Abstract
Disasters have many deleterious effects and are becoming more frequent. From a health-care perspective, disasters may cause periods of stress for hospitals and health-care systems. Telemedicine is a rapidly growing technology that has been used to improve access to health-care during disasters. Telemedicine applied in disasters is referred to as disaster telemedicine. Our objective was to conduct a scoping literature review on current use of disaster telemedicine to develop recommendations addressing the most common barriers to implementation of a telemedicine system for regional disaster health response in the United States. Publications on telemedicine in disasters were collected from online databases. This included both publications in English and those translated into English. Predesigned inclusion/exclusion criteria and a PRISMA flow diagram were applied. The PRISMA flow diagram was used on the basis that it would help streamline the available literature. Literature that met the criteria was scored by 2 reviewers who rated relevance to commonly identified disaster telemedicine implementation barriers, as well as how disaster telemedicine systems were implemented. We also identified other frequently mentioned themes and briefly summarized recommendations for those topics. Literature scoring resulted in the following topics: telemedicine usage (42 publications), system design and operating models (43 publications), as well as difficulties with credentialing (5 publications), licensure (6 publications), liability (4 publications), reimbursement (5 publications), and technology (24 publications). Recommendations from each category were qualitatively summarized.
Keywords: telemedicine, telehealth, disaster, literature, scoping, review
Telemedicine (used synonymously with telehealth and teleconsultation) describes the application of information technology, video conferencing, and digitally sending images and biometric data to improve and enhance health-care delivery. The ability to communicate, forward diagnostic test results, and remotely monitor patients improves clinician effectiveness when there is limited or no access to specialist care. Telemedicine can improve medical response, both in daily hospital operations and in crisis situations when regional hospital systems and tertiary care facilities are overwhelmed by sudden peaks in patient volume, all while concurrently caring for the normal census.1 With a surge in patient volume caused by a disaster, primary receiving hospitals are called upon to care for and manage critically ill patients triaged to their facility.
Telemedicine can alleviate patient surge challenges by serving as a workforce multiplier for clinicians and specialists. Telemedicine has been used nationally and internationally1,2 in disaster responses for earthquakes, hurricanes, and areas devastated by war. This technology is indispensable for organizations such as Médecins Sans Frontier3 (Doctors Without Borders or MSF) and the North Atlantic Treaty Organization4 (NATO), both of which have conducted extensive telemedicine pilots. Queueing analysis is a method for matching random demand with fixed capacity. In a stressed health-care setting, this method determines the resources necessary to meet surging patient demand. Researchers used queueing analysis to quantify the potential of this technology: increased patient throughput, lowered emergency department (ED) boarding, and lowered patient mortality.5
While many US hospitals have specialty-specific telemedicine programs, including emergency telemedicine programs, these efforts are not typically included in disaster preparedness planning. Disaster telemedicine brings together multiple specialties and has the potential to provide disaster victims access to appropriate specialty care, improve patient safety, and lower cost.
In 2018, the Office of the Assistant Secretary for Preparedness and Response in the US Department of Health and Human Services funded the development of the Massachusetts/Region 1 Partnership to develop a pilot Regional Disaster Health Response System (RDHRS) to improve state and regional medical response capabilities. This scoping review was conducted by the Telemedicine Advisory Group as part of a multi-institutional partnership to support development of a pilot disaster telemedicine system for implementation in regional disaster health response.
Our objective of this review was to examine prior disaster telemedicine use strategies with a focus on system design and operating models for implementing telemedicine. Ultimately, our goal was to develop a set of recommendations for regulatory and policy changes needed to overcome previously identified barriers to support successful clinical implementation. While the collected literature came from around the world, with relevant findings dating between 1989 and 2019, our conclusions and analysis were conducted with a US-centric perspective.
Methods
Selection of Databases
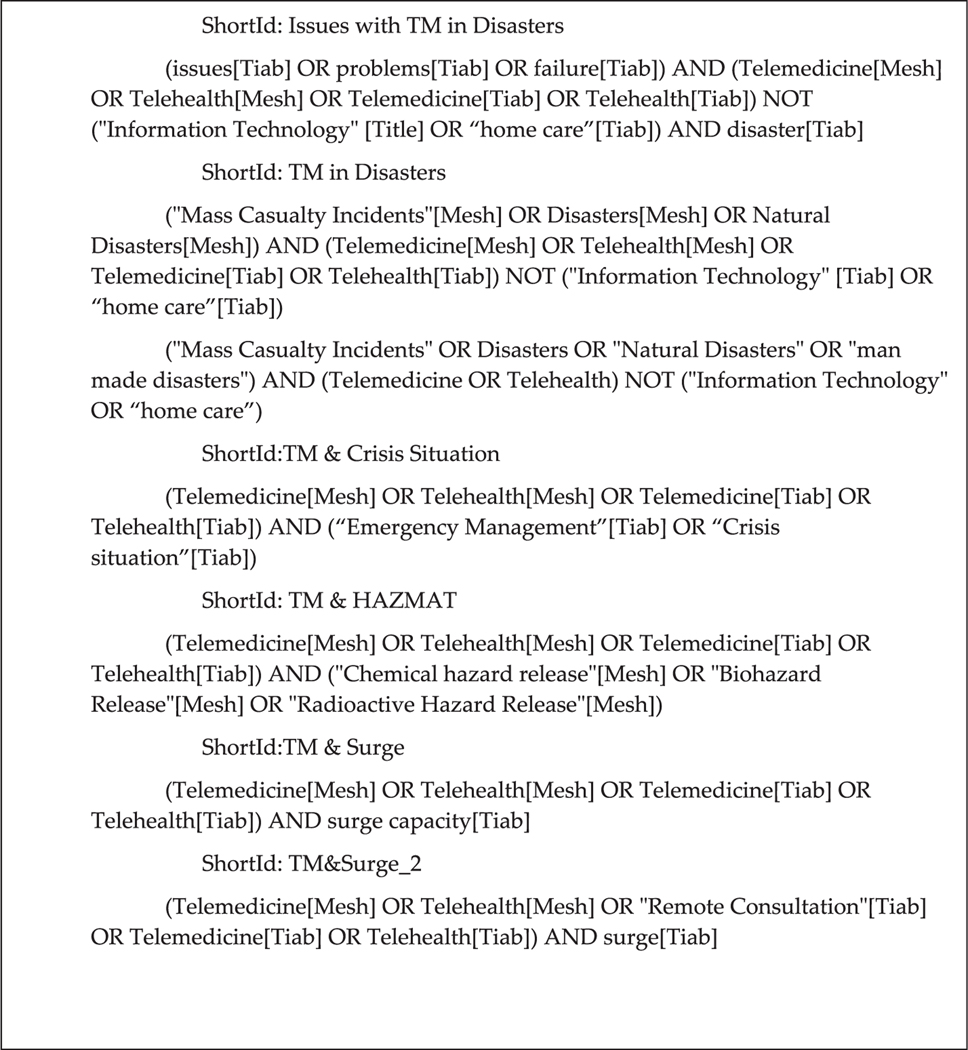
In collaboration with the Harvard University Countway Library and Brigham and Women’s Hospital Brigham Educational Institute, we collected literature on telemedicine in disasters on a rolling basis beginning in March 2019 until late July 2019 through weekly notifications set up per each search strategy. Literature concerning telemedicine in disasters was identified using various search strategies (Figure 1) in PubMed, Web of Science, Ovid Medline, ClinicalKey, Cochrane, PLoS, Google Scholar, and the AHRQ database.
