Abstract
Background
Most stroke survivors have sustained upper limb impairment in their distal joints. An electromyography (EMG)-driven wrist/hand exoneuromusculoskeleton (WH-ENMS) was developed previously. The present study investigated the feasibility of a home-based self-help telerehabilitation program assisted by the aforementioned EMG-driven WH-ENMS and its rehabilitation effects after stroke.
Methods
Persons with chronic stroke (n = 11) were recruited in a single-group trial. The training progress, including the training frequency and duration, was telemonitored. The clinical outcomes were evaluated using the Fugl–Meyer Assessment (FMA), Action Research Arm Test (ARAT), Wolf Motor Function Test (WMFT), Motor Functional Independence Measure (FIM), and Modified Ashworth Scale (MAS). Improvement in muscle coordination was investigated in terms of the EMG activation level and the Co-contraction Index (CI) of the target muscles, including the abductor pollicis brevis (APB), flexor carpi radialis-flexor digitorum (FCR-FD), extensor carpi ulnaris-extensor digitorum (ECU-ED), biceps brachii (BIC), and triceps brachii (TRI). The movement smoothness and compensatory trunk movement were evaluated in terms of the following two kinematic parameters: number of movement units (NMUs) and maximal trunk displacement (MTD). The above evaluations were conducted before and after the training.
Results
All of the participants completed the home-based program with an intensity of 63.0 ± 1.90 (mean ± SD) min/session and 3.73 ± 0.75 (mean ± SD) sessions/week. After the training, motor improvements in the entire upper limb were found, as indicated by the significant improvements (P < 0.05) in the FMA, ARAT, WMFT, and MAS; significant decreases (P < 0.05) in the EMG activation levels of the APB and FCR-FD; significant decreases (P < 0.05) in the CI of the ECU–ED/FCR–FD, ECU–ED/BIC, FCR–FD/APB, FCR–FD/BIC, FCR–FD/TRI, APB/BIC and BIC/TRI muscle pairs; and significant reductions (P < 0.05) in the NMUs and MTD.
Conclusions
The results suggested that the home-based self-help telerehabilitation program assisted by EMG-driven WH-ENMS is feasible and effective for improving the motor function of the paretic upper limb after stroke.
Trial registration ClinicalTrials.gov. NCT03752775; Date of registration: November 20, 2018.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12984-021-00930-3.
Keywords: Stroke, Robot, Rehabilitation, Home training, Telerehabilitation
Introduction
Most patients with stroke who are discharged home from inpatient poststroke rehabilitation have residual motor impairment of the upper limb, especially in the distal joints (i.e., the wrist and the fingers), which greatly inhibits their ability to perform activities of daily living (ADLs) [1, 2]. Although the traditional viewpoint on poststroke rehabilitation suggested that significant motor recovery mainly occurs in the first 6 months after the onset of a stroke (i.e., acute and subacute periods) [3], more recent studies have indicated that significant motor improvements could also be achieved in the chronic period after stroke through physical training as long as such training is as intensive as the one provided to inpatients [4, 5]. Continuous and regular physical therapy is required to improve the wrist/hand function of outpatients with chronic stroke [6]. The restoration of limb function after stroke depends on intensive and repetitive training of the paralyzed limb [7, 8] with maximized voluntary motor effort [9, 10] and minimized compensatory motions in close-to-normal muscular coordination [10, 11]. However, the provision of effective wrist/hand rehabilitation services for outpatients with chronic stroke is insufficient in the current healthcare system in the world.
In most cases, outpatients have limited access to wrist/hand treatments with the necessary training intensity [12, 13] because of resource constraints due to factors such as an expanding stroke population and a lack of professionals worldwide [14, 15], as well as other difficulties such as commuting [2] to the outpatient services in day hospitals, and the restriction of social distancing during the COVID-19 pandemic. Home-based telerehabilitation with minimum assistance and remote supervision by professionals (i.e., self-help operation) is a promising approach for sustaining of physical treatment after discharge and enhancing the accessibility of rehabilitation resources to improve the wrist/hand motor functions of discharged patients [16–18].
However, few studies have focused on techniques for effective self-help upper limb rehabilitation, especially for distal joints [16]. Currently, most studies on home-based telerehabilitation have been based on virtual reality (VR) techniques because home-based VR training is more convenient for and accessible to outpatients than conventional therapy in a clinic or day hospital [16, 19]. Nevertheless, those systems focus on assessment or monitoring of limb performance rather than providing the necessary physical assistance for the patients to achieve the desired movements [16, 20–24]. Rehabilitation robots have been developed to provide mechanical assistance that mimics physical support from a therapist in conventional therapy; these robots can alleviate the labor-intensive aspects of hands-on physical therapy by performing repetitive therapeutic tasks intensively under the supervision of a therapist [15], and these robotic therapies for distal joints have been reported to be effective for improving upper limb motor function [1, 25]. However, the majority of the existing rehabilitation robots are heavy, have complex mechanical designs, and require large power supplies, large physical spaces in conventional environments (e.g., clinic), and close professional supervision, which are significant deterrents to their use by patients independently at home [15, 26].
Furthermore, using robot alone has a limitation in directly activating the desired muscle groups because the target muscles of patients with stroke usually cooperate with compensatory motions from other muscular activities [27]. Compensatory motions from the trunk and the proximal joints, i.e., abnormal motor synergies, are commonly observed in most persons with chronic stroke when they attempt to reach an object or orient their hand to grasp an object [28]. When neuromuscular electrical stimulation (NMES) combined with robotic therapy, the robotic assistance could provide sensorimotor experiences with precise kinematics to realize the desired movements [29], and NMES could activate the target muscles and reduce compensation from alternative muscle synergies [30]. Thus, the combined NMES-robot treatment has been suggested to facilitate close-to-normal muscular coordination with reduced compensation motions, and it has yielded more effective rehabilitation outcomes than upper limb rehabilitation treatments that use only NMES or only robots [31]. Electromyography (EMG) of the paralyzed limb to indicate voluntary intention to integrate voluntary motor effort during practice has been recommended for optimizing therapeutic outcomes [32]. EMG-driven training systems have yielded superior improvements in motor functions with longer sustainability than those with passive limb motions [33], especially for voluntary motor control of the upper limb. Therefore, EMG-driven NMES-robot therapy for home-based self-help training is desirable for effective wrist/hand rehabilitation for outpatients with chronic stroke.
A novel EMG-driven exoneuromusculoskeleton (ENMS) for self-help upper limb rehabilitation after stroke was developed recently by our team [34, 35]. Taking the advantages of exoskeleton, pneumatic muscle, and NMES, the developed system is lightweight, compact, and has low power consumption. The system can assist the extension and flexion of the elbow, wrist, and finger joints under voluntary effort control through EMG. The system consists of an elbow module and a wrist/hand module that can work collectively or separately. The wrist/hand module can work independently as an EMG-driven wrist/hand ENMS (WH-ENMS) to assist wrist/hand movements during training (Fig. 1). The rehabilitation effects of the EMG-driven ENMS have been investigated in 15 participants with chronic stroke [35], followed by a 20-session training program in a neurorehabilitation laboratory, where the participants completed the training independently with the system after they received a tutorial session and three guided training sessions (including practicing device operation and training setup). The participants exhibited significant improvements in voluntary motor control and muscle coordination of the paretic limb after the EMG-driven ENMS-assisted upper limb training [35]. No safety problems were reported by either the experiment operators or the participants throughout the study period. The system offers the possibility of home-based self-help wrist/hand training for discharged patients with chronic stroke. However, the feasibility of using the EMG-driven WH-ENMS for self-help upper limb training and its rehabilitation effects in a home setting had not been investigated.
Fig. 1.
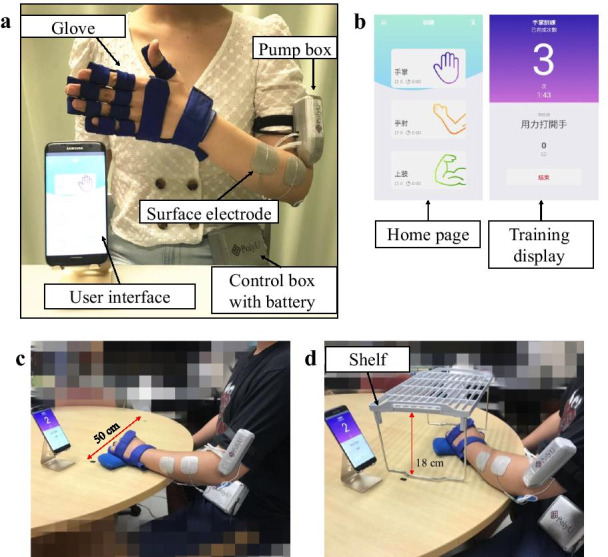
Experimental and training set up of the EMG-driven WH-ENMS. a Photograph of the EMG-driven WH-ENMS and b the screen captures of the interface. The training set up in a session assisted by the EMG-driven WH-ENMS and configuration of c the horizontal task and d vertical task
Therefore, in this study, we aimed to determine the feasibility of home-based self-help training assisted by the EMG-driven WH-ENMS on outpatients with chronic stroke and investigate its rehabilitation effects. Our hypothesis was that the participants who received the home-based self-help telerehabilitation training assisted by the EMG-driven WH-ENMS would obtain motor improvements in the distal joints, better muscle coordination of the paretic upper limb, and reduce compensatory movements when performing limb tasks.
Methods
A single-group trial was conducted on discharged patients with chronic stroke (n = 11) who underwent a home-based self-help telerehabilitation program consisting of 20 sessions of wrist/hand training assisted by the EMG-driven WH-ENMS. The training outcomes were evaluated through clinical assessments, EMG evaluations and kinematic analysis.
EMG-driven WH-ENMS
The EMG-driven WH-ENMS used in this study is shown in Fig. 1a, b. The system can be worn on the paretic upper limb and assist a stroke survivor in performing phasic wrist/hand coordinated movements, namely (1) wrist extension with the hand open and (2) wrist flexion with the hand close.
The system consists of a wearable glove with a textile bracing on the hand, a pump box mounted on the upper arm and a control box carried on the waist. A rechargeable 12-V Li-ion battery inside the control box can support continuous system usage for 4 h. The wearable glove with the embedded musculoskeletal hand comprises five pneumatic finger muscles and a three-dimensional printed exoskeletal connector fixed on the palm side. The pneumatic muscles can provide extension torque to individual digits during inflation, and it deflated when the valve is opened. Each pneumatic muscle can generate a maximal extension torque of 0.1 Nm across the MCP joint of a finger when its inner pressure reaches 96 kPa [35]. Two-channel NMES was applied to the wrist/finger extensors (i.e., the extensor carpi ulnaris (ECU) and the extensor digitorum (ED)) and flexors (i.e., the flexor carpi radialis (FCR) and the flexor digitorum (FD)) to assist wrist/finger extension and flexion, respectively, through two pairs of reusable surface electrodes (5 × 5 cm2, PALS Neurostimulation Electrodes, Axelgaard Manufacturing Co., Ltd., Fallbrook, CA, USA). The muscles of the ECU and ED and the muscles of the FCR and FD were treated as an ECU-ED muscle union and a FCR -FD muscle union, respectively, for both NMES and EMG detection in this study due to the close anatomical proximity between the FCR and FD muscles and between the ECU and ED muscles [36]. The NMES outputs were square pulses with a constant amplitude of 70 V, stimulation frequency of 40 Hz, and a manually adjustable pulse width in the range of 0–300 µs (with a threshold pulse width to evoke maximal muscle contraction) [35]. A pair of surface electrodes was used for both EMG detection and NMES delivery to a target muscle union, and these electrodes were located in the common area of the motor point of the two muscle bellies of the muscle union [35]. A reference electrode (2 × 3 cm2, Blue Sensor N, Ambu Inc., Ballerup, Denmark) was attached to the skin surface of the olecranon to attenuate the common mode noise.
