Abstract
Objective.
To evaluate the impact of a youth-led nutrition intervention on youth-leaders themselves
Design.
Mixed methods, including: in-depth interviews and a quasi-experimental quantitative study comparing youth-leaders and nonparticipant comparison youth
Analysis.
Qualitative analysis using direct content analysis. Difference-in-differences analyses assessing quantitative program impact.
Results.
Youth-leaders perceived that the intervention impacted themselves, the youth-participants, and their respective social networks. Youth-leaders experienced greater increases in intentions to eat healthfully (p=0.04), and greater decreases in support for healthy eating from their friends (p=0.01), than the comparison group.
Conclusions/Implications.
Youth-leaders reported multiple levels of intervention impact, and increased intentions for healthy eating; however, additional research is needed to enhance impact on behavioral outcomes.
Keywords: Youth-led, Peer-led, Obesity, Adolescent, Nutrition, African-American, Mentoring, Mixed-Methods
INTRODUCTION
Childhood and adolescent obesity rates in the United States have increased rapidly over the past three decades.1,2 Although there is some evidence that the rates have plateaued,3 and declined in some sub-groups,4 rates remain alarmingly high, and disproportionately affect low-socioeconomic status and minority youth.5,6 While progress has been made toward identifying strategies to reverse obesity trends,7 continued efforts are needed, particularly for low-income African-American youth.
Recognizing the strong influence of social relationships on adolescent behavior, health disciplines have incorporated youth into intervention teams to champion changes related to health issues such as HIV and smoking.8,9 To date, there have been a limited number of published youth-led obesity prevention programs.10,11,20–23,12–19 While these youth-led studies widely varied in their implementation, many showed promising results, including: increased sales of healthier options in schools;13,24 improvements in obesity-related psychosocial outcomes such as knowledge, attitudes, self-efficacy, and perceived social support;11,17–19,25–27 improved dietary intake, including increased fruit and vegetable intake,20,21 reduced intake of snacks/desserts,10 and sugar sweetened beverages;12,14 organizational and local-level policy change23; and improvement in anthropometric measures.10,16,26,28,29
These initial successes indicate that health improvements can result from youth-led programs; however, additional research is needed to understand the utility of incorporating youth-leaders in childhood obesity-prevention programs. A key gap in this literature is examining the impact of programs on the youth-leaders themselves. The literature indicates that youth-leaders may receive the largest impact of the intervention because they receive the highest dose.30 However, among the nutrition-related youth-leader studies, many fail to report any outcomes concerning the youth-leaders.12,14,17,26,31 In studies where youth-leaders were evaluated, they were often assessed using the same metrics as the general study population, which fails to capture factors specific to youth-leaders’ unique perceptions of the intervention as well as their role in intervention design or delivery. 15,16,28,29 The few studies that assessed youth-leaders separately used brief questionnaires or interviews to assess food/beverage intake, attitudes, social norms, and the youth-leaders’ perceptions of the project.10,24,30,32,33 None of these studies have comprehensively evaluated the intervention using multiple research strategies to obtain important information such as youth-leader characteristics, qualitative perceptions of the intervention impact, and quantitative impact of the intervention on the youth-leaders relative to a comparison group.
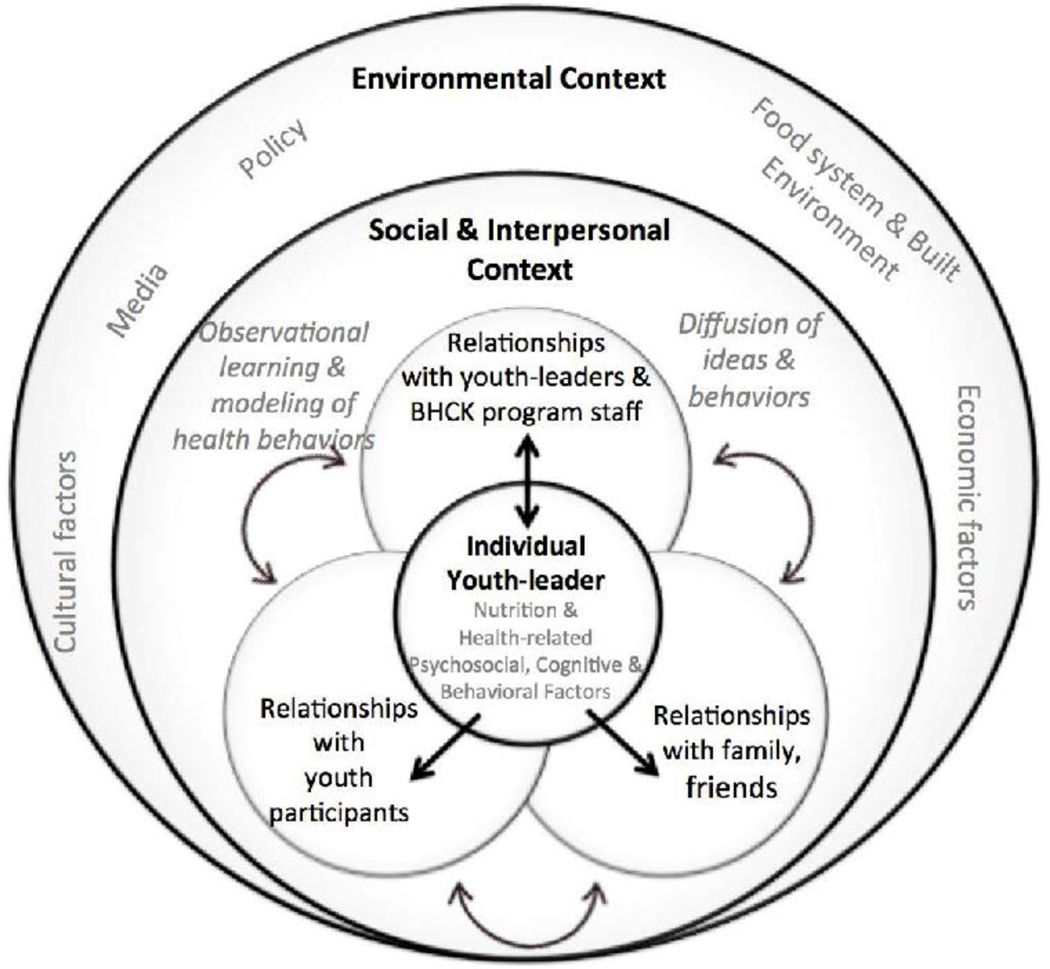
