Abstract
Wegener's granulomatosis or granulomatosis with polyangiitis (GPA) is multisystemic vasculitis. Kidney involvement in GPA often presents with rapidly progressive renal failure and requires urgent treatment. A 60-year-old female presented with prolonged history of fever, generalized weakness, decreased appetite, and weight loss over 4 months. Her renal function was normal; urine culture was sterile. On further evaluation, she was found to have large, hypodense solid lesion in mid pole of the right kidney on CECT. CT guided renal biopsy was done, which showed granulomatous interstitial nephritis with focal crescents. On further evaluation, she was found to have high titers of anti-MPO antibody. She was started on steroid and methotrexate with subsidence of fever. Follow-up after 12 months showed resolution of the lesion. GPA solely presenting as solid mass like lesion in the kidney is extremely rare presentation. Early diagnosis and prompt initiation of the treatment can prevent the progression of the disease.
Keywords: ANCA, GPA, granuloma, renal mass, vasculitis, Wegener's granulomatosis
Introduction
Wegener's granulomatosis or granulomatosis with polyangiitis (GPA) is multisystemic vasculitis. It most commonly involves the elderly population, although it can be seen in any age group.[1,2] The most common sites of involvement are the upper respiratory tract, lower respiratory tract, and kidneys. Clinically, it can have varied presentations ranging from nonspecific fever and weight loss to life-threatening pulmonary hemorrhage, ischemic colitis, and rapidly progressive renal failure. Herein is a case of a middle-aged female presented with constitutional symptoms along with a rare presentation of GPA as renal mass.
Case Summary
A 60-year-old female, with no known comorbidities came with complaints of intermittent fever, night sweats, nasal congestion, decreased appetite, and weight loss of 5-7 kgs over for 4 months. Her laboratory investigations were significant for mild anemia with persistent high ESR with normal renal function [Table 1]. On admission in another hospital 1 month back, USG abdomen showed hypoechoic lesion in the right kidney, and subsequently, CECT scan of the abdomen showed a large wedge-shaped solid, non-enhancing, hypodense area at the lower-mid pole of the right kidney suggestive of renal mass [Figure 1]. A PET CT showed avidity in the same region in the right kidney and in the nasal mucosa. USG-guided biopsy of the lesion in the kidney was done, which revealed granulomatous inflammation without any visible glomerular or vascular structure in the tissue. In view of strong suspicion of tubercular involvement of kidneys, urine was sent for PCR to isolate mycobacterium tuberculosis, which came negative. She was empirically started on antitubercular treatment (ATT). On admission at our hospital, her physical examination was significant for mild redness of the right eye and decreased hearing in the right ear. A detailed ear examination revealed right-sided sensorineural deafness that was attributed to the course of aminoglycoside she received in other hospital. Eye examination revealed mild episcleritis for which symptomatic treatment was provided. In view of previous inconclusive kidney biopsy report, a repeat CT-guided biopsy was done, which showed epithelioid granulomas along with focal crescents [Figure 2]. Immunofluorescence (IF) study revealed absence of glomerular immunoglobulins deposition. The nasal mucosa biopsy was done, which showed nonspecific inflammation. Further workup showed positive ANA by indirect IF. Anti-dsDNA by ELISA was negative, and p-ANCA by IF was positive with anti-MPO antibody showing high titer (>750 U/ml) [Table 1]. With the above-mentioned findings on physical examination, renal biopsy along with high titer of anti-MPO antibody, a diagnosis of GPA was made, ATT was stopped; she was started on prednisolone (60 mg/day) and methotrexate (15 mg/week). After the initiation of immunosuppression, she reported only one spike of fever in the next 7 days. She was discharged from the hospital with a tapering dose of steroid (2.5 mg/week till 5 mg/day is achieved) and methotrexate (20 mg/week). At 12 months of follow up, the patient was symptomatically better with no history of fever, normal renal function, improvement in her hearing. A repeat USG of kidneys showed a complete resolution of the lesion [Figure 3].
Table 1.
