Abstract
Background
The effects of the COVID-19 pandemic on mental health have been understudied among vulnerable populations, particularly in fragile and conflict-affected settings. We aimed to analyse how the pandemic is related to early changes in mental health and parenting stress among caregivers, many of whom are internally displaced persons (IDP), in a conflict-affected setting in Colombia.
Methods
For this cohort study, we used longitudinal data from a psychosocial support programme in which 1376 caregivers were randomly assigned across four sequential cohorts. Recruitment of participants took place in March, 2018, for cohort 1; July, 2018, for cohort 2; March, 2019, for cohort 3; and July, 2019, for cohort 4. Participants completed assessments at baseline, 1-month, and 8-month follow-ups. The 8-month assessment occurred before the COVID-19 pandemic for participants in cohorts 1 and 2 (n=573), whereas those in cohorts 3 and 4 (n=803) were assessed during the early stages of the pandemic, 2–5 weeks after the national lockdown began on March 25, 2020. Primary caregiver anxiety and depression were measured with a scale adapted from the Symptoms Checklist-90-Revised and parenting stress was measured with the short form of the Parenting Stress Index. We estimated how mental health changed by comparing prepandemic and postpandemic 8-month outcomes using lagged-dependent variable models.
Findings
Results showed that the likelihood of reporting symptoms above the risk threshold increased by 14 percentage points for anxiety (95% CI 10–17), 5 percentage points for depression (0·5–9), and 10 percentage points for parental stress (5–15). The deterioration in mental health was stronger for IDP, participants with lower education or pre-existing mental health conditions, and for those reporting a higher number of stressors, including food insecurity and job loss.
Interpretation
Maternal mental health significantly worsened during the early stages of the pandemic. Considering the vulnerability and pre-existing mental health conditions of this population, the estimated effects are substantial. Policies in fragile and conflict-affected settings targeting IDP and other vulnerable people will be important to mitigate further mental health and socioeconomic problems.
Funding
Saving Brains–Grand Challenges Canada, Fundación Éxito, Fundación FEMSA, United Way Colombia, Universidad de los Andes.
Translation
For the Spanish translation of the abstract see Supplementary Materials section.
Introduction
The COVID-19 pandemic and resulting public health measures implemented worldwide have had profound impacts on people's health, livelihoods, and daily life. Understanding the effects of the pandemic on mental health is important to guide policies to prevent further adverse effects, especially among vulnerable and underserved populations.
Emerging research has analysed the relationship between the pandemic and mental health in the general population. There is increasing evidence of negative early impacts. With longitudinal data from a representative sample in the UK, one study found that mental distress increased from 19% in 2018–19 to 27% 1 month into the lockdown, which began on March 25, 2020.1 Similar shifts have been observed in other studies in high-income countries2 and across high-income and middle-income countries.3, 4
Studies suggest that the psychosocial burden of the pandemic differs across populations. Socioeconomically vulnerable families, women with young children, and individuals with pre-existing mental health conditions are at a higher risk.1 The pandemic might thus exacerbate inequalities related to socioeconomic and mental health vulnerabilities. However, research in low-income and middle-income countries, and particularly within marginalised populations, remains scant.5 The effects of the pandemic in fragile and conflict-affected settings, and on internally displaced persons (IDP; as defined by the International Organization for Migration), have been largely unexplored.
Research in context.
Evidence before this study
We searched Google Scholar and PubMed with the terms “mental health”, “COVID-19/pandemic”, and “lockdowns/quarantine” between March 1, 2020, and Sept 18, 2020. We further consulted two research repositories: the Primer on Research Activities on COVID-19 and Forcibly Displaced People from the World Bank–UNHCR Joint Data Center of Forced Displacement, and the Research for Effective COVID-19 Responses from Innovations for Poverty Action, searching for “low and middle-income country” and “fragile and conflict affected setting”. A sizeable number of studies assess the early effect of the pandemic and related policy responses on mental health in the general population. However, most of these studies provided evidence for high-income countries, and many were limited to descriptive analyses with cross-sectional data, without pre-COVID-19 assessments, and without considering a counterfactual. Two studies reported more advanced evidence employing longitudinal data in the UK and in rural Bangladesh, whereas another exploited variation in the extent of lockdowns across the different states and times in the USA. These studies found a high prevalence of symptoms of psychological distress and other related difficulties. We did not identify studies that provided descriptive or rigorous evidence on the psychosocial effects of the pandemic in fragile and conflict-affected settings or among forcibly displaced people.
Added value of this study
To the best of our knowledge, our study is the first to consider the early changes in maternal mental health associated with the COVID-19 pandemic in a fragile and conflict-affected setting. We measured these changes using longitudinal data collected for a randomised controlled trial of conflict-affected and vulnerable caregivers whose children were enrolled at public early childhood development centres in Tumaco, Colombia. The phased-in design of the evaluation allowed us to estimate the changes in mental health associated with the pandemic by comparing outcomes for cohorts exposed and not exposed to the pandemic, adjusting for mental health and other characteristics at baseline. We observed substantial increases in anxiety, depression, and parenting stress. Furthermore, we saw a stronger deterioration in mental health for people with a history of internal displacement, lower levels of education, pre-existing mental health conditions, and more COVID-19 related stressors. This result underlines the vulnerabilities within communities in fragile and conflict-affected settings.