Figure 1.
Search strategies used for literature collection. Note: the strategies listed below follow the syntax used on the PubMed and Google Scholar databases. For other databases, these same strategies were used after adjusting the syntax to fit the user interface of those databases.
Data Collection and Processing
To better process the literature that met the search criteria, we applied the PRISMA flow diagram as a framework for identifying literature that was directly relevant to telemedicine in disasters. After applying the PRISMA Guidelines Flow Diagram (Figure 2) and the Inclusion/Exclusion Criteria (Table 1), researchers collected and stored publications using Zotero,6 a citation manager software.
Figure 2.
PRISMA Flow Diagram.
Table 1.
Inclusion/exclusion criteria
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
| |
|
Dates Sources for the Disaster Telemedicine category will not have a date range (the first documented usage of disaster telemedicine will be reported on in equal measure as the most recent) Setting There is no limitation to setting for disaster telemedicine. International disasters and telemedicine usage therein will be reported on Publication Type Works of journalism, other literature reviews, and coverage of conferences and meetings will be identified as its own category of literature and will be included. Study Design Due to the differences in quantitative data formats that exist in the relevant literature, both quantitative and qualitative studies will be considered for final inclusion. A metanalysis will not be conducted. Contents •Outpatient telepsychiatry and telemental health after a disaster will be included. Rehabilitation offerings of telemedicine will be included. •Telemedicine provided by ambulances will be reported on. •All operational/usage models are being considered. •Usage of telemedicine in low-power settings of under poor connectivity will only be considered as a barrier and is not included in qualitative synthesis. |
•Only cases where telemedicine was
utilized during or immediately after a disaster were
considered. •Literature that falls in the non-disaster category of telemedicine will be used as introductory/background material and in the discussion. •In all categories, telemedicine platforms considered for this review will not include devices/platforms that fulfill a portion of the necessary functions for medical consultations (e.g., devices that only perform ultrasound in a live digital feed, such as the products made by Terason). Likewise, telemedicine designed for and applied in highly specific settings (e.g., only a transplant center) will not be included, only mentioned as a type of telemedicine. •Language barriers will be identified as a possible difficulty that telemedicine platforms/providers/suppliers should consider addressing, but besides that, this issue will not be reported on. In currently available platforms, language barriers will be described as an issue whenever applicable. |
Data Analysis
Two reviewers independently read the full-text versions of each article that met the eligibility criteria. Reviewers scored the literature according to the Literature Review Scoresheet (Figure 3), which categorized the collected literature by type of publication and type of data presented. This scoresheet assigns Likert-scale ratings of 1 to 5 for author’s contributions to the following topics: usage of telemedicine, system design and operating models, and issues with credentialing, licensure, liability, reimbursement, and technology. Results were obtained by identifying works with a mutual rating of 4 or higher. While scoring the literature, other important themes were identified and summarized. Because the literature review scoresheet rating system did not encompass these additional themes, they were not ranked.
Results
The database search strategies yielded 320 unique publications for screening (Figure 2), with 83 (26%) meeting criteria for eligibility (Table 1). A metanalysis was not performed. Independent review and ranking of the publications by 2 reviewers using the Literature Review Scoresheet identified and isolated works that contributed well to the topics of usage (42 publications), system design/operating models (43 publications), credentialing (5 publications), licensure (6 publications), liability (4 publications), reimbursement (5 publications), and technological issues (24 publications) (Table 2). Recommendations regarding these issues were summarized (Table 3). Other major themes in addition to the 7 key themes were briefly summarized.
Table 2.
Highly rated publications, organized by issue and type of literature
| # of Articles by Theme | |||||||
|---|---|---|---|---|---|---|---|
| Type of Literature: | Usage of Telemedicine (n = 42) | System Design/ Operating Models (n = 43) | Credentialing (n = 5) | Licensure (n = 6) | Liability (n = 4) | Reimbursement (n = 5) | Technology (n = 24) |
| Case report of past disaster | 11 | 14 | 0 | 0 | 0 | 0 | 4 |
| Report of simulated disaster | 11 | 12 | 1 | 0 | 0 | 0 | 11 |
| Telemedicine pilot study report | 19 | 21 | 1 | 0 | 0 | 0 | 12 |
| Literature review | 4 | 3 | 0 | 0 | 0 | 0 | 1 |
| Guidelines by official organizations/experts | 3 | 4 | 2 | 3 | 2 | 3 | 1 |
| White paper | 4 | 2 | 1 | 1 | 1 | 1 | 4 |
| Other gray literature | 18 | 12 | 2 | 4 | 2 | 3 | 12 |
| Somewhat or very transferable to other settings | 36 | 38 | 5 | 6 | 4 | 5 | 18 |
| Relates telemedicine to disasters well | 21 | 27 | 3 | 1 | 0 | 1 | 13 |
Table 3.
