y, Sun X, Yin Z, Li H, Deng K, Zhao Y, Wang B, Ren Y, Zhang L, Zhou J, Han C, Liu X, Zhang D, Chen G, Hong S, Wang C, Hu D, Zhang M. (2018). Sleep duration interacts with lifestyle risk factors and health status to alter risk of all-cause mortality: The rural Chinese cohort study. Journal of Clinical Sleep Medicine; 14(5), 857–865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook EH Jr, Leventhal BL, DiLavore PC, Pickles A, & Rutter M (2000). The autism diagnostic observation schedule-generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 30(3), 205–223. [PubMed] [Google Scholar]
- Lord C, Rutter M, & Le Couteur A (1994). Autism Diagnostic Interview-Revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders, 24(5), 659–685. [DOI] [PubMed] [Google Scholar]
- Malow BA, Marzec ML, McGrew SG, Wang L, Henderson LM, & Stone WL (2006). Characterizing sleep in children with autism spectrum disorders: A multidimensional approach. Sleep, 29(12), 1563–1571. [DOI] [PubMed] [Google Scholar]
- Nadeau JM, Arnold EB, Keene AC, Collier AB, Lewin AB, Murphy TK, & Storch EA (2015). Frequency and clinical correlates of sleep-related problems among anxious youth with autism spectrum disorders. Child Psychiatry & Human Development, 46(4), 558–566. [DOI] [PubMed] [Google Scholar]
- Nieminen P, Lehtiniemi H, Vähäkangas K, Huusko A, & Rautio A (2013). Standardised regression coefficient as an effect size index in summarising findings in epidemiological studies. Epidemiology Biostatistics and Public Health, 10(4), 4–15. [Google Scholar]
- Okun ML (2011). Biological consequences of disturbed sleep: Important mediators of health? Japanese Psychological Research, 53(2), 163–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polimeni MA, Richdale AL, & Francis AJ (2005). A survey of sleep problems in autism, Asperger’s disorder and typically developing children. Journal of Intellectual Disability Research, 49(Pt 4), 260–268. [DOI] [PubMed] [Google Scholar]
- Richdale AL (1999). Sleep problems in autism: Prevalence, cause, and intervention. Developmental Medicine and Child Neurology, 41(1), 60–66. [DOI] [PubMed] [Google Scholar]
- Richdale AL, & Schreck KA (2009). Sleep problems in autism spectrum disorders: Prevalence, nature, & possible biopsychosocial aetiologies. Sleep Medicine Reviews, 13(6), 403–411. [DOI] [PubMed] [Google Scholar]
- Schafer JL, & Graham JW (2002). Missing data: Our view of the state of the art. Psychological Methods, 7(2), 147–177. [PubMed] [Google Scholar]
- Schreck KA (2021). Sleep quantity and quality as predictors of behavior and mental health issues for children and adolescents with autism. Research in Autism Spectrum Disorders, 84, 101767. [Google Scholar]
- Schreck KA, & Richdale AL (2020). Sleep problems, behavior, and psychopathology in autism: inter-relationships across the lifespan. Current Opinion in Psychology, 34, 105–111. [DOI] [PubMed] [Google Scholar]
- Souders MC, Mason TBA, Valladares O, Bucan M, Levy SE, Mandell DS, Weaver TE, & Pinto-Martin J (2009). Sleep behaviors and sleep quality in children with autism spectrum disorders. Sleep, 32(12), 1566–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, O’Donnell K, Marmot M, & Wardle J (2008). Positive affect, psychological well-being, and good sleep. Journal of Psychosomatic Research, 64(4), 409–415. [DOI] [PubMed] [Google Scholar]
- Tordjman S, Anderson GM, Pichard N, Charbuy H, & Touitou Y (2005). Nocturnal excretion of 6-sulphatoxymelatonin in children and adolescents with autistic disorder. Biological Psychiatry, 57(2), 134–138. [DOI] [PubMed] [Google Scholar]
- Tzischinsky O, Meiri G, Manelis L, Bar-Sinai A, Flusser H, Michaelovski A, Zivan O, Ilan M, Faroy M, Menashe I, & Dinstein I (2018). Sleep disturbances are associated with specific sensory sensitivities in children with autism. Molecular Autism, 9(1), 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uren J, Richdale AL, Cotton SM, & Whitehouse A (2019). Sleep problems and anxiety from 2 to 8 years and the influence of autistic traits: A longitudinal study. European Child & Adolescent Psychiatry, 28(8), 1117–1127. [DOI] [PubMed] [Google Scholar]
- van Heijst BF, & Geurts HM (2015). Quality of life in autism across the lifespan: A meta-analysis. Autism: The International Journal of Research and Practice, 19(2), 158–167. [DOI] [PubMed] [Google Scholar]
- van Steensel FJA, Bögels SM, & Perrin S (2011). Anxiety disorders in children and adolescents with autistic spectrum disorders: A meta-analysis. Clinical Child and Family Psychology Review, 14(3), 302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D (2008). Wechsler Adult Intelligence Scale (WAIS-IV) (4th edition). San Antonio, TX: Harcourt Assessment. [Google Scholar]
- Whitney DG, Shapiro DN, Peterson MD, & Warschausky SA (2019). Factors associated with depression and anxiety in children with intellectual disabilities. Journal of Intellectual Disability Research, 63(5), 408–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHOQOL Group (1998) Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychological Medicine 28: 551–558. [DOI] [PubMed] [Google Scholar]