Implications of all the available evidence
Although the COVID-19 pandemic and associated public health measures have had a global effect on mental health, the burden is not equally borne, and specific populations have had stronger and more persistent effects. For example, in fragile and conflict-affected settings, the vulnerability to the psychosocial consequences of the pandemic is intensified by multidimensional and overlapping challenges, which further contribute to deepening the vulnerability of these populations. This vulnerability can have consequences for wellbeing and poverty dynamics well beyond the pandemic. The observed deterioration in mental health affects the wellbeing of mothers and their young children, as shown by other studies. Unfortunately, internally displaced persons (IDP), and populations in fragile and conflict-affected settings are largely underserved and neglected in terms of psychosocial and social protection services. Strategies that leave no one behind are essential, especially given the protracted nature of the COVID-19 crisis and the scope of future lockdowns and economic recession. Providing improved access to mental health and enhanced social protection measures, such as cash transfers, which help attenuate the effect of key stressors, such as job loss and food insecurity, might be an effective way to help reduce disparities that affect IDP and communities exposed to violence worldwide.
An estimated 2 billion people reside in fragile and conflict-affected settings, and the total number of IDP increased to 79·5 million people by 2019, representing 1% of the population worldwide.6 IDP reside in environments characterised by persistent fragility, institutional failures, protracted conflict and violence, and socioeconomic vulnerability and exclusion.7 Their experience of violence and displacement also increases their likelihood of pre-existing mental health conditions.8 The psychosocial effect of the pandemic might be intensified by pre-existing vulnerabilities and have consequences for wellbeing beyond the pandemic. For example, negative effects on maternal mental health and parenting practices can disrupt early childhood development and have adverse long-term and intergenerational consequences.9
Decades of civil conflict have left strong marks in Colombia. With over 8 million IDP, representing 18% of its population, the country has accommodated the highest number of IDP of any country worldwide.10 After the peace agreement between the Colombian State and the Fuerzas Armadas Revolucionarias de Colombia guerrilla in 2016, armed groups fought for territorial control of specific municipalities, resulting in increased civilian victimisation and displacement. These municipalities, including Tumaco, were prioritised in the peace agreement because of their weak institutional capacity and history of continuing violent conflict.
The current study aimed to investigate the early changes in mental health and parenting stress associated with the onset of the pandemic among young caregivers in Tumaco, Colombia. Because the effects of COVID-19 itself cannot be distinguished from the effects of the policy responses and ensuing health and socioeconomic crises,11 we refer to the pandemic as the cumulative shock of these factors. Findings on the deterioration of mental health among this vulnerable population have great potential to raise awareness about the long-term consequences of inaction, especially in fragile and conflict-affected settings.
Methods
Setting
Tumaco is a municipality on the Pacific coast of Colombia with a population of 257 052 people, 90% of whom are Afro-Colombian. Strongly affected by the long-lasting civil conflict, Tumaco meets the criteria of a fragile and conflict-affected setting. The rate of homicide is five times above the national average and the rate of forced displacement is seven times above the national average. IDP account for 10% of the population, and most of the population have directly been exposed to violence. Tumaco is below the national averages in all socioeconomic indicators: 45% of its population is below the national multidimensional poverty line and 92% of its working-age population earns their income from informal work. Access to public services is also poor: 44% of the population have no access to safe drinking water, and available hospital beds and intensive care units are minimal. The disadvantaged profile of Tumaco is summarised in appendix 2 (p 2).
Participants and procedures
The participants in our cohort study were 1376 primary caregivers who took part in a cluster-randomised trial of Semillas de Apego, a psychosocial group programme based on the Child–Parent Psychotherapy.12 Participants were recruited in March, 2018, for cohort 1; July, 2018, for cohort 2; March, 2019, for cohort 3; and July, 2019, for cohort 4. The programme seeks to restore maternal mental health and improve early childhood development among violence-exposed families. The programme was implemented between 2018 and 2020 in 18 public early childhood development centres (ECDCs) serving 80% of the 1600 children aged 2–5 years enrolled across public ECDCs. The geographical distribution of ECDCs and poverty rates of the neighbourhoods where these centres are located are shown in appendix 2 (p 3).
Random assignment was done in two stages. First, ECDCs were randomised to the treatment or control groups. Second, with census data for each ECDC, all caregivers of children who were attending an ECDC were randomly allocated to four sequential cohorts following a phased-in approach. In each cohort, the treatment group caregivers were invited to participate in Semillas de Apego in addition to regular child and family services provided by the ECDC, whereas control group caregivers received regular services. Enrolment was open to all caregivers regardless of specific mental health needs. 1376 primary caregivers participated over the course of the programme in the treatment (n=714) or control (n=662) groups. The second randomisation over time gives rise to a natural occurring experiment, which is the focus of this study.
Participants completed comprehensive assessments at baseline, 1-month, and 8-month follow-ups. Data were collected in person, with the exception of the 8-month follow-up for cohorts 3 and 4, which were collected via phone due to the COVID-19 pandemic. Phone surveys were administered 2–5 weeks after the national lockdown began on March 25, 2020. Consequently, the 8-month assessment for participants in cohorts 3 and 4 occurred during the onset of the pandemic.
Study procedures were approved by the Ethics Committee of the Universidad de los Andes, Colombia (protocol 786, 2017). The trial was registered with ClinicalTrials.gov (NCT03502252) and the American Economic Association's registry for randomised controlled trials (AEARCTR-0002868). The amendment for phone surveys was registered to the American Economic Association's registry on April 20, 2020. The evaluation of the programme's effect, including whether it mitigated the burden of the pandemic, is ongoing.
Outcomes
Primary caregiver anxiety and depression were measured with a scale adapted from the Symptoms Checklist-90-Revised,13 which has been validated previously among IDP in Colombia.14 To reduce participant burden, phone surveys used an abbreviated version that only included items loading onto these two domains. Internal consistency was high for both anxiety (α=0·89) and depression (α=0·90), as were Cronbach's alphas for the instrument across cohorts, and in-person and phone surveys. Confirmatory factor analysis shows adequate fit (appendix 2 pp 7–8). Two summary indicators were obtained for each outcome: a T-score reflecting the sum of all items and a binary variable for when the T-score is above a critical threshold (Ti=63, as defined by the scale), indicating risk of developing severe symptoms.
