Abstract
Background and Objectives:
African-American family caregivers may have insufficient knowledge to make informed end-of-life (EOL) decisions for relatives with dementias. Advance Care Treatment Plan (ACT-Plan) is a community-based education intervention to enhance knowledge of dementia and associated EOL medical treatments, self-efficacy, intentions, and behavior (written EOL care plan). This study evaluated efficacy of the intervention compared to attention control.
Research Design and Methods:
In a theoretically based, 2-group, cluster randomized controlled trial, 4 similar Midwestern urban megachurches were randomized to experimental or control conditions. Each church recruited African-American caregivers, enrolling concurrent waves of 5 to 9 participants in 4 weekly 1-hour sessions (358 total: ACT-Plan n = 173, control n = 185). Dementia, cardiopulmonary resuscitation (CPR), mechanical ventilation (MV), and tube feeding (TF) treatments were discussed in ACT-Plan classes. Participants completed assessments before the initial class, after the final class (week 4), and at week 20. Repeated measures models were used to test the intervention effect on changes in outcomes across time, adjusting for covariates as needed.
Results:
Knowledge of CPR, MV, TF, and self-efficacy to make EOL treatment decisions increased significantly more in the ACT-Plan group at weeks 4 and 20. Knowledge of dementia also increased more in the ACT-Plan group at both points, reaching statistical significance only at week 20. Intentions to make EOL treatment decisions and actually an advance care plan were similar between treatment arms.
Discussion and Implications:
Findings demonstrate promise for ACT-Plan to increase informed EOL treatment decisions for African American caregivers of individuals with dementias.
Keywords: African Americans, dementia, Alzheimer disease, end-of-life (EOL) treatments, advance directives, palliative care
Introduction
African Americans are 3 times more likely than white Americans to be diagnosed with dementia, yet they receive less dementia care and education about making informed end-of-life (EOL) treatment decisions.1–4 Most patients rely on family caregivers to make treatment decisions, but informed advance care planning improves satisfaction with care, decreases use of life-prolonging treatments, and reduces health-care costs.2,5 Fewer than 13% of African Americans complete written advance directives, as opposed to 30% of white Americans.6–9
Our community-based EOL education intervention, the Advance Care Treatment Plan (ACT-Plan), promoted dialogue among family caregivers, other relatives, and dementia patients.10–13 Family caregivers were receptive to learning about advance care planning for cognitively impaired relatives and expressed a need for more educational instructions on cardiopulmonary resuscitation (CPR), mechanical ventilation (MV), and tube feeding (TF).12,13
The specific aim of this study was to compare experimental (ACT-Plan) and control groups for various effects on caregivers’ (a) knowledge of dementia, CPR, MV, and TF; (b) self-efficacy for CPR, MV, and TF treatment decisions; (c) intention to write an EOL care plan; and (d) behavior (written EOL care plan). We hypothesized that on posttests immediately after the 4-week intervention and 4 months later (week 20), the experimental group compared to the attention control group would demonstrate more knowledge, self-efficacy, intentions, and behaviors (written EOL care plans).
Methods
The Institutional Review Board of the University of Illinois at Chicago approved the study protocol.
Theoretical Framework
The Theory of Reasoned Action14 guided selection of the intervention outcomes: knowledge (dementia, CPR, MV, TF), self-efficacy, intention to write an EOL care plan, and behavior (written EOL care plan). According to the TRA, intention to perform a certain behavior predicts and precedes the actual behavior.
Kolb’s Experiential Learning Theory15 was used to design interactive educational techniques and specific learning activities through a structured cyclical learning format,12,13 using culturally focused teaching tools. Education interventions constructed with a theoretical model and within a cultural context are more likely to succeed.16,17 Our culturally tailored endeavors included conducting the intervention at African American community churches. Course content involved storytelling of participants’ unique lived experiences. African American actors were used for case study videotapes, handouts, and educational materials.
Design
We used a cluster randomized controlled trial to test efficacy of the ACT-Plan intervention in a 2-group, pre/posttest design. Four sites were randomized to 2 conditions (intervention and attention control) and stratified by size (2 large, 2 small). A sample size of 305 caregivers was determined a priori to provide 80% power based on our prior research.12
Setting and Sample
Settings were 4 large African American Protestant churches in metropolitan Chicago, Illinois. Three of the 4 are megachurches defined, in this study, as any religious institution that reports memberships greater than 2000. Range of congregants was from 1400 to 7000 people in the 4 churches. Although similar in operation, programs, geography, and low turnover rates (less than 3%), the churches were located in distinct communities. The median health-care ministries were for approximately 900 members, including family caregivers for loved ones with memory loss. All church pastors reported similar beliefs that encouraged parishioners to make the best EOL health-care treatments for loved ones within the context of their families and own religious beliefs.
From the 4 churches, 358 eligible participants consented, completed baseline measurements, and enrolled. Of these, 173 were in the experimental (ACT-Plan) group and 185 control group. Of those, 312 completed the 4-week training sessions and immediate posttest; 264 completed the 4-month posttest (consort Figure 1). All caregivers were African Americans, relatives, or surrogate relatives of a care recipient; knowledgeable about the care recipient’s recent and past medical history; and had no EOL care plan for care recipients or themselves. Care recipients were African Americans with moderate-to-severe dementia, without decisional capacity, and not in hospice care at study enrollment.
Figure 1.