Recommendations identified in the literature
| Theme/Issue | Recommendations Identified in Literature |
|---|---|
| Usage | 1. There is a wide variety of telemedicine
solutions. Depending on the needs of a health system, telemedicine can
serve as a tool to address a variety of clinical needs, from direct
connection to a subspecialist, to enabling physicians to remotely
monitor patients for continuity of care, to connecting specialists to
patients and physicians to specialists for triaging as a means of
improving ED throughput7–17 2. Telemedicine and disaster response: In disaster simulations, telemedicine has been used in concert with telematic medical admission/dispatch hardware to better coordinate patient placement as well as evacuation24 |
| System Design/Operating Models | 1. Ensuring proper maintenance: to maintain a reliable telemedicine system, an organization would need to be responsible for verifying contact and availability of telemedicine providers and connection reliability for all participants4,27 |
| Credentialing | 1. Interstate credentialing: The Department of
Health and Human Services describes the Uniform Emergency Volunteer
Health Practitioners Act as state-level policy that could enable,
“… recognition of public and private sector healthcare
professionals’ licenses and other credentials across State and
National borders”30 2. Disaster medical records: A “disaster medical record” that could be exported from/imported to electronic health record systems to facilitate providers’ temporary access to critical health data during a disaster31,32 3. Credentialing by proxy: The Centers for Medicare & Medicaid Services allows hospitals to “credential by proxy,” meaning that hospitals requesting telemedicine support could circumvent some credentialing challenges during a disaster by proactively contracting with other hospitals and credentialing their providers28 |
| Licensure | 1. Engage with licensure boards: ASTHO
recommends collaborating, “ …with provider licensure
boards to create policies that ensure safety and quality of services
provided via telehealth and increase adoption”12 2. Interstate medical licensing: Create medical license reciprocity between states.29,30,34 3. National regulations regarding telemedicine practice and malpractice: The American College of Emergency Physicians proposes, “… uniform rules governing the practice of medicine, physician discipline, and laws concerning malpractice throughout the United States to provide uniform, safe, and quality urgent and emergent patient care.”29 However, as Poe explains, Congress is limited in its constitutional authority to regulate licensure nationally33 4. Licensure waivers during disasters: Encourage states to waive licensure requirements and fees during emergencies and disasters30 5. Re-brand telemedicine providers as “consultants”: Kim posits that “consultation exceptions” allow providers, “… not licensed in a particular state to practice there at the request of, or in consultation with, a referring physician;” thereby circumventing licensure barriers to telemedicine practice34 |
| Liability | 1. Clarify liability via legislation: The
Department of Health and Human Services proposes a legislative approach
to clarifying liability based on practitioners’ immigration and
employment status30 2. Indemnify practitioners: Legislation could provide immunity from negligence and indemnify practitioners.30 3. Expand malpractice insurance coverage: Kim recommends that malpractice insurance cover the parties and facilities involved with providing telemedicine34 4. Limit liability of telemedicine providers for on-site issues: Kim recommends reducing the liability of telemedicine providers for issues presumably out of their control, such as, “… any patient injuries sustained at the local site, as a result of malfunction of the telemedicine and/or telecommunication equipment and for any acts or omissions of the local physician … ”34 5. Limit product liability: Kim proposes reducing the liability of telemedicine providers for equipment malfunction or inappropriate use of technology that impacts the telemedicine consult or outcomes34 6. Limit government liability for pilot programs: Kim also recommends reducing telemedicine providers’ liability for participating in government telemedicine demonstration projects34 |
| Reimbursement | 1. Reimbursement advocacy: The American
College of Emergency Physicians and other medical trade associations
support, “… advocating for appropriate billing and fair
payment for services rendered by emergency physicians providing
telemedicine services”29 2. Payment standardization: Standardize payment based on the types of facilities, practitioners, and services involved with providing telemedicine34 |
| Technology | 1. Low-bandwidth solutions: technology currently being used for telemedicine places strain on wireless networks. For telemedicine encounters where audio and video quality are prohibitive to patient care and unsatisfactory for physicians, the alternative is to use data compression and low-bandwidth networks36,37 |
Based on our review of the literature, we identified 7 key themes regarding telemedicine use and disasters: (1) usage of telemedicine, (2) system design/operating models, (3) credentialing issues, (4) licensure issues, (5) liability issues, (6) reimbursement issues, and (7) technology issues. Of note, some authors did not separate the credentialing and licensure categories; thus, the recommendations proposed addressed both issues.
Discussion
Recommendations found in the literature regarding these 7 themes are detailed in Table 3. It is important to note that literature published since the end of this review period continues the trend of recommendations discussed in this literature review. While adoption of telemedicine has skyrocketed across all different types of telemedicine, there have not been developments that contradicted the conclusions written here.
Usage
To describe ways that patients, physicians, and hospital systems can benefit from telemedicine, a major category for this scoping review is the usage of telemedicine in disasters. Authors contributed data that reflect the impact of telemedicine on patient care, throughput, cost savings for both patients and hospital systems, and other important variables to demonstrate the potential of this technology.
Telemedicine exists in various forms and serves many clinical specialties.7–12 Types of telemedicine include direct-to-patient, provider-to-provider (including midlevel providers, who are intrinsic participants in the telemedicine process), asynchronous, store-and-forward tools, as well as synchronous, and live video telemedicine encounters. This topic encompasses literature where authors detailed the clinical reasons telemedicine was used in disaster settings. Uses of telemedicine include: patient triage, patient placement, and disaster management;4,10,13–15 as well as direct clinical intervention9,16; and remote patient monitoring (in-hospital, tele-home care, telemedicine that aids in continuity of care).7 Key findings within this topic were collected from: (1) data simulations, (2) literature reviews, and (3) simulated disaster preparedness exercises.