Parenting stress was measured with the short form of the Parenting Stress Index,15 which has been validated in Latinx populations.16 Internal consistency was high (α=0·89), and confirmatory factor analysis shows adequate fit (appendix 2 pp 7–8). The Parenting Stress Index provides a T-score for total stress and a binary variable for when the T-score is above the critical threshold. Following Barroso and colleagues,17 we used the 73rd percentile of the distribution as the critical cutoff, given that we worked with at-risk populations.
Statistical analysis
We leveraged the phased-in evaluation design, and in particular, that the 8-month assessment occurred before the COVID-19 pandemic for participants randomly allocated to cohorts 1 and 2 (n=573) and 2–5 weeks into the pandemic for those randomly allocated to cohorts 3 and 4 (n=803). For brevity, we referred to these groups as the prepandemic and postpandemic cohorts, respectively.
First, we assessed the changes in mental health associated with the pandemic by comparing unconditional means for each mental health outcome at 8-month follow-up between participants in the prepandemic and postpandemic cohorts. A robustness analysis compared the 1-month and 8-month outcomes for participants in the postpandemic cohorts; this analysis involved the prepandemic and postpandemic comparison within these cohorts. Second, we estimated differences in the conditional means calculated from regressing each outcome on the exposure variable (an indicator variable for the postpandemic cohorts) and controlling for the baseline lagged-dependent variable and other demographic characteristics, similar to an ANCOVA model (appendix 2 p 5). The advantage of this approach is that it controls for the secular trend and for baseline individual characteristics. The outcome variables of interest are the binary measures because they provide a clear indicator of severity. We assessed the robustness of results under alternative thresholds, for continuous T-scores and when controlling for 1-month follow-up mental health outcomes.
Our empirical strategy builds on the random assignment of participants to cohorts and the resulting natural experiment in which the 8-month follow-up was administered early on during the pandemic for two of the cohorts. Balance in baseline characteristics and an F-statistic of 3·68 for joint-significance test confirmed the similarity of participants across prepandemic and postpandemic cohorts (table 1 , appendix 2 p 8). Further, the regression analysis accounts for remaining differences between the prepandemic and postpandemic cohorts and for secular trend. The identification assumption is that the exposure variable captures the difference in exposure to the pandemic between cohorts. Although the other factors that changed across the two periods cannot be excluded, there is a large and general agreement that the COVID-19 pandemic is by far the dominant factor, which makes attribution credible.18 The programme's timeline informing this empirical strategy is available in appendix 2 (p 4).
Table 1.
Sample profile and balance at baseline between prepandemic and postpandemic cohorts
| Full sample (n=1376) | Prepandemic cohorts 1 and 2 (n=573) | Postpandemic cohorts 3 and 4 (n=803) | Prepandemic vs postpandemic cohort differences (95% CI) | p value | |
|---|---|---|---|---|---|
| Participants' characteristics | |||||
| Caregiver's age, years | 29·06 (9·26) | 29·07 (9·30) | 29·05 (9·24) | −0·02 (−1·008 to 0·979) | 0·98 |
| Caregiver is female | 1319 (95·9%) | 538 (93·9%) | 781 (97·3%) | 0·03 (0·012 to 0·055) | 0·0020 |
| Mother is caregiver | 1199 (87·1%) | 487 (85·0%) | 712 (88·7%) | 0·04 (0·001 to 0·073) | 0·045 |
| Caregiver's years of education | 11·85 (3·67) | 11·86 (3·90) | 11·85 (3·51) | −0·01 (−0·404 to 0·384) | 0·96 |
| Household characteristics | |||||
| Household size | 5·00 (1·99) | 5·00 (2·06) | 5·00 (1·95) | 0·01 (−0·209 to 0·219) | 0·96 |
| Number of children younger than 5 years | 1·29 (0·56) | 1·32 (0·57) | 1·27 (0·55) | −0·05 (−0·107 to 0·013) | 0·13 |
| Index child age, months | 35·30 (8·38) | 34·53 (6·57) | 35·85 (9·42) | 1·31 (0·417 to 2·209) | 0·0041 |
| Two-parent household | 967 (70·3%) | 399 (69·6%) | 568 (70·7%) | 0·01 (−0·038 to 0·060) | 0·66 |
| Highest years of education in the household | 12·69 (3·31) | 12·68 (3·50) | 12·71 (3·18) | 0·03 (−0·324 to 0·388) | 0·86 |
| Asset index | −0·26 (1·37) | −0·20 (1·34) | −0·29 (1·38) | −0·09 (−0·236 to 0·056) | 0·23 |
| Access to public water supply | 734 (53·3%) | 300 (52·4%) | 434 (54·0%) | 0·02 (−0·037 to 0·070) | 0·54 |
| Access to sewage service | 300 (21·8%) | 112 (19·5%) | 188 (23·4) | 0·04 (−0·006 to 0·083) | 0·087 |
| Beneficiary of conditional cash transfers | 585 (42·5%) | 277 (48·3%) | 308 (38·4%) | −0·10 (−0·153 to −0·047) | 0·0002 |