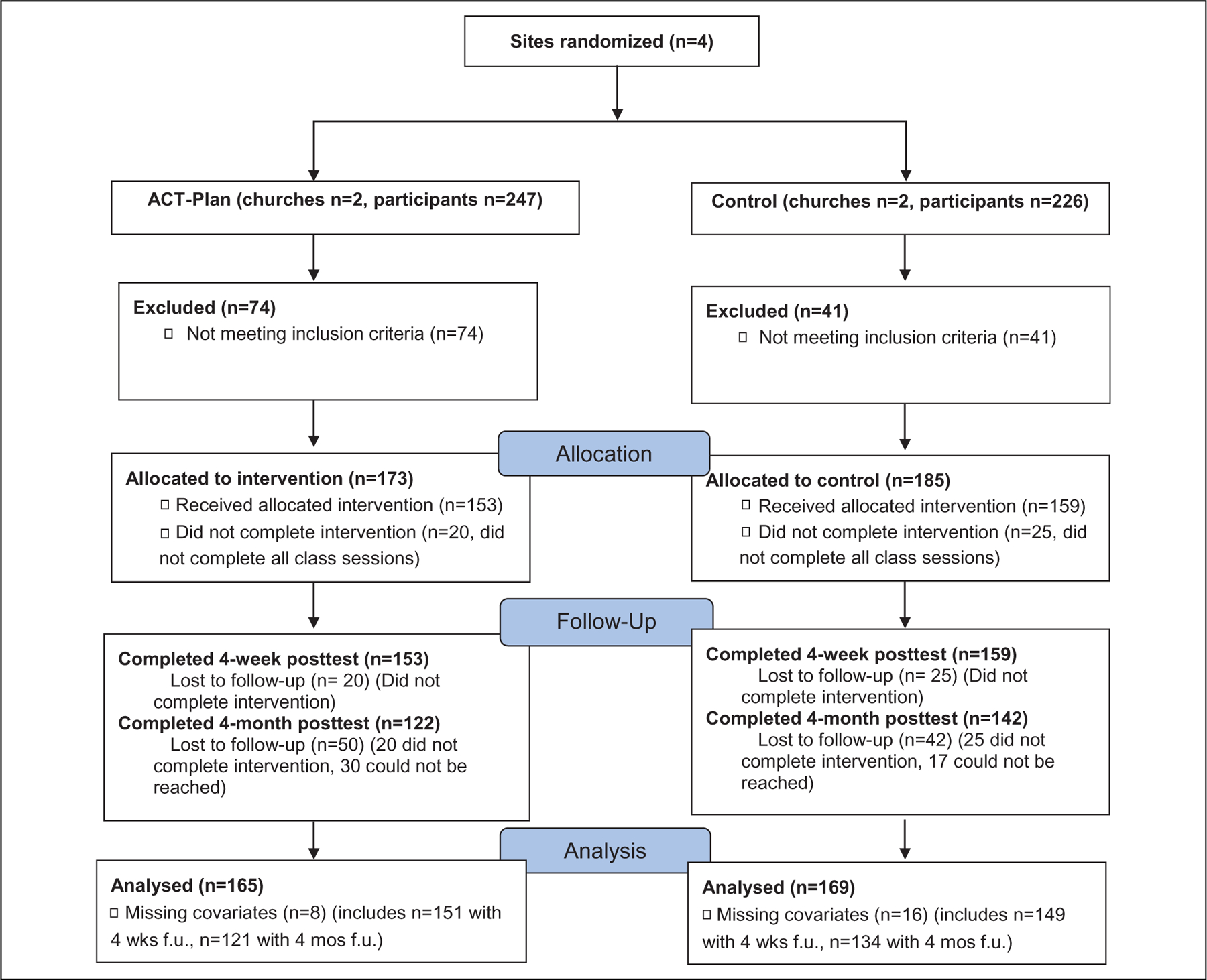
CONSORT flow diagram: Chicago IL (2014–2017). © 2017 G. Bonner, Reprinted with permission. All rights reserved.
Procedures
Recruitment.
Caregivers were recruited concurrently across sites, with multiple waves of the 4-week class for experimental and control conditions. Our primary source of recruitment was referral by church pastors and ministry leaders, to address sociohistorical barriers such as mistrust in health-care providers and researchers.18 Other recruitment methods include solicitation through church bulletins and videotaped announcements of the study at kiosks in church lobbies. Research assistants (RAs) solicited prospective participants at health ministry monthly meetings, scheduled health fairs, and manned booths in church lobbies. Potential participants who responded received a brief introduction and overview of the study, including eligibility requirements. Names and telephone numbers were retrieved for screening interviews.
Two screening questionnaires were administered to determine eligibility (13-item Advance Directive and 15-item Functional Assessment Staging scale). Caregivers who did not meet eligibility criteria were not solicited for participation. Monthly presentations by RAs at church meetings were conducted as needed until all participants were recruited. All prospective participants received an official attendance letter and phone call within 2 weeks of the scheduled first session that included the schedule for their pretest, 4 weekly sessions (either ACT-Plan or attention-control), and posttest. Consenting participants were assigned by convenience to groups at each ACT-Plan or attention-control site. They signed the Institutional Review Board–approved consent form and completed pretest measures immediately preceding the first-class session. Each 4-week class (1 hour per class session) was held onsite and typically contained 5 to 8 participants, resulting in a sample size of 358.
Intervention
Classes were taught by 2 master’s-prepared advanced practice public health professionals. Different African American staff guided the experimental (ACT-Plan) and attention control activities. Caregivers were taught about disease trajectory of dementias, as well as risk/benefits of CPR, MV, and TF. Subjective norms were addressed through homework assignments to discuss disease trajectories and the 3 treatment options with family members and significant others (eg, clergy, health-care providers). Participants shared families’ response in subsequent class sessions.
The teaching-around-the-circle format was predicated on culturally sensitive application of the 4 cyclical learning activities of Kolb’s model: concrete experience, perceptions using reflective observation, cognition through abstract conceptualization, and behaviors using active experimentation. For example, in the session on TF, as concrete experience an audiovisual presentation (DVD) is shown that includes a discussion between a physician and a caregiving daughter on recommendations of TF for a mother severely disabled with dementia, soliciting advice from study participants. In reflective observation, class participants discuss answers based on life experiences. Abstract conceptualization includes rationale for and against the TF treatment and advance care planning. In active experimentation, class participants restate and discuss their views on TF based on evidence presented in abstract conceptualization. The 4 phases are repeated in each of the 3 subsequent class sessions (Table 1).
