ABSTRACT
Introduction
Active matrix metalloproteinase (aMMP)-8 utilized in point-of-care testing (POCT) is regarded as a potential biomarker for periodontal and peri-implant diseases. Various host and microbial factors eventually influence the expression, degranulation, levels and activation of aMMP-8. The type of oral fluids (saliva, mouthrinse, gingival crevicular, and peri-implant sulcular fluids [GCF/PISF], respectively) affect the analysis.
Areas covered
With this background, we aimed to review here the recent studies on practical, inexpensive, noninvasive and quantitative mouthrinse and GCF/PISF chair-side POCT lateral flow aMMP-8 immunoassays (PerioSafe and ImplantSafe/ORALyzer) and how they help to detect, predict, monitor the course, treatment and prevention of periodontitis and peri-implantitis. The correlations of aMMP-8 POCT to other independent and catalytic activity assays of MMP-8 are also addressed.
Expert opinion
The mouthrinse aMMP-8 POCT can also detect prediabetes/diabetes and tissue destructive oral side-effects due to the head and neck cancers’ radiotherapy. Chlorhexidine and doxycycline can inhibit collagenolytic human neutrophil and GCF aMMP-8. Furthermore, by a set of case-series we demonstrate the potential of mouthrinse aMMP-8 POCT to real-time/online detect periodontitis as a potential risk disease for coronavirus disease 2019 (COVID-19). The clinical interdisciplinary utilization of aMMP-8 POCT requires additional oral, medical, and interdisciplinary studies.
KEYWORDS: Matrix metalloproteinase 8, Covid-19, oral fluids, diagnostics, mouth rinse, biomarkers, peri-implantitis, periodontitis
1. Introduction
Periodontitis is a major infection-induced chronic inflammatory disease that is caused by inflammatory response associated with and resulting from imbalanced interaction between host and the periodontal microbiome [1]. Periodontitis is classified by the severity and complexity of the disease and its management (stage of periodontitis) with assessment of the risk for further disease progression [2]. Periodontitis is not only leading to local tissue destruction in the tooth supporting structures (periodontium) but also associates with several systemic diseases such as diabetes and cardiovascular diseases [1]. Periodontitis increases the systemic inflammatory burden, as host-derived mediators of periodontal inflammation and tissue destruction (e.g., cytokines and metalloproteinases) are released from the inflamed periodontal tissue to the circulatory system [1]. Recent developments in the molecular periodontal and peri-implant research has addressed potential oral fluid [saliva, mouthrinse, GCF, peri-implant sulcular fluid (PISF)] biomarkers among them aMMP-8 POCT, to amend diagnostic procedures in periodontitis and peri-implantitis [3].
1.1. aMMP-8’s accuracy as oral fluid biomarker for periodontitis, peri-implantitis, diabetes disease, and radiotherapy induced side effects
Among the chair-side/point-of-care -tests (POCT) developed so far, active matrix metalloproteinase (aMMP)-8 POC-lateral flow-immunotests discovered and developed by Sorsa et al. and validated independently in various studies exerts promising results as an adjunctive diagnostic/screening and prognostic tool for periodontitis, peri-implantitis, diabetes, Chrohn’s disease, and oral periodontal side-effects of cancer radiotherapy [3–22].
Utilizing oral fluids (i.e., mouthrinse, peri-implant sulcular fluid [PISF], gingival sulcular fluid [GCF]) as samples; aMMP-8 serves as a biochemical marker to distinguish between the disease and health status of periodontal and peri-implant tissue. aMMP-8 POCT has also been implemented as not only a viable but a key biomarker relevant to the new classification of both periodontitis and peri-implantitis [4–6,18,23–25]. Assessment of aMMP-8 levels in oral fluids especially in mouth rinse and GCF/PISF [3–6,10,23,26–29], can thus provide adjunctive diagnostic and prognostic data on collagenolytic inflammation around natural teeth and dental implants prior to detectable clinical and radiographic changes [4–6,8,9,23]. Significantly higher aMMP-8 levels have also been found in whole saliva samples of patients suffering from periodontal disease when compared with healthy controls [3,30]. However, mouth-rinse, GCF/PISF aMMP-8, analysis, and testings were more precise than salivary total MMP-8 analysis [30–33]. Available data encourages utilization of aMMP-8 as the key diagnostic biomarker and predictor of periodontal/peri-implant disease progression, in addition to monitoring treatment and therapeutic outcomes [3–6,10,18,23,34,35].
In health, MMP-8 in oral fluids is mainly present in its latent form and is detected at considerably lower levels, while the expression of aMMP-8 increases in severe forms of the periodontal/peri-implant diseases [3–5,12,18,24,35–40]. The low level or absence of aMMP-8 signifies and indicates a state of periodontal/peri-implant health [3–5,23,24,39,40], whereas the activity, severity and progression of periodontitis and peri-implantitis have been significantly and positively associated with an increase in aMMP-8 levels. The same, however, has not been found when total/latent MMP-8 levels were utilized [3,10,12,26,36–40]. Currently, aMMP-8-based lateral flow immunoassays are commercially available as U.S. Food and Drug Administration (FDA) – and EU-approved chair-side (PoC) – test kits that are quantitative, sensitive, time-saving, specific, accurate and economical while discriminating periodontal and peri-implant health and disease [3–6,10,12,18,23,24]. The introduction of an aMMP-8-based point of care test, which utilizes mouthrinse samples, and not saliva [3–6,18,31,32], for monitoring periodontal disease is a ‘game-changer’ in the field not only by providing information about the current situation but also predictively susceptible individuals/sites and prognosis of treatment rendered [3–6,12,18,23,25]. It acts as an alarm in predicting collagenolysis in periodontitis/peri-implantitis situations, prior to the occurrence of irreversible clinical and x-ray manifestations [3–6,10,22,34,41]. With aMMP-8 POCT one can conveniently follow in real time and online the reversible and irreversible changes in grading and staging of periodontitis [22]. Finnish/Swedish studies have shown that an active MMP-8 PoC test (POCT) can effectively detect initial periodontitis associated with single nucleotide polymorphisms of Vitamin D Receptor (VDR) and MMP-3 genes [42,43]. Measurement of aMMP-8 by lateral-flow chair-side/PoC immunoassay demonstrated a high sensitivity (75–85%) and specificity (80–90%) for the detection of periodontitis while utilizing a 20 ng/ml cutoff value, with at least two sites exhibiting probing depth (PD) ≥5 mm vs. less than two PD≥5 mm sites [3,4,7,8,23,43–45]. The association of aMMP-8 level alterations with clinical parameters and radiographic findings has been demonstrated in several studies [6,8,9,12,18,35]. Although a chair-side/PoC aMMP-8 test could not discriminate between smokers and nonsmokers with progressive periodontitis [35,44,46], it was demonstrated that this assay could effectively predict the prognosis of smokers, in that elevated baseline-aMMP-8 levels indicated a poor response to conventional periodontal treatment (e.g. scaling and root planing [SRP]) [35,44,46] whereas sites which were non-responsive to treatment continued to express high levels of aMMP-8 [35,44,46]. Diseased peri-implant sites exhibit elevated aMMP-8 levels in PISF similar to the periodontitis sites [5,10,23,35,47–49], and the cellular source is mainly inflammatory cells, particularly neutrophils [3,35,50]. The severity of bone loss and osteolytic activity during peri-implantitis was found to be associated with an increase in aMMP-8 levels in PISF, which was further confirmed by studies utilizing independent polyclonal antibody and western-immunoblot technology for the aMMP-8 assessment [47–49,51,52]. Figure 1 shows that with aid of ImplantSafe it is possible to real-time and online monitor the effects of successful treatment on implantitis; positive (> 20 ng/ml aMMP-8) [8,53] aMMP-8 POCT sites were converted to negative (< 20 ng/ml aMMP-8) by successful treatment of peri-implantitis [8,53,54].
Figure 1.