| Monthly household income per capita (2017 US$) | 267·84 (629·66) | 266·97 (484·43) | 268·45 (715·80) | 1·48 (−66·087 to 69·058) | 0·97 |
| Head of household is employed in the previous week | 1136/1374 (82·7%) | 464 (81·0%) | 672/801 (83·9%) | 0·03 (−0·011 to 0·070) | 0·16 |
| Head of household has a formal job | 286/1346 (21·2%) | 115/557 (20·6%) | 171/789 (21·7%) | 0·01 (−0·034 to 0·055) | 0·65 |
| Days worked by head of household in a month | 23·75 (6·43); n=1105 | 23·35 (6·57); n=439 | 24·02 (6·32); n=666 | −0·20 (−1·054 to 0·653) | 0·087 |
| Exposure to violence | |||||
| Victim of direct violence | 1127 (81·9%) | 464 (81·0%) | 663 (82·6%) | 0·02 (−0·025 to 0·057) | 0·45 |
| Number of violent events | 2·36 (1·80) | 2·41 (1·87) | 2·33 (1·75) | −0·08 (−0·274 to 0·112) | 0·41 |
| Internally displaced persons | 787 (57·2%) | 349 (60·9%) | 438 (54·5%) | −0·06 (−0·117 to −0·011) | 0·019 |
| Mental health | |||||
| Anxiety T-score | 57·09 (6·87) | 57·21 (6·74) | 57·01 (6·96) | −0·20 (−0·938 to 0·536) | 0·59 |
| Anxiety above risk threshold | 220 (16·0%) | 85 (14·8%) | 135 (16·8%) | 0·02 (−0·02 to 0·059) | 0·32 |
| Depression T-score | 59·80 (6·99) | 59·91 (7·07) | 59·73 (6·93) | −0·19 (−0·936 to 0·564) | 0·63 |
| Depression above risk threshold | 376 (27·3%) | 151 (26·3%) | 225 (28·0%) | 0·02 (−0·031 to 0·065) | 0·49 |
| Parenting Stress Index T-score | 52·64 (7·08) | 52·14 (7·45) | 53·00 (6·79) | 0·87 (0·11 to 1·628) | 0·025 |
| Parenting Stress Index above risk threshold (73rd percentile was used as the cutoff) | 450 (32·7%) | 169 (29·5%) | 281 (35·0%) | 0·06 (0·005 to 0·105) | 0·032 |
Data are mean (SD), number (%), mean-difference test between the prepandemic cohorts and the postpandemic cohorts (95% CI), and p value for the difference. Cohorts 1 and 2 are referred to as the prepandemic cohorts because all assessments were administered before to the pandemic. Cohorts 3 and 4 are referred to as the postpandemic cohorts because their final assessment was conducted 2–5 weeks into the pandemic.
We did an exploratory analysis to understand two dimensions of heterogeneity. We assessed whether the changes in mental health varied according to baseline characteristics to explore which characteristics increased susceptibility to experiencing at-risk mental health symptoms. For this purpose, we estimated the same lagged-dependent variable model described earlier in this section, adding an interaction between an individual characteristic and the exposure variable. Because many of the characteristics of interest covary, we estimated separate models, one for each characteristic.19 We then explored how mental health varied according to the types of pandemic-related stressors. Since information on these stressors was only collected in phone surveys, this analysis was done for the postpandemic cohorts only. Specifically, we estimated separate models in which we regressed each mental health outcome on an indicator variable for each stressor, controlling for baseline mental health and demographic characteristics. In an alternative specification, we also estimated the effect of the number of pandemic-related stressors.
Role of the funding source
The funders had no role in the study design, data collection and analysis, or the writing of the report.
Results
Table 1 displays baseline characteristics of participants. The average participant age was 29 years, 1319 (96%) of 1376 were women, the average years of education was 11·85, and 1136 (83%) of 1376 were employed in the previous week, but only 286 (21%) of 1374 had a formal job. Households in the sample were 0·26 SD below the national mean on an asset-wealth index, confirming multidimensional poverty. 1127 (82%) of 1376 participants have had at least one episode of violence and 787 (57%) were IDP. At baseline, 220 (16%) of 1376 participants scored above the at-risk thresholds for anxiety, 376 (27%) for depression, and 450 (33%) for parenting stress, all above national averages.8 1245 (90%) of 1376 participants at baseline completed the second follow-up survey. Attrition was not different between the prepandemic (9%) and postpandemic cohorts (10%) and was not predicted by baseline characteristics (appendix 2 pp 9–12).
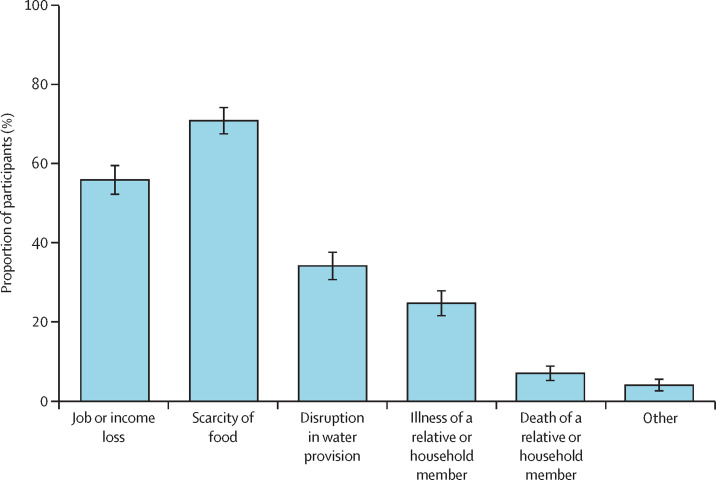
Figure 1 summarises the pandemic-related stressors occurring in the last 7 days obtained from phone surveys. A scarcity of food was reported most frequently by 510 (71%) of 723 participants, followed by job or income loss by 402 (56%) participants, and disruption in water supply by 245 (34%) participants. The scarcity of food and job and income loss persisted as the most frequent stressors over the 4 weeks of survey administration.
Figure 1.
Stressors triggered by the COVID-19 pandemic
Proportion of participants in the postpandemic cohorts who reported having issues the week before the 8-month follow-up survey. The error bars represent the 95% CI.