To facilitate the phasic wrist/hand movements, the ECU-ED and FCR -FD muscle unions were used as voluntary neuromuscular drives to control mechanical assistance and NMES assistance from the system. EMG-triggered control was adopted in this study [35]. Three times the standard deviation (SD) above the EMG baseline in the resting state was set as the threshold level in each motion phase. In the “wrist extension with the hand open” phase, once the EMG activation level of the ECU-ED reached the preset threshold, NMES was applied to the ECU-ED and mechanical extension torque was provided to the fingers by the inflated pneumatic finger muscles to assist joint extension of the wrist and the fingers throughout the motion phase. In the “wrist flexion with the hand close” phase, as soon as the EMG activation level of the FCR -FD reached the preset threshold, the pneumatic finger muscles were deflated passively and NMES was applied to the FCR-FD to assist joint flexion of the wrist and the fingers throughout the motion phase. The residual voluntary effort from the finger flexors of the paretic limb can facilitate the release of air from the pneumatic muscles during deflation. A detailed description of the assistive control can be found in our previous study on the design of the EMG-driven ENMS for poststroke rehabilitation [35].
The captured EMG signals were first amplified 1000 times (preamplifier: INA 333; Texas Instruments Inc., Dallas, TX, USA) and filtered from 10 to 500 Hz. These amplified and filtered signals were then sampled using an analog-to-digital converter (AD73360, Analog Devices Inc., Norwood, MA, USA) with a sampling frequency of 1000 Hz for each EMG channel. After digitization, the EMG signals were full-wave rectified and moving-averaged with 100-ms window to obtain the EMG activation level during real-time control [35].
Real-time control and wireless communication between the control unit and a mobile android application (app) were achieved on a smartphone by using a microprocessor and a Bluetooth module (Bluetooth HC-05, JMoon Technologies., New Delhi, India). The app was designed as the user interface to communicate with the system and provide visual indications to patients. The designed app emphasized patient convenience, ease of use, large-font instructions with clear options, and straightforward navigation for user-independent operation. A patient can start or stop a training session by simply tapping the button in the app interface. In addition, an emergency stop button of the battery power supply to the control box was also provided as the single switch of the control box to simplify system operation, and to shut down the system in case of an emergency. The training data was recorded by the app and transmitted to the server computer located in the laboratory through a mobile network of 3G or above automatically after a user had exited the app, for telemonitoring the training progress.
Home-based training program
Subject recruitment
After obtaining the ethical approval from the Human Subjects Ethics Subcommittee of the Hong Kong Polytechnic University, a total of 15 participants from local districts were screened. Eleven participants with chronic stroke were recruited in this study. The inclusion criteria included (1) at least 1 year after the onset of a singular and unilateral brain lesion due to stroke, (2) discharge from hospital, (3) the spasticity at the elbow, wrist and fingers were ≤ 3 as measured by the Modified Ashworth Scale (MAS) [37], (4) motor impairments in the affected upper limb ranging from severe to moderate according to the Fugl-Meyer Assessment (FMA; 15 < FMA < 45, with a maximal score of 66 for the upper limb) [38], (5) no visual deficits and the ability to understand and follow simple instructions, as assessed by the Mini-Mental State Examination (MMSE > 21) [39], (6) presence of detectable voluntary EMG signals from the driving muscle on the affected side (three times the SD above the EMG baseline), (7) presence of active ROM of shoulder from 30° to 80° flexion, (8) presence of passive ROM of wrist from 45° extension to 60° flexion, and the ability of the MCP finger joints to be passively extended to 170°, (9) fulfillment of minimum living environment requirements, including a table measuring at least with 60 × 40 cm2 as the training space, a bridge chair without wheels, and a 3G or above mobile network coverage at home. Subjects were excluded if they (1) were currently pregnant, (2) were epileptic or (3) had an implanted pacemaker. Before the commencement of the clinical trial, written informed consent was obtained from each participant. Figure 2 shows the Consolidated Standards of Reporting Trials flowchart of the experimental design.
Fig. 2.
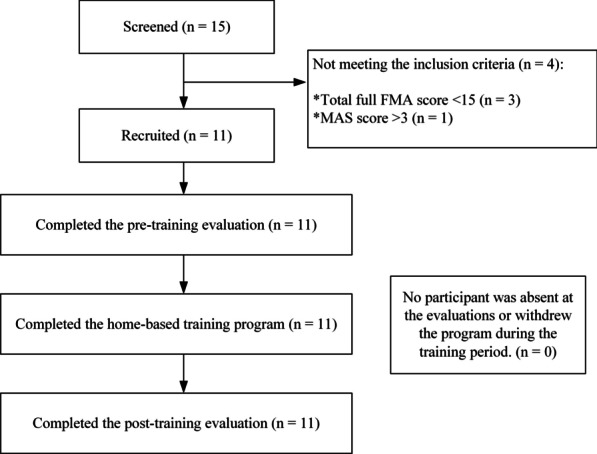
The Consolidated Standards of Reporting Trials flowchart of the experimental design
Interventions
The rehabilitation program consisted of a pre-training tutorial and a 20-session upper limb training assisted by the EMG-driven WH-ENMS (at least 60 min/session), with the intensity of 3–5 sessions/week, within 7 consecutive weeks, and with no more than 1 session/day.
Before the training, a pre-training tutorial lasting 30 to 45 min on donning and doffing the system, device operation and the training protocol was provided to each participant. The procedure of the pre-training tutorial is shown in Fig. 3. If any participant was not using an Android smartphone or if they did not have a smartphone, they were lent an Android smartphone with the developed app until they completed the training program. Regarding the setting of training parameters, the operator set the training parameters i.e., the EMG triggering levels of the driving muscle unions, maximum inner pressure of the wrist/hand module, and the applied pulse width of NMES for individual participants. These parameters remained fixed throughout the 20-session training. The maximal inner pressure of the wrist/hand module was set to < 100 kPa during training, to ensure stability of the pneumatic muscles under repeated inflations and deflations. When placing surface electrodes and reference electrode on the participant’s arm, the operator marked those positions on the participant’s skin and instructed the participants to retain these markings until the last session. Once the electrode position markings faded, the participants were required to remark them with a marker pen or a ballpoint pen. Moreover, safety instructions were provided during the tutorial.
Fig. 3.
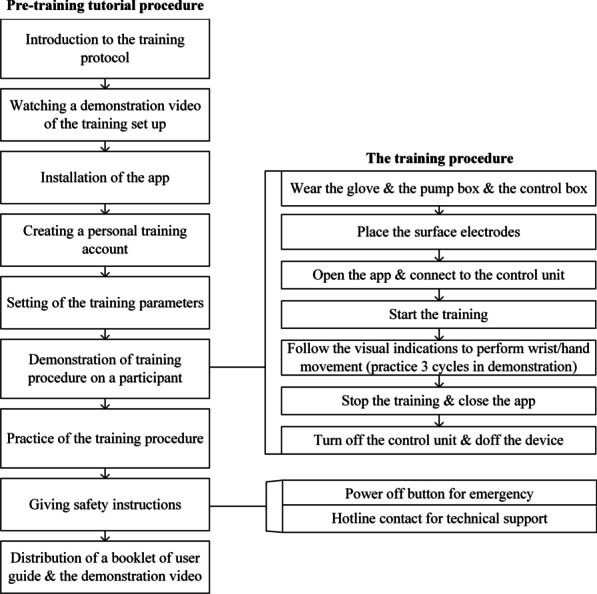
Pre-training tutorial procedure
The training started within 3 days after the tutorial. In each training session, the participants were required to sit at a table and to maintain a vertical distance of 30–40 cm between the table surface and their shoulder (Fig. 1c, d). The smartphone with the app was positioned on the table and placed in front of the participant at a horizontal distance of 30–60 cm. The participants were required to follow the visual indications displayed on the smartphone screen and perform the repetitive limb tasks assisted by the EMG-driven WH-ENMS on the paretic limb. The participants were then required to perform 30-min horizontal task and 30-min vertical task (Table 1) at their natural speed. A 10-min rest between two consecutive tasks was allowed to prevent muscle fatigue during training sessions.
Table 1.
Descriptions of the required upper limb movements for motion tasks
| Task | Description |
|---|---|
| Horizontal | A participant was instructed to grasp a sponge that was placed on one side of a table near the paretic side of the participant, transport the sponge 50 cm horizontally (i.e., horizontal transportation phase I), release it, grasp it again, move it back to the starting point (i.e., horizontal transportation phase II), and release it |
| Vertical | A participant was instructed to grasp the sponge on the table surface, lift it up (i.e., vertical transportation phase I), place it on the top of the shelf (with a vertical distance of 18 cm), grasp it again, place it back on the table surface (i.e., vertical transportation phase II), and release it |
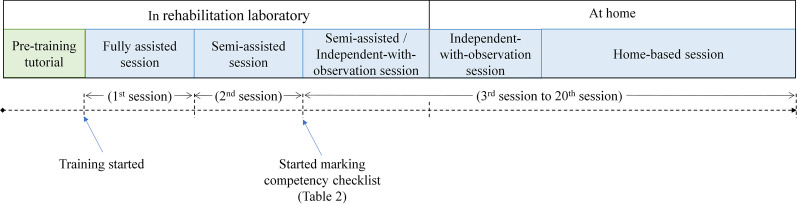
In this study, the first three training sessions were conducted in the rehabilitation laboratory and were supervised by the experiment operator to reinforce and test the competency of the participants in performing home-based self-help training. In the supervised sessions, nearby professional assistance was provided at varying levels, namely (1) fully assisted, where the operator supported the participants from the training setup and supervised the entire training process in the first session; (2) semi-assisted, where the participants completed the session mainly by themselves, with minimum assistance from the operator in the second session; and (3) independent-with-observation, where the participants completed the training session independently under close observation by the operator. An additional semi-assisted session was offered to participants who were not ready for the independent-with-observation session. During the third session, the operator marked the competency checklist (Table 2) to assess the participant’s competency in conducting home-based training with the system. Once the participants correctly demonstrated all of the technical items listed on the competency checklist, they were required to start the home-based training for the remaining sessions. If a participant had a personal caregiver, the caregiver was also invited to attend the tutorial and training sessions and allowed to provide assistance with the setup. Figure 4 shows the timeline of the EMG-driven WH-ENMS-assisted home-based self-help upper limb training program.