Table 1.
ACT-Plan Implementation of Kolb Experiential Learning Theory.
| Session | Learning Concept | ACT-Plan Session Content and Methods |
|---|---|---|
| 1 | Concrete experience | DVD video of case study. Patient diagnosed with dementia (Alzheimer) admitted to hospital with pneumonia. Physician asks caregiver to make decision for life support (TF). What should caregiver do? |
| Reflective observation | Each participant reflects on thoughts about vignette including dementia, TF, physicians’ motives for suggesting life support, trust/mistrust of health-care system and preferred TF decision for own relative. | |
| Abstract conceptualization | Facilitator presents accurate information on topics including family caregiver’s legal rights as health-care proxy, dementias, risk/benefit of TF, EOL care planning via case study vignette. | |
| Active experimentation | Practice application of problem (action plan). Using information just received, share actual personal experience about hospitalized loved one’s dehydration, inability to swallow, experiences with physicians about TF, hydration and nutrition. Take home assignment: Discuss with family/important others TF decisions made in class session. Return to next class with outcomes from family discussion. |
|
| 2 | Concrete experience | Discuss take-home assignment. DVD case study continued. Patient’s condition worsen, physician suggests intubation for aspiration pneumonia. What should caregiver do? |
| Reflective observation | Caregivers reflect on actions in video and personal feelings about MV. Discuss preferred MV decision for own relative. | |
| Abstract conceptualization | Facilitator continues discussions on accurate information on the dementias, EOL care planning introduces risk/benefit of MV. | |
| Active experimentation | Practice application of problem (Action plan). Using knowledge gained to make MV decisions, discuss own situation with class. Take-home assignment: Discuss TF and MV with care recipient’s physician. Return next session with outcomes from discussions. |
|
| 3 | Concrete experience | Discuss take-home assignment DVD video case study continued. Patient’s condition continues to deteriorate may need CPR intervention. What should caregiver do? |
| Reflective observation | Reflections on what caregiver in video should do and own preferences for CPR if confronted with similar situation. | |
| Abstract conceptualization | Content topic continues with the dementias, risk/benefits of CPR at EOL, and introduction of religious beliefs as related to decisions. Write care plan. |
|
| Active experimentation | Practice application (Actionplan). Discuss own situation in relationship to CPR and religious beliefs. Take-home assignment: Discuss TF, MV, and CPR with religious leader (church pastor). Return next session to discuss outcomes. |
|
| 4 | Concrete experience | DVD video case study continued with caregiver confronted in ER by physician who insists on ordering TF treatments against caregiver’s wishes. What should caregiver do? |
| Reflective observation and Abstract conceptualization | Caregiver reflects on knowledge gained in class and established decisions against TF for relative. | |
| Active experimentation | Practice application (Action plan). Discuss caregiver’s options and treatment decisions based on informed choices and recipient’s verbal or written preferences. Discuss strategies to use when confronted in ER by health care professions in hospital settings. |
Abbreviations: ACP-Plan, Advance Care Treatment Plan; CPR, cardiopulmonary resuscitation; EOL, end of life; MV, mechanical ventilation; TF, tube feeding.
Participants in the attention-control condition received interactive discussions on health promotion topics, including hypertension, diabetes mellitus, nutrition, and exercise, because family caregivers are at risk of developing chronic diseases due to stress associated with caregiving.19 The 4 learning elements of Kolb’s model were also applied to each topic for controls to engage participants in classes and homework assignments, similar to ACT-Plan. After completing the second posttest at week 20, attention-control group participants were offered discussions on advance care planning.
The number of sessions, frequency, education content, and intervention model were derived from our 6 community-based preliminary studies.10,11 Separate African American health-care facilitators with master’s degrees trained by the PI using standard training protocol conducted the ACT-Plan and control group classes. Trained RAs, assigned for the study duration to the control or experimental groups, monitored intervention delivery fidelity with checklists at all classes. All sessions were 60 minutes, with sessions 1 and 4 having an extra 30 minutes for pre-/posttest.
A second face-to-face posttest was completed at week 20. Study instruments were distributed by trained RA interviewers who answered questions and observed for literacy. All instruments were collected, counted, and checked immediately for missing items. Participants were asked to complete any missed items. An honorarium of $50 was given to each participant; $25 at week 4 posttest and week 20 posttest.
Booster follow-ups.
Both intervention and control groups received refresher telephone boosters approximately 2 weeks before the week 20 posttest. Refresher content was based on ACT-Plan knowledge deficits on dementia, CPR, MV, and TF or attention control deficits such as stress reduction, exercise, and diabetes. Content was delivered by separate advanced care specialists on yes/no knowledge questionnaire items taught to family caregivers at week 4 posttest. Answers missed were immediately corrected.
Measures
Measurements addressed knowledge, self-efficacy, intention to write a care plan, and behavior (written care plans). Caregivers reported basic demographic information for themselves and the care recipient, as well as caregiver burden, religious beliefs, and their role as a caregiver. Caregivers also provided clinical details related to the care recipient’s dementia.
Outcome variables.
Knowledge of dementia, CPR, MV, TF, and health promotion was assessed by correct responses on a questionnaires with 6 to 17 dichotomous “true/false” items.12,20 Self-efficacy was assessed with 12 five-point Likert item scales (1 = not at all confident to 5 = extremely confident), a modified version of the Confidence in Treatment Decisions Made questionnaire (Cronbach α: .89–.96).10,12 Intention to make a Care Plan with CPR, MV, and TF was assessed using the dichotomous (yes/no) 3-item Treatment Decisions Questionnaire. Written care plan behavior was measured in a similar manner.
Covariates.