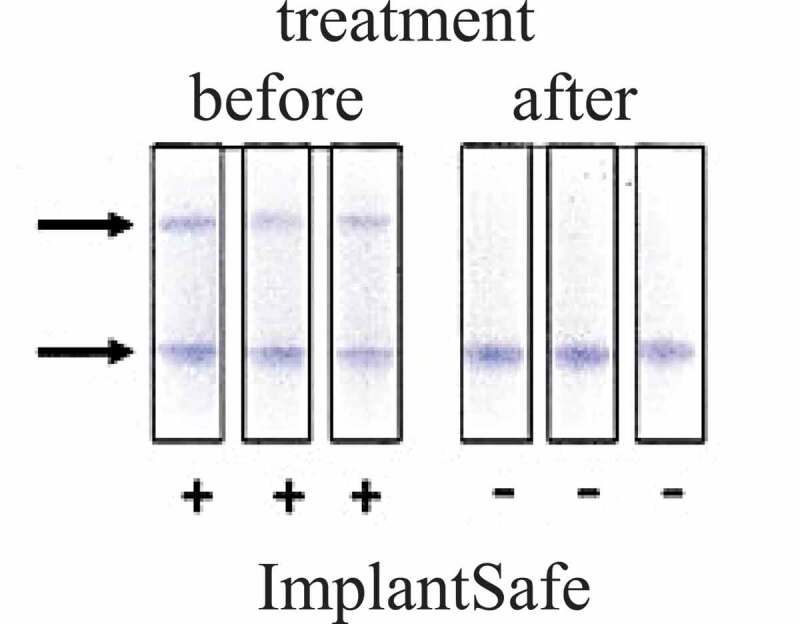
Implantitis sites were tested before (+), two lines indicated by arrows and after (-), one line indicated by arrows surgical treatment by ImplantSafe; treatment caused positive sites (before, +) to be negative (after, -). Elevated active matrix metalloproteinase (aMMP)-8 levels in PISF detected by ImplantSafe positivity (before, +, two lines) and associated significantly with peri-implantitis and could be PoC -detected in 5 min by ImplantSafe
Results from a ten-year retrospective analysis, indicated a positive correlation between upregulated and fragmented aMMP-8 expression in oral fluids (GCF/PISF), the degree of inflammation and severity of periodontitis [26,27,33]. Similar to natural dentition, the therapeutic response of tissues supporting dental implants can be predicted by measuring aMMP-8 levels in mouth-rinse and/or PISF more precisely than salivary measurements [31,32]. The cutoff points of aMMP-8 in oral fluids i.e. 20 ng/ml in mouth-rinse, PISF and GCF, have been determined to differentiate with sensitivity of the 75–85% and specificity of 80–90% a healthy state from both periodontitis and peri-implantitis [3–5,7,8,17,23,43,45]. One study has utilized a 10 ng/ml cutoff; however, no test kits with this cut off test value are commercially available or have been fabricated [6,18]. The lower sensitivity (35%) assessed by Deng et al. [18] was eventually due to their periodontally healthier patient cohort with lesser clinical disease activity in comparison to cohort with enhanced clinical disease activities by Lähteenmäki et al. [10] and Sorsa et al. [4,6]. Thus in patients on maintenance therapy or in those with low disease activity, aMMP-8 values are known to be lower [15,16,18] than those in patients with more enhanced periodontal clinical disease activity [4,6,10,22,24].
Genetic polymorphisms of MMP-3 and Vitamin D Receptor (VDR) are significantly associated with aMMP-8 levels; thus the MMP-8 POCT identifies genetically susceptible subjects [35,43]. Results from aMMP-8 POCT were consistent with treatment needs determined by Community Periodontal Index of Treatment Needs (CPITN)-index in both adults and adolescents [35,55]. HbA1c along with aMMP-8 POC testing can provide dentists and medical professionals an opportunity to diagnose prediabetic and diabetic patients [20,21,35]. aMMP-8 was twice higher in terms of sensitivity and more accurate than bleeding on probing (BOP) in detecting early stages of periodontal disease [18,32,35]. aMMP-8 was positively associated with the severity of periodontitis by virtue of mediating the pathogenicity of potent periodontopathogens, such as the activation of Treponema denticola protease [33,56–59]. aMMP-8 POCT correctly diagnosed all healthy and peri-implantitis cases, and discriminated health from peri-implantitis with higher accuracy than BOP, calprotectin, total MMP-8, polymorphonuclear neutrophil (PMN)-elastase, MMP-2, MMP-9, tissue inhibitor of matrix metalloproteinase (TIMP)-1, and myeloperoxidase (MPO) [3–6,10,12,23,31,32,35]. These data clearly indicate that aMMP-8 POCT can be implemented as the key biomarker for staging and grading (i.e. the new Tonetti-classification [25]) of both periodontitis and peri-implantitis [4–6,10,18,23,24,28].
The PerioSafe® and ImplantSafe® aMMP-8-POCT kits are efficient adjunctive tools in enhancing the accuracy of diagnostic and prognostic of periodontal and peri-implant diseases. They are commercially available FDA (USA)- and EU – approved technologies [2–6,12,18,32,35]. Future development of these POC test kits should ideally take into account the assured criteria introduced by the World Health Organization (WHO) [6,12,18]. The quantitative, noninvasive and economic PerioSafe® and ImplantSafe®/ORALyzer® tests have already been validated to function sufficiently and fluently with a single biomarker, i.e., aMMP-8 that is demonstrated as a biomarker of significance in the new classifications of both periodontitis and peri-implantitis [4–6,10,12,18,23,24,27,28]. Further studies are required to increase their diagnostic and prognostic power through combining with other possible biomarkers and integrating these test kits into periodontal risk assessment [12,18,35]. However, POCT methodologies utilizing multiple biomarkers are yet to be developed [3,30,35,60].
aMMP-8 present in periodontitis-affected oral fluids, i.e., in periodontitis-affected GCF and that degranulated by triggered human neutrophils [59,60], can be inhibited and down-regulated not only by doxycycline but also by chlorhexidine (Figure 2A and B) [58,60,61].
Figure 2.

Inhibition of native type I collagen degradation by human neutrophil (PMN) active matrix metalloproteinase (aMMP)-8 and adult chronic periodontitis gingival crevicular fluid (GCF) aMMP-8 by chlorhexidine (CHX). Figure 2A, lane 1: 1.5 µM native type I collagen; lanes 2 and 3: 1.5 µM native type I collagen incubated with PMN aMMP-8 (400 ng [59]) for 8 h at 22°C; lanes 4 and 5: as lanes 2 and 3 but in the presence of 0.01%, 0.02%, and 0.04% CHX. Figure 2B, lane 1: 1.5 µM native type I collagen; lanes 2 and 3: 1.5 µM native type I collagen incubated with GCF aMMP-8 for 8 h at 22°C; lanes 4−8: as lanes 2 and 3 but in presence of 0.005%, 0.01%, 0.02%, and 0.04% CHX. β indicates intact native type I collagen dimers and α indicates intact native type I collagen monomers, βA, and αA indicate classical ¾ (75%) – degradation products resulting from catalytically competent (active) collagenolytic action of aMMP-8 on native type collagen. Observe the dose – dependent inhibition of type I collagenolytic activity of aMMP-8 by CHX
Overall, the aMMP-8 chair-side-POCT technologies are used for diagnostic and prognostic purpose in periodontitis, peri-implantitis, prediabetes/diabetes (diabetes I, II, and pregnancy-related diabetes I), Crohn’s disease, radiotherapy-related immunodeficiency, and other oral destructive side-effects of head and neck cancers [4–7,10,12,18–23]. At present oral fluid, i.e., salivary POCTs have also been developed for calprotectin and MMP-9 [62,63]. Noteworthy recent comparative studies have shown that mouthrinse aMMP-8 POCT is more precise than salivary total MMP-8, calprotectin, MMP-9, human neutrophil elastase, myeloperoxidase immunoassays, and BOP [10,12,18,23]. Lee et al. [36], Mancini et al. [37], Teronen et al. [47], Mc Crudden et al. [40], Uitto et al. [39] by specific catalytic independent activity assays for aMMP-8 have consistently and repeatedly shown that aMMP-8 but not latent/total MMP-8 is associated with, and reflects the ethiopathogenesis, course and severity of periodontitis, and peri-implantitis.
As established, the aMMP-8 POCT assumes greater value during the COVID-19 pandemic in light of periodontal disease predisposing demonstrably greater COVID-19 related adverse outcomes. The ability of this testing methodology to indicate the staging and grading of periodontitis, especially in the early stages, may prove to be invaluable, not only as a point-of-care test in the ICU but also as an at-home test in order to decide whether professional opinion should be sought.
1.2. SARS CoV-2 and the oral cavity
It remains to be clarified, whether the oral fluid aMMP-8-chair-side-POCT can be utilized to identify periodontitis as a potential disease/comorbidity increasing the risk and severity of Coronavirus disease 2019 (COVID-19) [12,64,65]. The emergence of severe acute respiratory syndrome coronavirus 2 (SARS CoV-2) has posed a significant challenge to clinical practice forcing many branches of medicine to reevaluate the established concepts. Dental treatments have been limited with the urgent procedures putting aside the elective interventions. The focus lately, seems to be on avoiding aerosol generating procedures, which for the large part, form the entire purview of modern clinical dental practice. This, however, stems from evidence suggesting the transmission of SARS CoV-2 via aerosols. High viral titers have been recovered not only from the saliva of infected individuals, but also from the GCF. This is a serious concern as these oral fluids are unavoidable entities while working inside the oral cavity, excluding certain procedures that can be performed using a rubber dam. A vast number of seemingly urgent procedures in the maxillofacial region have been either deferred or managed by methods other than conventionally established protocols [66,67].