Table 2 reports the percentage of participants who scored above the at-risk thresholds for anxiety, depression, and parenting stress index at each assessment, reporting unconditional means. These scores provide a first picture of the deterioration in mental health associated with the pandemic. At baseline, there were small and statistically insignificant differences between the prepandemic and postpandemic cohorts in at-risk symptoms of anxiety (2 percentage points; 95% CI −2 to 6) and depression (2 percentage points; −3 to 7), and a statistically significant difference for at-risk parental stress (6 percentage points; 0·5 to 11). At the 1-month follow-up, participants in the postpandemic cohort showed a lower prevalence of at-risk symptoms of anxiety, depression, and parenting stress than participants in the prepandemic cohort. These differences are statistically significant for at-risk anxiety (7 percentage points; 95% CI −10 to −3) and depression (5 percentage points; −9 to −0·4), but not for parental stress (3 percentage points: −80 to 20). At the 8-month follow-up, these differences revert and at-risk symptoms become larger and statistically different for the postpandemic cohort relative to the prepandemic cohort signalling to the deterioration of mental health associated with the pandemic. Participants in the postpandemic cohorts had a probability of being above the risk threshold that was 14 percentage points higher for anxiety (10–18), 5 percentage points higher for depression (0·4–10), and 10 percentage points higher for parental stress (5–15) relative to participants in the prepandemic cohorts.
Table 2.
Unconditional means and differences in the likelihood of experiencing at-risk mental health symptoms
| Prepandemic cohorts 1 and 2 (n=573) | Postpandemic cohorts 3 and 4 (n=803) | Difference (percentage points, 95% CI) | p value | |
|---|---|---|---|---|
| Baseline | ||||
| Anxiety above risk threshold | 85/573 (14·8%) | 135/803 (16·8%) | 2 (−2 to 6) | 0·32 |
| Depression above risk threshold | 151/573 (26·4%) | 225/803 (28·0%) | 2 (−3 to 7) | 0·49 |
| Parenting Stress Index above risk threshold (73rd percentile was used as the cutoff) | 169/573 (29·5%) | 281/803 (35·0%) | 6 (0·5 to 11) | 0·032 |
| 1-month follow-up | ||||
| Anxiety above risk threshold | 87/553 (15·7%) | 68/765 (8·9%) | −7 (−10 to −3) | 0·0001 |
| Depression above risk threshold | 135/553 (24·4%) | 149/765 (19·5%) | −5 (−9 to −0·4) | 0·032 |
| Parenting Stress Index above risk threshold (73rd percentile was used as the cutoff) | 184/553 (33·3%) | 232/765 (30·3%) | −3 (−80 to 20) | 0·25 |
| 8-month follow-up | ||||
| Anxiety above risk threshold | 44/522 (8·4%) | 159/723 (22·0%) | 14 (10 to 18) | <0·0001 |
| Depression above risk threshold | 99/522 (19·0%) | 174/723 (24·1%) | 5 (0·4 to 10) | 0·032 |
| Parenting Stress Index above risk threshold (73rd percentile was used as the cutoff) | 141/522 (27·0%) | 267/723 (36·9%) | 10 (5 to 15) | 0·0002 |
Data are number of participants (%) with mental health symptoms above the at-risk thresholds in the prepandemic and postpandemic cohorts, mean-difference test between the prepandemic and postpandemic cohorts in percentage points (95% CI), and p value of the difference. Cohorts are referred to as the prepandemic and postpandemic cohorts, signaling that all assessments were administered before the pandemic for cohorts 1 and 2, but the second follow-up for cohorts 3 and 4 was administered 2–5 weeks into the pandemic. Data on the continuous T-scores at each assessment are reported in the appendix 2 (p 5). Statistics are based on the original sample at baseline, and the smaller samples observed at 1-month and 8-month follow-ups due to attrition.
For participants in cohorts 3 and 4, data are available for the 1-month follow-up, just before the pandemic, and for the 8-month follow-up, just into the pandemic (appendix 2 p 5). These data allow comparison of the changes in outcomes within participants before and after the pandemic began. We observe changes in at-risk anxiety of 13 percentage points (95% CI 9–17), at-risk depression of 4 percentage points (0·4–9), and at-risk parental stress of 6 percentage points (2–11).
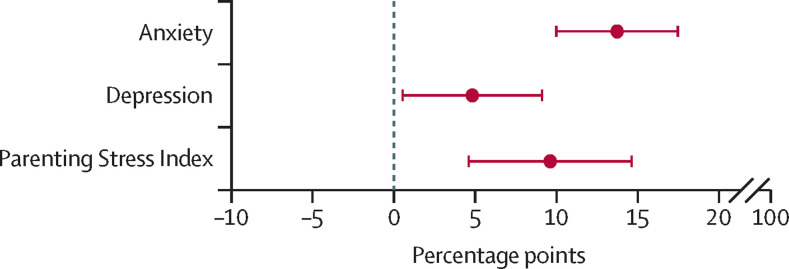
Figure 2 shows the point estimates for the conditional differences in the likelihood of at-risk symptoms of anxiety, depression, and parenting stress between prepandemic and postpandemic cohorts following the lagged-dependent variable model (appendix 2 p 6). The COVID-19 pandemic is associated with a sizeable deterioration on each mental health dimension. Participants in postpandemic cohorts had, on average, a 14-percentage point higher probability of reporting anxiety rates above the at-risk threshold compared with the prepandemic cohorts (95% CI 10–17). This represents an 88% increase in the probability of scoring above the risk threshold relative to the baseline mean. Participants in the postpandemic cohorts had a 5-percentage point higher probability of reporting depression rates above the risk threshold (0·5–9), representing a 19% increase relative to the baseline mean. For parental stress, participants had a 10-percentage point higher probability of scoring above the risk threshold postpandemic (5–15), representing a 30% increase relative to baseline.