Caregiver characteristics included gender, age, education, income, years of caregiving, relationship to care recipient, caregiver burden, and religiosity. Care recipient variables included age, income, years with dementia, and severity of disability. Caregiver burden was measured using the 12-item Likert Zarit Caregiver Burden Interview Short Form Scale. Higher scores indicate increased stress. Cronbach a’s are .88 and .78 for personal and role strain, respectively.21 Religious beliefs were measured using the 12-item Religiosity Scale.10,12 Its Cronbach α is .81.22 This 3-dimensional Likert scale measures official membership, formal participation, and religious beliefs.
Statistical Analysis
All data were analyzed using SAS software (SAS, Cary, North Carolina), with P < .05 considered statistically significant. Separate models were conducted to determine treatment arm differences for each of 8 outcomes: 5 knowledge scales (dementia, CPR, MV, TF, and health promotion), self-efficacy, intention to write a care plan, and behavior (writing a care plan).
Mixed effects, multiple linear, or logistic regression models were used for continuous and binary outcomes, respectively, with random intercepts to account for repeated measurements of participants across time. These work best when outcomes are missing at random, a plausible assumption for this study. Having only 2 churches per condition precluded estimation of variance due to clusters within a condition. Instead, variation across the 4 churches was estimated as a fixed effect using 3 contrasts: variation within the control condition (difference score between 2 sites), variation within the intervention condition (difference score between 2 sites), and the intervention effect (difference between the average of the 2 intervention sites and the 2 control sites).
Potentially important covariates were examined for imbalance between treatment arms using χ2 tests and t tests. Covariates that differed significantly between arms were included in regression models as additional independent variables. Mixed models were used to evaluate the intervention effects and estimate mean outcomes across time for descriptive purposes, while adjusting for relevant covariates.
The intervention effect was evaluated for each outcome by comparing change between treatment arms, adjusted for relevant covariates. For continuous outcomes, variation due to the 3 time points was estimated with 2 contrasts: change from pretest to week 4 and from pretest to week 20. The intervention effect was evaluated at weeks 4 and 20 as the interaction between the intervention effect and the respective change score. The binary outcomes indicating intention to write a care plan and behavior (written care plan) were not measured at pretest; “no” was assumed for all participants. Thus, the percentage responding “yes” at follow-up was interpreted as change from pretest. The intervention effect for binary outcomes was evaluated by comparing outcomes at weeks 4 and 20, combining the 2 waves using logistic regression with random intercepts. Evaluation of multiple end points increases the probability of type I error. Application of the conservative Bonferroni correction to adjust for testing 8 outcomes at 2 time points would involve using α = .05/16 = .003 as a significance criterion to ensure a type I error rate of α = .05. We reported results using this more conservative criterion.
Results
Demographics
Most caregiver participants and care recipients were women (Tables 2 and 3). Forty-three percent of care recipients in the ACT-Plan group and 51% of care recipients in the control group had dementia for less than 4 years. However, most caregivers did not know the care recipients’ type of dementia diagnoses (not reported in Table 3). Advance Care Treatment Plan participants had a slightly higher average level of caregiver burden, but both groups’ means were ≥17, the threshold indicating a high level of burden. Religiosity was similar for each group and could be interpreted as between fairly and very religious on the 1- to 4-point scale. Statistical comparisons between ACT-Plan and control sites suggested differences in caregivers’ occupation type and education level, caregivers’ relationship with care recipients, and severity of care recipients’ dementia. These 4 variables were included in multiple regression models evaluating outcomes. Statistical comparisons showed great diversity of characteristics between the 2 control sites but few between the 2 ACT-Plan sites.
Table 2.
Demographics and Background Characteristics of Caregivers by Church Site.
| ACT-Plan Intervention Sites, n = 173 |
Control Sites, n = 185 |
ACT-Plan vs Control |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Site 1, n = 76 |
Site 2, n = 97 |
Site 1 vs 2 | Site 3, n = 124 |
Site 4, n = 61 |
Site 3 vs 4 | ||||||
| % or mean | % or mean | % or mean | % or mean | P Value | |||||||
| Caregiver Characteristics | N | (SD) | n | (SD) | P Value | n | (SD) | n | (SD) | P Value | |
| Gender | |||||||||||
| Female | 60 | 79.0% | 81 | 83.5% | .4435 | 104 | 84.5% | 50 | 84.7% | .9731 | .4341 |
| Male | 16 | 21.0% | 16 | 16.5% | 19 | 15.5% | 9 | 15.3% | |||
| Age | |||||||||||
| Mean (SD) | 69 | 54.7 (9.2) | 87 | 55.5 (13.2) | .6452 | 112 | 57.3 (11.5) | 55 | 51.8 (15.2) | .0201 | .8077 |
| Education | |||||||||||
| High school or less | 13 | 17.1% | 15 | 15.6% | .7940 | 37 | 30.3% | 21 | 35.6% | .4767 | .0006 |
| Some college or more | 63 | 82.9% | 81 | 84.4% | 85 | 69.7% | 38 | 64.4% | |||
| Income | |||||||||||
| Less than $25 000 | 21 | 32.3% | 28 | 32.9% | .9347 | 38 | 36.5% | 27 | 52.9% | .0518 | .0944 |
| $25 000 or more | 44 | 67.7% | 57 | 67.1% | 66 | 63.5% | 24 | 47.1% | |||
| Occupation | |||||||||||
| Skilled craft or trade | 8 | 10.5% | 10 | 10.4% | .8605 | 6 | 5.0% | 5 | 8.5% | .0779 | .0084 |
| Managerial or Administrative | 10 | 13.1% | 17 | 17.7% | 5 | 4.2% | 9 | 15.3% | |||
| Professional | 17 | 22.4% | 24 | 25.0% | 21 | 17.5% | 10 | 16.9% | |||
| Retired | 22 | 29.0% | 22 | 22.9% | 45 | 37.5% | 16 | 27.1% | |||
| Other | 19 | 25.0% | 23 | 24.0% | 43 | 35.8% | 19 | 32.2% | |||
| Years as caregiver | |||||||||||
| 1–3 years | 51 | 68.9% | 60 | 64.5% | .3154 | 74 | 61.7% | 32 | 58.2% | .0313 | .2473 |
| 4–6 years | 11 | 14.9% | 22 | 23.7% | 17 | 14.2% | 16 | 29.1% | |||
| 7 or more years | 12 | 16.2% | 11 | 11.8% | 29 | 24.2% | 7 | 12.7% | |||
| Caregiver burden | |||||||||||
| Mean (SD) | 76 | 18.0 (8.4) | 89 | 18.8 (9.3) | .5524 | 119 | 17.0 (8.7) | 58 | 16.1 (9.3) | .4991 | .0795 |
| Religiosity | |||||||||||
| Mean (SD) | 76 | 33. (4.6) | 89 | 33.7 (4.6) | .9330 | 116 | 33.6 (4.6) | 58 | 32.2 (5.6) | .0815 | .3143 |
Abbreviations: ACP-Plan, Advance Care Treatment Plan; SD, standard deviation.