The SARS CoV-2 has been detected in a number of intraoral tissues which can subsequently act as or mediate points of entry for the virus. This is attributed to the presence of angiotensin converting enzyme (ACE)-2 receptors, the entry points for the virus, being exhibited in generous numbers in the tissues of the oral cavity. The greatest concentration of these receptors is at the floor of the mouth and the oral portion of the tongue, followed by gingival tissue and cells lining the buccal mucosa [68].
Both early and late stages of the COVID-19 disease process relate to salivary viral shedding, with ductal openings serving as the primary source of the virus in later stages of the disease. It has been found in rhesus macaques, that glandular epithelial cells expressing the ACE-2 receptors acted as initial targets for infection by the SARS CoV. The recovery of live viral load of SARS CoV-2 from saliva cannot be solely attributed to it, since saliva composes both GCF and/or sputum. Regardless of the source, saliva plays a key role in virus transmission with high viral titers being detectable within the first seven days of disease presentation and continuing up to a post-onset period of 25 days. A number of potential advantages such as the ease and noninvasive nature of the collection along with the possibility of self- or home-collection of samples make saliva preferential as the diagnostic fluid [69,70]
1.3. Immune response, COVID-19 infection and periodontal disease
The prevalence of periodontal disease far outweighs that of COVID-19, something to consider in the midst of a pandemic. Especially when the two diseases seem have a confluence in terms of the responsible immunological mechanisms. The etiopathogenesis of periodontal disease involves host immune response as the chief pathway to promote tissue destruction. The immunological fallout of the disease process involves the local and systemic elevation of a number of cytokines which have been utilized over the years as diagnostic and prognostic tools not only for periodontal disease but also for the systemic conditions it might influence. COVID-19 symptomatology has also been related to the occurrence of a proverbial ‘cytokine storm’ translating as elevated levels of interleukin (IL)-2, IL-1 beta, IL-7, IL-10, IL-17, granulocyte macrophage-colony stimulating factor (GM-CSF), tumor necrosis factor (TNF)-alpha, granulocyte colony-stimulating factor (G-CSF), monocyte chemoattractant protein (MCP)-1 and macrophage inflammatory protein (MIP)1A [68,71]. This can be associated with an elevated response profile of the Th17 pathway as was previously reported in infections with SARS-CoV and Middle East respiratory syndrome coronavirus (MERS-CoV) [66,68].
There seems to be a peculiar similarity in the periodontal disease-like inflammatory profile of patients developing such a cytokine storm and their subsequent progress into a condition similar to acute respiratory distress syndrome (ARDS). Bronchoalveolar lavage fluid recovered from patients of acute chronic obstructive pulmonary disease (COPD) and ARDS exhibits neutrophil extracellular trap (NET) formation [68]. Being a form of cell death, NETosis is a disaster at the cellular level where it contributes to destruction. A similar brand of bystander damage is elicited in periodontal disease by means of TNF-alpha induced NETosis. Hence, there seems enough evidence at an immunological level to advocate an association between COVID-19 and periodontal disease.
1.4. Maintenance of oral hygiene in COVID-19 infection and periodontal disease
With the immunological plausibility between periodontal disease and COVID-19 being present along with the existence of certain reports in literature commenting on an association between periodontal disease and COVID-19-related adverse outcomes, oral hygiene maintenance would assume greater significance in battling the pandemic.
The standard recommendation of maintaining oral hygiene practices would seem to stand firm in the face of the SARS CoV-2 as well. This seems logical since maintenance of hand hygiene with soaps, detergents and antiseptics has been propounded since the beginning of the pandemic and a number of oral hygiene products contain similar preparations [72]. Recent laboratory studies have reported that zinc or stannous containing toothpastes are capable of eliminating the SARS CoV-2 to the tune of 99.9% [71]. Moreover, there has been an increasing contention lately that the risk of contracting infection via contaminated surfaces is rather low [73]. Since toothbrushes along with toothpaste are the recommended means to maintain oral hygiene, it would seem logical to assume that any viruses shed on to the head of the toothbrush would be destroyed by the antimicrobial components of the toothpaste. As such, there is sparse evidence in literature on toothbrush contamination. Furthermore, patient compliance forms a significant aspect of oral hygiene maintenance. Toothbrushing is generally recommended to last not less than 2 min. If a disinfection protocol including multiple steps and different antiseptic solutions prior to and/or after brushing were to be recommended possibly lasting for up to 20 minutes, patient compliance may be at risk.
As the world continues to grapple with COVID-19, post-COVID-19 sepsis appears to be an issue itself. A number of studies have pointed out the association between diabetes and COVID-19-related adverse outcomes [74]. Mucormycosis, regarded as a rare infection, continues to be one of the most catastrophic complications in patients with uncontrolled diabetes. The immune exhaustion, which accompanies post COVID-19 sepsis along with the fallout of utilizing steroid therapy and anti-IL-6 treatment strategies to combat the infection leave the patient susceptible to the development of this infection. The most significant manifestations of these infections seem to be pulmonary and rhino-orbital-cerebral. A hallmark feature to be observed clinically in order to discern the infection is the manifestation of an eschar, necrotic lesion or a black-colored discharge from the oral or nasal cavity. Other significant clinical clues are pansinusitis and involvement of the ethmoids [75]. Dentists working both in the clinical and hospital settings need to be aware of this presentation along with other important signs such as involvement of the cranial nerves, orbits and ocular tissue, in order to affect prompt referrals. The treatment involves management of underlying conditions, antifungal therapy and debridement of the lesions. It is important to identify and act on this condition promptly as improper diagnosis can lead to further steroid and antibacterial prescriptions which would tend to compound the problem.
1.5. COVID-19 and aMMP-8
Periodontitis, being a chronic inflammatory disease has been hypothesized to be associated and involved with adverse COVID-19 related outcomes. There remains, however, a dearth of literature to validate this concept. Matrix metalloproteinase-8 belongs to the MMP superfamily, which are a set of genetically distinct but structurally related endopeptidases. Pathological levels of especially aMMP-8 are associated with the tissue destruction in periodontitis/peri-implantitis diseases [4–6,9,12,18,64,76–78]. It has been established that this enzyme is elevated beyond its physiological limits in COVID-19 patients seen to be in what has been purportedly labeled as ‘cytokine storm.’ This knowledge can be utilized to ratify whether periodontal disease and the ensuing underlying inflammatory process contribute to the overall host immune response in patients suffering from COVID-19. For this purpose, it would seem logical to utilize a rapid bedside noninvasive aMMP-8 POCT [4,6,12,18] which could aid in the real-time monitoring of MMP-8 status in these patients. This would not only validate if periodontal disease may play any role in the overall clinical presentation but also serve as a convenient diagnostic tool to tailor therapy in order to achieve ideal therapeutic outcomes all the while sensitizing patients to the importance of oral health care as a component of overall wellbeing. Moreover, the treatment of COVID-infection patients’ oral diseases involve often chlorhexidine-rinsing (Figure 2A and B), especially in intensive care unit (ICU) [6,61,64,77–79]. Furthermore, identification of periodontitis as the potential COVID-infection linked risk disease or comorbidity identified by the aMMP-8 POCT can eventually be demonstrated (Figure 3 and 4) [64,65,71,76–78].
Figure 3.
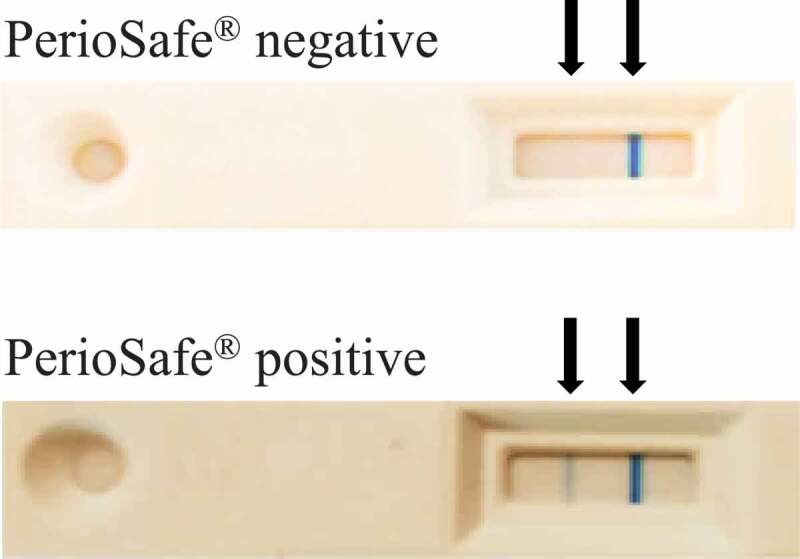
PerioSafe kit (negative: < 20 ng/ml; positive: > 20 ng/ml), a mouthrinse active matrix metalloproteinase (aMMP)-8 point-of-care test (POCT)
Figure 4.

