Abstract
Physical fatigability, or susceptibility to physical fatigue, is strongly associated with aging, disease, and disability. Over the lifecourse, personality traits are also connected to numerous age-related vulnerabilities and resistance—yet, their longitudinal association with fatigability remains unknown. Well-functioning community-dwelling volunteers aged ≥ 50 (N = 995) from the Baltimore Longitudinal Study of Aging, were assessed over an average of 2 years on personality traits (NEO-PI-R; openness, conscientiousness, extraversion, agreeableness, and neuroticism) and perceived fatigability (Borg Rating of Perceived Exertion (RPE) after a 5-minute slow treadmill walk; 6 (low) to 20 (high) exertion). Linear and multinomial logistic regression models examined cross-sectional associations (treating fatigability continuously and by RPE category: low (6-7), intermediate (8-9), and high (10+). Generalized estimating equations (GEE) tested longitudinal associations. All models were adjusted for demographics and comorbid conditions. In cross-sectional models, openness (β= −.09 RPE (SE=.03); p <.01), conscientiousness (β= −.07(.03); p <.05), and extraversion (β= −.10 (.03); p <.01) were negatively associated with fatigability. In parallel, lower openness (OR: .98, 95% CI: .96-1.00), conscientiousness (OR: .98, 95% CI: .96-1.00), and extraversion (OR: .97, 95% CI: .95-.99) corresponded with higher odds of having high versus low fatigability. In longitudinal models (mean follow-up time 2±2 years), openness, conscientiousness, and extraversion associations remained significant and did not change over time (trait x year p-values > 0.34). Together, findings suggest that personality plays a role in the perceived tolerance of fatigue in well-functioning older adults.
Keywords: Fatigue, Vitality, Big Five, Normative Aging, Individual Differences, Baltimore Longitudinal Study of Aging
Fatigue is a well-documented health concern for many older adults and their families that restricts activities of daily living (ADLs), reduces quality of life, and is associated with increased mortality (Moreh et al., 2010). Although fatigue may be a signifier of decline – capturing and leveraging the experience has been notoriously difficult as individuals tend to equilibrate their activity (e.g., slow down or bypass) to diminish or avoid fatigue, particularly in response to age-related functional limitations (Eldadah, 2010). Likewise, the etiology of fatigue is convoluted with aging as factors such as decreased physical capacities with normative aging and presence of diseases – as cardiovascular and cancers are concurrently associated with easily becoming fatigued (Avlund, 2010; Eldadah, 2010; Gresham et al., 2018; Harvey et al., 2008; Zengarini et al., 2015). Correspondingly, perceived fatigability is a construct created by The National Institute of Aging in 2010 during the Bedside to Bench Research Conference – and honed and validated by subsequent public health studies – to better use the fatigue experience in relation to a standardized workload (i.e., subjective rates of exertion after a 5-minute slow treadmill task; Simonsick et al., 2014). As a result, from over a decade of interdisciplinary science – perceived fatigability is burgeoning as a promising prognostic indicator of phenotypic aging, captured with a self-report of an individual’s whole-body feeling of tiredness or exertion [for details of the distinction between perceived fatigability and performance fatigability see Schrack et al., 2020].
In well-functioning older adults, higher perceived fatigability (i.e., feeling more significant levels of exhaustion after completing slow treadmill walk) has been associated with lower objective physical activity (Richardson et al., 2015; Wanigatunga, Simonsick, et al., 2018), subjective and performance-based mobility (Simonsick et al., 2016, 2018), and worse inflammatory biomarker levels (Cooper et al., 2019; Wanigatunga, Varadhan, et al., 2018). High perceived fatigability is also more prevalent in those with a history of disease including preclinical cardiovascular disease (Qiao et al., 2019), peripheral artery disease (Martinez-Amezcua et al., 2018), cancer (Gresham et al., 2018), cognition (Salerno et al., 2019), and sleep (Alfini et al., 2020). Although several popular adages:
“It takes a much energy to wish as it does to plan” - Eleanor Roosevelt, American Political Figure “Our fatigue is often caused not by work, but by worry, frustration and resentment” - Dale Carnegie, American Writer
“Age is not measured by years. Nature does not equally distribute energy. Some people are born old and tired while others are going strong at seventy” - Dorothy Thompson, American Journalist
—support the link between individual differences and perceived fatigability—the empirical associations remain relatively unknown.
Personality traits are dimensions of individual differences in tendencies to illustrate consistent patterns of thoughts, feelings, and actions (Costa & McCrae, 1992). Over the lifecourse, personality traits are postulated to direct people towards engaging in behaviors that either increase or decrease their cardiovascular, strength, and mental capacities (Shanahan et al., 2014; Terranciano et al., 2013). For instance, people who are highly extraverted and open to experience may engage in more social activities over their lifetimes (i.e., out and about), therefore increasing their physical reserves; furthermore, people who are low in conscientiousness and high on neuroticism may rarely engage in scheduled health behavior activities (i.e., there is never a good time to go for a walk).