Following a disaster-based data simulation, authors recommend that procedures for telemedicine consultations are clearly defined and provided in advance as a preparedness measure. They also concluded that the use of telemedicine should be a routine part of disaster training.17
Queueing modeling analysis, a method for matching random health-care demand with fixed hospital capacity, was performed of a simulated earthquake and found a reduction in ED wait time and lowered mortality when using a telemedicine hub for triage and remote treatment as opposed to relying on standard communication and transfer protocols.5 The authors reported system-wide mortality decreases ranging in magnitude from 5.4 to 36.5% (depending on severity of earthquake event).5 One simulated Designated Receiving Center projected a mortality decrease ranging from 15 to 99%.5 Likewise, authors reported a projected decrease in ED wait time ranging from 40.72 to 94.34%.5
To describe the effects of using telemedicine, authors of previous literature reviews contribute that telemedicine produces cost savings for both patients18,19 and hospital systems by increasing patient throughput and lowering practice and resource costs.20–22 Estimating the cost savings is difficult because there are many types of telemedicine, and specific figures are only offered in pilot studies.23
In disaster preparedness exercises (a type of simulation tool), telemedicine has been used in concert with medical admission and dispatch hardware to better coordinate patient placement, as well as evacuation.24
The Usage of Telemedicine category of literature is fundamental to comprehending how telemedicine has previously benefited disaster response and patient throughput, while also highlighting its future potential. These findings provide significant insight into how telemedicine may benefit patients, physicians, and health-care systems universally. The remaining categories provide insights into what is necessary to make disaster telemedicine possible.
System Design/Operating Models
To harness the benefits of telemedicine for disaster medical response, it is important to understand how telemedicine operates. “Operating model” refers to the organizational design (staffing, scheduling, monitoring, and quality assurance, etc.) that enables telemedicine. This topic also refers to telemedicine encounter workflows, as well as the logistical preparation required to use telemedicine (such as creating an on-call roster of subspecialists).25 “System Design” refers to the technological elements that enable telemedicine such as proprietary hardware, data logistics, and bandwidth requirements across multiple hardware options (satellite, data, wi-fi, radio, etc.) Rather than discussing the impact and clinical use of telemedicine, these categories jointly describe the technological and operating requirements for implementing a telemedicine system.
Key findings for the system design and operating models category include authors matching different types of users with types of telemedicine. Literary contributions list the following successful operating models: telemedicine conducted between first responders (civilian and military settings) and physicians for the purpose of triage, clinical management of critical patients, and disaster management4,13–15; telemedicine conducted between generalists and subspecialists, including triage and secondary triage,4 clinical management (decision-making, diagnostic support,16,22 and remote procedural guidance9,16); and telemedicine between patients and physicians, including clinical management, remote patient monitoring, store-and-forward of laboratory results and diagnostic imaging.2,4,16
Telemedicine facilitates connections between multiple participants. There are different modes fundamental to telemedicine, such as direct connection, in which telemedicine uses video or audio conferencing to directly connect participants; and connection by means of proxy, where requesting patients or clinicians are connected to a coordinator who triages their request and connects to a specialist.3 Digital proxies also exist where a request for telemedicine is coded and read by a software before being triaged with increased precision to a specialist.11,26
Another key finding from this category of literature is the need for maintenance. Authors found that it is necessary to use an organization that would be tasked with maintaining the contact information for the providers of telemedicine.4,27 Maintaining telecommunication reliability is also recommended.4,27
Credentialing Issues
“Credentialing” refers to the accreditation of physicians that enables the practice of telemedicine.12 Credentialing is a known barrier to effectively providing telemedicine, particularly in disaster scenarios and across US state lines and in countries with similar credentialing arrangements. The Joint Commission subjects a telemedicine provider to the credentialing requirements of the patient’s location.28 The American College of Emergency Physicians (ACEP) similarly recommends that telemedicine providers abide by all credentialing requirements required for standard in-person care.29 Requiring authentication of each telemedicine system user during an emergency response, while protecting system security, could compromise system functionality, perhaps impacting speed of care.27 Furthermore, state government emergency powers during a disaster vary, limiting some states’ ability to enable temporary licensing or credentialing for out-of-state providers.30
Technical31 and policy innovations,28–30 if implemented, could reduce the credentialing challenges providers face32. The literature offered 3 recommendations to overcome this: (1) implement interstate credentialing30; (2) create disaster medical records that facilitate providers’ temporary access to critical health data31; and (3) credential practitioners by proxy, developing streamlined channels between medical staff offices that account for interfacility provision of telemedicine.28
Licensure Issues
“Licensure” is the formal regulatory recognition of a physician’s education, training, and performance on exams that enable physicians to provide telemedicine.12 As above, ACEP recommends that telemedicine providers abide by all licensure requirements required for standard in-person care.29 Several “interstate licensure compacts” exist to support licensure compliance across multiple states.12,28 However, requiring practitioners to be licensed in multiple states places significant financial and educational burden upon practitioners to remain compliant with each states’ requirements.33 Additionally, only some states can waive licensure requirements during federally declared disasters, which is unhelpful to states without that authority and for all states responding to non–federally declared disasters.28,30
Again, as above, the policy landscape surrounding the licensure process during disasters for telemedicine providers is difficult to navigate and may cause delays in care. State licensure policies are not keeping pace with new technology and must be updated to reduce barriers to telemedicine use.12,28,34 The literature included 5 recommendations to address licensure barriers: (1) engage with licensure boards to create telemedicine-friendly policies12; (2) create interstate medical licensing29,30,34; (3) establish national regulations regarding telemedicine practice and malpractice29; (4) implement licensure waivers during disasters30; and, (5) rebrand telemedicine providers as “consultants” to circumvent licensure barriers.34
Liability Issues