ImplantSafe kit (negative: < 20 ng/ml; positive: > 20 ng/ml), a site-specific peri-implant sulcular and gingival crevicular fluid (PISF/GCF) active matrix metalloproteinase (aMMP)-8 point-of-care test (POCT)
The COVID-19 pandemic has, for the large part involved the repurposing of existing treatment modalities based on what is established in literature. Research in periodontal medicine has led to the identification of therapeutic targets which can aid in the management of respiratory disease of a severe nature. This primary stems from an understanding of the commonality in the host-side immune response in both COVID-19 and periodontal disease. Pulmonary tissue damage and eventual mortality observed in SARS CoV-2 infections can be attributed to a hyperactivity of the neutrophil response elicited. At the same time, as a result of microbial insult, periodontal disease also involves the constant influx of hyperactive neutrophils which lead to tissue destruction. With a background of this knowledge, it seems quite logical that host modulation therapy (HMT) designed to tackle the host’s immune response and proteolytic burden in periodontal disease can be repurposed to manage the acute respiratory distress syndrome pathophysiology as observed in COVID-19 [78]. As a short-term and provisional treatment modality, chlorhexidine, as inhibitor of aMMP-8 (Figure 2A and 2B), can also be used to tackle both the microbial and proteolytic burden in the COVID mouth [61,79,80].
1.6. Doxycycline therapy and chair-side diagnostics in the treatment of high-risk COVID-19- positive patients
With no cure in sight, the COVID-19 pandemic has seen a number of drugs being repurposed in order to tackle the presentation of this novel entity. The pathophysiology of this disease involves elevated levels of pro-inflammatory cytokines, which have been dubbed in serious cases as a ‘cytokine storm’ or at the least been related to the symptomatic presentation of cases.
Respiratory failure as a result of acute respiratory distress syndrome (ARDS) has been touted as the most significant reason for mortality [78]. The pathological features of COVID-19 bear an uncanny resemblance to those observed in SARS CoV infections which are known to cause remodeling of the lung tissue as a result of a number of pathways including those involving matrix metalloproteinases (MMPs) [78].
MMPs are responsible for the deterioration of the extracellular matrix and lung tissue remodeling which eventually leads to an increase in vascular permeability and damage to the basal lamina of the endothelium [78]. To compound the problem, ARDS management entails mechanical ventilation, which can result in MMP mediated lung injury via induction from ventilation [78]. MMP-8 along with MMP-2, MMP-9, and TIMP-1 has been observed to be elevated and activated in early stages of sepsis and has been related to mortality.
The role of MMPs is elucidated not only in acute conditions but also in those of a more chronic and/or low-grade variety such as obesity. Obesity has been linked to diabetes with insulin resistance. This has been purportedly attributed to the elevated levels of MMPs, specially MMP-8 in obese and otherwise healthy patients. High levels of MMPs, especially MMP-8, correlate in metabolic syndrome and the resulting diabetes, which have been linked with adverse outcome of COVID-19. While females seem to have less severe forms of COVID-19, the level of MMP-8 in obese women seem to be less pronounced as well.
It has been suggested that cleavage of the human insulin receptor protein by MMP-8 is responsible for the development of insulin resistance and subsequent diabetes mellitus in these cohorts.
MMP-8 levels have also been found to be indicative of not only local infections but also systemic and multi-organ problems [4,27,78,81–83]. Metabolic syndrome increases the levels of ACE2 receptors. ACE2 receptor is a key entry point to the Sars-CoV-2 in the lungs. This receptor is counteracting the ACE receptor, commonly antagonized in hypertension treatment. The use of ACE inhibitors modulate the expression of the ACE2 and might increase the number of ACE2 receptors. However, the use of ACEi medication seem to have little or no impact in morbidity of COVID-19. This observation goes in hand with the fact, that the ACE inhibition does not change the MMP-8 levels either.
However, MMPs have been demonstrated to have an anti-inflammatory and protective role as well, in physiological levels. It would hence, seem logical to utilize ‘leaky’ MMP inhibitors such as a chemically modified tetracyclines or sub-antimicrobial dose doxycycline in order to modify host response while maintaining adequate levels of safety [81].
Doxycycline through its pleiotropic mechanisms provides an improvement in the symptomatic presentation of COVID-19 cases by virtue of its action as a pro-inflammatory inhibitor encompassing the entire family of MMPs in addition to possessing antiviral properties [81]. There is evidence in literature to support the role doxycycline plays to protect the lung against injury [81]. It has been observed to be efficacious in the management of viral infections such as chikungunya and dengue. The action of doxycycline on viral replication pathways confers unique antiviral properties as it can potentially inhibit the papain-like protease (PLpro) and 3 C-like protease (3CLpro) components [81].
Elevated levels of inflammatory biomarkers have been associated with poorer clinical outcomes [81]. MMPs have been suspected to facilitate early viral entry into cells. Inhibition of these MMPs along with that of IL-6 can in part, explain the efficacy of doxycycline in managing COVID-19 infections since these components are key regulators of the purported ‘cytokine storm’ observed in severe COVID-19 cases. Not only this, but doxycycline being an ionophore, also mediates intracellular zinc transport which, in vitro, has been demonstrated to impede the replication of the coronavirus [81]. Doxycycline also acts in the inhibition of the nuclear factor-kB which in turn brings about a direct inhibition of the Dipeptidyl peptidase-4 (DPP4) receptor on the cell surface which can subsequently diminish the chances of viral entry via this route. Extracellular matrix metalloproteinase inducer (CD147/EMMPRIN) has been suspected to facilitate T-lymphocyte SARS CoV-2 entry. Low dose doxycycline which is essentially non-antimicrobial in nature has been demonstrated to inhibit these receptors [81]. Hence, the role of doxycycline in COVID-19 management, seems quite evident.
In a double-blind placebo-controlled study by Payne & Golub on post-menopausal women, all subjects received scaling and root planing and oral hygiene instructions every 3-month over a 2-year protocol, after due approval from the Ethics Committee [83]. Following random allocation in test and control groups, the women on Periostat® (20 mg doxycycline twice daily or 40 mg once a day) recorded 50% lower mean serum MMP-8 levels than those on placebo capsules (Table 1); indicating direct evidence of effect of low dose doxycycline on the systemic MMP-8 levels. This sub antimicrobial dose of doxycycline is available as a sustained release tablet which produces peak blood levels of approximately 0.5 µg/ml vis. a vis. the usual antimicrobial dose of 100 mg which produces a peak of 2–5 µg/ml.
Table 1.
Active Matrix metalloproteinase (aMMP)-8 levels in post-menopausal women adherent to a 2-year study protocol as described in Payne & Golub [83]
| Group | Number of subjects | aMMP-8 levels in serum (ng/mL) |
|
|---|---|---|---|
| Mean | Standard Deviation | ||
| Placebo | 16 | 46.0 | 48.6 |
| Sub antimicrobial dose doxycycline | 22 | 22.6 | 14.0 |
aMMP-8: Active matrix metalloproteinase-8
A ‘two-hit’ concept has been discussed in literature where in local and systemic predilection of inflammatory disease processes may be equated [83]. A local inflammatory process such as endotoxins released by pathogenic oral microflora (first ‘hit’) may induce a cascade of events which ultimately lead to elevated levels of MMPs [83]. This is further compounded by the underlying systemic level (second ‘hit’) such as diabetes, cardiovascular disease, rheumatoid arthritis, post-menopausal osteoporosis etc [83]. To reverse engineer this concept in order to aid disease management, it can be argued that the utilization of validated natural remedies like the lingonberry mouthwash to lower the inflammatory load at the local level (first ‘hit’) of the oral cavity, would manifest in a reduction of systemic inflammation as well. Their addition to the sub antimicrobial dose doxycycline regime/ chemically modified tetracycline therapy aimed at targeting the second ‘hit’ would then have synergistic benefits in such compromised patients.