The Five-Factor Model of Personality (“Big 5”) is the most empirically backed framework, by decades of research (Costa & McCrae, 1992), which includes the following five traits: 1) openness, 2) conscientiousness, 3) extraversion, 4) agreeableness, and 5) neuroticism. Broadly, lower openness, conscientiousness, extraversion, and agreeableness are generally associated with adverse health outcomes, while lower neuroticism has been associated with positive outcomes. Correspondingly, tendencies towards engaging in adaptive or maladaptive health behaviors over the lifecourse have led to various works finding that each of the five personality traits are linked to numerous biomarkers and health outcomes that are closely related to perceived fatigability—including, inflammation (Luchetti et al., 2014), aerobic capacity (Terracciano et al., 2013), muscle strength (Tolea et al., 2012), physical activity (Tolea et al., 2012), functional limitations (Goodwin & Friedman, 2006), frailty (Stephan et al., 2017), mortality risk (Graham et al., 2017), Alzheimer’s disease (Terracciano et al., 2017), and vitality (Ryan & Frederick, 1997).
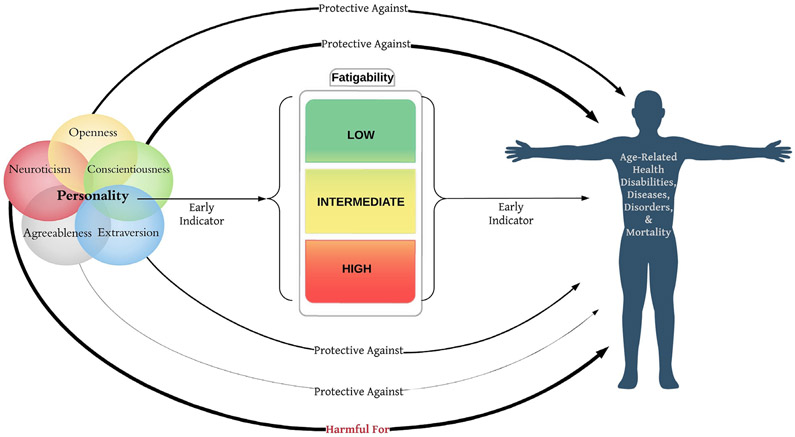
In this study, we examine whether differences in the Big 5 personality traits are linked to proneness to fatigability (i.e., fatigue in response to a physical task) during the aging process. More precisely, Figure 1 illustrates our hypotheses that openness, conscientiousness, extraversion, and agreeableness are negatively associated with perceived fatigability, while neuroticism is positively associated with perceived fatigability. Our hypotheses are based on evidence that personality is linked to cardiovascular fitness and strength involved in performing physical tasks, as well as psychological resilience and perception of exhaustion (Terracciano et al., 2013; Tolea et al., 2012). Although we do not directly study the health behaviors associated with the Big 5 and fatigue – our study aims to examine the linkage between the Big 5 personality traits and perceived fatigability as a foundational step towards testing the individual differences and health outcome model in Figure 1.
Figure 1.
Conceptual and empirical links between high expression of each personality trait, fatigability, and age-related health outcomes. Each pathway represents an association between a specific personality trait with age-related health outcomes (e.g., high on conscientiousness→low fatigability→protective against age-related disability). Separately, personality and fatigability are shown to be early indicators of age-related disabilities. Evidence suggests personality is relatively stable after age 30, thus finding links between fatigability and personality—assessment and monitoring of certain personality traits may help predict functional vulnerabilities earlier in the lifespan. The thickness of lines symbolizes the degree of association found in the literature.
We use data from the Baltimore Longitudinal Study of Aging (BLSA) to assess both cross-sectional and longitudinal associations between each major personality trait and perceived fatigability. Findings from this study inform researchers and medical professionals of the individual-level differences that may signify vulnerability or resistance to fatigability. Since high fatigability tends to precede or coincide with many age-related health outcomes (Gresham et al., 2018; Salerno et al., 2019; Simonsick et al., 2014; Wanigatunga, Simonsick, et al., 2018)—evaluating personality trait differences leads to the better identification of higher-risk individuals and more efficient or appropriately tailored interventions to prevent or manage age-related morbidity and disability (Conrod et al., 2013; Kolanowski, Litaker, Buettner, Moeller, & Costa Jr., 2011; Rouch et al., 2018).
Methods
Study Design and Participants
The BLSA is a continuous enrollment cohort study of normative aging conducted by the National Institute on Aging (NIA) Intramural Research Program. BLSA participants are community-dwelling volunteers who are free from cognitive impairment, functional limitations, chronic diseases [except hypertension], and with no cancer history within the past ten years at the time of enrollment. Depending on age, participants attend regularly scheduled evaluations over a 3-day visit every 1-4 years (Simonsick et al., 2016). Trained and certified staff administer all assessments following standardized protocols. The National Institute for Environmental Health Sciences Internal Review Board approved all study protocols.
Longitudinal data for this study were collected between 2008 when fatigability was introduced and 2016 covering 1,482 participants. After exclusion for: 1) age less than 50 years (n = 231) and 2) absence of concurrent personality data (n = 21) or fatigability data (n = 235), the final analytic sample was 995.
Personality Assessment
The Revised NEO Personality Inventory (NEO-PI-R; (Costa & McCrae, 1992); (Terracciano et al., 2017)), is a 240-item, self-administered questionnaire that measures: 1) openness – the tendency to seek and be receptive to novel ideas, values, and behaviors, 2) conscientiousness – the tendency to be goal-directed, dependable, and premeditative, 3) extraversion – the tendency to be sociable, energetic, and assertive, 4) agreeableness – the tendency to be altruistic, compliant, and trusting, and 5) neuroticism – the tendency to worry, be self-conscious, and feel negative emotions. Raw scores for each personality trait were standardized to T-scores (M = 50, SD = 10) using combined-sex norms for adults reported in the NEO Manual (Costa & McCrae, 1992). The NEO-PI-R in the BLSA sample shows high congruence with normative structure, high internal consistency and test-retest correlations over a mean interval of 10 years (Terracciano et al., 2006).