“Liability” refers to the legal protections for physicians engaging in telemedicine consultations, including malpractice insurance.12 Telemedicine providers are encouraged to be knowledgeable of the laws, policies, and regulations of the states in which they practice (ie, where their patients are located during their telemedicine evaluations).29 However, this can be challenging given the ambiguity surrounding telemedicine malpractice liability and tort law jurisdiction.30,33 Poe notes, “Few legal precedents exist and legislation has not kept pace with telemedicine’s practical applications,” specifically with regard to telemedicine and its interface with informed consent, confidentiality, privacy, security, and standards of care.33
Employment status and the location of the disaster can affect practitioners’ liability protection.30 There are important differences between the tort liability of government employees and private sector providers. Furthermore, there are different tort liability protections available to out-of-state practitioners under policies and regulations such as but not limited to states’ emergency powers, Good Samaritan statutes, and federal volunteer protections.30
Additionally, the Department of Health and Human Services explains that telemedicine practitioners are not indemnified even if they are immune from civil action.30 While a legal case against a telemedicine practitioner may be stopped, the practitioner may still have to pay the costs associated with their legal defense.30 There have not been many telemedicine malpractice cases to date; perhaps contributing to the ambiguity about telemedicine liability during disasters.28 The Department of Health and Human Services notes that, “This lack of protection could serve as a potential barrier to engaging health-care practitioners to assist during public health emergency or disaster medical responses.”30
Ambiguous and dated Federal and state liability laws and protections may create a barrier to engaging providers in disaster telemedicine.30 There are 6 recommendations in the literature to address liability barriers to telemedicine practice: (1) clarify practitioners’ liability,30,34 particularly by means of legislation30; (2) indemnify telemedicine practitioners30; (3) expand the scope of malpractice insurance coverage34; (4) limit liability of telemedicine providers for on-site issues34; (5) limit the liability of telemedicine practitioners for equipment issues34; and, (6) limit the liability of telemedicine providers when participating in government pilot programs.34
Reimbursement Issues
“Reimbursement” refers to the methods of payment to physicians engaging in telemedicine consultations.12 As authors for the journal HealthcareReady note, “Reimbursement is widely considered the largest barrier for telehealth.”28 In 2006, the Pandemic and All Hazards Preparedness Act (P.L. 109–417) framed payment and reimbursement for telemedicine as an, “Immediate (challenge) to the use of Telehealth for public health emergencies and disaster medical responses.”30
The American College of Emergency Physicians cautions telemedicine providers to be vigilant regarding federal and state reimbursement policies until there is uniform, national telemedicine reimbursement regulation.29 The Association of State and Territorial Health Officials (ASTHO) explains that, “… how states define telehealth or telemedicine in legislation affects the reimbursement and coverage of services and state legislation or rulemaking can impact Medicaid or private payer coverage.”12 This finding is supported by HealthcareReady, “Varied policies across Medicare, Medicaid, and private payers are also constantly evolving, compounding challenges in understanding reimbursement for telehealth.”28
The literature also refers to telemedicine parity. Telemedicine parity laws, “require private payers in a state to reimburse for telehealth services the same way they would for an in-person service.”12 There is no parity for telemedicine under Medicare, and Medicare restricts the type and location of reimbursable telemedicine services.12,28,34 The federal government sets Medicare reimbursement policies.28 Conversely, Medicaid coverage is set at the state level28 and is more expansive than Medicare: according to ASTHO, “As of March 2017, a total of 48 states and the District of Columbia have some type of (Medicaid) coverage for telemedicine.”12 As of 2017, there is state employee health plan coverage for telemedicine in 26 states, and 56% of federal employee health plans cover telemedicine.12 However, when telemedicine services are reimbursed, it is frequently at a lower rate than traditional services, which disincentivizes practitioners from participating in telemedicine.28
Addressing reimbursement challenges is critical to the future of telemedicine. As indicated by HealthcareReady, “Providers surveyed by the US Government Accountability Office (GAO) cited inadequate payment and coverage options as the principal barrier to (telemedicine) adoption.”28 The literature offered 2 recommendations to address telemedicine reimbursement challenges: (1) advocate for better reimbursement29; and (2) standardize payment based on the types of facilities, practitioners, and services involved with providing telemedicine.34
Technology Issues
Successful operation of a telemedicine system requires a reliable technological infrastructure. The technology issues theme encompasses literature that detailed challenges that users of telemedicine encountered and what steps were taken to overcome those issues. Fundamental failures in the telemedicine system can include but are not limited to the inability to form a connection for connectivity or system capacity reasons, and a prohibitively poor transmission of video, audio, images.
Although recommendations in the literature are limited, there are low bandwidth solutions for what is currently being done using high-bandwidth technology. For still image transmission over poor connectivity (radiology results), options exist to compress image files. This compression makes files small enough for weaker networks, such as satellite networks,35 to transmit (larger file sizes failed to transmit).19 Such compression works for audio and video multimedia.36,37 For extending wireless reliability into zones where network access is limited, another solution is using a system of Local Access Networks for Internet connection.10
Other Salient Themes
Other themes that arise frequently in the literature as challenges or important considerations for telemedicine use in disaster response include: protecting patient privacy and confidentiality12,16,22,30,33,34,38–41; ensuring the security of technology used in telemedicine (which directly relates to protecting patient privacy and confidentiality)14,22,30,33,34,38,42; respecting patients’ right to education and informed consent12,29,33–35,38,39; upholding standards of care and maintaining the integrity of the physician-patient relationship12,28,29,33–35,38,41; creating clinician-friendly protocols for telemedicine use and documentation, continuing education, and quality improvement11,17,33,34,38,39; increasing cultural acceptance of telemedicine, particularly among medical leaders, and consequently integrating telemedicine into preparedness planning3,9,11,28,30,31,37,38,41,43–46; providing sufficient training to practitioners involved in telemedicine4,12,16,17,19,28,30,38,44,45; and securing ongoing funding for telemedicine initiatives.12,19,22,28,30
Limitations
There were several limitations encountered throughout the process of this scoping review, including use of online databases to access literature, the academic quality of the identified literature, and the quantity and uniformity of telemedicine data available.