Laboratory parameters of the patient
| Investigations | 3 months back | 1 month back | On admission at our hospital | 6 months after admission | 12 months after admission |
|---|---|---|---|---|---|
| Hemoglobin, g/dL | 11.8 | 10.9 | 11.1 | 12.1 | 13.1 |
| TLC, cells/uL | 6350 | 9700 | 8200 | 7800 | 10000 |
| ESR, mm/h | 70 | 72 | 85 | 15 | 12 |
| Mantoux test | Negative | ||||
| Serum Creatinine (mg/dL) | 0.9 | 1.01 | 0.76 | 0.81 | 0.89 |
| Urine routine | Urine RBC 3-5/hpf | Urine RBC 5-10/hpf | Urine RBC 5-10/hpf | Urine RBC 0-3/hpf | Urine RBC 0-3/hpf |
| Urine C/S | Sterile | Sterile | Sterile | ||
| Spot urine PC Ratio | 0.04 g/g | 0.03 g/g | 0.07g/g | ||
| IgG4, mg/dL (5-200) | 150 | 122 | |||
| ACE levels, mcg/L (<40) | 25 | ||||
| ANA, IF | positive 3+ (centromeric) | ||||
| ANTI-dsDNA | Negative | ||||
| C-ANCA (IF) | Negative | ||||
| P-ANCA (IF) | Positive | ||||
| Anti-MPO antibody (ELISA) | >750 U/L | 112 U/L | |||
| Anti-PR3 antibody (ELISA) | Negative |
TLC- Total Leucocyte Count, Urine C/S- urine culture and sensitivity, Urine P:C ratio- urine Protein Creatinine Ratio, IF-Immunofluorescence
Figure 1.
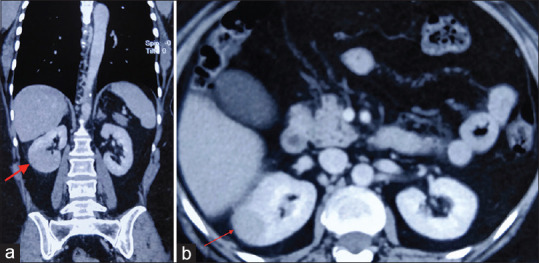
CECT abdomen. (a) Coronal section showing mass in the mid-pole of the right kidney (red arrow). (b) Axial section showing the right bulky kidney with 5.7 × 2.9 cm wedge shaped hypodense, solid area in the mid-lower pole (red arrow)
Figure 2.
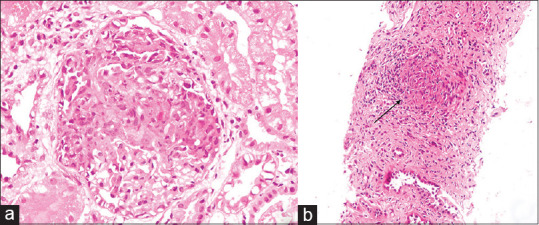
Renal biopsy. (a) A glomerulus showing circumferential cellular crescent (H&E, 400 × original magnification). (b) Epithelioid cell granuloma (black arrow) surrounded by inflammatory cells (H&E, 100 × original magnification)
Figure 3.
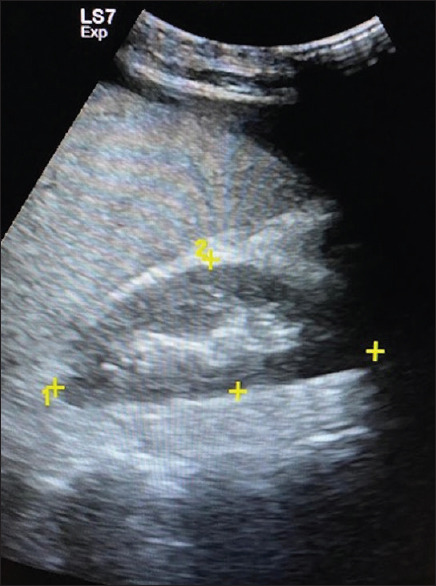
Ultrasound abdomen – showing complete resolution of the lesion in the right kidney after 12 months of treatment
Discussion
GPA is a multisystemic disorder involving almost all organs of the body; nevertheless, it can present as a disease limited solely to the kidneys and is termed as renal limited ANCA-vasculitis. Kidney involvement in the disease is typically severe, with characteristics of rapidly progressive renal disease. However, rarely GPA can present as renal infarction, papillary necrosis, or hydronephrosis due to ureteral stenosis.[3]
This patient presented with a prolonged duration of fever without any localizing signs or symptoms, which delayed her diagnosis. Her incidental findings of renal lesion raised the suspicion of a renal mass. After the biopsy of the lesion, which yielded granulomatous interstitial nephritis, the etiology was unclear. The differential diagnosis of granulomatous kidney disease is broad, and the most common causes are sarcoidosis, drugs including antibiotics, diuretics, and infection, including tuberculosis.[4] Considering her symptoms of prolonged fever, weight loss along with granuloma in the kidney, TB was a strong possibility which despite negative tissue stain, Mantoux test and negative urine for AFB, and GeneXpert was considered and she was treated for the same, however with little success.