As mentioned previously, an absolute inhibition of MMP activity is in fact deleterious and MMPs need only be lowered to within their physiological limits for treatment to be effective. To accomplish this, the ideal requirement would be that of a noninvasive, bedside diagnostic tool which provided real- time assessment. It would hence, be both prudent and practical to have at our disposal, a noninvasive aMMP-8 PoC test, a quick diagnostic tool which aids in the real-time determination of the cytokine profile of patients. The MMP-8 PoC test is a point of care test which provides a quantitative and visual determination of MMP-8 levels [4]. It can be utilized as a bed side test and the sampling methodology involves rinsing to obtain saliva samples [4]. Oral fluids have been validated as being reflective of systemic MMP-8 levels in previous studies. Utilizing these validated bed-side test can aid in monitoring and subsequently tailoring the disease management process to improve patient outcomes and provide caregivers with an accurate real-time picture of the therapeutic response rendered.
1.7. Expert opinion
There remains a limited understanding of the reasons for clinical variability of coronavirus disease 2019 (COVID-19), and a lack of oral fluid-based biomarkers to identify individuals at potential risk of developing severe periodontal and lung diseases. We have addressed aMMP-8 POCT and a potential vascular route of invasion and transfer of SARS-CoV-2 from the oral cavity to the systemic circulation and lungs. Oral fluid aMMP-8 POCT can be regarded as an interdisciplinary ‘C-reactive protein (CRP)’ of mouth [4,6,10,12,18]. Saliva/oral fluids can thus be regarded as a potential reservoir of SARS-CoV-2, and consequently any breach in the immune defenses in the mouth may eventually facilitate entrance of the virus and microbial infectants to the systemic circulation through the proteolytically (aMMP-8) processed inflamed gingival/implant sulcus or periodontal pocket. It is suggested that dental plaque accumulation (T. denticola and P. gingivalis) and periodontal inflammation with aMMP-8 burden would further intensify this pathway. T. denticola, P. gingivalis and Candidal proteases can degrade basement membrane components laminin 5 ƴ 2-chain and occludin as well as activate proMMP-8 thus not only degrading tissue basement membranes but also potentially promoting microbial and viral invasion [48,57–59,84–89]. Therefore, it is suggested that optimal plaque control and oral healthcare should be prioritized as such measures could be potentially lifesaving for COVID-19 patients. If justified, this elevated oral fluid aMMP-8 POCT, and proposed pathological pathway, may provide significant improvement in disease management. Simple low-cost diagnostic aMMP-8 POCT and therapeutic approaches, such as use of specific mouthwashes [79,80], could decrease the salivary viral and microbial burden and invasion, and protect from aMMP-8 proteolytic and proinflammatory burden load, and help prevent or mitigate the development of lung disease related to the severe COVID-19.
The aMMP-8 technology has been demonstrated to be utilized a systemic biomarker in the destructive inflammatory and infectious disease activity such as in sepsis, obesity/diabetes; bacteremia, meningitis, cardiovascular diseases and pancreatitis [90–95].
The COVID-19 pandemic has created indications to surge to the teledentistry. A significant number of patients have been unable to attend for regular dental checkups have also had oral health concerns, of which the examinations and managements have been a challenge. Periodontal disease is chronic in nature, usually painless, contributes to local/systemic morbidity and requiring a certain level of experience and expertise to diagnose and manage. The presence of periodontal disease has also been correlated to poorer COVID-19-related outcomes [64,65,75,76,96]. These studies do, however, have the obvious drawback of not assessing active periodontal disease or its activity and severity [64,65,75,76].
With this background many practices are initiating to resort to tele- or e-dentistry, it would thus be useful to have a diagnostic methodology for periodontal/peri-implant diseases without a formal face-to-face examination. Oral fluid point-of-care aMMP-8 POCT diagnostics provide for simple, noninvasive, quick and real-time assessment of a patient’s periodontal/peri-implant status [10,12,23]. The test can even be self-administered by patients similarly to the classical pregnancy test (Alassiri et al., 2018). aMMP-8 levels above 20 ng/ml are indicative of active periodontal disease, diagnosing which can lead to timely and needed the therapeutic intervention [10,12]. It is available as a mouthrinse (PerioSafe; Figure 3) and sulcular fluid/gingival crevicular fluid (ImplantSafe; Figure 4) variants [4,5,8,18,53]. PerioSafe can be utilized as an indicator of general periodontal status, whereas the ImplantSafe variant can be used as a site-specific test. It has the evident advantage of being user friendly and practical tool-kit, and general practitioners/medical professionals can also interpret the results and then decide if a dental specialist referral is required [12]. The results can be both qualitative and quantitative utilizing the ORALyser reader [4,6,8,10,12,18]. In older patients who are more prone to having COVID-19 related adverse outcomes and are, at the same time more likely to have dental implants, the ImplantSafe variant can be utilized to assess the implant status as well. Lastly, patients admitted in the ICU, may not always be amenable to specialist referral or to a full-fledged oral/periodontal examination. aMMP-8 POCT diagnostics thus provide a highly convenient methodology to assess/monitor the periodontal status of such patients and institute care where necessary [96]. These aMMP-8 POCT technologies, owing to their simplicity may thus be conducted by patients, laymen, and healthcare workers alike.
Funding Statement
This research was funded by the Helsinki and Uusimaa Hospital District (HUS) (TYH2016251,TYH2017251, TYH2018229, TYH2019319, Y1014SL017, Y1014SL018, Y1014SULE1), Finland; Suomen Hammaslääkäriseura Apollonia (Finnish Dental Association Apollonia), Finland; Karolinska Institutet, Sweden.
Article highlights
There is a need for reliable complementary adjunctive chair-side/point-of-care (POC) diagnostic tool in periodontitis and peri-implantitis. Lateral flow quantitative active matrix metalloproteinase (aMMP)-8 point-of-care testing (POCT) is a potential such tool with sensitivity 75–85% and specificity 80–90%. It agrees well with other independent catalytic protease activity assays of aMMP-8.
aMMP-8 as the key biomarker can be implemented in the new periodontitis and peri-implantitis disease classification. Mouthrinse aMMP-8 POCT can additionally detect prediabetes/diabetes and tissue degenerative oral side-effects of head and neck cancer radiotherapy.
Chlorhexidine and doxycycline can inhibit aMMP-8 originating from collagenolytic human neutrophils as well as from gingival crevicular fluid (GCF) of periodontitis patients
Mouthrinse aMMP-8 POCT can furthermore be utilized to identify periodontitis as a potential risk disease for coronavirus disease 2019 (COVID-19).
aMMP-8 -technology, as a systemic medical biomarker, is useful in cardiovascular diseases, diabetes, obesity, bacteremia, sepsis, meningitis, and pancreatitis.
Declaration of interest
Prof. Timo Sorsa is the inventor of U.S. 5,652,223, 5,736,341, 5,864,632, 6,143,476 and US 2017/0023571A1 (issued 6 June 2019), WO 2018/060553 A1 (issued 31 May 2018), 10,488,415 B2, and US 2017/0023671A1, Japanese Patent 2016-554,676 and South Korean patent 10-2016-7,025,378. Dr. Lorne M. Golub is listed as an inventor on several patents on host-modulation therapies and these have been fully assigned to his institution, Stony Brook University, State University of New York.
The other authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose
References
Papers of special note have been highlighted as either of interest (•) or of considerable interest (••) to readers.
- 1.Hajishengallis G, Chavakis T.. Local and systemic mechanisms linking periodontal disease and inflammatory comorbidities. Nat Rev Immunol. 2021;21(7):426–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Caton JG, Armitage G, Berglundh T, et al. A new classification scheme for periodontal and peri-implant diseases and conditions - Introduction and key changes from the 1999 classification. J Clin Periodontol. 2018;45(Suppl 20):S1–S8. [DOI] [PubMed] [Google Scholar]
- 3.Sorsa T, Gürsoy UK, Nwhator S, et al. Analysis of matrix metalloproteinases, especially MMP-8, in gingival creviclular fluid, mouthrinse and saliva for monitoring periodontal diseases. Periodontol 2000. 2016;70(1):142–163. [DOI] [PubMed] [Google Scholar]; •• Comprehensive review behind the POCT technology mentioned in the current review.
- 4.Sorsa T, Alassiri S, Grigoriadis A, et al. Active MMP-8 (aMMP-8) as a grading and staging biomarker in the periodontitis classification. Diagnostics (Basel). 2020;10(2):61. [DOI] [PMC free article] [PubMed] [Google Scholar]; •• Important work to denote aMMP-8 as the key biomarker to be implemented in the current periodontal disease classification system.