Table 3.
Demographics and Background Characteristics of Caregiver Recipients by Church Site.
| ACT-Plan Intervention Sites, n = 173 |
Control Sites, n = 185 |
ACT-Plan vs Control |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Site 1, n = 76 |
Site 2, n = 97 |
Site 1 vs 2 | Site 3, n = 124 |
Site 4, n = 61 |
Site 3 vs 4 | ||||||
| % or mean | % or mean | % or mean | % or mean | P Value | |||||||
| Care Recipient Characteristics | N | (SD) | n | (SD) | P Value | N | (SD) | n | (SD) | P Value | |
| Gender | |||||||||||
| Female | 55 | 72.4% | 74 | 76.3% | .5568 | 92 | 75.4% | 44 | 74.6% | .9032 | .9014 |
| Male | 21 | 27.3% | 23 | 23.7% | 30 | 24.6% | 15 | 25.4% | |||
| Age | |||||||||||
| Mean (SD) | 75 | 79.3 (10.5) | 97 | 78.8 (10.7) | .7463 | 120 | 78.1 (10.9) | 58 | 74.3 (14.8) | .0828 | .0857 |
| Education | |||||||||||
| High school or less | 53 | 69.7% | 56 | 58.3% | .1232 | 78 | 66.1% | 43 | 74.1% | .2796 | .2894 |
| Some college or more | 23 | 30.3% | 40 | 41.7% | 40 | 33.9% | 15 | 25.9% | |||
| Income | |||||||||||
| Less than $25 000 | 39 | 75.0% | 39 | 54.9% | .0224 | 47 | 63.5% | 25 | 65.8% | .8119 | .8896 |
| $25 000 or more | 13 | 25.0% | 32 | 45.1% | 27 | 36.5% | 13 | 34.2% | |||
| Relationship to caregiver | |||||||||||
| Parent | 57 | 77.0% | 59 | 64.1% | .2942 | 61 | 52.1% | 30 | 51.7% | .0391 | .0070 |
| Spouse/partner | 4 | 5.4% | 4 | 4.3% | 16 | 13.7% | 5 | 8.6% | |||
| Grandparent | 3 | 4.1% | 3 | 3.3% | 3 | 2.6% | 5 | 8.6% | |||
| Sibling | 3 | 4.1% | 8 | 8.7% | 7 | 6.0% | 3 | 5.2% | |||
| Aunt/uncle | 4 | 5.4% | 14 | 15.2% | 13 | 11.1% | 13 | 22.4% | |||
| Other relation | 3 | 4.1% | 4 | 4.3% | 17 | 14.5% | 2 | 3.4% | |||
| Caregiver’s parent? | |||||||||||
| Yes | 57 | 77.0% | 59 | 64.1% | .0718 | 61 | 52.1% | 30 | 51.7% | .9590 | .0007 |
| No | 17 | 23.0% | 33 | 35.9% | 56 | 47.9% | 28 | 48.3% | |||
| Years with dementia | |||||||||||
| Less than 4 years | 32 | 43.8% | 41 | 43.2% | .2290 | 63 | 53.4% | 27 | 46.5% | .3279 | .3101 |
| 4–6 years | 35 | 48.0% | 38 | 40.0% | 42 | 35.6% | 27 | 46.5% | |||
| 7 or more years | 6 | 8.2% | 16 | 16.8% | 13 | 11.0% | 4 | 6.9% | |||
| Missing | 3 | 3.9% | 2 | 2.1% | 6 | 4.8% | 3 | 4.9% | |||
| Severity of disability | |||||||||||
| Severely disabled | 4 | 5.3% | 4 | 4.1% | .8873 | 13 | 10.9% | 7 | 11.9% | .0033 | .0088 |
| Moderately disabled | 35 | 46.0% | 42 | 43.3% | 35 | 29.4% | 17 | 28.8% | |||
| Mildly disabled | 24 | 31.6% | 36 | 37.1% | 56 | 47.1% | 15 | 25.4% | |||
| Not at all | 13 | 17.1% | 15 | 15.5% | 15 | 12.6% | 20 | 33.9% | |||
Abbreviations: ACP-Plan, Advance Care Treatment Plan; SD, standard deviation.
Treatment Completion and Week 20 Posttest
Findings indicated high recruitment (n = 358) and retention: 87% at week 4 and 74% at week 20. Posttest questionnaires were administered to participants who completed all 4 weekly classes. Participants who failed to complete the 4 classes had missing outcomes at week 20. Both study arms had similar completion rates for the 4 classes and week 4 posttest (ACT-Plan: 88.4%; control: 85.9%; χ2(1) = 0.5, P = .481) and week 20 posttest (ACT-Plan: 70.5%; control: 76.8%; χ2(1) = 1.8, P = .180).