Table 2.
Competency checklist
| Is the participant able to demonstrate the following abilities appropriately when using the system? | Yes | No |
|---|---|---|
| Don and doff the device | ||
| Turn on and turn off the device | ||
| Login and logout of the personal training account | ||
| Connect the app and the device | ||
| Attach the electrodes onto their arm | ||
| Start and stop the training | ||
| Recharge the device | ||
| Is the participant able to demonstrate the following abilities appropriately during the training? | Yes | No |
| Safely and correctly perform all of the training tasks in a session | ||
| Place two markers at a horizontal distance of 50 cm on the table for the horizontal task | ||
| Place the shelf with the correct setting for the vertical tasks | ||
| Understand the safety precautions and warnings associated with device usage during training | ||
|
If the participant joins with a caregiver, the caregiver is allowed to assist with the training setup If the answer is “No” for any item, the participant is deemed to be not competent to perform the home-based training with the system. Otherwise, the participant is deemed as competent Experiment operator: ______________________ Signature: _____________________ Date: Number of current session: |
Fig. 4.
Timeline of the EMG-driven WH-ENMS-assisted home-based self-help upper limb training program
Logistics Management of Home-based Training
Prior to the commencement of the home-based training, the operator first arranged the training schedules for the remaining sessions agreed by a participant, and subsequently delivered the system with a battery charger and training props (e.g., a sponge and a shelf) to the participants’ homes. In the first home-based session, the operator visited the participants’ homes to inspect environmental safety (e.g., training space and nearby electricity) and then observed the entire session to ensure consistency with the session in the laboratory. The participants were required to complete the remaining sessions at home without on-site professional supervision (home-based sessions). The participants could change the training schedule occasionally by informing the operator 1 day in advance so that the operator could arrange a make-up session for the participant without violating the protocol intensity, i.e., 3–5 sessions/week. Finally, the participants were required to return the system to the research team during their post-training evaluation visit to the laboratory, which was scheduled 1 day after the last training session.
The logistics management data recorded by the developed app, including the number of completed wrist/hand movement cycles, total training time, and completion date/time point of a session, were automatically transmitted via a mobile network to the server computer located in the laboratory. The data were reviewed by the operator through an encrypted network which required the operator to enter a pre-set login account and password [40], for telemonitoring the training progress of the participants. The experiment operator remotely monitored the completion of each home-based session based on the participants’ commitment to the training schedule. Once a missing session was found, the operators contacted the participant by telephone to schedule a make-up session.
If there was any technical issue during the home-based sessions, the participants were able to inform the experiment operator immediately through a phone call or a message. A backup system was prepared for each participant and used to replace the malfunctioning system. The participants were required to return the malfunctioning system to the laboratory and have it replaced with the backup system in 1 working day.
Evaluation of training outcomes
Clinical assessments, EMG measurements, and kinematic measurements were adopted to investigate the rehabilitation outcomes of the home-based self-help upper limb training assisted by the EMG-driven WH-ENMS. All evaluations were conducted at the laboratory. All of the participants underwent evaluations just before the pre-training tutorial (i.e., pre-training evaluation) and 1 day after the last training session (i.e., post-training evaluation).
Clinical assessments for functional evaluation
In this study, clinical assessments were used to evaluate the motor functional improvements of each participant and were conducted by a training-blinded assessor. The adopted clinical assessments included (1) the FMA that the full score is 66 for the upper limb assessment, which has been sub-scaled into shoulder/elbow (42/66) and wrist/hand (24/66) [41], was adopted to measure the motor functional impairment in voluntary limb movements; (2) the Action Research Arm Test (ARAT) [42], was applied to evaluate the upper limb voluntary functions with a focus on the finger activities; (3) the Wolf Motor Function Test (WMFT) [43], was used to assess the functional ability and motion speed of the upper limb in daily tasks; (4) the Motor Functional Independence Measure (FIM) [44], was adopted to evaluate the basic quality of participant’s ADLs; and (5) the MAS [37] on the flexors related to the elbow, wrist, and fingers, was used to measure the poststroke spasticity at the related joints.
Evaluation of muscular coordination in the upper limb by EMG
Two EMG parameters were used to obtain quantitative information on the muscle activation and coordination patterns of the paretic limb. They were (1) the EMG activation level of each target muscle and (2) the EMG co-contraction index (CI) between muscle pairs [45, 46]. More details of the EMG measurement are described in Additional file 1: Appendix S1 Part A with experimental setup shown in Fig. 5.
Fig. 5.
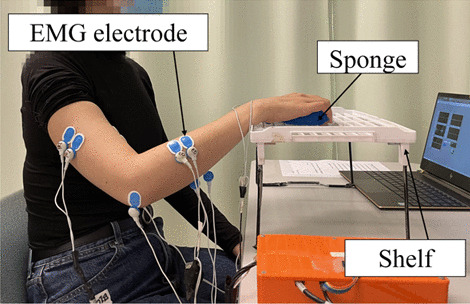
Configuration of EMG recording during the bare arm test
Evaluation of movement smoothness and compensatory trunk movement
Three-dimensional motion analysis was performed to quantify the kinematic performance of the upper limb, and this was used as an outcome measure to evaluate impaired movement after stroke [47, 48]. Two kinematic parameters, (1) number of movement units (NMUs) and (2) maximal trunk displacement (MTD) [49, 50], were adopted to obtain quantitative information about movement smoothness and compensatory trunk movement. More details of the kinematic measurement are shown in Additional file 1: Appendix S1 Part B with experimental setup shown in Fig. 6.
Fig. 6.
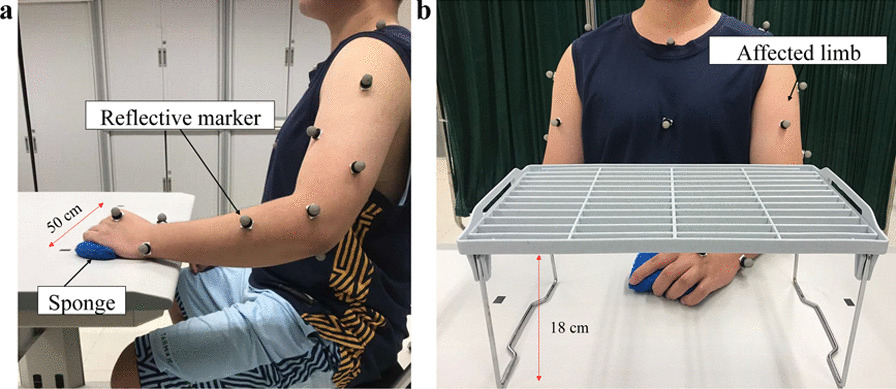
Experimental setup for a the horizontal task and b vertical task during three-dimensional motion capturing
Statistics
The normality tests on the clinical scores, EMG parameters and kinematic parameters were evaluated using the Shapiro test with a significance level of 0.05 [51, 52]. The MAS exhibited significance in the normality test (P < 0.05), and the FMA, ARAT, WMFT, FIM, EMG parameters and kinematic parameters exhibited nonsignificant probabilities (P > 0.05). Wilcoxon’s signed rank test was performed on the MAS using a paired comparison of the scores before and after the training. Paired-sample t test was used to detect the differences in the FMA, ARAT, WMFT, FIM, EMG data and kinematic data before and after the training. The primary outcome of this study was the FMA. The other clinical scores, EMG parameters, and kinematic parameters were secondary outcomes. The statistically significant level of 0.05 was used for all tests in this study. The significance levels at 0.01 and 0.001 were indicated as well.
Results
All of the recruited participants (n = 11) completed the home-based self-help upper limb training assisted by the EMG-driven WH-ENMS. The demographic data of the participants are shown in Table 3. The demographic characteristics of each participant are shown in Table S1A in Additional file 2: Appendix S2.
Table 3.
Demographic characteristics of the patients with stroke recruited for the home-based self-help upper limb training program (n = 11)
| Subject No. | Gender Female/Male |
Stroke Types Hemorrhagic/ Ischemic |
Side of Hemiparesis Left/ Right |
Age (years) Mean ± SD |
Years after onset of stroke Mean ± SD |
|---|---|---|---|---|---|
| 11 | 6/5 | 5/6 | 8/3 | 57.6 ± 13.2 | 13.4 ± 10.4 |
Independency in self-help upper limb training at home
In this study, all of the participants were determined as having sufficient competence to perform the home-based training after the third session, and no additional semi-assisted session was required by them. Six of the participants completed the training at home independently, whereas the others completed the training with partial assistance from their caregivers at home. Four of the participants conducted and completed the home-based self-help training during the COVID-19 pandemic in Hong Kong. No adverse event (e.g., pain or injury) during or after the training was reported by either the experiment operators or the participants throughout the study period.
According to the logistic data captured using the app, the average training frequency in the 20-session training was 3.73 ± 0.75 (mean ± SD) sessions/week, with a range of 3–5 sessions/week. Variability was observed in the duration of the home-based training, with an average session duration of 63.0 ± 1.90 (mean ± SD) min/session (ranging from 60 to 66 min/session), and average complete wrist/hand movement cycles per session of 116 ± 8.72 (mean ± SD). More details of the recorded logistic data are shown in Table S1B in Additional file 2: Appendix S2. The earliest and latest training times were 07:00 and 22:00, respectively. The peak training hours were between 14:00 to 16:00 and 19:00 to 21:00, with more than 80% of the home-based sessions being conducted during those periods. Five participants encountered technical issues during the home-based training sessions, among which three were related to broken leads because of excessive pulling on the leads and two were related to air leakage from the musculoskeleton hand due to hard and repeated squeezing of the pneumatic muscles during inflation. These problems were solved within 1 working day, and the related components were further reinforced. Furthermore, the malfunctioning systems were also replaced with backup systems within 1 working day.
Training outcomes of the home-based self-help program
Clinical assessments
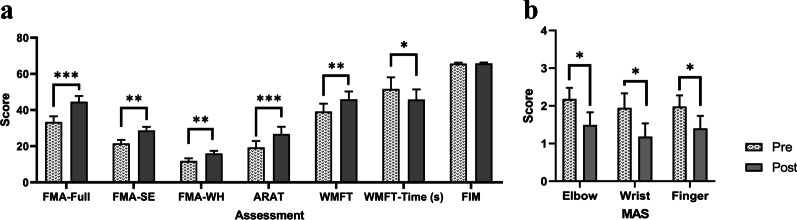
Table 4 lists all of the clinical scores measured in this study (i.e., the means and 95% confidence intervals of each clinical assessment, together with the paired-sample t test/ Wilcoxon’s signed rank test probabilities with effect sizes (EFs) for evaluations before and after the training). The comparison of the clinical scores measured before and after the training is shown in Fig. 7. In Fig. 7a, a significant increase was found after the training in the FMA full score, FMA shoulder/elbow, FMA wrist/hand, ARAT, WMFT score, and WMFT time (P < 0.05, paired-sample t test). In Fig. 7b, a significant decrease in the MAS scores was observed after the training at the elbow, the wrist and the fingers (P < 0.05, Wilcoxon’s signed rank test). The individual outcomes of clinical scores of each participant are shown in Table S1C in Additional file 2: Appendix S2.