Figure 2.
Conditional differences in the likelihood of at-risk mental health symptoms
Coefficient plot of point estimates and 95% CIs for the differences in the at-risk mental health symptoms between prepandemic and postpandemic cohorts. Estimates come from the lagged-dependent variable model discussed in the Methods section in which the probability of having anxiety, depression, or parenting stress symptoms above the at-risk thresholds was regressed on the postpandemic treatment indicator, controlling for the baseline lagged-dependent variable and a set of baseline demographic and socioeconomic controls (appendix 2 p 6).
Results were robust when using continuous T-scores for mental health domains and when considering alternative Parenting Stress Index thresholds. Differences were slightly larger when controlling for mental health at 1-month follow-up (appendix 2 pp 16–17).
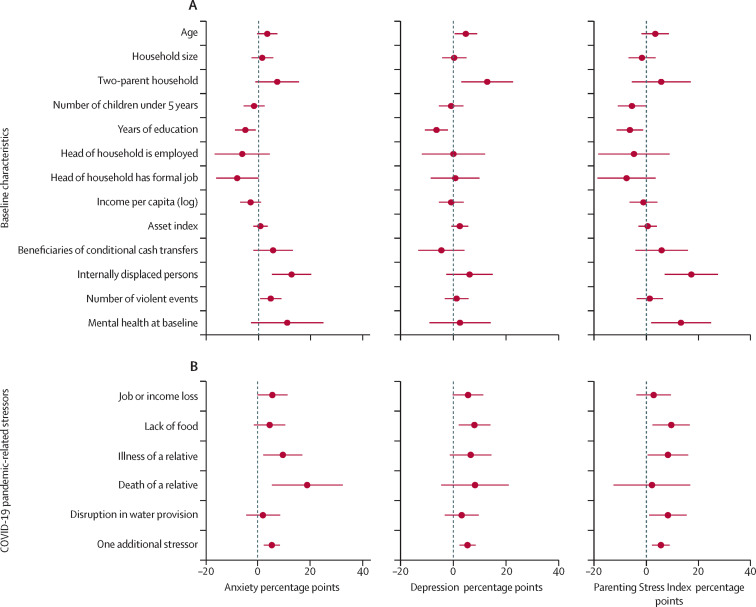
Figure 3 reports the results from the exploratory analysis on the moderating role of baseline characteristics and pandemic-related stressors. IDP, caregivers with less education, and those with pre-existing mental health conditions were more susceptible to worsening mental health symptoms. IDP status increased the likelihood of at-risk anxiety by 13 percentage points (95% CI 5–20) and parenting stress by 17 percentage points (7–28). IDP status also increased the probability of at-risk depression by 6 percentage points, but this was not statistically significant at conventional levels (−3 to 15). An extra year of education reduced the toll on anxiety by 0·5 percentage points (1–9), on depression by 0·6 percentage points (2–11), and on parenting stress by 0·6 percentage points (1–12). Although beneficiaries of conditional cash transfers were eligible for additional aid from the Colombian Government, their symptoms of mental health problems are similar to those of non-beneficiaries. Finally, the likelihood of at-risk anxiety increased by 11 percentage points (95% CI −3 to 25), although, this difference is not statistically significant at conventional levels, whereas at-risk parenting stress increased by 13 percentage points (2–25) for those already at-risk at baseline (appendix 2 p 6).
Figure 3.
Moderating factors
Coefficient plot of the point estimates and 95% CIs for the moderating role of baseline demographic and socioeconomic characteristics (A) and pandemic-related stressors (B) on differences in mental health between prepandemic and postpandemic cohorts. Estimates for the baseline demographic and socioeconomic characteristics are from separate models in which the mental health outcome was regressed on the postpandemic treatment indicator and the interaction of this indicator with the variable listed in the vertical axis. Estimates for the pandemic-related stressors are from separate models in which the mental health outcome was regressed on the pandemic-related stressors. All models control for the baseline lagged-dependent variable and demographic and socioeconomic controls. Continuous moderators are standardised. The full results are reported in the appendix 2 (pp 6–7).
Figure 3B displays the heterogeneity according to pandemic-related stressors. Anxiety increased by 6 percentage points (95% CI 0–11) for those who reported job or income loss, by 10 percentage points (2–17) for those who reported illness, and by 19 percentage points (6–32) for those who reported death of a relative. Participants who reported food insecurity also showed an increased likelihood of at-risk depression of 8 percentage points (2–14) and of parenting stress of 10 percentage points (2–17). Illness of a relative resulted in a larger deterioration of 8 percentage points on at-risk parenting stress (0·5–16). Overall, one additional stressor raised the probability by 5 percentage points of at-risk anxiety (2–9), depression (2–8), and parenting stress (2–9). Full results are in the appendix 2 (p 7).
The risk threshold analysis undervalues the overall deterioration of mental health. Analysis of the corresponding T-scores indicated substantial and significant overall increases in at-risk symptoms, especially for IDP and participants who reported food insecurity or pre-existing mental health conditions (appendix 2 pp 19, 21, 23).
Discussion
This study responds to the call for rapid research to further understand the indirect effects of the COVID-19 pandemic.20 Findings complement emerging literature1, 5, 21 by examining how the pandemic is associated with worsening maternal mental health among a highly vulnerable and violence-exposed population of caregivers with young children in Colombia. To our knowledge, this study provides the first rigorous evidence on the deterioration in mental health associated with the COVID-19 pandemic in a fragile and conflict-affected setting.