Perceived Fatigability
Participants performed a standardized slow-paced walk (0.67 m/s; 1.5 mph) for 5 minutes on a treadmill at 0% grade. Immediately after completion, participants were instructed to rate their perceived exertion using the Borg Rating of Perceived Exertion scale (RPE) ranging from 6 to 20 where 6 = no exertion at all, 9 = very light, 11 = light, 12 = somewhat hard, and 20 = maximal exertion (Borg, 1990). Perceived fatigability was measured on a continuous scale, with higher scores on the RPE indicating higher perceived fatigability. As previously published (Wanigatunga et al., 2018), perceived fatigability was also categorized into three groups as follows: low (RPE = 6-7), intermediate (RPE = 8-9), and high (RPE = 10+).
Covariates
Demographic covariates included self-reported age, sex, race. Weight, height, and body mass index (BMI; weight and height kg/m2) were measured in the clinic. At the clinic, a health history interview was used to captured comorbidities of cardiovascular disease, hypertension, hyperlipidemia, cerebrovascular disease, diabetes, cancer, and osteoarthritis; a subsequent comorbidity conditions index was created through the summation of each morbidity occurrence (0, 1, and 2+).
Statistical Analyses
Baseline associations between each personality trait and perceived fatigability as both a continuous and categorical measure were examined using linear and multinomial logistic regression, respectively. Continuous longitudinal associations between each personality trait and perceived fatigability were evaluated using generalized estimating equations (GEE), using an interaction term between each personality trait and time (years). All GEE analyses used a Gaussian distribution with identity link and an exchangeable correlation matrix for estimation.
Analyses were modeled in a successive order to test the unique contributions and alterative explanatory factors between personality traits and fatigability. Initial models were unadjusted for regressions or time adjusted for GEE analyses. Subsequently, demographics (age, sex, race), then BMI, and lastly comorbidities were entered at each step. All final models were adjusted for age, sex, race, BMI, and comorbidities. The interaction term of Time was removed from covariate-adjusted models due to its non-significance (NS). Two-tailed hypothesis testing was at an alpha level of 0.05. Analyses were conducted using Stata (v15.1; Stata Corporation, College Station, TX).
Results
Baseline participant characteristics are shown by fatigability category in Table 1. The study sample was 52% women and 69% white with a mean age of 70.3 (SD = 9.9), mean BMI of 27 (SD = 4.5) kg/m2, 65% with two or more comorbidities, and a mean RPE of 8.5 (SD = 2.3). Those with higher fatigability tended to be older, female, have a higher BMI, and were more likely to have a history of diabetes and osteoarthritis. Regarding personality, those with higher fatigability had lower scores for openness, conscientiousness, and extraversion, and higher scores for neuroticism.
Table 1.
Participant Characteristics Across Categories of Perceived Fatigability (N = 995)
|
Low (RPE: 6-7; n = 460) |
Intermediate (RPE: 8-9; n = 268) |
High (RPE: 10+; n = 267) |
P Value | |
|---|---|---|---|---|
| Age (years), mean (SD) | 67.3 (9.4) | 70.9 (9.7) | 74.7 (9.3) | <.001 |
| Female, n (%) | 226 (49.1) | 128 (47.8) | 162 (60.7) | <.01 |
| White, n (%) | 320 (69.6) | 197 (73.5) | 178 (66.7) | .223 |
| BMI (kg/m2), mean (SD) | 26.6 (4.2) | 27.4 (4.6) | 27.9 (4.8) | <.001 |
| Two or more comorbidities, n (%) | 311 (67.6) | 202 (75.4) | 196 (73.4) | .055 |
| Cardiovascular disease, n (%) | 40 (8.7) | 30 (11.2) | 38 (14.2) | .067 |
| Hypertension, n (%) | 198 (43.0) | 137 (51.1) | 135 (50.6) | .049 |
| Hyperlipidemia, n (%) | 270 (58.7) | 178 (66.4) | 160 (59.9) | .107 |
| Cerebrovascular disease, n (%) | 11 (2.4) | 12 (4.5) | 17 (6.4) | .028 |
| Diabetes, n (%) | 64 (13.9) | 51 (19.0) | 60 (22.5) | .011 |
| Cancer, n (%) | 134 (29.1) | 97 (36.2) | 84 (31.5) | .141 |
| Osteoarthritis, n (%) | 227 (49.4) | 137 (51.1) | 161 (60.3) | .014 |
| Borg’s Rate of Perceived Exertiona | 6.7 (0.5) | 8.8 (0.4) | 11.9 (1.7) | ---- |
| Personality Traitsb | ||||
| Openness, mean (SD) | 54.6 (10.5) | 52.3 (10.0) | 52.3 (9.6) | <.001 |
| Conscientiousness, mean (SD) | 53.0 (9.9) | 50.7 (10.0) | 50.4 (9.3) | <.001 |
| Extraversion, mean (SD) | 49.8 (9.2) | 49.1 (9.3) | 47.5 (8.8) | .001 |
| Agreeableness, mean (SD) | 52.3 (9.7) | 51.9 (10.3) | 52.5 (8.8) | .814 |
| Neuroticism, mean (SD) | 45.6 (8.7) | 46.0 (8.4) | 46.2 (8.2) | .372 |
Notes.