Table 4.
Means and 95% confidence intervals of each measurement in the clinical assessments and the probabilities and estimated effect sizes in the statistical analyses. Differences with statistical significance are denoted by * (P ≤ 0.05), ** (P ≤ 0.01), and *** (P ≤ 0.001)
| Evaluation | Pre | Post | Change () | Paired-sample t test | |
|---|---|---|---|---|---|
| Mean (95% Confidence interval) | P-value | Cohen's d | |||
| FMA | |||||
| Full Score | 33.4 (30.2 to 39.7) | 44.5 (41.3 to 51.0) | 11.2 (7.53 to 14.8) | < 0.001*** | 1.84 |
| Shoulder/Elbow | 21.5 (19.6 to 25.4) | 28.6 (26.6 to 32.7) | 7.10 (3.78 to 10.4) | 0.002** | 1.29 |
| Wrist/Hand | 11.8 (10.3 to 14.8) | 15.9 (14.4 to 18.9) | 4.10 (2.18 to 6.00) | 0.002** | 1.29 |
| ARAT | 19.3 (15.7 to 26.5) | 26.7 (22.7 to 34.8) | 7.45 (4.09 to 10.8) | 0.001*** | 1.34 |
| WMFT | |||||
| Score | 39.2 (34.8 to 47.9) | 45.9 (41.6 to 54.6) | 6.72 (3.23 to 10.2) | 0.003** | 1.16 |
| Time | 51.6 (45.2 to 64.5) | 45.7 (40.1 to 57.0) | − 5.89 (− 10.7 to − 1.12) | 0.033* | − 0.75 |
| FIM | 65.6 (65.1 to 66.8) | 65.7 (65.2 to 66.9) | 0.09 (− 0.09 to 0.27) | 0.341 | 0.30 |
| MAS | Wilcoxon’s signed ranks test | ||||
|---|---|---|---|---|---|
| P-value | r | ||||
| Elbow | 2.18 (1.59 to 2.77) | 1.49 (0.82 to 2.17) | − 0.69 (− 1.16 to − 0.22) | 0.026* | − 0.67 |
| Wrist | 1.95 (1.17 to 2.72) | 1.18 (0.48 to 1.89) | − 0.76 (− 1.35 to − 0.17) | 0.026* | − 0.67 |
| Finger | 1.98 (1.39 to 2.58) | 1.40 (0.73 to 2.07) | − 0.58 (− 0.98 to − 0.18) | 0.024* | − 0.68 |
Fig. 7.
The measured clinical scores of the a FMA, ARAT, WMFT and FIM, and b the MAS before (Pre) and after (Post) the training represented by means and standard errors. Significance levels are indicated by * (P ≤ 0.05), ** (P ≤ 0.01), and *** (P ≤ 0.001)
EMG parameters
Table 5 lists the measured EMG parameters (i.e., the means and 95% confidence intervals of each clinical assessment, together with the paired-sample t test probabilities with EFs of the evaluation before and after the training). Figure 8 illustrates the EMG parameters (i.e., the normalized EMG activation level and the normalized CI) that were statistically significant before and after the training. A significant decrease in EMG activation level was detected in the APB and FCR-FD (P < 0.05) after the training (Fig. 8a). A significant reduction of CI in the muscle pairs of ECU-ED/FCR-FD, ECU-ED/BIC, FCR-FD/APB, FCR-FD/BIC, FCR-FD/TRI, APB/BIC and BIC/TRI (P < 0.05) was found after the training (Fig. 8b). No significant increase or decrease was observed in the EMG parameters of the other target muscles and muscle pairs.
Table 5.
Means and 95% confidence intervals of each measurement in the EMG parameters as well as the probabilities and estimated effect sizes in the statistical analyses. Differences with statistical significance are denoted by * (P ≤ 0.05), ** (P ≤ 0.01), and *** (P ≤ 0.001)
| EMG parameters | Pre | Post | Change () | Paired-sample t test | |
|---|---|---|---|---|---|
| Mean (95% Confidence interval) (%) | P-value | Cohen's d | |||
| Normalized EMG activation level | |||||
| APB | 10.8 (7.61 to 14.1) | 6.25 (3.60 to 8.91) | − 4.59 (− 6.95 to − 2.23) | 0.001*** | − 0.83 |
| ECU-ED | 9.84 (7.45 to 12.2) | 7.44 (5.20 to 9.68) | − 2.40 (− 5.78 to 0.98) | 0.17 | − 0.30 |
| FCR-FD | 6.52 (4.73 to 8.32) | 3.21 (2.26 to 4.16) | − 3.31 (− 4.72 to − 1.90) | < 0.001*** | − 1.00 |
| BIC | 7.71 (5.92 to 9.49) | 6.12 (4.89 to 7.36) | − 1.58 (− 3.45 to 0.28) | 0.11 | − 0.36 |
| TRI | 7.05 (3.89 to 10.20) | 5.77 (3.32 to 8.23) | − 1.27 (− 4.81 to 2.26) | 0.48 | − 0.15 |
| Normalized CI | |||||
| APB/ ECU-ED | 7.19 (4.65 to 9.72) | 4.94 (2.56 to 7.32) | − 2.25 (− 5.49 to − 0.99) | 0.18 | − 0.30 |
| APB/ FCR-FD | 5.98 (4.10 to 7.86) | 2.58 (1.64 to 3.51) | − 3.41 (− 5.25 to − 1.57) | 0.001*** | − 0.79 |
| APB/BIC | 5.82 (4.24 to 7.40) | 2.91 (2.17 to 3.64) | − 2.91 (− 4.65 to − 1.18) | 0.003** | − 0.72 |
| APB/ TRI | 6.04 (3.16 to 8.91) | 4.56 (2.26 to 6.85) | − 1.48 (− 4.59 to 1.63) | 0.35 | − 0.20 |
| ECU-ED/FCR-FD | 5.34 (3.83 to 6.86) | 2.69 (1.89 to 3.48) | − 2.65 (− 4.14 to − 1.17) | 0.002** | − 0.76 |
| ECU-ED/BIC | 4.97 (4.14 to 5.81) | 3.60 (2.81 to 4.40) | − 1.37 (− 2.48 to − 0.26) | 0.022* | − 0.53 |
| ECU-ED/TRI | 4.18 (3.09 to 5.26) | 3.88 (2.39 to 5.37) | − 0.30 (− 1.73 to 1.14) | 0.684 | − 0.09 |
| FCR-FD/BIC | 4.37 (3.15 to 5.59) | 2.42 (1.75 to 3.08) | − 1.95 (− 3.04 to − 0.87) | 0.002** | − 0.77 |
| FCR-FD/ TRI | 3.80 (2.59 to 5.01) | 2.17 (1.42 to 2.92) | − 1.62 (− 2.67 to − 0.58) | 0.005** | − 0.67 |
| BIC/TRI | 6.64 (4.80 to 8.49) | 4.59 (3.54 to 5.63) | − 2.06 (− 3.92 to − 0.19) | 0.039* | − 0.47 |
Fig. 8.
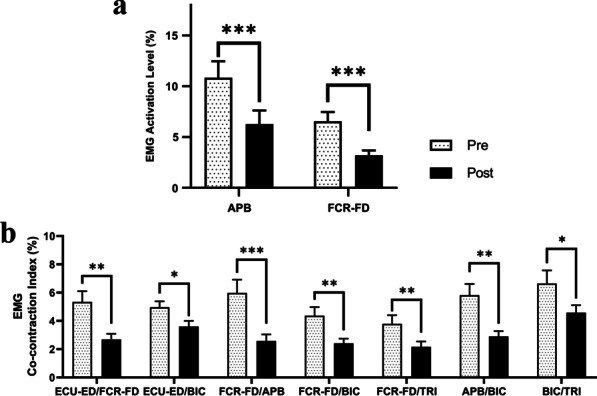
a EMG activation levels of the APB and FCR–FD during the bare hand evaluations, and b the EMG CI between the FCR–FD and ECU–ED, ECU–ED and BIC, FCR–FD and APB, FCR–FD and BIC, FCR–FD and TRI, APB and BIC, and BIC and TRI during the bare hand evaluations before (Pre) and after (Post) the training represented by means and standard errors. Significance levels are indicated by * (P ≤ 0.05), ** (P ≤ 0.01), and *** (P ≤ 0.001)
Kinematic parameters
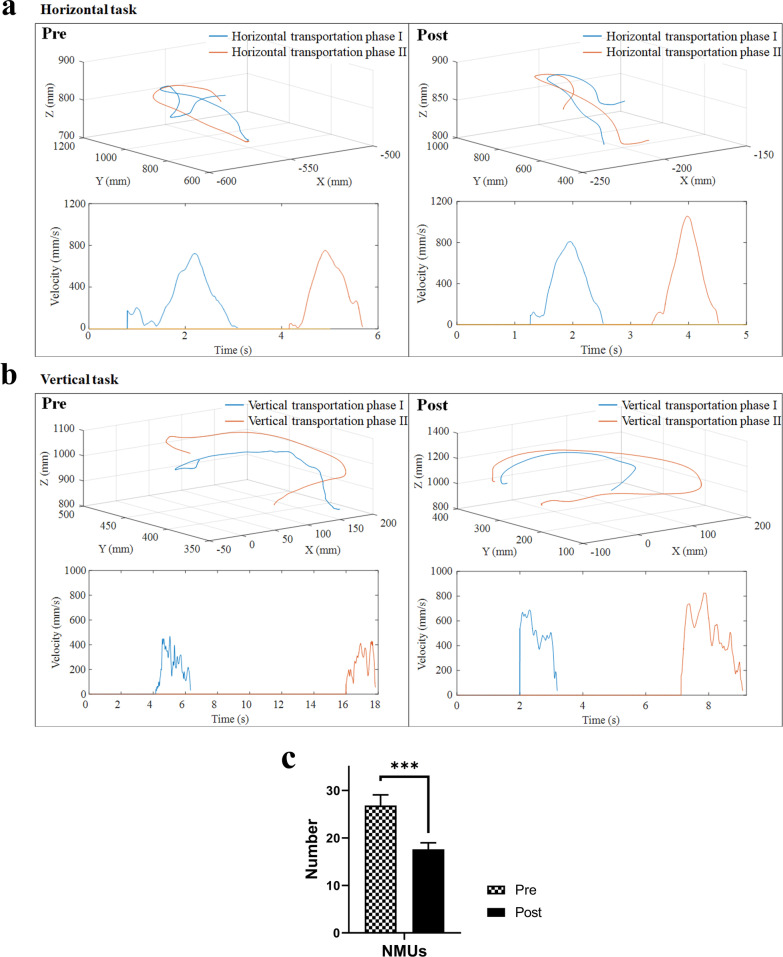
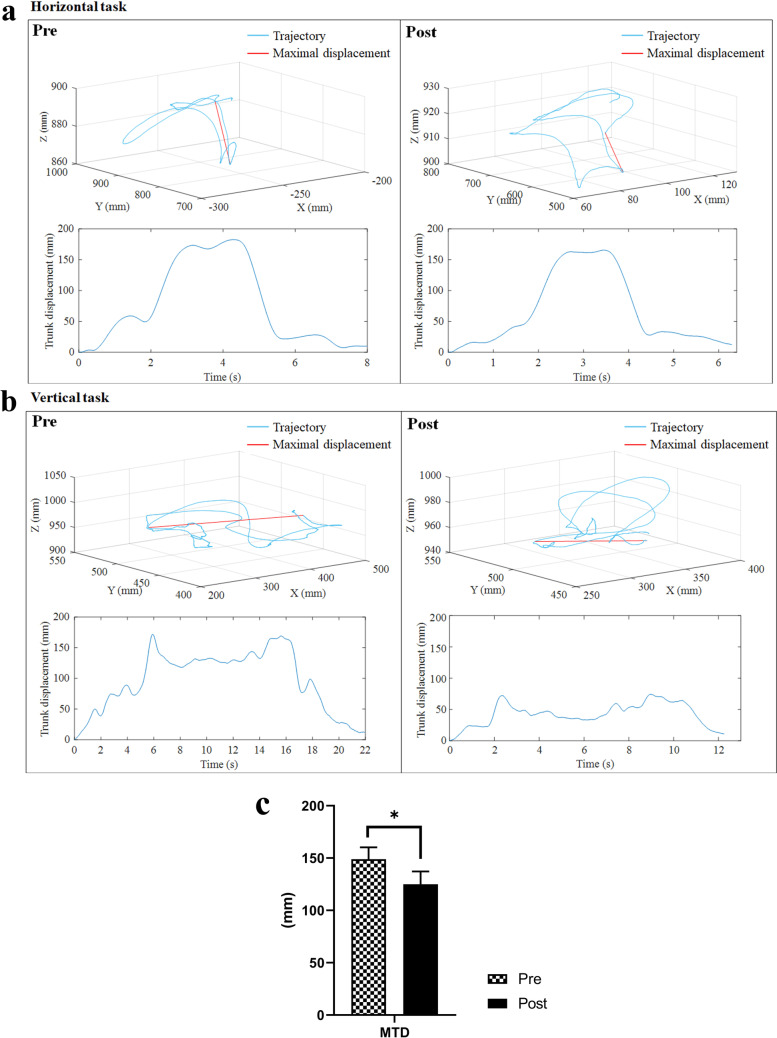
The measured kinematic parameters are listed in Table 6 (i.e., the means and 95% confidence intervals of each clinical assessment, together with the paired-sample t test probabilities with EFs of the evaluation before and after the training). Figure 9a, b shows the representative velocity profiles of the horizontal and vertical tasks before and after the training of a participant with respect to the three-dimensional trajectory of the hand marker during the transport phases. A significant decrease in NMUs was observed after the training (Fig. 9c; P < 0.05). Figure 10a, b illustrates the representative displacement profiles of a participant during horizontal and vertical tasks before and after the training with respect to the three-dimensional trajectory of the thorax marker throughout the entire trial. A significant reduction in MTD was found after the training (Fig. 10c; P < 0.05).