GPA has been reported to present as solitary or multiple, bilateral, solid lesions in the kidney mimicking renal mass with or without other systemic involvement,[5,6,7,8,19] although it rarely has been reported to present solely as a renal mass without any other systemic involvement.[12,14,16,19] In a similar case report by Nelson et al., they reported a case of a 66-year-old male with 2 months history of fever.[19] He was incidentally found to have multiple solid renal lesions, which on histopathological examination revealed multiple noncaseating granulomas. There was no evidence of disease activity in other organs.
The prognosis of the kidney is good as compared to the crescentic vasculitis presentation with the treatment. In 15 cases reported so far, one case had progressed to ESRD as he refused the treatment, one case was lost to follow up after the initial presentation and returned with advanced renal failure, and one case expired due to massive pulmonary hemorrhage before starting the treatment.[14,18,11] Even though, in cases where only the kidney is involved initially, without immunosuppression disease may progress and can involve other systems. In a report by smith et al., patient underwent total nephrectomy in view of renal mass, which was consistent with granulomas without any evidence of vasculitis.[13] However, she relapsed with fever and blocked nose, which immediately responded to immunosuppression. Most case reports have used a combination of steroid and cyclophosphamide or methotrexate. Few studies have resorted to partial nephrectomy, although it was done in suspicion of a tumor, later started on treatment once the diagnosis was made on histopathology. The treatment of choice in this rare presentation is difficult to ascertain, but we suggest that the addition of cyclophosphamide or methotrexate with steroid is ideal than the only steroid as it was seen in the case reported by Nelson et al., where the patient had relapsed initially when discharged on steroids and later tapered off.[19] We preferred methotrexate over cyclophosphamide in the present case, as it was a non-organ threatening presentation.
We suggest that GPA should be among the working diagnosis of clinician while evaluating the renal mass-like lesion or granulomatous inflammation, where the cause is not evident. Extrarenal symptoms should be looked for subtle signs as in this case since renal symptoms and renal function with urine examination may be normal, as seen in most of the case reports. Noninvasive tests of ANCA vasculitis should be included in work up. Renal biopsy of suspected lesions should be done before any radical surgical procedure. It is essential to recognize this rare presentation of the GPA as it responds completely to the treatment with an excellent prognosis.