Shortly after the Colombian Government issued a national lockdown on March 25, 2020, caregivers in this study were surveyed and reported the accumulation of different stressors, including job losses, food insecurity, and the illness or death of a household member. Compared with the cohorts assessed before the pandemic, caregivers had significant increases in anxiety, depression, and parenting stress, reaching thresholds at the risk level for developing clinical disorders. Significant increases in at-risk anxiety, depression, and parenting stress are particularly concerning given that participants had above-average symptoms at baseline. The deterioration in mental health most likely reflects the multiplicity of challenges faced in fragile and conflict-affected settings, which increase vulnerability to developing mental health problems.
For instance, findings indicated that the adverse changes in mental health associated with the pandemic varied depending on socioeconomic and violence-related vulnerabilities. Caregivers with higher levels of education had lower changes, suggesting that education might serve as a protective factor, consistent with evidence from natural disasters and other calamities,22 and emerging evidence on the pandemic in Colombia.23 By contrast, IDP and participants with pre-existing mental health conditions were more likely to have increased anxiety, depression, and parenting stress. This elevated vulnerability might be associated with the precarious income and employment and restricted social support of IDP.24 Because of previous histories of trauma and violence, IDP might also have had more difficulty in managing stressors related to the COVID-19 pandemic.8 These results are consistent with previous evidence1, 5 and underscore that the consequences of the pandemic are by the vulnerability of IDP, exposing them to simultaneous and reinforcing risks.
We cannot isolate the effects of the spread of COVID-19 from the effects of contingency measures, socioeconomic crisis, and reduction in public health provisions. These factors were common to all participants in the postpandemic assessments. Nevertheless, exploratory analyses on the moderating role of different stressors indicates that job loss and food insecurity, along with death or illness of a relative or friend, contributed to heightened mental health problems. Results also indicated a dose-dependent response: participants who reported more stressors, had a higher likelihood of reporting at-risk symptoms. Findings are consistent with previous studies among broader populations on the mental health effects of poverty25 and previous pandemics.26, 27
The worsening in mental health associated with the pandemic might have direct long-term consequences by reinforcing poverty dynamics and socioeconomic exclusion.25 Likewise, the detrimental psychosocial changes can have long-term and intergenerational consequences. Food insecurity and the disruption of health services heightens the risk of child and maternal mortality among the poor, as indicated by a recent modelling study in low-income and middle-income countries in the wake of the COVID-19 pandemic.28 Furthermore, heightened rates of maternal depression, anxiety, and parenting stress might stunt child physical, cognitive, and socioemotional development, and can also augment chances of household violence. Together, these factors can have harmful effects on the life trajectories of mothers and children.29, 30
Our study has several limitations. The absence of data on stressors for the prepandemic cohort and the low underlying variation in pandemic related stressors limited our capacity to explore the mechanisms in a more comprehensive way; our analysis on moderators is largely exploratory. Phone-based survey administration limited the amount and depth of data obtained at endline for these cohorts—for example, on attitudes and coping strategies and on reception of transfers. The comparison over time does not consider time-variant factors that might have affected mental health simultaneously. Finally, our study focuses on the early mental health deterioration associated with the pandemic. Further studies on longer-term effects on mental health, on whether differential effects on anxiety and depression persist, and on outcomes such as early childhood development are needed.
The findings of this study highlight the heightened struggle faced by more vulnerable populations in coping with COVID-19. Although the study is set in a particular setting, many of the observed challenges are common to fragile and conflict-affected settings in Colombia and worldwide. Developing an inclusive approach to mitigate negative mental health effects of the pandemic, particularly among IDP and communities exposed to violence worldwide, is crucial. Increased provision of mental health services and improved social protection is also needed.24 Additionally, widespread implementation of cash transfer programmes coupled with psychosocial services is a promising way to help reduce disparities that have been exacerbated by the pandemic.
Data sharing
All anonymised individual participant data and a data dictionary will be made available immediately after the preprint of the Semillas de Apego impact evaluation is made public by mid-2021. Data will be available by the corresponding author upon a signed data access agreement.
Declaration of interests
AM reports grants from Saving Brains–Grand Challenges Canada, Fundación Exito, Fundación Femsa, and United Way Colombia, which supported implementation and impact evaluation of the Semillas de Apego programme in Tumaco, Colombia, and grants from Universidad de los Andes, which supported the analysis of the data from the phone survey. MJT reports grants from Saving Brains–Grand Challenges Canada, Fundación Exito, Fundación Femsa, and United Way Colombia, during the conduct of the study. All other authors declare no competing interests.
Acknowledgments
Acknowledgments
We are grateful to the participants of the Semillas de Apego programme for their contribution to this study, especially during these difficult times. We thank Iquartil, Bogotá, Colombia, which did all data collection. Data collection was funded by Saving Brains–Grand Challenges Canada (grant number SB-POC-1809-19901), Fundación Éxito, Fundación FEMSA, and United Way Colombia.
Contributors
AM devised the study. AM and PS designed the empirical strategy with input from all authors. AM and MJT carried out data analysis and produced tables and figures. All authors contributed to the interpretation of study findings, writing the different drafts of the manuscript, and editing and commenting on the final version. All authors had access to the data and AM, PS, and MJT verified the data. The corresponding author oversaw all stages of the study, collected all data, and had final responsibility for the decision to submit for publication.