- 5.Sorsa T, Bacigalupo J, Könönen M, et al. Host-modulation therapy and chair-side diagnostics in the treatment of peri-implantitis. Biosensors (Basel). 2020;10(5):44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sorsa T, Grigoriadis A, Sakellari D, et al. On the accuracy, sensitivity and grading of mouthrinse aMMP-8 point of care testing (POCT). (A letter). J Clin Periodonl. 2021, in press. DOI: 10.1111/jcpe.13521. [DOI] [PubMed] [Google Scholar]; •• Crucial article which covers the internationally validated cut off point for aMMP-8 POCT as well as its correlation with periodontal disease.
- 7.Nwhator SO, Ayanbadejo PO, Umeizudike KA, et al. Clinical correlates of a lateral-flow immunoassay oral risk indicator. J Periodontol. 2014;85(1):188–194. [DOI] [PubMed] [Google Scholar]
- 8.Alassiri S, Pärnänen P, Rathnayake N, et al. The ability of quantitative, specific, and sensitive point-of-care/chair-side oral fluid immunotests for aMMP-8 to detect periodontal and peri-implant diseases. Dis Markers. 2018;2018:1306396. [DOI] [PMC free article] [PubMed] [Google Scholar]; •• Important work which describes the validity, sensitivity and specificity of the aMMP-8 based POCT methodology.
- 9.Leppilahti JM, Harjunmaa U, Järnstedt J, et al. Diagnosis of newly delivered mothers for periodontitis with a novel oral-rinse aMMP-8 point-of-care test in a Rural Malawian population. Diagnostics (Basel). 2018;8(3):67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lähteenmäki H, Umeizudike KA, Heikkinen AM, et al. aMMP-8 point-of-care/chairside oral fluid technology as a rapid, non-invasive tool for periodontitis and peri-implantitis screening in a medical care setting. Diagnostics (Basel). 2020;10(8):562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lupi SM, Redoglia L, Rodriguez Y Baena A, et al. Detection of peri-implant inflammation by the use of a matrix metalloproteinase-8 chair-side test. Minerva Stomatol. 2019;68(4):168–176. [DOI] [PubMed] [Google Scholar]
- 12.Räisänen IT, Sorsa T, Tervahartiala T, et al. Low association between bleeding on probing propensity and the salivary aMMP-8 levels in adolescents with gingivitis and stage I periodontitis. J Periodontal Res. 2021;56(2):289–297. [DOI] [PubMed] [Google Scholar]
- 13.Lorenz K, Keller T, Noack B, et al. Evaluation of a novel point-of-care test for active matrix metalloproteinase-8: agreement between qualitative and quantitative measurements and relation to periodontal inflammation. J Periodontal Res. 2017;52(2):277–284. [DOI] [PubMed] [Google Scholar]
- 14.Izadi Borujeni S, Mayer M, Eickholz P. Activated matrix metalloproteinase-8 in saliva as diagnostic test for periodontal disease? A case-control study. Med Microbiol Immunol. 2015;204(6):665–672. [DOI] [PubMed] [Google Scholar]
- 15.Schmalz G, Kummer MK, Kottmann T, et al. Association of chairside salivary aMMP-8 findings with periodontal risk assessment parameters in patients receiving supportive periodontal therapy. J Periodontal Implant Sci. 2018;48(4):251–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ziebolz D, Schmalz G, Gollasch D, et al. Microbiological and aMMP-8 findings depending on peri-implant disease in patients undergoing supportive implant therapy. Diagn Microbiol Infect Dis. 2017;88(1):47–52. [DOI] [PubMed] [Google Scholar]
- 17.Johnson N, Ebersole JL, Kryscio RJ, et al. Rapid assessment of salivary MMP-8 and periodontal disease using lateral flow immunoassay. Oral Dis. 2016;22(7):681–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deng K, Pelekos G, Jin L, et al. Diagnostic accuracy of a point-of-care aMMP-8 test in the discrimination of periodontal health and disease. J Clin Periodontol. 2021;48(8):1051–1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rautava J, Gürsoy UK, Kullström A, et al. An oral rinse active matrix metalloproteinase-8 point-of-care immunotest may be less accurate in patients with Crohn’s disease. Biomolecules. 2020;10(3):395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grigoriadis A, Sorsa T, Räisänen I, et al. Prediabetes/diabetes can be screened at the dental office by a low-cost and fast chair-side/point-of-care aMMP-8 Immunotest. Diagnostics (Basel). 2019;9(4):151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grigoriadis A, Räisänen IT, Pärnänen P, et al. Prediabetes/diabetes screening strategy at the periodontal clinic. Clin Exp Dent Res. 2021;7(1):85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Keskin M, Lähteenmäki H, Rathnayake N, et al. Active matrix metalloproteinase-8 and interleukin-6 detect periodontal degeneration caused by radiotherapy of head and neck cancer: a pilot study. Expert Rev Proteomics. 2020;17(10):777–784. [DOI] [PubMed] [Google Scholar]
- 23.Golub LM, Räisänen IT, Sorsa T, et al. An unexplored pharmacologic/diagnostic strategy for peri-implantitis: a protocol proposal. Diagnostics (Basel). 2020;10(12):1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vö Ö, Emingil G, Umeizudike K, et al. Evaluation of active matrix metalloproteinase-8 (aMMP-8) chair-side test as a diagnostic biomarker in the staging of periodontal diseases. Arch Oral Biol. 2021;124:105065. [DOI] [PubMed] [Google Scholar]
- 25.Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis: framework and proposal of a new classification and case definition. J Periodontol. 2018;89(Suppl 1):S159–S172. [DOI] [PubMed] [Google Scholar]
- 26.Sorsa T, Hernández M, Leppilahti J, et al. Detection of gingival crevicular fluid MMP-8 levels with different laboratory and chair-side methods. Oral Dis. 2010;16(1):39–45. [DOI] [PubMed] [Google Scholar]; •• Important as it provides evidence supporting the utilisation of GCF as a diagnostic fluid for MMP-8 detection. It is also the first paper to provide evidence that active MMP-8 is more precise than total MMP-8.
- 27.Sorsa T, Mäntylä P, Tervahartiala T, et al. MMP activation in diagnostics of periodontitis and systemic inflammation. J Clin Periodontol. 2011;38(9):817–819. [DOI] [PubMed] [Google Scholar]
- 28.Keles Yucel ZP, Afacan B, Emingil G, et al. Local and systemic levels of aMMP-8 in gingivitis and stage 3 grade C periodontitis. J Periodontal Res. 2020;55(6):887–894. [DOI] [PubMed] [Google Scholar]
- 29.Chaparro A, Realini O, Hernández M, et al. Early pregnancy levels of gingival crevicular fluid matrix metalloproteinases-8 and −9 are associated with the severity of periodontitis and the development of gestational diabetes mellitus. J Periodontol. 2021;92(2):205–215. [DOI] [PubMed] [Google Scholar]
- 30.Liukkonen J, Gűrsoy UK, Könönen E, et al. Immunological and microbiological profiling of cumulative risk score for periodontitis. Diagnostics (Basel). 2020;10(8):560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Räisänen IT, Heikkinen AM, Nwhator SO, et al. On the diagnostic discrimination ability of mouthrinse and salivary aMMP-8 point-of-care testing regarding periodontal health and disease. Diagn Microbiol Infect Dis. 2019;95(4):114871. [DOI] [PubMed] [Google Scholar]; • Important as it differentiates between mouthrinse and salivary diagnostic sampling for aMMP-8 POCT and concludes the higher precision of mouthrinse as an analyte matrix as compared to saliva.
- 32.Räisänen IT, Heikkinen AM, Pakbaznejad Esmaeili E, et al. A point-of-care test of active matrix metalloproteinase-8 predicts triggering receptor expressed on myeloid cells-1 (TREM-1) levels in saliva. J Periodontol. 2020;91(1):102–109. [DOI] [PubMed] [Google Scholar]
- 33.Gürsoy UK, Könönen E, Tervahartiala T, et al. Molecular forms and fragments of salivary MMP-8 in relation to periodontitis. J Clin Periodontol. 2018;45(12):1421–1428. [DOI] [PubMed] [Google Scholar]
- 34.Leppilahti JM, Sorsa T, Kallio MA, et al. The utility of gingival crevicular fluid matrix metalloproteinase-8 response patterns in prediction of site-level clinical treatment outcome. J Periodontol. 2015;86(6):777–787. [DOI] [PubMed] [Google Scholar]
- 35.Gul SS, Abdulkareem AA, Sha AM, et al. Diagnostic accuracy of oral fluids biomarker profile to determine the current and future status of periodontal and peri-implant diseases. Diagnostics (Basel). 2020;10(10):838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee W, Aitken S, Sodek J, et al. Evidence of a direct relationship between neutrophil collagenase activity and periodontal tissue destruction in vivo: role of active enzyme in human periodontitis. J Periodontal Res. 1995;30(1):23–33. [DOI] [PubMed] [Google Scholar]; • First paper to provide evidence of aMMP-8 [and not total MMP-8] being a predictive biomarker of progressive periodontal disease activity.