Fatigability based on Borg’s Rate of Perceived Exertion (RPE) score during a 5-minute, 0.67 m/s, 0% grade standardized treadmill walk, scored 6 to 20, higher scores indicate higher perceived fatigability.
Personality Traits were sex normalized from the 240-item NEO-PI-R.
Fully-covariate adjusted linear regression models revealed that openness (β = −.09 (SE =.03; p < .01)), conscientiousness (β = −.07 (SE =.03; p < .05)), and extraversion (β = −.10 (SE=.03; p < .01)) were negatively associated with fatigability, while agreeableness and neuroticism were not (Table 2, Continuous Models). Fully-adjusted multinomial logistic regression models (Table 2, Categorical Models) provided parallel results when comparing either intermediate or high fatigability with low fatigability groups. Notably, participants with lower extraversion were more likely to experience high fatigability (OR: .97, 95% CI: .95-.99)—suggesting that every one-unit higher extraversion was associated with 3% lower odds of being in the high fatigability group. Extraversion did not differentiate the odds of intermediate fatigability as compared to low fatigability (OR: 0.99, 95% CI: .97-1.01).
Table 2.
Baseline Associations Between Personality Traits and Perceived Fatigability (N = 995)
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| standardized beta coefficient (SE) | ||||
| Continuous | ||||
| Openness | −.12 (.03)*** | −.10 (.03)** | −.10 (.03)** | −.09 (.03)** |
| Conscientiousness | −.12 (.03)** | −.09 (.03)** | −.07 (.03)* | −.07 (.03)* |
| Extraversion | −.11 (.03)*** | −.07 (.03)* | −.10 (.03)** | −.10 (.03)** |
| Agreeableness | .02 (.03) | −.04 (.03) | −.03 (.03) | −.03 (.03) |
| Neuroticism | .02 (.03) | .04 (.03) | .03 (.03) | .03 (.03) |
| Categorical | Odds ratio (95% CI), reference: Low Fatigability (n = 460) | |||
| Openness | ||||
| Intermediate | .98 (.96-.99)** | .98 (.96-1.00)** | .98 (.97-1.00)* | .98 (.97-1.00)* |
| High | .98 (.96-.99)** | .98 (.96-.99)** | .98 (.96-1.00)* | .98 (.96-1.00)* |
| Conscientiousness | ||||
| Intermediate | .98 (.96-.99)** | .98 (.96-.99)** | .98 (.96-1.00)* | .98 (.96-.99)* |
| High | .97 (.96-.99)** | .98 (.96-.99)** | .98 (.97-1.00)* | .98 (.96-1.00)* |
| Extraversion | ||||
| Intermediate | .99 (.97-1.00) | 1.00 (.98-1.01) | .99 (.97-1.01) | .99 (.97-1.01) |
| High | .97 (.96-.99)** | .98 (.96-1.00)* | .97 (.95-.99)** | .97 (.95-.99)** |
| Agreeableness | ||||
| Intermediate | .99 (.98-1.01) | .99 (.98-1.01) | .99 (.98-1.01) | .99 (.98-1.01) |
| High | 1.00 (.99-1.02) | .98 (.97-1.00) | .99 (.97-1.00) | .99 (.97-1.01) |
| Neuroticism | ||||
| Intermediate | 1.01 (.99-1.03) | 1.01 (.99-1.03) | 1.01 (.99-1.03) | 1.01 (.99-1.03) |
| High | 1.01 (.99-1.03) | 1.01 (.99-1.03) | 1.01 (.99-1.03) | 1.01 (.99-1.03) |
Notes. Dependent variable = perceived fatigability, intermediate fatigability n = 268
high fatigability n = 267; CI = confidence interval.
Model 1: Unadjusted model
Model 2: Adjusted for age, sex, race
Model 3: Model 2 + adjusted for body mass index
Model 4: Model 3 + adjusted for comorbidities
p <.001
p <.01
p <.05.
Fully adjusted GEEs, over the average follow-up of approximately 2±2 years, detected no association between any trait and longitudinal change in perceived fatigability (year x personality interaction p > 0.34 for all traits; Table 3). However, significant main effects for openness (β = −.08 (SE =.02; p < .001)), conscientiousness (β = −.08 (SE =.02; p < .001)), and extraversion (β = −.10 (SE =.02; p < .001)) on fatigability were detected, reiterating the cross-sectional association. Moreover, a significant main effect for neuroticism (β = .05 RPE (SE =.02; p < .05)) emerged after full covariate adjustment.
Table 3.
Longitudinal Associations Between Personality Traits and Perceived Fatigability (N = 995)
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| standardized beta coefficient (SE) | ||||
| Openness (O) | −.12 (.03)*** | −.09 (.02)*** | −.08 (.02)*** | −.08 (.02)*** |
| Time (T) | −.01 (.02) | −.08 (.02)*** | −.09 (.02)*** | −.09 (.02)*** |
| O x T | .00 (.01) | NS† | NS† | NS† |
| Conscientiousness (C) | −.12 (.03)*** | −.09 (.02)*** | −.08 (.02)*** | −.08 (.02)*** |
| Time (T) | −.00 (.02) | −.08 (.02)*** | .09 (.02)*** | −.09 (.02)*** |
| C x T | .01 (.02) | NS† | NS† | NS† |
| Extraversion (E) | −.11 (.03)*** | −.07 (.02)** | −.10 (.02)*** | −.10 (.02)*** |
| Time (T) | −.00 (.02) | −.08 (.02)*** | −.09 (.02)*** | −.09 (.02)*** |
| E x T | −.02 (.02) | NS† | NS† | NS† |
| Agreeableness (A) | −.00 (.03) | −.05 (.02)* | −.04 (.02) | −.04 (.02) |
| Time (T) | −.00 (.02) | −.08 (.02)*** | −.09 (.02)*** | −.09 (.02)*** |
| A x T | −.03 (.02) | NS† | NS† | NS† |
| Neuroticism (N) | .03 (.03) | .05 (.02)* | .05 (.02)† | .05 (.02)* |
| Time (T) | −.00 (.01) | −.08 (.02)*** | −.09 (.02)*** | −.09 (.02)*** |
| N x T | .01 (.02) | NS† | NS† | NS† |
Notes. Dependent variable = perceived fatigability
Model 1: Adjusted for time (years)
Model 2: Adjusted for age, sex and race
Model 3: Model 2 + adjusted for body mass index
Model 4: Model 3 + adjusted for comorbidities
Interaction term was removed from covariate-adjusted models when not significant (NS)
p <.001
p <.01
p <.05
p >.051.