Intervention Outcomes
For each outcome, a mixed-effects regression model was used to estimate adjusted means (Figure 2) and evaluate the intervention effect at weeks 4 and 20 (Table 4). Continuous outcomes were tested, comparing change scores from pretest, and binary outcomes were tested, comparing proportions between ACT-Plan sites and control sites at weeks 4 and 20.
Figure 2.
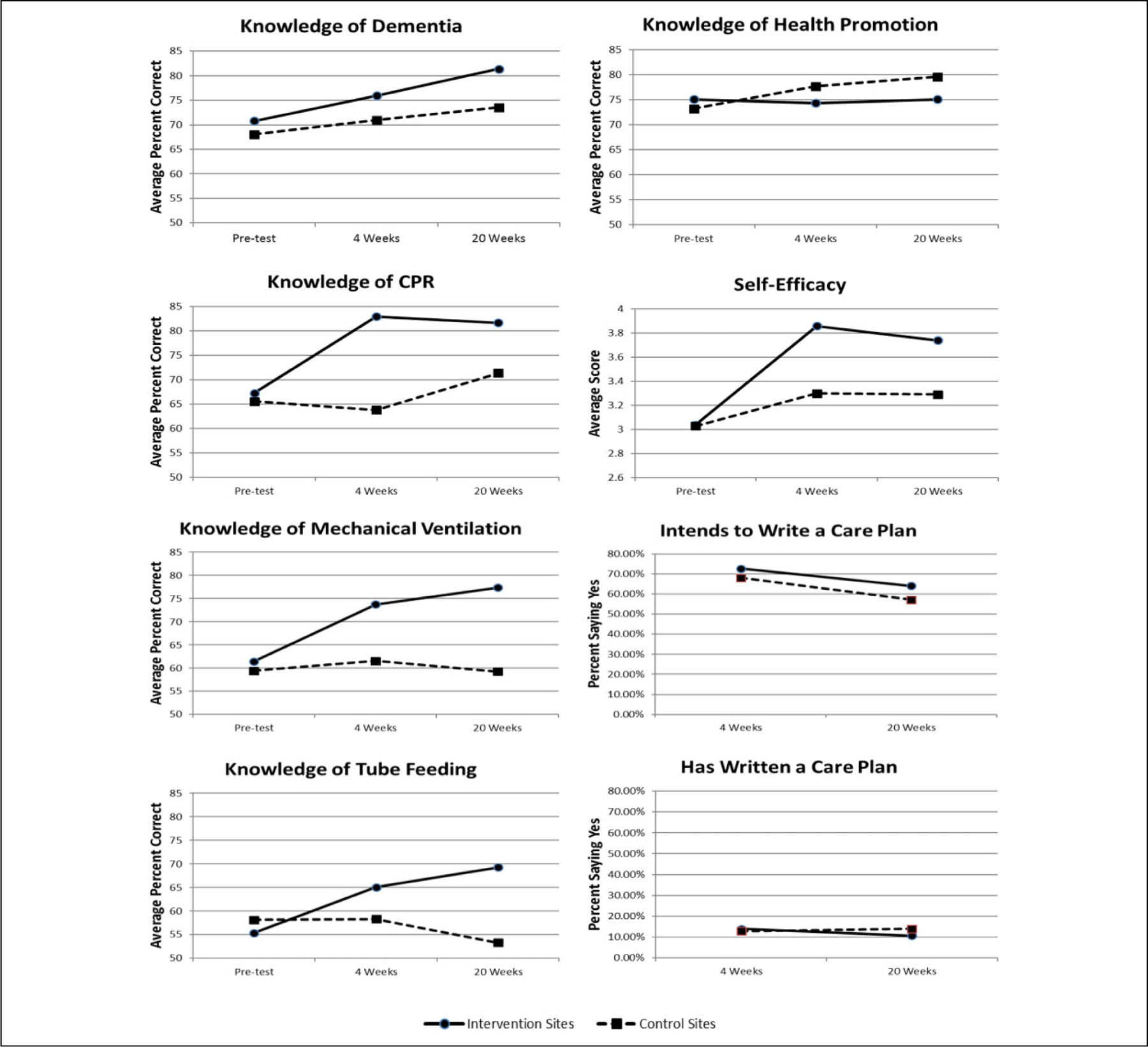
Mean outcomes across time by condition. *Adjusted for caregiver education (>High school y/n), caregiver occupation (5 categories), patient is caregiver’s parent (y/n), and severity of disability (4 categories) using multiple linear regression random intercept models for continuous outcomes and multiple logistic regression random intercept models for binary outcomes.
Table 4.