- 37.Mancini S, Romanelli R, Laschinger CA, et al. Assessment of a novel screening test for neutrophil collagenase activity in the diagnosis of periodontal diseases. J Periodontol. 1999;70(11):1292–1302. [DOI] [PubMed] [Google Scholar]
- 38.Romanelli R, Mancini S, Laschinger C, et al. Activation of neutrophil collagenase in periodontitis. Infect Immun. 1999;67(5):2319–2326. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Evidence that aMMP-8 and not total MMP-8 reflects, and is associated with periodontitis.
- 39.Uitto VJ, Suomalainen K, Sorsa T. Salivary collagenase. Origin, characteristics and relationship to periodontal health. J Periodontal Res. 1990;25(3):135–142. [DOI] [PubMed] [Google Scholar]
- 40.Mc Crudden MTC, Irwin CR, El Karim I, et al. Matrix metalloproteinase-8 activity in gingival crevicular fluid: development of a novel assay. J Periodontal Res. 2017;52(3):556–561. [DOI] [PubMed] [Google Scholar]
- 41.Leppilahti JM, Kallio MA, Tervahartiala T, et al. Gingival crevicular fluid matrix metalloproteinase-8 levels predict treatment outcome among smokers with chronic periodontitis. J Periodontol. 2014;85(2):250–260. [DOI] [PubMed] [Google Scholar]
- 42.Heikkinen AM, Raivisto T, Kettunen K, et al. Pilot study on the genetic background of an active matrix metalloproteinase-8 test in finnish adolescents. J Periodontol. 2017;88(5):464–472. [DOI] [PubMed] [Google Scholar]
- 43.Heikkinen AM, Nwhator SO, Rathnayake N, et al. Pilot study on oral health status as assessed by an active matrix metalloproteinase-8 chairside mouthrinse test in adolescents. J Periodontol. 2016;87(1):36–40. [DOI] [PubMed] [Google Scholar]
- 44.Mäntylä P, Stenman M, Kinane DF, et al. Gingival crevicular fluid collagenase-2 (MMP-8) test stick for chair-side monitoring of periodontitis. J Periodontal Res. 2003;38(4):436–439. [DOI] [PubMed] [Google Scholar]; • First paper on the site-specific aMMP-8 POCT.
- 45.Hoffmann T, Lorenz K, Netuschil L, et al. The methodological evaluation of a novel qualitative aMMP-8 chairside test as an early indicator of tissue destructive inflammatory periodontal diseases. evaluation of agreement between qualitative aMMP-8 chairside test scores and quantitative aMMP-8 ELISA measurements. [master’s thesis]. Department of Periodontology, University of Dresden; 2009. [Google Scholar]; • Estimation of cut-off at 20 ng/ml for aMMP-8 POCT.
- 46.Mäntylä P, Stenman M, Kinane D, et al. Monitoring periodontal disease status in smokers and nonsmokers using a gingival crevicular fluid matrix metalloproteinase-8-specific chair-side test. J Periodontal Res. 2006;41(6):503–512. [DOI] [PubMed] [Google Scholar]; • Site-specific aMMP-8 POCT identifies progressive periodontitis sites and patients.
- 47.Teronen O, Konttinen YT, Lindqvist C, et al. Human neutrophil collagenase MMP-8 in peri-implant sulcus fluid and its inhibition by clodronate. J Dent Res. 1997;76(9):1529–1537. [DOI] [PubMed] [Google Scholar]; • First paper to demonstrate that aMMP-8 and not total MMP-8 in PISF reflects and is associated with peri-implantitis.
- 48.Kivelä-Rajamäki MJ, Teronen OP, Maisi P, et al. Laminin-5 gamma2-chain and collagenase-2 (MMP-8) in human peri-implant sulcular fluid. Clin Oral Implants Res. 2003;14(2):158–165. [DOI] [PubMed] [Google Scholar]; • Confirms that aMMP-8 and not total MMP-8 in PISF reflects and is associated with peri-implantitis.
- 49.Kivelä-Rajamäki M, Maisi P, Srinivas R, et al. Levels and molecular forms of MMP-7 (matrilysin-1) and MMP-8 (collagenase-2) in diseased human peri-implant sulcular fluid. J Periodontal Res. 2003;38(6):583–590. [DOI] [PubMed] [Google Scholar]
- 50.Sorsa T, Tjäderhane L, Konttinen YT, et al. Matrix metalloproteinases: contribution to pathogenesis, diagnosis and treatment of periodontal inflammation. Ann Med. 2006;38(5):306–321. [DOI] [PubMed] [Google Scholar]
- 51.Xu L, Yu Z, Lee HM, et al. Characteristics of collagenase-2 from gingival crevicular fluid and peri-implant sulcular fluid in periodontitis and peri-implantitis patients: pilot study. Acta Odontol Scand. 2008;66(4):219–224. [DOI] [PubMed] [Google Scholar]
- 52.Buduneli E, Mäntylä P, Emingil G, et al. Acute myocardial infarction is reflected in salivary matrix metalloproteinase-8 activation level. J Periodontol. 2011;82(5):716–725. [DOI] [PubMed] [Google Scholar]
- 53.Al-Majid A, Alassiri S, Rathnayake N, et al. Matrix metalloproteinase-8 as an inflammatory and prevention biomarker in periodontal and peri-implant diseases. Int J Dent. 2018;2018:7891323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Thierbach R, Maier K, Sorsa T, et al. Peri-implant sulcus fluid (PISF) matrix metalloproteinase (MMP) −8 levels in peri-implantitis. J Clin Diagn Res. 2016;10(5):ZC34–38. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Treatment of dental implantitis reduces aMMP-8 in PISF.
- 55.Räisänen IT, Heikkinen AM, Siren E, et al. Point-of-care/chairside aMMP-8 analytics of periodontal diseases’ activity and episodic progression. Diagnostics (Basel). 2018;8(4):74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yakob M, Kari K, Tervahartiala T, et al. Associations of periodontal microorganisms with salivary proteins and MMP-8 in gingival crevicular fluid. J Clin Periodontol. 2012;39(3):256–263. [DOI] [PubMed] [Google Scholar]
- 57.Sorsa T, Ingman T, Suomalainen K, et al. Identification of proteases from periodontopathogenic bacteria as activators of latent human neutrophil and fibroblast-type interstitial collagenases. Infect Immun. 1992;60(11):4491–4495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sorsa T, Ding YL, Ingman T, et al. Cellular source, activation and inhibition of dental plaque collagenase. J Clin Periodontol. 1995;22(9):709–717. [DOI] [PubMed] [Google Scholar]
- 59.Nieminen MT, Listyarifah D, Hagström J, et al. Treponema denticola chymotrypsin-like proteinase may contribute to orodigestive carcinogenesis through immunomodulation. Br J Cancer. 2018;118(3):428–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gűrsoy UK, Könönen E, Pussinen PJ, et al. Use of host- and bacteria-derived salivary markers in detection of periodontitis: a cumulative approach. Dis Markers. 2011;30(6):299–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Azmak N, Atilla G, Luoto H, et al. The effect of subgingival controlled-release delivery of chlorhexidine chip on clinical parameters and matrix metalloproteinase-8 levels in gingival crevicular fluid. J Periodontol. 2002;73(6):608–615. [DOI] [PubMed] [Google Scholar]; • Chlorhexidine used as a drug for periodontal diseases, inhibits MMP-8.
- 62.Kim HD, Lee CS, Cho HJ, et al. Diagnostic ability of salivary matrix metalloproteinase-9 lateral flow test point-of-care test for periodontitis. J Clin Periodontol. 2020;47(11):1354–1361. [DOI] [PubMed] [Google Scholar]; • Demonstration of MMP-9 POCT in periodontitis.
- 63.Kido JI, Murakami S, Kitamura M, et al. Useful immunochromatographic assay of calprotectin in gingival crevicular fluid for diagnosis of diseased sites in patients with periodontal diseases. J Periodontol. 2018;89(1):67–75. [DOI] [PubMed] [Google Scholar]; • Demonstration of Calprotectin POCT in periodontitis.