Discussion
A critical issue when assessing fatigue is the need to consider the context (the activity) and the subjective experience (the person). To untangle this complexity, we used the construct of perceived fatigability to capture the subjective experience of exertion in relation to a standardized physical task controlling for speed and duration. Fatigability was measured by having participants engage in a slow walk (0.67 m/s) on a treadmill for five minutes, then assessing their exertion levels. Personality traits were measured through a comprehensive 240-item assessment (NEO-PI-R Inventory). We assessed personality traits and fatigability over an average of eight-years. Results from linear and binary logistic regression along with multi-level models consistently demonstrated associations between the personality traits of openness, conscientiousness, and extraversion with fatigability. Findings from multi-level models revealed that neuroticism was only significantly linked to perceived fatigability after considering people’s BMI and comorbidities—suggesting the deleterious bidirectional link between higher neuroticism with higher perceived fatigability in individuals with poorer health. Overall, results indicate personality may be a potential psychological underpinning of high fatigability in later life and may have implications for detecting fatigability in the normative aging process and its associated health challenges. Further, personality may play an important role in considering the design and implementation of potential individualized interventions to reduce the burden of fatigue (Conrod et al., 2013; Hirsh et al., 2012).
Our study expands the whole-body work of personality traits by leveraging kinesthetic methodologies to assess the complex individual differences in fatigue experience with aging. A critical issue when assessing fatigue is the need to consider context, individual characteristics, and subjective experience (Schrack et al., 2020). Likewise, our findings strengthen lifecourse ties between people’s earlier life cognitive orientation with energy levels – measured through stamina in later life (Colerick, 1985; Shanahan et al., 2014). We aimed to tackle this issue using the perceived fatigability paradigm to capture the subjective experience of exertion (Borg Rating of Perceived Exertion) in relation to a standardized activity (slow-paced walking). Our results may suggest a need to consider current perceived fatigability measures in the context of personality traits, as reports of exhaustion may be amplified depending on personality profiles. Additional structural equation modeling or measurement studies are needed to delve into the convergent links between kinesthetic methodologies (i.e., movement markers) with more nuanced personality facets (i.e., the components that makeup personality traits). Conducting this work will better target questions such as “what about conscientiousness uniquely drives the association with being exhausted after a treadmill walk (e.g., competence, order, dutifulness, achievement striving, self-discipline, deliberation)?”
Our findings of individuals with poorer health who were higher on neuroticism supports the argument that high neuroticism is one hallmark of “the disease personality,” people more prone to sickness and fatigue (Lahey, 2009). People high on neuroticism also have lower medication adherence following coronary syndrome (Molloy et al., 2012) and increased risk of cardiovascular morbidity, and including low exercise tolerance (Denollet et al., 1996)—suggesting early cardiovascular monitoring and intervention may be most beneficial for downstream fatigability risks. Greater knowledge targeting the individualized psychological tendencies that explain fatigability is a promising approach to enhance early detection of lifecourse trajectories toward functional decline—and may affect people’s ability to perform activities important to daily life.
Earlier Detection and Person-centered Intervention.
Previous research suggests high fatigability is an early marker of age-related disease and disability (Avlund, 2010). Given personality is relatively stable early in the lifespan—beginning in the 30s (Terracciano et al., 2006)—identifying individual psychological trait-level differences may offer a novel avenue for targeting risk reduction interventions to mitigate high fatigability in mid-to-late life. Specifically, detecting risk factors for high fatigability that are both psychological and physiological earlier in the lifespan offers avenues for potential prevention focused on building energetic capacities to maintain quality of life with aging.
Findings from the current work are also consistent with and extend previous research examining personality and frailty (Gale et al., 2017; Stephan et al., 2017), of which one defining feature is fatigue. Specifically, our results provide further evidence that low conscientiousness and low extraversion may partially contribute to a lower reserve against frailty through fatigability. Additionally, our findings add to growing evidence suggesting that individuals high in openness seeking novelty and variety in activity participation are linked to better health outcomes in later life (Terracciano et al., 2006). Lastly, our findings between neuroticism and fatigability also highlight a potential intricate link it may have to experiences of fatigue over time through health conditions such as excessive BMI or comorbidities such as the presence of cardiovascular disease or osteoarthritis.