| Change From Pretest to Week 4 |
Change From Pretest to Week 20 |
|||||
|---|---|---|---|---|---|---|
| Continuous Outcomes | Intervention Sites Mean (SE) | Control Sites Mean (SE) | P Value Intervention vs Controla | Intervention Sites Mean (SE) | Control Sites Mean (SE) | P Value Intervention vs Controla |
| Knowledge of dementia (N = 334, n = 868) | 5.18 (2.34) | 2.88 (2.46) | .1759 | 10.61 (2.51) | 5.48 (2.51) | .0004 |
| Knowledge of CPR (N = 334, n = 873) | 15.67 (3.60) | −1.75 (3.75) | <.0001 | 14.40 (3.85) | 5.81 (3.85) | .0017 |
| Knowledge of MV (N = 334, n = 869) | 12.27 (3.45) | 2.10 (3.61) | <.0001 | 15.90 (3.70) | −0.18 (3.69) | <.0001 |
| Knowledge of TF (N = 334, n = 864) | 9.69 (3.83) | 0.16 (4.01) | .0006 | 13.88 (4.09) | −4.83 (4.08) | <.0001 |
| Knowledge of health promotion (N = 334, n = 875) | −0.75 (2.99) | 4.48 (3.08) | .0151 | −0.02 (3.19) | 6.44 (3.16) | .0042 |
| Self-efficacy (N = 334, n = 867) | 0.82 (0.15) | 0.27 (0.16) | <.0001 | 0.70 (0.16) | 0.26 (0.16) | <.0001 |
|
| ||||||
| Percent Saying “Yes” at Week 4 |
Percent Saying “Yes” at Week 20 |
|||||
| Binary outcomes | Intervention Sites Mean (SE) | Control Sites Mean (SE) | P Value Intervention vs Controla | Intervention Sites Mean (SE) | Control Sites Mean (SE) | P Value Intervention vs Controla |
|
| ||||||
| Intends to make a care plan for CPR, MV, and TF (N = 299, n = 543) | 72.7% (8.3%) | 68.1% (8.7%) | .5474 | 64.1% (10.1%) | 57.1% (10.3%) | .3401 |
| Has made a care plan for CPR, MV, and TF (N = 298, n = 543) | 13.9% (6.2%) | 12.9% (6.3%) | .8307 | 10.7% (6.0%) | 14.0% (6.8%) | .4722 |
Abbreviations: CPR, cardiopulmonary resuscitation; MV, mechanical ventilation; SE, Standard error ; TF, tube feeding.
N = total participants, n = total observations.
All means and SEs are adjusted for caregiver education (>High school y/n), caregiver occupation (5 categories), patient is caregiver’s parent (y/n), and severity of disability (4 categories) using multiple linear regression random intercept models for continuous outcomes and multiple logistic regression random intercept models for binary outcomes. P values are for tests of interactions between time and site contrast (average of intervention sites minus average of control sites) against zero for continuous outcomes and comparisons of predicted percentage at each time point for binary outcomes.
Knowledge of CPR, MV, TF, and self-efficacy increased from pretest in the ACT-Plan sites significantly more than in the control sites, at both week 4 (P < .0001, P < .0001, P = .0006, P < .0001) and week 20 (P = .0017, P < .0001, P < .0001, P < .0001). The increase in dementia knowledge was also greater in ACT-Plan sites at both points, statistically significant only at week 20 (P = .1749, P =.0004). Knowledge of health promotion increased more in control sites than ACT-Plan sites at both points (P = .0151, P = .0042), probably due to the health promotion content of the control condition. Proportions reporting intentions and behaviors toward a care plan were similar between ACT-Plan and control sites, with no statistically significant intervention effects at either time points (all P > .3). Differences in outcomes between sites within each condition (not shown) were significant only for dementia knowledge between the 2 control sites.
Use of the Bonferroni correction would change our conclusions for only one outcome in Table 4: knowledge of health promotion, which increased more in the control sites.
Discussion and Implications
As hypothesized, at weeks 4 and 20, the experimental group demonstrated more knowledge and self-efficacy. However, intentions and behaviors (written care plans) were not significantly different between the 2 groups. Two surprising findings were the low rates of intentions to write care plans and actual care plans written by participants in the ACT-Plan group, given significant increases in knowledge and self-efficacy. However, the outcome is consistent with findings from our previous feasibility study and cited in other literature.5,9,12,23 Further exploration is required to investigate reasons for the low rates.
Knowledge of CPR, MV, and TF increased after completion of the ACT-Plan. This result supports that caregivers are prepared to make informed treatment choices when they have knowledge about the risks and benefits. Although dementia knowledge scores were higher in the ACT-Plan group compared to attention control at week 4, significant increases were demonstrated at week 20. It is reasonable to assume that random error existed or participants in both groups were highly motivated to learn about dementia. The difference at week 20 is likely an effect of the booster sessions and emphasizes the need to repeat education content.
Wicher and Meeker3 reported that African Americans were likely to request all EOL treatments. However, after ACT-Plan, they were less likely to request all EOL treatments. Thus, a culturally acceptable educational approach may enable African American caregivers to make decisions consistent with the health needs of terminally ill relatives.24
Unbiased support allows caregivers to make such decisions with greater assurance of treatments consistent with family values and may decrease health-care costs to families and institutions.25 Although acquired knowledge is important for informed decision-making, implementation of behavioral intentions may require other factors beyond the scope of this investigation.
Study limitations include homogenous sampling and the small number of sites: 2 per condition. Statistically, this means we could underestimate standard errors for test effects. Selection bias may distort findings of association from samples exclusively taken from churches. However, we posited that megachurches are good sources to recruit African Americans for community-based studies because most are religious, protestant, and attend church services regularly.26 Therefore, the African American Church may provide representative samples for community-based trials. We selected 4 Protestant African American megachurches with combined memberships of approximately 16 000 people to recruit participants for this intervention. Lastly, the ACT-Plan model may not be as appropriate for other cultures that use a more individualistic and autonomous approach with decision-making.27
The education program could serve as a model for implementation in African American community settings. Implementation using in-person delivery by expert personnel in small group sessions is labor-intensive, limiting distribution due to cost and geographical area. We are currently in the process of developing a self-guided multimedia version of the ACT-Plan program suitable for wide dissemination.