- 64.Marouf N, Cai W, Said KN, et al. Association between periodontitis and severity of COVID-19 infection: a case-control study. J Clin Periodontol. 2021;48(4):483–491. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Periodontitis can be regarded as a risk disease for COVID-19 infection.
- 65.Räisänen IT, Umeizudike KA, Pärnänen P, et al. Periodontal disease and targeted prevention using aMMP-8 point-of-care oral fluid analytics in the COVID-19 era. Med Hypotheses. 2020;144:110276. [DOI] [PMC free article] [PubMed] [Google Scholar]; • aMMP-8 POCT also identifies diabetes as a potential risk disease for COVID-19 infection.
- 66.Sahni V. Battle ready for maxillofacial injuries. Injury. 2020;51(10):2325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sahni V. A protocol for the management of maxillofacial injuries in the wake of the COVID-19 pandemic. Injury. 2020;51(10):2326–2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Xu H, Zhong L, Deng J, et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020;12(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Khurshid Z, Zafar M, Khan E, et al. Human saliva can be a diagnostic tool for Zika virus detection. J Infect Public Health. 2019;12(5):601–604. [DOI] [PubMed] [Google Scholar]
- 70.Hamid H, Khurshid Z, Adanir N, et al. COVID-19 Pandemic and Role of Human Saliva as a Testing Biofluid in Point-of-Care Technology. Eur J Dent. 2020;14(S 01):S123–S129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gupta S, Sahni V. The intriguing commonality of NETosis between COVID-19 & Periodontal disease. Med Hypotheses. 2020;144:109968. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Delineates the possibility of the involvement of NETosis in the pathophysiology of COVID-19 and relates this to periodontal disease.
- 72.Addy M. Toothbrushing against coronavirus. Br Dent J. 2020;228(7):487. [DOI] [PubMed] [Google Scholar]
- 73.Harvey AP, Fuhrmeister ER, Cantrell M, et al. Longitudinal monitoring of SARS-CoV-2 RNA on high-touch surfaces in a community setting. Environ Sci Technol Lett. 2020;8:168-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Singh AK, Gupta R, Ghost A, et al. Diabetes in COVID-19: prevalence, pathophysiology, prognosis and practical considerations. Diabetes Metab Syndr. 2020;14(4):303–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kontoyiannis DP, Lewis RE. How I treat mucormycosis. Blood. 2011;118(5):1216–1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sampson V, Kamona N, Sampson A. Could there be a link between oral hygiene and the severity of SARS-CoV-2 infections? Br Dent J. 2020;228(12):971–975. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Oral hygiene disturbance predisposes to COVID-19 infection severity.
- 77.Larvin H, Wilmott S, Wu J, et al. The impact of periodontal disease on hospital admission and mortality during COVID-19 pandemic. Front Med. 2020;7:604980. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Periodontal disease is a potential risk disease for COVID-19 infection.
- 78.Cardoso EOC, Fine N, Glogauer M, et al. The advent of covid-19; periodontal research has identified therapeutic targets for severe respiratory disease; an example of parallel biomedical research agendas. Front Dent Med. 2021;2:674056. [Google Scholar]; • Host modulation treatment may be used as a useful adjunctive medication in COVID-19 infection.
- 79.Gendron R, Grenier D, Sorsa T, et al. Inhibition of the activities of matrix metalloproteinases 2, 8, and 9 by chlorhexidine. Clin Diagn Lab Immunol. 1999;6(3):437–439. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Confirms that chlorhexidine inhibits both MMP-2 and MMP-8.
- 80.Sorsa T, Suomalainen K, Helenius J, et al. Periodontal disease. (A letter). N Engl J Med. 1990;323:133–135.2163023 [Google Scholar]; • First paper to provide evidence that chlorhexidine inhibits both MMP-8 activity and MMP-8 activation.
- 81.Malek AE, Granwehr BP, Kontoyiannis DP. Doxycycline as a potential partner of COVID-19 therapies. IDCases. 2020;21:e00864. [DOI] [PMC free article] [PubMed] [Google Scholar]; • (Doxycycline via MMP-inhibition was found to be useful therapeutic agent for COVID-19 cases).
- 82.Yates PA, Newman SA, Oshry LJ, et al. Doxycycline treatment of high risk COVID-19 positive patients with comorbid pulmonary disease. Ther Adv Respir Dis. 2020;14:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Doxycycline via MMP-inhibition was found to be useful therapeutic agent for COVID-19 cases.
- 83.Payne JB, Golub LM, Stoner JA, et al. The effect of subantimicrobial-dose–doxycycline periodontal therapy on serum biomarkers of systemic inflammation: a randomized, double-masked, placebo-controlled clinical trial. J Amer Dent Assoc. 2011;142(3):262–273. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Lays emphasis on the therapeutic role low dose doxycycline may play in a re-purposed manner to manage COVID-19.
- 84.Golub LM, Payne JB, Reinhardt RA, et al. Can systemic diseases co-induce (not just exacerbate) periodontitis? A hypothetical “two-hit” model. J Dent Res. 2006;85(2):102–105. [DOI] [PubMed] [Google Scholar]
- 85.Pirilä E, Sharabi A, Salo T, et al. Matrix metalloproteinases process the laminin-5 gamma 2-chain and regulate epithelial cell migration. Biochem Biophys Res Commun. 2003;303(4):1012–1017. [DOI] [PubMed] [Google Scholar]
- 86.Emingil G, Kuula H, Pirilä E, et al. Gingival crevicular fluid laminin-5 gamma2-chain levels in periodontal disease. J Clin Periodontol. 2006;33(7):462–468. [DOI] [PubMed] [Google Scholar]
- 87.Emingil G, Atilla G, Sorsa T, et al. Effectiveness of adjunctive low-dose doxycycline therapy on clinical parameters and gingival crevicular fluid laminin-5 gamma2 chain levels in chronic periodontitis. J Periodontol. 2004;75(10):1387–1396. [DOI] [PubMed] [Google Scholar]
- 88.Gupta S, Sahni V, Räisänen IT, et al. Linking oral microbial proteolysis to aMMP-8 PoC diagnostics along with the stage and grade of periodontitis: a cross-sectional study. Oral Dis. 2021Aug17; DOI: 10.1111/odi.14008. Epub ahead of print. PMID: 34402146. [DOI] [PubMed] [Google Scholar]; •• aMMP-8 POCT can be linked to oral dysbiotic periodontopathogens microbial proteolysis.
- 89.Pärnänen P, Sorsa T, Tervahartiala T, et al. Isolation, characterization and regulation of moonlighting proteases from Candida glabrata cell wall. Microb Pathog. 2020;149:104547. [DOI] [PubMed] [Google Scholar]
- 90.Lauhio A, Hästbacka J, Pettilä V, et al. Serum MMP-8, −9 and TIMP-1 in sepsis: high serum levels of MMP-8 and TIMP-1 are associated with fatal outcome in a multicentre, prospective cohort study. Hypothetical impact of tetracyclines. Pharmacol Res. 2011;64(6):590–594. [DOI] [PubMed] [Google Scholar]
- 91.Lauhio A, Färkkilä E, Pietiläinen KH, et al. Association of MMP-8 with obesity, smoking and insulin resistance. Eur J Clin Invest. 2016;46(9):757–765. [DOI] [PubMed] [Google Scholar]
- 92.Tuomainen AM, Nyyssönen K, Laukkanen JA, et al. Serum matrix metalloproteinase-8 concentrations are associated with cardiovascular outcome in men. Arterioscler Thromb Vasc Biol. 2007;27(12):2722–2728. [DOI] [PubMed] [Google Scholar]
- 93.Savonius O, Roine I, Alassiri S, et al. The potential role of matrix metalloproteinases 8 and 9 and myeloperoxidase in predicting outcomes of bacterial meningitis of childhood. Mediators Inflamm. 2019;2019:7436932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Forsblom E, Tervahartiala T, Ruotsalainen E, et al. Matrix metalloproteinase MMP-8, TIMP-1 and MMP-8/TIMP-1 ratio in plasma in methicillin-sensitive Staphylococcus aureus bacteremia. PLoS One. 2021;16(5):e0252046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Turunen A, Kuuliala K, Kuuliala A, et al. Activated matrix metalloproteinase 8 in serum predicts severity of acute pancreatitis. Pancreatology. 2021;7:S1424–3903. [DOI] [PubMed] [Google Scholar]
- 96.Gupta S, Mohindra R, Singla M, et al. The clinical association between periodontitis and COVID-19. Clin Oral Investig. 2021, In press. DOI: 10.1007/s00784-021-04111-3. [DOI] [PMC free article] [PubMed] [Google Scholar]; •• Periodontitis can be regarded as a risk disease for COVID-19 infection.