Implications
Our findings suggest that leveraging personality traits may lead to improved monitoring of and intervening on fatigue-related health decline. For instance, openness may be malleable with non-psychopharmacological intervention in older adults (Roberts et al., 2017)—making it an encouraging modifiable target to decrease the risk of high fatigability. Our associations between openness and fatigability further support facilitating novelty-seeking activities pathway to improve functioning in later life (Chan et al., 2018; Chan & Carlson, 2016; Moored et al., 2018; Wu et al., 2016). Additionally, conscientiousness is also a promising malleable trait that can be fostered through intervention (Magidson et al., 2014). Facilitating higher conscientiousness breeds greater organized disciplined behaviors that favor beneficial downstream effects on energy levels—fostering time to engage in physical activity—leading to cumulative benefits in energy expenditure that maintain muscle strength and aerobic capacity (Nelson, 2007). Lastly, extraversion is positively associated with energy and vigor levels throughout the lifespan (Ryan & Frederick, 1997), and an innate facet of extraversion (activity; Costa & McCrae, 1992). Further longitudinal investigation that parses the six facets of extraversion (e.g., warmth, gregariousness, assertiveness, activity, excitement seeking, and positive emotions) and their link to perceived fatigability is needed to gain a better understanding of what about extraversion predicts physical perceived fatigability (i.e., energy capacities).
Strengths and Limitations
Strengths of our study include the use of a large sample size, repeated measures of personality and fatigability, a comprehensive assessment of personality, advanced methodology to capture perceived fatigability, and comprehensive models that account for demographics, behavioral factors, and medical history. However, the generalizability of our results may be limited since BLSA participants tend to be healthier than the general population, in which case, our findings likely underestimate the association between personality traits and fatigability relative to the general aging population. Further, our results suggest no longitudinal change between personality and fatigability: this may be due to the relatively short follow-up (2 years) and the lack of change in either personality or fatigability. More longitudinal research examining personality and fatigability across adulthood is needed to differentiate the trajectories of fatigability with aging. Future mediation analyses between personality traits, behavior, and fatigability are needed to illuminate better causal mechanisms behind personality’s association with the development of fatigability. Future clinical trials may help determine whether identifying personality traits to complement traditional behavior modifications, like increasing physical activity, may enhance the effectiveness of interventions to reduce fatigue and fatigability that occur progressively with aging.
Conclusion
The current study finds evidence that individual-level differences, measured with personality traits, are linked to fatigability levels in middle and later life. Results suggest that people with lower openness, conscientiousness, and extraversion traits are more likely to feel fatigued in response to a physical task. Findings highlight personality traits as potential pieces of the puzzle to explain the complexities between increases in the rate of fatigability associated with aging. Although it is well-established that the depletion of stamina is a part of the normative aging process, our results suggest that being highly open, conscientious, and extraverted may be part of the formula to help maintain one’s energy and vigor longer over the lifecourse.
Acknowledgments
This research was supported by the Intramural Research Program of the National Institute on Aging of the National Institutes of Health. Data used in the analyses were obtained and approved for use from the Baltimore Longitudinal Study of Aging (BLSA), a study performed by the National Institute on Aging Intramural Research Program. BLSA data are available based on request made through the National Institutes of Health website: https://www.blsa.nih.gov/how-apply, and reviewed by The BLSA Sharing Proposal Review Committee. Fatigability analyses were supported by R21AG053198 and P30AG021334. Thomas Chan is supported by T32AG000247, RL5GM118975, and UL1GM118976. Amal A. Wanigatunga is supported by T32AG000247 and P30AG021334. Jennifer A. Schrack is supported by R21AG053198, P30AG021334, and U01AG057545. Antonio Terracciano is supported by R21AG057917 and R01AG053297.
Footnotes
Paul T. Costa receives royalties from the publisher (PAR, Inc.) for the NEO-PI-R. All other authors have no conflict of interest to disclose.
References
- Alfini AJ, Schrack JA, Urbanek JK, Wanigatunga AA, Wanigatunga SK, Zipunnikov V, Ferrucci L, Simonsick EM, & Spira AP (2020). Associations of actigraphic sleep parameters with fatigability in older adults. The Journals of Gerontology: Series A, glaa137. 10.1093/gerona/glaa137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avlund K (2010). Fatigue in older adults: An early indicator of the aging process? Aging Clinical and Experimental Research, 22(2), 100–115. 10.1007/BF03324782 [DOI] [PubMed] [Google Scholar]
- Borg G (1990). Psychophysical scaling with applications in physical work and the perception of exertion. Scandinavian Journal of Work, Environment & Health, 16, 55–58. 10.5271/sjweh.1815 [DOI] [PubMed] [Google Scholar]