Table 6.
Means and 95% confidence intervals of each measurement in the kinematic parameters as well as the probabilities and estimated effect sizes in the statistical analyses
| Kinematic parameters | Pre | Post | Change () | Paired-sample t test | |
|---|---|---|---|---|---|
| Mean (95% Confidence interval) | P-value | Cohen's d | |||
| NMUs | 26.8 (22.3 to 31.3) | 17.6 (14.8 to 20.4) | − 9.23 (− 13.0 to − 5.50) | < 0.001*** | − 1.06 |
| MTD | 149 (126 to 172) | 125 (101 to 149) | − 23.9 (− 42.1 to − 5.70) | 0.016* | − 0.56 |
Differences with statistical significance are denoted by * (P ≤ 0.05) and *** (P ≤ 0.001)
Fig. 9.
Representative measured trajectory of the hand marker during the transport phases in a the horizontal task and b vertical task for a participant, and the related velocity profiles of the trial before and after training. c The NMUs before (Pre) and after (Post) the training represented in terms of the mean and standard error. Significance levels are indicated by *** (P ≤ 0.001)
Fig. 10.
Representative measured trajectory of the thorax marker over the entire trial for a the horizontal task and b vertical task for a participant, and the related displacement profiles in the trial before and after the training. c The MTD before (Pre) and after (Post) the training represented in terms of the mean and standard error. Significance levels are indicated by * (P ≤ 0.05)
Discussion
The results of this study support the hypothesis that it is feasible to use EMG-driven WH-ENMS to support the home-based self-help upper limb training of discharged participants with chronic stroke. After 20-session training, motor function improvements associated with improved clinical scores, EMG parameters, and kinematic parameters were observed in all of the participants.
Training outcomes of the home-based self-help program
Clinical scores
The significant increase in the FMA (shoulder/elbow and wrist/hand) score indicated an improvement in voluntary motor control of the entire upper limb after the training, especially on the joint stability and ROMs at the related joints on the paretic limb (Fig. 7a). The ARAT was adopted mainly to evaluate motor functions with hand tasks and focused on the finger functions, including holding/releasing objects in different shapes, sizes and weights. The significant increase in the ARAT score indicated the improvements in the hand function of the participants when handling different objects and coordination of the fingers for fine precision grasping (Fig. 7a). The increased WMFT scores suggested an overall improvement in the entire upper limb and increased ability to perform daily activities (Fig. 7a). The reduced time for conducting WMFT tasks (WMFT time) implied an improvement in movement efficiency and improved muscle coordination in the upper limb (Fig. 7a).
A significant improvement in the ability to perform daily activities was observed (as manifested in the increased WMFT scores and decreased WMFT time), but the improvement in the functional use of ADLs was not confirmed by the FIM scores. It indicated that the regained motor functions might not be translated into the functional use of the paretic limb to perform ADLs, even though the ability in the performance of daily tasks increased after the training. This was probably due to the two following characteristics of patients with chronic stroke: (1) learned nonuse could have become a habit, and the limb may not be used in functional activities although the individual has ability to move it [28], and (2) the unaffected limb attempts to execute all of the motor actions required for daily living [53]. It is suggested that outpatient rehabilitation should start as early as possible to minimize the development of learned nonuse and facilitate that the motor gains could translate into the functional use of the affected limb in ADLs.
The significant decrease in MAS score at the flexors of the elbow indicated that the spasticity of the elbow joint was reduced (Fig. 7b). The significantly reduced MAS scores at the flexors of the wrist and fingers indicated a release of spasticity of the distal joints (Fig. 7b). The reduced MAS score reflected a superior control over synergic muscle activity and a decrease in compensatory muscular activity [28, 54]. The decrease in the MAS scores of the elbow, wrist, and finger joints implied improved muscle coordination and joint stability of the proximal and distal joints during arm reaching, which was consistent with the observations in the FMA.
EMG parameters
A reduction in excessive muscle activities and improved muscle coordination was revealed by the decrease in the EMG activation levels at the flexors of the distal joints, co-contractions between the antagonist muscle pairs related to the wrist/hand and elbow, and co-contraction between the proximal and the distal joints (Fig. 8). The decreased EMG activation levels could be attributed to the reduced spasticity that led to a reduction in the extra muscle activities [55]. The significant decrease in the EMG activation levels of the APB and the FCR-FD muscles reflected a release of muscle spasticity at the fingers and the wrist, which was manifested in decreased MAS scores in the distal joints. The reduction of excessive muscle activities of the APB and the FCR-FD suggested an improvement in muscle coordination and voluntary motor controls during grasp and release movements, which was consistent with the findings in the FMA. A significant reduction in the CI of the ECU-ED/FCR-FD and the BIC/TRI muscle pairs was observed, indicating improved coordination between the flexors and extensors at the related joints, and improved independence in muscle contraction after the training. The significant disease in the CI of the ECU-ED/BIC, FCR-FD/BIC, FCR-FD/TRI, APB/BIC muscle pairs implied a release in the muscle co-contraction between the proximal and distal joints during arm reaching/withdrawing and grasping/releasing. A significant reduction in the CI of the FCR-FD/APB muscle pair was observed, suggesting a release in muscle co-contraction between the distal joints and the thumb, which contributed to the motor improvements in hand grasping, as manifested in the increased ARAT scores. The decreased EMG activation levels and co-contractions between the antagonist muscle pairs were also related to the reductions in abnormal muscle coactivation pattern caused by obligatory synergies in many hemiparetic patients after stroke [11, 56].
Kinematic parameters
A significant decrease in NMUs was found after the training, indicating increased smoothness of movement (Fig. 9). Oscillatory velocity profiles with multiple peaks were observed in the performance of a limb task of a patient with stroke using a paretic limb, as opposed to the smooth bell-shaped velocity profile with one predominant peak of the nonparetic limb [50]. These peaks reflect repetitive acceleration and deceleration when performing the limb task, which was due to the limited ability of patients with stroke to produce accommodative joint torque to maintain muscle tone during multi-joint coordinated limb movements [57]. The increased smoothness suggested an improvement in fine motor control [49, 58] and improved inter-joint coordination [58], which was consistent with the observations in the cross-joint CIs. It is a common observation that stroke patients rely on compensatory strategies that involving the trunk to overcome limb impairments during arm reaching associated with distal movements [28, 59, 60]. The significant reduction in MTD revealed a reduction in compensatory trunk movements when performing the multi-joint coordinated limb task, especially during object transportation (Fig. 10). The reduced requirement of trunk involvement to assist object transportation suggested an improvement in muscle strength in the shoulder and elbow and a release of spasticity in the elbow [61].
Improvements in the whole upper limb
Motor improvements in the entire upper limb (including both the proximal and distal joints) were found after the training. During the training, the assistance from the EMG-driven WH-ENMS was incorporated in the coordinated tasks related to the arm reaching/withdrawing and hand open/close of the whole upper limb. Thus, the proximal joints were also practiced voluntarily, although there was no device assistance directly applied. Furthermore, the proximal improvements could also be related to the compensatory contraction of proximal upper extremity (UE) muscles during the recruitment of distal muscles in the training and the competitive interaction between distal and proximal muscles during the sequenced motion tasks [62]. It was also reported that motor improvements in both the proximal and distal joints could be obtained through physical training involving the multi-joint coordinated task [63]. Furthermore, the introduction of NMES into the distal joints could promote motor coordination between the proximal and distal joints during rehabilitation, which could facilitate the improvement in the entire upper limb [64–66].