Supplementary Materials
References
- 1.Pierce M, Hope H, Ford T. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7:883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sønderskov KM, Dinesen PT, Santini ZI, Østergaard SD. The depressive state of Denmark during the COVID-19 pandemic. Acta Neuropsychiatr. 2020;32:226–228. doi: 10.1017/neu.2020.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salari N, Hosseinian-Far A, Jalali R. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health. 2020;16:57. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Serafini G, Parmigiani B, Amerio A, Aguglia A, Sher L, Amore M. The psychological impact of COVID-19 on the mental health in the general population. QJM. 2020;113:531–537. doi: 10.1093/qjmed/hcaa201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hamadani JD, Hasan MI, Baldi AJ. Immediate impact of stay-at-home orders to control COVID-19 transmission on socioeconomic conditions, food insecurity, mental health, and intimate partner violence in Bangladeshi women and their families: an interrupted time series. Lancet Glob Health. 2020;8:e1380–e1389. doi: 10.1016/S2214-109X(20)30366-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.United Nations High Commissioner for Refugees . United Nations High Commissioner for Refugees; Geneva: 2019. Global trends: forced displacement in 2018. [Google Scholar]
- 7.WHO . World Health Organization; Geneva: 2020. Health financing in fragile and conflict-affected situations: a review of the evidence. [Google Scholar]
- 8.Moya A. Violence, psychological trauma, and risk attitudes: evidence from victims of violence in Colombia. J Dev Econ. 2018;131:15–27. [Google Scholar]
- 9.Wachs TD, Black MM, Engle PL. Maternal depression: a global threat to children's health, development, and behavior and to human rights. Child Dev Perspect. 2009;3:51–59. [Google Scholar]
- 10.Registro Único de Víctimas Unidad para las Víctimas. July, 2020. https://www.unidadvictimas.gov.co/es/registro-unico-de-victimas-ruv/37394
- 11.Lin Z, Meissner CM. Health vs. wealth? Public health policies and the economy during COVID-19. Nov 11, 2020. http://www.nber.org/papers/w27099
- 12.Lieberman AF, Van Horn P, Ippen CG. Toward evidence-based treatment: child-parent psychotherapy with preschoolers exposed to marital violence. J Am Acad Child Adolesc Psychiatry. 2005;44:1241–1248. doi: 10.1097/01.chi.0000181047.59702.58. [DOI] [PubMed] [Google Scholar]
- 13.Derogatis LR, Savitz KL. In: The use of psychological testing for treatment planning and outcomes assessment. Maruish ME, editor. Lawrence Erlbaum Associates Publishers; New Jersey, NJ: 1999. The SCL-90-R, brief symptom inventory, and matching clinical rating scales; pp. 679–724. [Google Scholar]
- 14.Londoño NH, Agudelo DM, Martínez E, Anguila D, Aguirre DC, Arias JF. Validation of Derogatis' questionnaire of 90 symtoms (SCL-90-R) in a Colombian clinical sample. MedUNAB. 2018;21:45–60. (in Spanish). [Google Scholar]
- 15.Abidin RR. Psychological Assessment Resources; Lutz, FL: 2012. Parenting stress index, 4th edn: PSI-4; professional manual. [Google Scholar]
- 16.Aracena M, Gómez E, Undurraga C, Leiva L, Marinkovic K, Molina Y. Validity and reliability of the parenting stress index short form (PSI-SF) applied to a Chilean sample. J Child Fam Stud. 2016;25:3554–3564. [Google Scholar]
- 17.Barroso NE, Hungerford GM, Garcia D, Graziano PA, Bagner DM. Psychometric properties of the parenting stress index-short form (PSI-SF) in a high-risk sample of mothers and their infants. Psychol Assess. 2016;28:1331–1335. doi: 10.1037/pas0000257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bottan N, Hoffmann B, Vera-Cossio D. The unequal impact of the coronavirus pandemic: evidence from seventeen developing countries. PLoS One. 2020;15 doi: 10.1371/journal.pone.0239797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aguinis H. Guilford Press; New York, NY: 2004. Regression analysis for categorical moderators. [Google Scholar]
- 20.Holmes EA, O'Connor RC, Perry VH. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nguyen LH, Drew DA, Graham MS. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5:e475–e483. doi: 10.1016/S2468-2667(20)30164-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andrabi T, Daniels B, Das J. Human capital accumulation and disasters: evidence from the Pakistan earthquake of 2005. May 25, 2020. [DOI]
- 23.Parra-Saavedra M, Villa-Villa I, Pérez-Olivo P. Attitudes and collateral psychological effects of COVID-19 in pregnant women in Colombia. Int J Gynaecol Obstet. 2020;151:203–208. doi: 10.1002/ijgo.13348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ibáñez AM, Moya A. Vulnerability of victims of civil conflicts: empirical evidence for the displaced population in Colombia. World Dev. 2010;38:647–663. [Google Scholar]
- 25.Ridley M, Rao G, Schilbach F, Patel V. Poverty, depression, and anxiety: causal evidence and mechanisms. Science. 2020;370 doi: 10.1126/science.aay0214. [DOI] [PubMed] [Google Scholar]
- 26.Pellecchia U, Crestani R, Decroo T, Van den Bergh R, Al-Kourdi Y. Social consequences of Ebola containment measures in Liberia. PLoS One. 2015;10 doi: 10.1371/journal.pone.0143036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blendon RJ, Benson JM, DesRoches CM, Raleigh E, Taylor-Clark K. The public's response to severe acute respiratory syndrome in Toronto and the United States. Clin Infect Dis. 2004;38:925–931. doi: 10.1086/382355. [DOI] [PubMed] [Google Scholar]
- 28.Roberton T, Carter ED, Chou VB. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Health. 2020;8:e901–e908. doi: 10.1016/S2214-109X(20)30229-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Herba CM, Glover V, Ramchandani PG, Rondon MB. Maternal depression and mental health in early childhood: an examination of underlying mechanisms in low-income and middle-income countries. Lancet Psychiatry. 2016;3:983–992. doi: 10.1016/S2215-0366(16)30148-1. [DOI] [PubMed] [Google Scholar]
- 30.Shonkoff JP, Garner AS, Siegel BS. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129:e232–e246. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All anonymised individual participant data and a data dictionary will be made available immediately after the preprint of the Semillas de Apego impact evaluation is made public by mid-2021. Data will be available by the corresponding author upon a signed data access agreement.