The scope of this scoping review only extended to publications that are stored and maintained on online databases. As shown in (Figure 1), where search strategies contained the code MESH, some search strategies relied on the indexing of these publications, which is rarely done for the most recently published works. To limit the impact of this, weekly updates were enabled for each search strategy.
This scoping review did not include a metanalysis due to the lack of compatible quantitative data in the literature. The investigative methods used by authors yield a wide variety of data. While there are exceptions, small-scale telemedicine pilots (ie, pilots of telemedicine that last for approximately a year, encompass 1–3 specialties, and vary greatly in terms of how they describe demand for telemedicine services) were a general trend. While results from such pilots are valuable, it is difficult to draw definitive conclusions for a wider range of implementation (ie, statewide). The lack of case-control comparison groups is also a trend in the literature; while there are exceptions, pilot studies of telemedicine and reports of past disasters do not provide input on how hospitals fared using standard consultative methods compared with telemedicine use. Another limitation is the limited input on patient-centered outcomes.
This scoping review illustrates the wide use of multiple telemedicine operating models, both during disasters and in preparedness drills and pilot programs. To date, telemedicine suppliers and enterprising health-care organizations have produced and tested a wide variety of technological options and solutions, some of which have already been and continue to be used in disasters in the forms of pilot programs. Many lessons have been learned in how to construct a telemedicine system and operate it.
A trending finding in the literature is that a policy landscape that addresses credentialing, licensure, liability, and reimbursement needs to be implemented to facilitate interstate telemedicine use. While solutions exist for each category of issues (credentialing, licensure, liability, reimbursement), the available literature has fundamentally not quantified the impact or scale of existing laws and regulations on telemedicine for patient care during a disaster. There is also need for further research into the efficacy of the different telemedicine platforms in disasters. While it is evident that the telemedicine industry of today is comprised of various small-scale telemedicine programs at individual hospitals/hospital systems, a region-wide (ideally nationwide) telemedicine system would make it possible for overtaxed hospitals and their patients to benefit from improved access to specialty care during disasters. To achieve this, there is an urgent need to continue to guide the current policy landscape toward wider and easier emergency telemedicine adoption, to improve physician familiarity and comfort with telemedicine, and to develop more robust telemedicine system solutions.
Supplementary Material
Glossary
- Assistant Secretary for Preparedness Response (ASPR)
An agency within the US Department of Health and Human Services
- Credentialing
“Credentialing is the process by which an employer, most frequently a hospital or health maintenance organization (HMO), verifies that a practitioner has the required education, training, and experience to practice in the state. State or local laws and rules can specify the types of credentials and verification processes that a hospital or other healthcare provider must address in credentialing a practitioner. Credentialing is typically done when a practitioner is first employed with an entity and may be updated periodically.”12
- Disaster
The United Nations Office for Disaster Risk Reduction defines disasters as “A serious disruption of the functioning of a community or a society at any scale due to hazardous events interacting with conditions of exposure, vulnerability and capacity, leading to 1 or more of the following: human, material, economic and environmental losses and impacts.”2,47
- Licensing
“Licensing is the formal recognition by a regulatory agency or body that a person has passed all the qualifications to practice that profession in that state. Typically, licensure requirements include some combination of education, training and examination to demonstrate competency. Licensure requirements also involve continuing education, training, and, for some, periodic re-examination. If a practitioner licensed in 1 state seeks licensure in another state, the existing license and any disciplinary records are considered as part of the licensing process in the new state.”12
- Liability
“Out-of-state healthcare professionals may also have liability concerns when assisting during a public health emergency and disaster medical response. States vary in the degree to which liability protections are offered and enforced. […] Legislation could clarify liability protections for domestic and foreign healthcare professionals, whether they are volunteers or paid employees working outside their regular employment duties.”30
- Reimbursement
“As a field, telehealth is growing, and policies dedicated to coverage and reimbursement are evolving. […] some states put specific restrictions within the definitions of telehealth, often limiting locations where telehealth can be delivered (e.g., limiting the home as a reimbursable site or that the originating site cannot be in the same community as the distant site), or limiting the term to “live” or “interactive.” […] With telehealth parity laws and Medicaid coverage, telehealth services can be reimbursed in a variety of ways, including fee-for-service and value-based payments. However, telehealth services can also include other fees, such as originating site facility fees. These fees vary across states.”12
- Regional Disaster Health Response System (RDHRS)
RDHRS refers both to the Massachusetts/Region 1 Partnership, a multihospital cooperative, and the response system that is being tested as part of the overall project this literature review is written for. https://www.phe.gov/Preparedness/planning/RDHRS/Pages/rdhrs-overview.aspx
- Telemedicine
“Telemedicine is the use of medical information exchanged from 1 site to another via electronic communications to improve a patient’s clinical health status. Telemedicine includes a growing variety of applications and services using 2-way video, e-mail, smart phones, wireless tools, and other forms of telecommunication technology. Telemedicine is not a separate medical specialty. It is a delivery tool or system. […] Videoconferencing, transmission of still images and other data, e-health, including patient portals, m-health, remote monitoring, continuing medical education, and medical call centers, are all considered part of telemedicine and telehealth.”38
- System Design
A term developed for the purposes of the literature review. This term aims to capture the technical elements that enable telemedicine: what hardware is the telemedicine program run on, what servers are used, what the logistics of information transfer (i.e., via satellite, radio, cellular data, etc.), and what data is being sent through this system (image resolution, video resolution and frames per second, audio quality, audio and video latency, etc.). The topic of documentation blends elements of this topic and the topic of Operating Model
- Operating Model
A term developed for the purposes of this literature review. This term aims to capture the operating elements that telemedicine requires: how does the usage of telemedicine fit in with daily hospital operations, who participates in telemedicine encounters, how does the administrative component function, what work is done to run a telemedicine system (IT, development of on-call rosters, maintenance of on-call rosters, recruitment, hiring, etc.), are there patient queues, and how documentation is completed
Footnotes
Supplementary material. To view supplementary material for this article, please visit https://doi.org/10.1017/dmp.2020.473
References
- 1.Shahid W, Xinhai L. A case study of telemedicine for disaster management in underdeveloped remote districts of Balochistan, Pakistan. J Econ Sustain Dev. 2013:4(20). [Google Scholar]
- 2.Patoli AQ. Role of telemedicine in disaster management. https://www.slideserve.com/kara/role-of-telemedicine-in-disaster-management. Accessed February 11, 2021.