Independency in self-help upper limb training at home
Currently, most robotic therapies require therapists on-site, and limited techniques are available to support self-help post-stroke rehabilitation training [15, 26]. In this study, the feasibility and rehabilitation outcomes of a home-based self-help training assisted by EMG-driven WH-ENMS have been confirmed. The training setup used in the rehabilitation program and the system were easy to learn and easy to operate. All of the participants had received a pre-training tutorial and 3-session training at the laboratory before they could successfully conduct the home-based training with the prescribed training intensity and duration without any on-site professional supervision. There has been an exoskeleton robot (Myopro) developed for upper limb rehabilitation for self-help training at home for outpatients with stroke [67]. The participants had received at least 12 supervised sessions training with MyoPro (60 to 90 min per session) in the clinic to grasp device operation before the self-help training [67]. In the case of MyoPro, the rigid exoskeleton (1.8 kg, elbow–wrist–hand orthotic device) with nonnegligible weights mounted onto the paretic limb might cause incorrect alignment or migration during repeated practice [15, 68]. This additional safety concern pertaining to user-independent usage at home probably led a longer supervised training duration for the patients to gain the competency required for independent use of the device.
In the present study, the training progress of the participants was telemonitored and found to be compliant with the prescribed training intensity. In the home-based training, the variation in the training among the participants ranged from 60 to 66 min per session. It is reported that training intensity and duration are important factors for clinical improvement [12, 69]. In a study on self-administered home-based training with a passive dynamic wrist-hand orthosis accompanied by gaming exercises [70], participants were trained independently at home for six weeks and were recommended to practice for 30 min per day, six days per week. Limited motor improvement (i.e., no significant improvement in FMA) was found after the training. Besides the different effectiveness levels of the assistive devices, the inability to complete the recommended training duration was another key difficulties reported in that study [70]. A large amount of variation in training duration was observed among individuals, ranging from 2 to 60 min per day, because of lenient management and control of the training schedule (e.g., a lack of make-up sessions based on a quantitative and consistent protocol and delayed monitoring and follow-up in weeks rather than in days). Therefore, efficient monitoring of the training progress according to the prescribed rehabilitative protocol and schedule is important to ensure effective home-based self-help rehabilitation.
It also suggested that malfunctioning training systems in home-based rehabilitation should be easy to restore. Otherwise, unexpected drop-outs of recruited patients and violation of the training protocol could be encountered, as reported in a study on technology-supported home-based training [71]. In the present study, the technical problems were solved by directly replacing the malfunctioning systems efficiently with backup systems without violating the training protocol, leading to effective rehabilitation and smooth user experience. Moreover, the availability of multiple duplications of the device required a low-cost design for home-based training systems.
The compact design of the system could increase the feasibility of robot-assisted home-based training. Several existing home-based rehabilitation robots require a large physical space in the user’s living environment [16], which could be a challenge for patients living in crowded or small spaces [21, 72]. All of the participants in this study had adequate space in their house to accommodate the EMG-driven WH-ENMS due to the mobile and compact design of the system. Furthermore, the existing robotic devices are usually heavy and complex and require regular home visits for on-site installation, maintenance, and retrieval [16]. In the case of the system used in the present study, the participants could bring the system back to the laboratory for replacement or return without the need for additional home visits by the experimental operator.
The system provides flexibility in terms of training schedule; for instance, a patient can choose to use it at weekends or even at midnight, which is not possible with traditional clinical services. It was found that the preferred training time slots selected by the participants were 14:00 to 16:00 and 19:00 to 21:00. However, in traditional out-patient rehabilitation, it is difficult to accommodate all patients in these time slots. This could be one of the reasons for the low compliance with and attendance of long-term service for outpatient rehabilitation after stroke [73, 74]. Furthermore, the home-based upper limb rehabilitation of four participants in this study was not stopped during the COVID-19 pandemic, but conventional face-to-face physiotherapy and occupational therapy have been largely suspended due to social distancing restrictions worldwide. The robotic technique and the associated home-based and self-help training mode in this study provided an additional and effective option to the traditional rehabilitation to minimize the impact of physical distance control during the pandemic.
Limitation and future work
A single-group trial was used in this study to investigate the feasibility and effectiveness of EMG-driven WH-ENMS assisted home-based self-help telerehabilitation. The results demonstrated that it was feasible for persons with chronic stroke to complete the training tasks in a home-based environment with significant motor improvements. A randomized controlled trial with a larger sample size will be conducted in future studies to compare the rehabilitation effectiveness of the EMG-driven WH-ENMS assisted telerehabilitation with the conventional treatments. The psychometric information during the home-based training has not been collected in this study. It will also be investigated by surveys in future studies.
The training task in this study is to simulate the coordination of the joints in the arm reaching out, hand open for grasping, and withdrawing in daily activities, in order to restore the ability in the performance of daily tasks to the patients with stroke. During the EMG measurement and kinematic measurement, the participant was required to perform the training task without assistance from the EMG-driven WH-ENMS to evaluate if the participants have gained the ability to perform the trained movement. However, using the training tasks in the evaluation was a limitation to investigate the generalization of the motor gains in ADLs. In the result measured by FIM, the motor improvements in the affected limb have not been translated into the functional use in ADLs for the chronic stroke in this work. A more detailed design of the evaluation on the generalization of the motor improvements in ADLs will be included in our future studies.
Conclusion
The results of this study suggested that the home-based self-help upper limb training assisted by the EMG-driven WH-ENMS was feasible and effective for improving upper limb function after stroke. After the training program, the participants exhibited significant motor improvement in the entire upper limb. Significant improvements were found in the voluntary motor control and muscle coordination of the upper limb, the increased smoothness and reduced compensatory trunk movement during arm reaching coordinated with distal movements, and the release of muscular spasticity at the elbow, wrist and fingers. This new training mode of home-based self-help telerehabilitation could be an additional and effective option to support regular and long-term rehabilitation for outpatients with stroke.
Supplementary Information
Additional file 1: Appendix S1. Part A. Evaluation of muscular coordination in the upper limb by EMG. Part B. Evaluation of movement smoothness and compensatory trunk movement.
Additional file 2: Appendix S2.Table S1A. The demographic characteristics of each patient with stroke recruited for the home-based self-help upper limb training program (n =11). Table S1B. The 20-session training data (including training frequency, session duration and complete wrist/hand movement cycles per session) of each participant recruited for the home-based self-help upper limb training program (n =11). Table S1C. The individual outcomes of clinical scores of each participant recruited for the home-based self-help upper limb training program (n =11).
Acknowledgements
Not applicable.
Abbreviations
- ADLs
Activities of daily living
- VR
Virtual reality
- NMES
Neuromuscular electrical stimulation
- EMG
Electromyography
- ENMS
Exoneuromusculoskeleton
- WH-ENMS
Wrist/hand exoneuromusculoskeleton
- APB
Abductor pollicis brevis
- FCR
Flexor carpi radialis
- FD
Flexor digitorum
- FCR-FD
Flexor carpi radialis-flexor digitorum
- ECU
Extensor carpi ulnaris
- ED
Extensor digitorum
- ECU-ED
Extensor carpi ulnaris-extensor digitorum
- BIC
Biceps brachii
- TRI
Triceps brachii
- SD
Standard deviation
- MMSE
Mini-Mental State Examination
- FMA
Fugl-Meyer Assessment
- ARAT
Action Research Arm Test
- WMFT
Wolf Motor Function Test
- FIM
Functional Independence Measurement
- MAS
Modified Ashworth Score
- CI
Co-contraction index
- MVCs
Maximum voluntary contractions
- NMUs
Number of movement units
- MTD
Maximal trunk displacement
- EF
Effect size
- UE
Upper extremity
Authors' contributions
CN contributed to the experimental design, training experiment, data collection and analysis and manuscript drafting. BZ and TC contributed to the training experiment. FY and YH and ZG contributed to the subject recruitment and data collection. WL and RW contributed to the system maintenance. WP contributed to the clinical trial design and subject management. XH conceived of the study and coordinated the whole project, including the study design, human subject experiments and manuscript revising. All authors read and approved the final manuscript.
Funding
This project was funded by the National Natural Science Foundation of China (NSFC 81771959) and the Innovation Technology Commission of the Hong Kong Government (ITS/073/16) and (ITT/005/19GP).
Availability of data and materials
The datasets analyzed in the current study are not publicly available, because it has been stated in the consent approved by the Human Subjects Ethics Sub-Committee of the Hong Kong Polytechnic University that the results of the experiment may be published, but the individual results should be kept confidentially for each subject.
Declarations
Ethics approval and consent to participate
The human experiments were conducted after we obtained the ethical approval from the Human Subjects Ethics Sub-Committee of the Hong Kong Polytechnic University and the written informed consent from all subjects.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests related to this study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Chingyi Nam, Email: 16902874r@connect.polyu.hk.
Bingbing Zhang, Email: bingbing.zhang@connect.polyu.hk.
Tszying Chow, Email: tszying.chow@connect.polyu.hk.
Fuqiang Ye, Email: fuqiang.ye@connect.polyu.hk.
Yanhuan Huang, Email: yanhuan.j.huang@connect.polyu.hk.
Ziqi Guo, Email: tank.guo@connect.polyu.hk.
Waiming Li, Email: deo-li@hotmail.com.
Wei Rong, Email: rongwei@live.com.
Xiaoling Hu, Email: xiaoling.hu@polyu.edu.hk.
Waisang Poon, Email: wpoon@cuhk.edu.hk.