Acknowledgments
The authors thank Kevin Grandfield, University of Illinois, College of Nursing, for editorial support with writing assistance in this manuscript. The authors acknowledge support from the UIC Center for Clinical and Translational Science (CCTS), grant number UL1TR002003, for the use of REDCap. The authors thank the religious leaders at the 4 participating churches for the continued support throughout the project. Successful completion of the investigation relied heavily on their committed contributions.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This grant was supported by the National Institute of Aginig (NIA), National Institutes of Health (NIH) grant number R01AG043485. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIA or NIH.The final peer-reviewed manuscript is subject to the National Institutes of Health Public Access Policy.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Clark PC, Kutner NG, Goldstein FC, et al. Impediments to timely diagnosis of Alzheimer’s disease in African Americans. J Am Geriatr Soc 2005;53(11):2012–2017. [DOI] [PubMed] [Google Scholar]
- 2.Teno JM, Gruneir A, Schwartz Z, Nanda A, Wetle T. Association between advance directives and quality of end-of-life care: a national study. J Am Geriatr Soc 2007;55(2);189–194. [DOI] [PubMed] [Google Scholar]
- 3.Wicher CP, Meeker MA. What influences African American end-of-life preferences? J Health Care Poor Underserved 2012;23(1):28–58. [DOI] [PubMed] [Google Scholar]
- 4.Zaide GB, Pekmezaris R, Nouryan CN, et al. Ethnicity, race, and advance directives in an inpatient palliative care consultation service. Palliat Support Care 2013;11(1):5–11. [DOI] [PubMed] [Google Scholar]
- 5.Nicholas LH, Langa KM, Iwashyna TJ, Weir DR. Regional variation in the association between advance directives and end-of-life Medicare expenditures. JAMA 2011;306(13):1447–1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bonner G, Williams S, Wilkie D, Hart A, Burnett G, Peacock G. Trust building recruitment strategies for researchers conducting studies in African American churches: lessons learned. Am J Hosp Palliat Care 2016;34(10):912–917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chin AL, Negash S, Hamilton R. Diversity and disparity in dementia: the impact of ethnoracial differences in Alzheimer disease. Alzheimer Dis Assoc Disord 2011;25(3):187–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Connell CM, Roberts JS, McLaughlin SJ, Carpenter BD. Black and white adult family members’ attitudes toward a dementia diagnosis. J Am Geriatr Soc 2009;57(9):1562–1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang CS, Crowther M, Allen RS, et al. A pilot feasibility intervention to increase advance care planning among African Americans in the Deep South. J Palliat Med 2016;19(2):164–173. [DOI] [PubMed] [Google Scholar]
- 10.Bonner G, Gorelick PB, Prohaska T, Freels S, Theis S, Davis L. African American caregivers’ preferences for life-sustaining treatment. J Ethics Law Aging 1999;5(1):3–15. [PubMed] [Google Scholar]
- 11.Bonner GJ, Darkwa OK, Gorelick PB. Autopsy recruitment program for African Americans. Alzheimer Dis Assoc Disord 2000; 14(4):202–208. [DOI] [PubMed] [Google Scholar]
- 12.Bonner GJ, Wang E, Wilkie DJ, Ferrans CE, Dancy B, Watkins Y. Advance care treatment plan (ACT-plan) for African American family caregivers: a pilot study. Dementia 2014;13(1):79–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Watkins YJ, Bonner GJ, Wang E, Wilkie DJ, Ferrans CE, Dancy B. Relationship among trust in physicians, demographics, and end-of-life treatment decisions made by African American dementia caregivers. J Hosp Palliat Nurs 2012; 14(3):238–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ajzen L, Fishbein M. Understanding Attitudes and Predicting Social Behavior Englewood Cliffs, NJ: Prentice Hall; 1980. [Google Scholar]
- 15.Kolb DA, Rubin IM, McIntyre JM. Organizational Psychology: An Experimental Approach Englewood Cliffs, NJ: Prentice-Hall; 1971. [Google Scholar]
- 16.Dilworth-Anderson P. Introduction to the science of recruitment and retention among ethnically diverse populations. Gerontologist 2011;51(suppl_1):S1–S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krakauer EL, Crenner C, Fox K. Barriers to optimum end-of-life care for minority patients. J Am Geriatr Soc 2002;50(1):182–190. [DOI] [PubMed] [Google Scholar]
- 18.Braun UK, McCullough LB, Beyth RJ, Wray NP, Kunik ME, Morgan RO. Racial and ethnic differences in the treatment of seriously ill patients: a comparison of African-American, Caucasian and Hispanic veterans. J Natl Med Assoc 2008;100(9):1041–1051. [DOI] [PubMed] [Google Scholar]
- 19.Alzheimer’s Association. Alzheimers facts and figures 2019 rA. Alzheimer Dement 2019;15(3):321–387. https://www.alz.org/media/documents/alzheimers-facts-and-figures-2019-r.pdf. [Google Scholar]
- 20.Ayalon L, Areán PA. Knowledge of Alzheimer’s disease in four ethnic groups of older adults. Int J Geriatr Psychiatry 2004; 19(1):51–57. [DOI] [PubMed] [Google Scholar]
- 21.Bedard M, Molloy DW, Squire L, Dubois S. The Zarit Burden interview: a new short version and screening version. Gerontologist 2001;41(5):652–657. [DOI] [PubMed] [Google Scholar]
- 22.Taylor RJ, Chatters LM. Church-based informal support among elderly blacks. Gerontologist 1986;26(6):637–642. [DOI] [PubMed] [Google Scholar]
- 23.Song MK, Ward SE, Fine JP, et al. Advance care planning and end-of-life decision making in dialysis: a randomized controlled trial targeting patients and their surrogates. Am J Kidney Dis 2015;66(5):813–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Becker C, Clark E, Despelder LA, et al. ; International work group for death, dying and bereavement (IWG). A call to action: an IWG charter for a public health approach to dying, death, and loss. Omega 2014;69(4):401–420. [DOI] [PubMed] [Google Scholar]
- 25.Alzheimer’s Association. Alzheimer’s disease facts and figures. Alzheimers Dement 2018;14(3):367–429. https://www.alz.org/media/Documents/alzheimers-facts-and-figures-infographic.pdf. [Google Scholar]
- 26.Pew Research Center. 5 Facts about the Religious lives of African Americans 2018. https://www.pewresearch.org/.../07/5-facts-about-the-religious-lives-of-african-americans. [Google Scholar]
- 27.Searight R, Gafford J. Cultural diversity at the end of life: issues and guidelines for family physicians. Am Fam Physician 2005; 71(3):515–522. [PubMed] [Google Scholar]