- 3.Delaigue S, Bonnardot L, Steichen O, et al. Seven years of telemedicine in Médecins Sans Frontières demonstrate that offering direct specialist expertise in the frontline brings clinical and educational value. J Glob Health. 2018;8(2):020414. doi: 10.7189/jogh.08.020414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Doarn CR, Latifi R, Poropatich RK, et al. Development and validation of telemedicine for disaster response: The North Atlantic Treaty Organization Multinational System. Telemed E Health. 2018;24(9):657–668. doi: 10.1089/tmj.2017.0237 [DOI] [PubMed] [Google Scholar]
- 5.Xiong W, Bair A, Sandrock C, et al. Implementing telemedicine in medical emergency response: concept of operation for a regional telemedicine hub. J Med Syst. 2012;36(3):1651–1660. doi: 10.1007/s10916-010-9626-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roy Rosenzweig Center for History and New Media. Zotero [Computer software]. 2016. www.zotero.org/download. Accessed February 11, 2021.
- 7.Reissman DB, Schreiber M, Klomp RW, et al. The virtual network supporting the front lines: addressing emerging behavioral health problems following the tsunami of 2004. Mil Med. 2006;171(10 Suppl 1):40–43. [DOI] [PubMed] [Google Scholar]
- 8.Uscher-Pines L, Fischer S,Tong I, et al. Virtual first responders: the role of direct-to-consumer telemedicine in caring for people impacted by natural disasters. J Gen Intern Med. 2018;33(8):1242–1244. doi: 10.1007/s11606-018-4440-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sahloul MZ, Monla-Hassan J, Sankari A, et al. War is the enemy of health. Pulmonary, critical care, and sleep medicine in war-torn Syria. Ann Am Thorac Soc. 2016;13(2):147–155. doi: 10.1513/AnnalsATS.201510-661PS [DOI] [PubMed] [Google Scholar]
- 10.Simmons SC, Murphy TA, Blanarovich A, et al. Telehealth technologies and applications for terrorism response: a report of the 2002 coastal North Carolina domestic preparedness training exercise. J Am Med Inform Assoc. 2003;10(2):166–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Burke RV, Berg BM, Vee P, et al. Using robotic telecommunications to triage pediatric disaster victims. J Pediatr Surg. 2012;47(1):221–224. doi: 10.1016/j.jpedsurg.2011.10.046 [DOI] [PubMed] [Google Scholar]
- 12.Association of State and Territorial Health Officials (ASTHO). Telehealth Resource Guide. 2017. https://www.astho.org/Health-Systems-Transformation/Medicaid-and-Public-Health-Partnerships/Telehealth-Resource-Guide/. Accessed February 11, 2021.
- 13.Hwang JS, Lappan CM, Sperling LC, et al. Utilization of telemedicine in the U.S. military in a deployed setting. Mil Med. 2014;179(11):1347–1353. doi: 10.7205/MILMED-D-14-00115 [DOI] [PubMed] [Google Scholar]
- 14.Kocev I, Achkoski J, Bogatinov D, et al. Novel approach for automating medical emergency protocol in military environment. Technol Health Care. 2018;26(2):249–261. doi: 10.3233/THC-170852 [DOI] [PubMed] [Google Scholar]
- 15.Balch D, Taylor C, Rosenthal D, et al. Shadow Bowl 2003: a collaborative exercise in community readiness, agency cooperation, and medical response. Telemed J E Health. 2004;10(3):330–342. doi: 10.1089/tmj.2004.10.330 [DOI] [PubMed] [Google Scholar]
- 16.Teich JM, Wagner MM, Mackenzie CF, et al. The informatics response in disaster, terrorism, and war. J Am Med Inform Assoc. 2002;9(2): 97–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garshnek V, Burkle FM Jr. Applications of telemedicine and telecommunications to disaster medicine: historical and future perspectives. J Am Med Inform Assoc. 1999;6(1):26–37. doi: 10.1136/jamia.1999.0060026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saadi A, Mateen FJ. International issues: teleneurology in humanitarian crises: Lessons from the Médecins Sans Frontières experience. Neurology. 2017;89(3):e16–e19. doi: 10.1212/WNL.0000000000004114 [DOI] [PubMed] [Google Scholar]
- 19.Istepanian RS, Nikogosian H. Telemedicine in Armenia. J Telemed Telecare. 2000;6(5):268–272. doi: 10.1258/1357633001935897 [DOI] [PubMed] [Google Scholar]
- 20.Smith SW, Jamin CT, Malik S, et al. Freestanding emergency critical care during the aftermath of Hurricane Sandy: implications for disaster preparedness and response. Disaster Med Public Health Prep. 2016;10(3):496–502. doi: 10.1017/dmp.2016.84 [DOI] [PubMed] [Google Scholar]
- 21.Rolland-Harris E, Mangtani P, Moore KM. Who uses telehealth? Setting a usage baseline for the early identification of pandemic influenza activity. Telemed J E Health. 2012;18(2):153–157. doi: 10.1089/tmj.2011.0110 [DOI] [PubMed] [Google Scholar]
- 22.ISfTeH. Advances in international telemedicine and e-health around the world. MediPage 2006;1. ISBN 83–89769-22–0. [Google Scholar]
- 23.Chu Y, Ganz A. WISTA: a wireless telemedicine system for disaster patient care. Mob Netw Appl. 2007;12(2–3):201–214. doi: 10.1007/s11036-007-0012-6 [DOI] [Google Scholar]
- 24.Cabrera MF, Arredondo MT, Rodriguez A, et al. Mobile technologies in the management of disasters: the results of a telemedicine solution. Proc AMIA Symp. 2001:86–89. [PMC free article] [PubMed] [Google Scholar]
- 25.Dichter JR, Kanter RK, Dries D, et al. System-level planning, coordination, and communication. Chest. 2014;146(4):e87S–e102S. doi: 10.1378/chest.14-0738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Min H, Megumi S, Andrew RH, et al. Mobile healthcare system for health checkups and telemedicine in post-disaster situations. Stud Health Technol Inform. 2015;216:79–83. doi: 10.3233/978-1-61499-564-7-79 [DOI] [PubMed] [Google Scholar]
- 27.Kyriacou E, Nicolaidou I, Hadjichristofi G, et al. Health and rescue services management system during a crisis event. Healthc Technol Lett. 2016;3(3):205–211. doi: 10.1049/htl.2016.0040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.HealthcareReady. Telehealth’s applications for preparedness and response. Resilient and ready: healthcare’s impact in emergency preparedness report. https://healthcareready.org/wp-content/uploads/2019/12/HCR_Telehealth_White_Paper_SCREEN.pdf. Accessed February 11, 2021. [Google Scholar]
- 29.American College of Emergency Physicians. Policy statement. Emergency Medicine Telemedicine. 2016. https://www.acep.org/globalassets/new-pdfs/policy-statements/emergency-medicine-telehealth.pdf. Accessed February 11, 2021.