References
- 1.Takahashi CD, Der-Yeghiaian L, Le V, Motiwala RR, Cramer SC. Robot-based hand motor therapy after stroke. Brain. 2008;131(2):425–437. doi: 10.1093/brain/awm311. [DOI] [PubMed] [Google Scholar]
- 2.Dobkin BH. Rehabilitation after stroke. N Engl J Med. 2005;352(16):1677–1684. doi: 10.1056/NEJMcp043511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hendricks HT, van Limbeek J, Geurts AC, Zwarts MJ. Motor recovery after stroke: a systematic review of the literature. Arch Phys Med Rehabil. 2002;83(11):1629–1637. doi: 10.1053/apmr.2002.35473. [DOI] [PubMed] [Google Scholar]
- 4.Duncan PW, Sullivan KJ, Behrman AL, Azen SP, Wu SS, Nadeau SE, Dobkin BH, Rose DK, Tilson JK, Cen S, et al. Body-weight-suspported treadmill rehabilitation after stroke. N Engl J Med. 2011;364:2026–2036. doi: 10.1056/NEJMoa1010790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hung CS, Hsieh YW, Wu CY, Lin YT, Lin KC, Chen CL. The effects of combination of robot-assisted therapy with task-specific or impairment-oriented training on motor function and quality of life in chronic stroke. J Injury Funct Rehab. 2016 doi: 10.1016/j.pmrj.2016.1001.1008. [DOI] [PubMed] [Google Scholar]
- 6.Langhorne P, Coupar F, Pollock A. Motor recovery after stroke: a systematic review. Lancet Neurol. 2009;8(8):741–754. doi: 10.1016/S1474-4422(09)70150-4. [DOI] [PubMed] [Google Scholar]
- 7.Harris JE, Eng JJ. Strength training improves upper-limb function in individuals with stroke: a meta-analysis. Stroke. 2010;41(1):136–140. doi: 10.1161/STROKEAHA.109.567438. [DOI] [PubMed] [Google Scholar]
- 8.Sun J, Ke Z, Yip SP, Hu XL, Zheng XX, Tong KY. Gradually increased training intensity benefits rehabilitation outcome after stroke by BDNF upregulation and stress suppression. BioMed Res Int. 2014 doi: 10.1155/2014/925762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Farmer J, Zhao X, Van Praag H, Wodtke K, Gage FH, Christie BR. Effects of voluntary exercise on synaptic plasticity and gene expression in the dentate gyrus of adult male Sprague-Dawley rats in vivo. Neuroscience. 2004;124(1):71–79. doi: 10.1016/j.neuroscience.2003.09.029. [DOI] [PubMed] [Google Scholar]
- 10.Volpe BT, Ferraro M, Lynch D, Christos P, Krol J, Trudell C, Krebs HI, Hogan N. Robotics and other devices in the treatment of patients recovering from stroke. Curr Neurol Neurosci Rep. 2005;5(6):465–470. doi: 10.1007/s11910-005-0035-y. [DOI] [PubMed] [Google Scholar]
- 11.Dewald JPA, Sheshadri V, Dawson ML, Beer RF. Upper-limb discoordination in hemiparetic stroke: implications for neurorehabilitation. Top Stroke Rehabil. 2001;8(1):1–12. doi: 10.1310/WA7K-NGDF-NHKK-JAGD. [DOI] [PubMed] [Google Scholar]
- 12.Kwakkel G. Impact of intensity of practice after stroke: issues for consideration. Disabil Rehabil. 2006;28(13–14):823–830. doi: 10.1080/09638280500534861. [DOI] [PubMed] [Google Scholar]
- 13.Kwakkel G, Veerbeek JM, van Wegen EE, Wolf SL. Constraint-induced movement therapy after stroke. Lancet Neurol. 2015;14(2):224–234. doi: 10.1016/S1474-4422(14)70160-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Woo J, Chan SY, Sum MWC, Wong E, Chui YPM. In patient stroke rehabilitation efficiency: influence of organization of service delivery and staff numbers. BMC Health Serv Res. 2008;8(1):86. doi: 10.1186/1472-6963-8-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maciejasz P, Eschweiler J, Gerlach-Hahn K, Jansen-Troy A, Leonhardt S. A survey on robotic devices for upper limb rehabilitation. J Neuroeng Rehabil. 2014;11(1):3. doi: 10.1186/1743-0003-11-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen Y, Abel KT, Janecek JT, Chen Y, Zheng K, Cramer SC. Home-based technologies for stroke rehabilitation: a systematic review. Int J Med Informatics. 2019;123:11–22. doi: 10.1016/j.ijmedinf.2018.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Allen L, John-Baptiste A, Meyer M, Richardson M, Speechley M, Ure D, Markle-Reid M, Teasell R. Assessing the impact of a home-based stroke rehabilitation programme: a cost-effectiveness study. Disability Rehabil. 2019;41(17):2060–2065. doi: 10.1080/09638288.2018.1459879. [DOI] [PubMed] [Google Scholar]
- 18.Sarfo FS, Ulasavets U, Opare-Sem OK, Ovbiagele B. Tele-rehabilitation after stroke: an updated systematic review of the literature. J Stroke Cerebrovasc Dis. 2018;27(9):2306–2318. doi: 10.1016/j.jstrokecerebrovasdis.2018.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Laver KE, Lange B, George S, Deutsch JE, Saposnik G, Crotty M. Virtual reality for stroke rehabilitation. Cochrane Database Syst Rev. 2017;11:1. doi: 10.1002/14651858.CD008349.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dodakian L, McKenzie AL, Le V, See J, Pearson-Fuhrhop K, Burke Quinlan E, Zhou RJ, Augsberger R, Tran XA, Friedman N. A home-based telerehabilitation program for patients with stroke. Neurorehabil Neural Repair. 2017;31(10–11):923–933. doi: 10.1177/1545968317733818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sivan M, Gallagher J, Makower S, Keeling D, Bhakta B, O’Connor RJ, Levesley M. Home-based Computer Assisted Arm Rehabilitation (hCAAR) robotic device for upper limb exercise after stroke: results of a feasibility study in home setting. J Neuroeng Rehabil. 2014;11(1):163. doi: 10.1186/1743-0003-11-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Held JP, Ferrer B, Mainetti R, Steblin A, Hertler B, Moreno-Conde A, Dueñas A, Pajaro M, Vargiu E, Zarco MJ: Autonomous rehabilitation at stroke patients home for balance and gait: safety, usability and compliance of a virtual reality system. 2017. doi: 10.23736/S21973-29087.23717.04802-X. [DOI] [PubMed]
- 23.Triandafilou KM, Tsoupikova D, Barry AJ, Thielbar KN, Stoykov N, Kamper DG. Development of a 3D, networked multi-user virtual reality environment for home therapy after stroke. J Neuroeng Rehabil. 2018;15(1):88. doi: 10.1186/s12984-018-0429-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sheehy L, Taillon-Hobson A, Sveistrup H, Bilodeau M, Yang C, Welch V, Hossain A, Finestone H. Home-based virtual reality training after discharge from hospital-based stroke rehabilitation: a parallel randomized feasibility trial. Trials. 2019;20(1):1–9. doi: 10.1186/s13063-019-3438-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lambercy O, Dovat L, Yun H, Wee SK, Kuah CW, Chua KS, Gassert R, Milner TE, Teo CL, Burdet E. Effects of a robot-assisted training of grasp and pronation/supination in chronic stroke: a pilot study. J Neuroeng Rehabil. 2011;8(1):63. doi: 10.1186/1743-0003-8-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Balasubramanian S, Klein J, Burdet E. Robot-assisted rehabilitation of hand function. Curr Opin Neurol. 2010;23(6):661–670. doi: 10.1097/WCO.0b013e32833e99a4. [DOI] [PubMed] [Google Scholar]
- 27.Levin MF, Kleim JA, Wolf SL. What do motor “recovery” and “compensation” mean in patients following stroke? Neurorehabil Neural Repair. 2009;23(4):313–319. doi: 10.1177/1545968308328727. [DOI] [PubMed] [Google Scholar]
- 28.Raghavan P. Upper limb motor impairment after stroke. Physical Medicine and Rehabilitation Clinics. 2015;26(4):599–610. doi: 10.1016/j.pmr.2015.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Volpe BT, Lynch D, Rykman-Berland A, Ferraro M, Galgano M, Hogan N, Krebs HI. Intensive sensorimotor arm training medicated by therapist or robot improves hemiparesis in patients with chronic stroke. Neurorehabil Neural Repair. 2008;22:305–310. doi: 10.1177/1545968307311102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chae J, Kilgore K, Triolo R, Yu D. Neuromuscular stimulation for motor neuroprosthesis in hemiplegia. Crit Rev Phys Rehabil Med. 2000;12:1–23. doi: 10.1615/CritRevPhysRehabilMed.v12.i1.10. [DOI] [Google Scholar]
- 31.Rodgers MM, Alon G, Pai VM, Conroy RS. Wearable technologies for active living and rehabilitation: Current research challenges and future opportunities. J Rehabil Assist Technol Eng. 2019;26:6. doi: 10.1177/2055668319839607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Basteris A, Nijenhuis SM, Stienen AH, Buurke JH, Prange GB, Amirabdollahian F. Training modalities in robot-mediated upper limb rehabilitation in stroke: a framework for classification based on a systematic review. J Neuroeng Rehab. 2014;11(1):111. doi: 10.1186/1743-0003-11-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hu XL, Tong KY, Song R, Zheng XJ, Leung WWF. A comparison between electromyography-driven robot and passive motion device on wrist rehabilitation for chronic stroke. Neurorehabil Neural Repair. 2009;23(8):837–846. doi: 10.1177/1545968309338191. [DOI] [PubMed] [Google Scholar]
- 34.Hu XL, W. Rong, W.M. Li, C.Y. Nam, Y.J. Wei, T.C. Cheung, H.H. Wai, and J.Y. Hu: Physical rehabilitation apparatus, method, computer storage medium and electronic device. 2018:Application Number: PCT/CN2018/125005.
- 35.Nam C, Rong W, Li W, Cheung C, Ngai W, Cheung T, Pang M, Li L, Hu J, Wai H, et al. An Exoneuromusculoskeleton for Self-Help Upper Limb Rehabilitation After Stroke. Soft Robot. 2020 doi: 10.1089/soro.2020.0090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Qiuyang Q, Nam C, Guo Z, Huang Y, Hu XL, Ng SC, Zheng Y, Poon W. Distal versus proximal-an investigation on different supportive strategies by robots for upper limb rehabilitation after stroke: a randomized controlled trial. J Neuroeng Rehabil. 2019;16(1):64. doi: 10.1186/s12984-019-0537-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ashwoth B. Preliminary trial of carisoprodol in multiple sclerosis. Practitioner. 1964;192:540–542. [PubMed] [Google Scholar]
- 38.Fugl-Meyer AR, Jääskö L, Leyman I, Olsson S, Steglind S. The post-stroke hemiplegic patient. 1. a method for evaluation of physical performance. Scand J Rehab Med. 1975;7(1):13–31. [PubMed] [Google Scholar]
- 39.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state.” A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 40.Provos N, Mazieres D: A Future-Adaptable Password Scheme. In: USENIX Annual Technical Conference, FREENIX Track: 1999; 1999: 81–91.