- Carlson MC, Parisi JM, Xia J, Xue Q-L, Rebok GW, Bandeen-Roche K, & Fried LP (2012). Lifestyle activities and memory: Variety may be the spice of life. The Women’s Health and Aging Study II. Journal of the International Neuropsychological Society, 18(02), 286–294. 10.1017/S135561771100169X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan T, & Carlson MC (2016). Building upon the CALLA Framework: The intersection of novel problem solving and applied wisdom. Human Development, 59(6), 366–371. 10.1159/000464309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan T, Parisi JM, Moored KD, & Carlson MC (2018). Variety of enriching early-life activities linked to late-life cognitive functioning in urban community-dwelling African Americans. The Journals of Gerontology: Series B. 10.1093/geronb/gby056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colerick EJ (1985). Stamina in later life. Social Science & Medicine, 21(9), 997–1006. 10.1016/0277-9536(85)90421-6 [DOI] [PubMed] [Google Scholar]
- Conrod PJ, O’Leary-Barrett M, Newton N, Topper L, Castellanos-Ryan N, Mackie C, & Girard A (2013). Effectiveness of a selective, personality-targeted prevention program for adolescent alcohol use and misuse: A cluster randomized controlled trial. JAMA Psychiatry, 70(3), 334. 10.1001/jamapsychiatry.2013.651 [DOI] [PubMed] [Google Scholar]
- Cooper R, Popham M, Santanasto AJ, Hardy R, Glynn NW, & Kuh D (2019). Are BMI and inflammatory markers independently associated with physical fatigability in old age? International Journal of Obesity, 43(4), 832–841. 10.1038/s41366-018-0087-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa PT, & McCrae RR (1992). NEO™ Revised NEO) Personality Inventory (NEO PI-R) and the NEO Five-Factor Inventory (NEO-FFI) Professional Manual. Psychological Assessment Resources. Odessa, FL. [Google Scholar]
- Denollet J, Rombouts H, Gillebert TC, Brutsaert DL, Sys SU, Brutsaert DL, & Stroobant N (1996). Personality as independent predictor of long-term mortality in patients with coronary heart disease. The Lancet, 347(8999), 417–421. 10.1016/S0140-6736(96)90007-0 [DOI] [PubMed] [Google Scholar]
- Eldadah BA (2010). Fatigue and fatigability in older adults. Physical Medicine and Rehabilitation, 2(5), 406–413. 10.1016/j.pmrj.2010.03.022 [DOI] [PubMed] [Google Scholar]
- Gale CR, Mõttus R, Deary IJ, Cooper C, & Sayer AA (2017). Personality and risk of frailty: The English Longitudinal Study of Ageing. Annals of Behavioral Medicine, 51(1), 128–136. 10.1007/s12160-016-9833-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin RD, & Friedman HS (2006). Health status and the five-factor personality traits in a nationally representative sample. Journal of Health Psychology, 11(5), 643–654. 10.1177/1359105306066610 [DOI] [PubMed] [Google Scholar]
- Graham EK, Rutsohn JP, Turiano NA, Bendayan R, Batterham PJ, Gerstorf D, Katz MJ, Reynolds CA, Sharp ES, Yoneda TB, Bastarache ED, Elleman LG, Zelinski EM, Johansson B, Kuh D, Barnes LL, Bennett DA, Deeg DJH, Lipton RB, … Mroczek DK (2017). Personality predicts mortality risk: An integrative data analysis of 15 international longitudinal studies. Journal of Research in Personality, 70, 174–186. 10.1016/j.jrp.2017.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gresham G, Dy SM, Zipunnikov V, Browner IS, Studenski SA, Simonsick EM, Ferrucci L, & Schrack JA (2018). Fatigability and endurance performance in cancer survivors: Analyses from the Baltimore Longitudinal Study of Aging: Fatigability in Cancer Survivors. Cancer, 124(6), 1279–1287. 10.1002/cncr.31238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsh JB, Kang SK, & Bodenhausen GV (2012). Personalized persuasion: Tailoring persuasive appeals to recipients’ personality traits. Psychological Science, 23(6), 578–581. 10.1177/0956797611436349 [DOI] [PubMed] [Google Scholar]
- Kolanowski A, Litaker M, Buettner L, Moeller J, & Costa PT Jr. (2011). A randomized clinical trial of theory-based activities for the behavioral symptoms of dementia in nursing home residents: Theory-based activities. Journal of the American Geriatrics Society, 59(6), 1032–1041. 10.1111/j.1532-5415.2011.03449.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB (2009). Public health significance of neuroticism. American Psychologist, 64(4), 241–256. 10.1037/a0015309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luchetti M, Barkley JM, Stephan Y, Terracciano A, & Sutin AR (2014). Five-factor model personality traits and inflammatory markers: New data and a meta-analysis. Psychoneuroendocrinology, 50, 181–193. 10.1016/j.psyneuen.2014.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magidson JF, Roberts BW, Collado-Rodriguez A, & Lejuez CW (2014). Theory-driven intervention for changing personality: Expectancy value theory, behavioral activation, and conscientiousness. Developmental Psychology, 50(5), 1442–1450. 10.1037/a0030583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez-Amezcua P, Matsushita K, Simonsick EM, Ferrucci L, & Schrack JA (2018). Fatigability and functional performance among older adults with low-normal ankle-brachial index: Cross-sectional findings from the Baltimore Longitudinal Study of Aging. Atherosclerosis, 272, 200–206. 10.1016/j.atherosclerosis.2018.03.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molloy GJ, Randall G, Wikman A, Perkins-Porras L, Messerli-Burgy N, & Steptoe A (2012). Type D personality, self-efficacy, and medication adherence following an acute coronary syndrome. Psychosomatic Medicine, 74(1), 100–106. 10.1097/PSY.0b013e31823a5b2f [DOI] [PubMed] [Google Scholar]
- Moored KD, Chan T, Varma VR, Chuang Y-F, Parisi JM, & Carlson MC (2018). Engagement in enriching early-life activities is associated with larger hippocampal and amygdala volumes in community-dwelling older adults. The Journals of Gerontology: Series B. 10.1093/geronb/gby150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreh E, Jacobs JM, & Stessman J (2010). Fatigue, function, and mortality in older adults. The Journals of Gerontology: Series A, 65A(8), 887–895. 10.1093/gerona/glq064 [DOI] [PubMed] [Google Scholar]