- 30.Department of Health and Human Services. Pandemic and All Hazards Preparedness Act. Telehealth report to Congress. Public Law 109–417. 2009. https://www.phe.gov/Preparedness/legal/pahpa/Documents/telehealthrtc-091207.pdf. Accessed February 11, 2021. [Google Scholar]
- 31.Simmons S, Alverson D, Poropatich R, et al. Applying telehealth in natural and anthropogenic disasters. Telemed J E Health. 2008;14(9):968–971. doi: 10.1089/tmj.2008.0117 [DOI] [PubMed] [Google Scholar]
- 32.Morton MJ, DeAugustinis ML, Velasquez CA, et al. Developments in surge research priorities: a systematic review of the literature following the Academic Emergency Medicine Consensus Conference, 2007–2015. Acad Emerg Med. 2015;22(11):1235–1252. doi: 10.1111/acem.12815 [DOI] [PubMed] [Google Scholar]
- 33.Poe K Telemedicine liability: Texas and other states delve into the uncertainties of health care delivery via advanced communications technology. The Review of Litigation. 2001;20(3). [Google Scholar]
- 34.Kim YS. Telemedicine in the USA with focus on clinical applications and issues. Yonsei Med J. 2004;45(5):761–775. [DOI] [PubMed] [Google Scholar]
- 35.Turnock M, Mastouri N, Jivraj A. Pre-Hospital Application of Telemedicine in Acute-Onset Disaster Situations. McMaster University; 2008. [Google Scholar]
- 36.Olariu S, Maly K, Foudriat EC, et al. Telemedicine for disaster relief: a novel architecture. J Mob Multimed. 2006;1(4):285–306. [Google Scholar]
- 37.Meade K, Lam DM. A deployable telemedicine capability in support of humanitarian operations. Telemed J E Health. 2007;13(3):331–340. doi: 10.1089/tmj.2006.0040 [DOI] [PubMed] [Google Scholar]
- 38.Davis TM, Barden C, Dean S, et al. American Telemedicine Association Guidelines for TeleICU Operations. Telemed E Health. 2016;22(12): 971–980. doi: 10.1089/tmj.2016.0065 [DOI] [PubMed] [Google Scholar]
- 39.Turvey C, Coleman M, Dennison O, et al. American Telemedicine Association Practice Guidelines for Video-Based Online Mental Health Services. Telemed E Health. 2013;19(9):722–730. doi: 10.1089/tmj.2013.9989 [DOI] [PubMed] [Google Scholar]
- 40.HealthcareReady. Telehealth in emergency preparedness and response. HealthcareReady. https://healthcareready.org/wp-content/uploads/2019/12/HCR_Telehealth_Brief_SCREEN_2.pdf. Accessed February 11, 2021. [Google Scholar]
- 41.Chen ET. Considerations of telemedicine in the delivery of modern healthcare. Am J Manage. 2017;17(3). [Google Scholar]
- 42.Arisoylu M, Mishra R, Rao R, et al. 802.11 Wireless infrastructure to enhance medical response to disasters. AMIA Annu Symp Proc. 2005; 2005:1–5. [PMC free article] [PubMed] [Google Scholar]
- 43.Stănescu A, Gordon PE, Copotoiu SM, et al. Moving toward a universal digital era in mass casualty incidents and disasters: emergency personnel’s perspective in Romania. Telemed J E Health. 2018;24(4):283–291. doi: 10.1089/tmj.2017.0037 [DOI] [PubMed] [Google Scholar]
- 44.Norris AC, Martinez S, Labaka L, et al. Disaster E-Health: A New Paradigm for Collaborative Healthcare in Disasters. 2015. http://idl.iscram.org/files/acnorris/2015/1252_ACNorris_etal2015.pdf. Accessed February 11, 2021.
- 45.Rolston DM, Meltzer JS. Telemedicine in the intensive care unit: its role in emergencies and disaster management. Crit Care Clin. 2015;31(2):239–255. doi: 10.1016/j.ccc.2014.12.004 [DOI] [PubMed] [Google Scholar]
- 46.Reynolds HN, Sheinfeld G, Chang J, et al. The Tele-Intensive Care Unit during a disaster: seamless transition from routine operations to disaster mode. Telemed E Health. 2011;17(9):746–749. doi: 10.1089/tmj.2011.0046 [DOI] [PubMed] [Google Scholar]
- 47.UNDRR. Terminology online glossary. https://www.undrr.org/terminology/disaster. Accessed February 11, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.