In conclusion, GPA as renal mass is rare but known presentation of this disease. Its recognition in early stage and prompt treatment can prevent progression of the disease.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Jennette JC, Falk RJ. Small-vessel vasculitis. N Engl J Med. 1997;337:1512–23. doi: 10.1056/NEJM199711203372106. [DOI] [PubMed] [Google Scholar]
- 2.Seo P, Stone JH. The antineutrophil cytoplasmic antibody-associated vasculitides. Am J Med. 2004;117:39–50. doi: 10.1016/j.amjmed.2004.02.030. [DOI] [PubMed] [Google Scholar]
- 3.Rich LM, Piering WF. Ureteral stenosis due to recurrent Wegener's granulomatosis after kidney transplantation. J Am Soc Nephrol. 1994;4:1516–21. doi: 10.1681/ASN.V481516. [DOI] [PubMed] [Google Scholar]
- 4.Shah S, Carter-Monroe N, Atta MG. Granulomatous interstitial nephritis. Clin Kidney J. 2015;8:516–23. doi: 10.1093/ckj/sfv053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maguire R, Fauci AS, Doppman JL, Wolff SM. Unusual radiographic features of Wegener's granulomatosis. AJR Am J Roentgenol. 1978;130:233–8. doi: 10.2214/ajr.130.2.233. [DOI] [PubMed] [Google Scholar]
- 6.Schapira HE, Kapner J, Szporn AH. Wegener granulomatosis presenting as renal mass. Urology. 1986;28:307–9. doi: 10.1016/0090-4295(86)90012-9. [DOI] [PubMed] [Google Scholar]
- 7.Krambeck AE, Miller DV, Blute ML. Wegener's granulomatosis presenting as renal mass: A case for nephron-sparing surgery. Urology. 2005;65:798. doi: 10.1016/j.urology.2004.10.018. [DOI] [PubMed] [Google Scholar]
- 8.Negi A, Camilleri JP, Matthews PN, Crane MD. Wegener's granulomatosis presenting as a disappearing renal mass. Rheumatology. 2006;45:1554. doi: 10.1093/rheumatology/kel219. [DOI] [PubMed] [Google Scholar]
- 9.Roussou M, Dimopoulos SK, Dimopoulos MA, Anastasiou-Nana MI. Anastasiou-Nana MI. Wegener's granulomatosis presenting as a renal mass. Urology. 2008;71:547. doi: 10.1016/j.urology.2007.11.046. e1-2. [DOI] [PubMed] [Google Scholar]
- 10.Frigui M, Ben HM, Kechaou M, Jlidi R, Bahloul Z. Wegener's granulomatosis presenting as multiple bilateral renal masses: Case report and literature review. Rheumatol Int. 2009;29:679–83. doi: 10.1007/s00296-008-0715-4. [DOI] [PubMed] [Google Scholar]
- 11.Mohammadi Sichani M, Hadi M, Talebi A, Khalighinejad P. Renal solid mass as a rare presentation of Wagener's granulomatosis: A case report. Case Rep Urol. 2012;2012:1–3. doi: 10.1155/2012/793014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schydlowsky P, Rosenkilde P, Skriver E, Helin P, Brændstrup O. Wegeners granulomatosis presenting with a tumor-like lesion in the Kidney. Scand J Rheumatol. 1992;21:204–5. doi: 10.3109/03009749209099223. [DOI] [PubMed] [Google Scholar]
- 13.Smith DJ, Milroy CM, Chapple CR. An unusual renal mass:. Wegener's granulomatosis? Br J Urol. 1993;72:980–1. doi: 10.1111/j.1464-410x.1993.tb16319.x. [DOI] [PubMed] [Google Scholar]
- 14.Boubenider SA, Akhtar M, Nyman R. Wegener's granulomatosis limited to the kidney as a masslike lesion. Nephron. 1994;68:500–4. doi: 10.1159/000188314. [DOI] [PubMed] [Google Scholar]
- 15.Fairbanks KD, Hellmann DB, Fishman EK, Ali SZ, Stone JH. Wegener's granulomatosis presenting as a renal mass. Am J Roentgenol. 2000;174:1597–8. doi: 10.2214/ajr.174.6.1741597. [DOI] [PubMed] [Google Scholar]
- 16.Carazo ER, Benitez AM, Milena GL, Espigares JR, León L, Marquez B. Multiple renal masses as initial manifestation of Wegener's granulomatosis. Am J Roentgenol. 2001;176:116–8. doi: 10.2214/ajr.176.1.1760116. [DOI] [PubMed] [Google Scholar]
- 17.Verswijvel G, Eerens I, Messiaen T, Oyen R. Granulomatous renal pseudotumor in Wegener's granulomatosis: Imaging findings in one case. Eur Radiol. 2000;10:1265–7. doi: 10.1007/s003300000344. [DOI] [PubMed] [Google Scholar]
- 18.Kapoor A, Balfour-Dorsey RA, George DL. Wegener's granulomatosis presenting as multiple kidney masses. Am J Med. 2002;112:82–3. doi: 10.1016/s0002-9343(01)00946-9. [DOI] [PubMed] [Google Scholar]
- 19.Leung N, Ytterberg SR, Blute ML, Lager DJ, Specks U, Fervenza FC. Wegener's granulomatosis presenting as multiple bilateral renal masses. Nephrol Dial Transplant. 2004;19:984–7. doi: 10.1093/ndt/gfh058. [DOI] [PubMed] [Google Scholar]