- 41.Krebs HI, Volpe BT: Rehabilitation robotics. In: Handbook of clinical neurology. vol. 110: Elsevier; 2013: 283–294. [DOI] [PMC free article] [PubMed]
- 42.Carroll D. A quantitative test of upper extremity function. J Chronic Dis. 1965;18(5):479–491. doi: 10.1016/0021-9681(65)90030-5. [DOI] [PubMed] [Google Scholar]
- 43.Wolf SL, Lecraw DE, Barton LA, Jann BB. Forced use of hemiplegic upper extremities to reverse the effect of learned nonuse among chronic stroke and head-injured patients. Exp Neurol. 1989;104(2):125–132. doi: 10.1016/S0014-4886(89)80005-6. [DOI] [PubMed] [Google Scholar]
- 44.Granger CV, Hamilton BB, Keith RA, Zielezny M, Sherwin FS. Advances in functional assessment for medical rehabilitation. Topics in geriatric rehabilitation. 1986;1(3):59–74. doi: 10.1097/00013614-198604000-00007. [DOI] [Google Scholar]
- 45.Hu XL, Tong KY, Song R, Tsang VS, Leung PO, Li L. Variation of muscle coactivation patterns in chronic stroke during robot-assisted elbow training. Arch Phys Med Rehabil. 2007;88(8):1022–1029. doi: 10.1016/j.apmr.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 46.Hu XL, Tong KY, Song R, Zheng XJ, Lui KH, Leung WWF, Ng S, Au-Yeung SSY. Quantitative evaluation of motor functional recovery process in chronic stroke patients during robot-assisted wrist training. J Electromyogr Kinesiol. 2009;19(4):639–650. doi: 10.1016/j.jelekin.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 47.Oh HS, Kim EJ, Kim DY, Kim SJ. Effects of adjuvant mental practice on affected upper limb function following a stroke: results of three-dimensional motion analysis, fugl-meyer assessment of the upper extremity and motor activity logs. Ann Rehabil Med. 2016;40(3):401. doi: 10.5535/arm.2016.40.3.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hingtgen B, McGuire JR, Wang M, Harris GF. An upper extremity kinematic model for evaluation of hemiparetic stroke. J Biomech. 2006;39(4):681–688. doi: 10.1016/j.jbiomech.2005.01.008. [DOI] [PubMed] [Google Scholar]
- 49.Murphy MA, Willén C, Sunnerhagen KS. Kinematic variables quantifying upper-extremity performance after stroke during reaching and drinking from a glass. Neurorehabil Neural Repair. 2011;25(1):71–80. doi: 10.1177/1545968310370748. [DOI] [PubMed] [Google Scholar]
- 50.Kamper DG, McKenna-Cole AN, Kahn LE, Reinkensmeyer DJ. Alterations in reaching after stroke and their relation to movement direction and impairment severity. Arch Phys Med Rehabil. 2002;83(5):702–707. doi: 10.1053/apmr.2002.32446. [DOI] [PubMed] [Google Scholar]
- 51.Shapiro SS, Wilk MB, Chen HJ. A comparative study of various tests for normality. J Am Stat Assoc. 1968;63(324):1343–1372. doi: 10.1080/01621459.1968.10480932. [DOI] [Google Scholar]
- 52.Shapiro SS, Wilk MB. An analysis of variance test for normality (complete samples) Biometrika. 1965;52(3/4):591–611. doi: 10.2307/2333709. [DOI] [Google Scholar]
- 53.Cauraugh J, Light K, Kim S, Thigpen M, Behrman A. Chronic motor dysfunction after stroke: recovering wrist and finger extension by electromyography-triggered neuromuscular stimulation. Stroke. 2000;31(6):1360–1364. doi: 10.1161/01.STR.31.6.1360. [DOI] [PubMed] [Google Scholar]
- 54.Chae J, Yang G, Park BK, Labatia I. Muscle weakness and cocontraction in upper limb hemiparesis: relationship to motor impairment and physical disability. Neurorehabil Neural Repair. 2002;16(3):241–248. doi: 10.1177/154596830201600303. [DOI] [PubMed] [Google Scholar]
- 55.Bakheit A, Maynard V, Curnow J, Hudson N, Kodapala S. The relation between Ashworth scale scores and the excitability of the α motor neurones in patients with post-stroke muscle spasticity. J Neurol Neurosurg Psychiatry. 2003;74(5):646–648. doi: 10.1136/jnnp.74.5.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dewald JP, Pope PS, Given JD, Buchanan TS, Rymer WZ. Abnormal muscle coactivation patterns during isometric torque generation at the elbow and shoulder in hemiparetic subjects. Brain. 1995;118(2):495–510. doi: 10.1093/brain/118.2.495. [DOI] [PubMed] [Google Scholar]
- 57.Nordin N, Xie SQ, Wünsche B. Assessment of movement quality in robot-assisted upper limb rehabilitation after stroke: a review. J Neuroeng Rehabil. 2014;11(1):137. doi: 10.1186/1743-0003-11-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rohrer B, Fasoli S, Krebs HI, Hughes R, Volpe B, Frontera WR, Stein J, Hogan N. Movement smoothness changes during stroke recovery. J Neurosci. 2002;22(18):8297–8304. doi: 10.1523/JNEUROSCI.22-18-08297.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wu C-y, Yang C-l, Lin K-c, Wu L-l. Unilateral versus bilateral robot-assisted rehabilitation on arm-trunk control and functions post stroke: a randomized controlled trial. J Neuroeng Rehabil. 2013;10(1):35. doi: 10.1186/1743-0003-10-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Thielman G, Kaminski T, Gentile AM. Rehabilitation of reaching after stroke: comparing 2 training protocols utilizing trunk restraint. Neurorehabil Neural Repair. 2008;22(6):697–705. doi: 10.1177/1545968308315998. [DOI] [PubMed] [Google Scholar]
- 61.Levin MF, Michaelsen SM, Cirstea CM, Roby-Brami A. Use of the trunk for reaching targets placed within and beyond the reach in adult hemiparesis. Exp Brain Res. 2002;143(2):171–180. doi: 10.1007/s00221-001-0976-6. [DOI] [PubMed] [Google Scholar]
- 62.Takeuchi N, Izumi S-I. Maladaptive plasticity for motor recovery after stroke: mechanisms and approaches. Neural Plast. 2012;2012:1. doi: 10.1155/2012/359728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Susanto EA, Tong RK, Ockenfeld C, Ho NS. Efficacy of robot-assisted fingers training in chronic stroke survivors: a pilot randomized-controlled trial. J Neuroeng Rehabil. 2015;12(1):42. doi: 10.1186/s12984-015-0033-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hu X-L. Tong RK-y, Ho NS, Xue J-j, Rong W, Li LS: Wrist Rehabilitation assisted by an electromyography-driven neuromuscular electrical stimulation robot after stroke. Neurorehab Neural Rep. 2015;29(8):767–776. doi: 10.1177/1545968314565510. [DOI] [PubMed] [Google Scholar]
- 65.Nam C, Rong W, Li W, Xie Y, Hu XL, Zheng YP. The effects of upper-limb training assisted with an electromyography-driven neuromuscular electrical stimulation robotic hand on chronic stroke. Front Neurol. 2017;8:679. doi: 10.3389/fneur.2017.00679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Huang Y, Nam C, Li W, Rong W, Xie Y, Liu Y, Qian Q, Hu X. A comparison of the rehabilitation effectiveness of neuromuscular electrical stimulation robotic hand training and pure robotic hand training after stroke: A randomized controlled trial. Biomed Signal Process Control. 2020;56:101723. doi: 10.1016/j.bspc.2019.101723. [DOI] [Google Scholar]
- 67.McCabe JP, Henniger D, Perkins J, Margaret S, Curtis T, Pundik S. Feasibility and clinical experience of implementing a myoelectric upper limb orthosis in the rehabilitation of chronic stroke patients: a clinical case series report. PLoS ONE. 2019;14:4. doi: 10.1371/journal.pone.0215311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Islam M, Spiewak C, Rahman M, Fareh R. A brief review on robotic exoskeletons for upper extremity rehabilitation to find the gap between research porotype and commercial type. Adv Robot Autom. 2017;6(3):2. doi: 10.4172/2168-9695.1000177. [DOI] [Google Scholar]
- 69.Burgar CG, Lum PS, Scremin A, Garber SL, Van der Loos H, Kenney D, Shor P. Robot-assisted upper-limb therapy in acute rehabilitation setting following stroke: Department of Veterans Affairs multisite clinical trial. J Rehabil Res Dev. 2011;48(4):445–458. doi: 10.1682/JRRD.2010.04.0062. [DOI] [PubMed] [Google Scholar]
- 70.Nijenhuis SM, Prange-Lasonder GB, Stienen AH, Rietman JS, Buurke JH. Effects of training with a passive hand orthosis and games at home in chronic stroke: a pilot randomised controlled trial. Clin Rehabil. 2017;31(2):207–216. doi: 10.1177/0269215516629722. [DOI] [PubMed] [Google Scholar]
- 71.Nijenhuis SM, Prange GB, Amirabdollahian F, Sale P, Infarinato F, Nasr N, Mountain G, Hermens HJ, Stienen AH, Buurke JH. Feasibility study into self-administered training at home using an arm and hand device with motivational gaming environment in chronic stroke. J Neuroeng Rehabil. 2015;12(1):89. doi: 10.1186/s12984-015-0080-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cherry COB, Chumbler NR, Richards K, Huff A, Wu D, Tilghman LM, Butler A. Expanding stroke telerehabilitation services to rural veterans: A qualitative study on patient experiences using the robotic stroke therapy delivery and monitoring system program. Disabil Rehabil Assist Technol. 2017;12(1):21–27. doi: 10.3109/17483107.2015.1061613. [DOI] [PubMed] [Google Scholar]
- 73.Mohd Nordin NA, Aziz NAA, Abdul Aziz AF, Ajit Singh DK, Omar Othman NA, Sulong S, Aljunid SM. Exploring views on long term rehabilitation for people with stroke in a developing country: findings from focus group discussions. BMC Health Serv Res. 2014;14(1):118. doi: 10.1186/1472-6963-14-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pishkhani MK, Dalvandi A, Ebadi A, Hosseini M. Factors affecting adherence to rehabilitation in Iranian stroke patients: A qualitative study. J Vasc Nurs. 2019;37(4):264–271. doi: 10.1016/j.jvn.2019.07.001. [DOI] [PubMed] [Google Scholar]
- 75.Hu XL, Tong KY, Wei XJ, Rong W, Susanto EA, Ho SK. The effects of post-stroke upper-limb training with an electromyography (EMG)-driven hand robot. J Electromyogr Kinesiol. 2013;23(5):1065–1074. doi: 10.1016/j.jelekin.2013.07.007. [DOI] [PubMed] [Google Scholar]
- 76.Qian Q, Hu XL, Lai Q, Ng SC, Zheng YP, Poon WS. Early stroke rehabilitation of the upper limb assisted with an electromyography-driven neuromuscular electrical stimulation-robotic arm. Front Neurol. 2017;8:447. doi: 10.3389/fneur.2017.00447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Canning CG, Ada L, O’Dwyer NJ. Abnormal muscle activation characteristics associated with loss of dexterity after stroke. J Neurol Sci. 2000;176(1):45–56. doi: 10.1016/S0022-510X(00)00305-1. [DOI] [PubMed] [Google Scholar]
- 78.Kamper DG, Rymer WZ. Impairment of voluntary control of finger motion following stroke: role of inappropriate muscle coactivation. Muscle Nerve. 2001;24(5):673–681. doi: 10.1002/mus.1054. [DOI] [PubMed] [Google Scholar]
- 79.Cutti AG, Paolini G, Troncossi M, Cappello A, Davalli A. Soft tissue artefact assessment in humeral axial rotation. Gait Posture. 2005;21(3):341–349. doi: 10.1016/j.gaitpost.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 80.Murray IA. Determining upper limb kinematics and dynamics during everyday tasks. In: Doctoral dissertation. Newcastle upon Tyne: Newcastle University; 1999.
- 81.Tabak J. Geometry: the language of space and form. New York: Infobase Publishing; 2014. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Appendix S1. Part A. Evaluation of muscular coordination in the upper limb by EMG. Part B. Evaluation of movement smoothness and compensatory trunk movement.
Additional file 2: Appendix S2.Table S1A. The demographic characteristics of each patient with stroke recruited for the home-based self-help upper limb training program (n =11). Table S1B. The 20-session training data (including training frequency, session duration and complete wrist/hand movement cycles per session) of each participant recruited for the home-based self-help upper limb training program (n =11). Table S1C. The individual outcomes of clinical scores of each participant recruited for the home-based self-help upper limb training program (n =11).
Data Availability Statement
The datasets analyzed in the current study are not publicly available, because it has been stated in the consent approved by the Human Subjects Ethics Sub-Committee of the Hong Kong Polytechnic University that the results of the experiment may be published, but the individual results should be kept confidentially for each subject.