- National Institute on Aging (2019). Fatigue in Older Adults. Retrieved May 10, 2019, from https://www.nia.nih.gov/health/fatigue-older-adults [Google Scholar]
- Nelson. (2007). Physical activity and public health in older Adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Circulation, 116(9), 1094–1105. 10.1161/CIRCULATIONAHA.107.185650 [DOI] [PubMed] [Google Scholar]
- Qiao Y, Martinez-Amezcua P, Wanigatunga AA, Urbanek JK, Simonsick EM, Ferrucci L, & Schrack JA (2019). Association between cardiovascular risk and perceived fatigability in mid-to-late life. Journal of the American Heart Association, 8(16). 10.1161/JAHA.119.013049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson CA, Glynn NW, Ferrucci LG, & Mackey DC (2015). Walking energetics, fatigability, and fatigue in older adults: The study of energy and aging pilot. The Journals of Gerontology: Series A, 70(4), 487–494. 10.1093/gerona/glu146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts BW, Luo J, Briley DA, Chow PI, Su R, & Hill PL (2017). A systematic review of personality trait change through intervention. Psychological Bulletin, 143(2), 117–141. 10.1037/bul0000088 [DOI] [PubMed] [Google Scholar]
- Rouch I, Leveque Y, Tillmann B, Trombert B, Getenet JC, Auguste N, Krolak-Salmon P, Laurent B, & Dorey J-M (2018). Personality modulates the efficacy of art intervention on chronic pain in a population of patients with Alzheimer’s Disease. Journal of Alzheimer’s Disease, 63(2), 617–624. 10.3233/JAD-170990 [DOI] [PubMed] [Google Scholar]
- Ryan RM, & Frederick C (1997). On Energy, personality, and health: Subjective vitality as a dynamic reflection of well-being. Journal of Personality, 65(3), 529–565. 10.1111/j.1467-6494.1997.tb00326.x [DOI] [PubMed] [Google Scholar]
- Salerno EA, Wanigatunga AA, An Y, Urbanek JK, Simonsick EM, Ferrucci L, Resnick SM, & Schrack JA (2019). Longitudinal association between perceived fatigability and cognitive function in older adults: Results from the Baltimore Longitudinal Study of Aging. The Journals of Gerontology: Series A, glz287. 10.1093/gerona/glz287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrack JA, Simonsick EM, & Glynn NW (2020). Fatigability: A prognostic indicator of phenotypic aging. The Journals of Gerontology: Series A, 75(9), e63–e66. 10.1093/gerona/glaa185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanahan MJ, Hill PL, Roberts BW, Eccles J, & Friedman HS (2014). Conscientiousness, health, and aging: The life course of personality model. Developmental Psychology, 50(5), 1407–1425. 10.1037/a0031130 [DOI] [PubMed] [Google Scholar]
- Simonsick EM, Glynn NW, Jerome GJ, Shardell M, Schrack JA, & Ferrucci L (2016). Fatigued, but not frail: Perceived fatigability as a marker of impending decline in mobility-intact older adults. Journal of the American Geriatrics Society, 64(6), 1287–1292. 10.1111/jgs.14138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonsick EM, Schrack JA, Glynn NW, & Ferrucci L (2014). Assessing fatigability in mobility-intact older adults. Journal of the American Geriatrics Society, 62(2), 347–351. 10.1111/jgs.12638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonsick EM, Schrack JA, Santanasto AJ, Studenski SA, Ferrucci L, & Glynn NW (2018). Pittsburgh Fatigability Scale: One-page predictor of mobility decline in mobility-intact older adults. Journal of the American Geriatrics Society, 66(11), 2092–2096. 10.1111/jgs.15531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephan Y, Sutin AR, Canada B, & Terracciano A (2017). Personality and frailty: Evidence from four samples. Journal of Research in Personality, 66, 46–53. 10.1016/j.jrp.2016.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, An Y, Sutin AR, Thambisetty M, & Resnick SM (2017). Personality change in the preclinical phase of Alzheimer Disease. JAMA Psychiatry, 74(12), 1259–1265. 10.1001/jamapsychiatry.2017.2816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, Costa PT, & McCrae RR (2006). Personality plasticity after age 30. Personality and Social Psychology Bulletin, 32(8), 999–1009. 10.1177/0146167206288599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, Schrack JA, Sutin AR, Chan W, Simonsick EM, & Ferrucci L (2013). Personality, metabolic rate and aerobic capacity. PLoS ONE, 8(1), e54746. 10.1371/journal.pone.0054746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolea MI, Terracciano A, Simonsick EM, Jeffrey Metter E, Costa PT, & Ferrucci L (2012). Associations between personality traits, physical activity level, and muscle strength. Journal of Research in Personality, 46(3), 264–270. 10.1016/j.jrp.2012.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wanigatunga AA, Simonsick EM, Zipunnikov V, Spira AP, Studenski S, Ferrucci L, & Schrack JA (2018). Perceived fatigability and objective physical activity in mid- to late-life. The Journals of Gerontology: Series A, 73(5), 630–635. 10.1093/gerona/glx181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wanigatunga AA, Varadhan R, Simonsick EM, Carlson OD, Studenski S, Ferrucci L, & Schrack JA (2018). Longitudinal relationship between interleukin-6 and perceived fatigability among well-functioning adults in mid-to-late life. The Journals of Gerontology: Series A. 10.1093/gerona/gly120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu R, Rebok GW, & Lin FV (2016). A novel theoretical life course framework for triggering cognitive development across the lifespan. Human Development, 59(6), 342–365. 10.1159/000458720 [DOI] [Google Scholar]