The B’More Healthy Communities for Kids (BHCK) study provides a novel opportunity to assess the impact of a nutrition-intervention on youth-leaders. BHCK was a multi-level obesity prevention intervention focused on improving the nutritional health of low-income, urban, African-American youth ages 10–14.34 Within the BHCK study, a cohort of Baltimore-based racial and ethnic minority high school and college students were trained as youth-leaders, with the purpose of delivering a nutrition intervention to younger peers. The BHCK study was developed based upon social cognitive theory (SCT), social ecology, and systems theory, the theoretical basis of the overall study is described elsewhere34. The youth-leader component of BHCK specifically drew from social learning theory (SLT)35, the social ecological model (SEM)36, and diffusion of innovations theory (DoI)37. The SEM posits that the individual is nested within broad social and environmental contexts that reciprocally influence multiple psychosocial, cognitive, and behavioral processes of that individual36. In addition, SLT specifically describes the concepts of observational learning or modeling in which an individual observes the behaviors of others and then reproduces those behaviors35. DoI describes the ways that ideas spread, particularly through leaders/early adopters who spread ideas to others37. We hypothesized that by being engaged in BHCK, youth-leaders would experience observation learning/modeling of healthy behaviors, and help spread those ideas through their interactions with others. The integrated application of these theories in this youth-led intervention is depicted in Figure 1.
Figure 1.
Conceptual Framework for the Integration of Social Learning Theory, the Social Ecological Model, and the Diffusion of Innovations Theory into the Youth-leader Intervention Design.
The combined use of SCT/SLT and the SEM as a theoretical framework for identifying influential factors on eating behaviors in youth population is common, with Story and colleagues providing a foundational framework 38, which has been used to develop previous youth-focused nutrition interventions10,11,24,31. In addition, youth-led nutrition interventions11 and other health-related youth-lead interventions8,39 often incorporate the DoI theory (which explains the adoption or spread of new ideas in a group), complementing the observational learning principles emphasized in SLT.
The purpose of this paper is to assess the intervention impact on the BHCK youth-leader cohort. To do so, three research questions were addressed:
What are the characteristics of youth who participated as youth-leaders? Were they able to implement the intervention?
What were youth-leaders’ perceptions of the BHCK intervention and its impact on themselves, intervention participants, and individuals outside of the BHCK intervention?
Did participation in the program improve psychosocial factors, dietary intake, and leadership characteristics of youth-leaders relative to a comparison group?
METHODS
B’More Healthy Communities for Kids Study
The BHCK trial was a systems-oriented childhood obesity prevention intervention, with the goal of preventing obesity among 9–15 years-old youth by creating synergistic intervention strategies at multiple levels of the food system. The BHCK trial used a group-randomized study design, where 30 low-income neighborhoods served as either intervention (n=14) or comparison (n=16) areas. The intervention was implemented in two waves (Wave 1: July 2014-February 2015; and Wave 2: November 2015-August 2016). Eligibility criteria required all participating neighborhoods to be predominantly low-income, African-American food deserts.34
BHCK Youth-leader Intervention
The youth-leader component of the BHCK intervention involved recruiting, training, and evaluating 16 Baltimore-based college or GED students (Wave 1) and 9 Baltimore-based high school students (Wave 2) whose primary role was to deliver a 14-session nutrition curriculum to younger peers (9–15 years old) in recreation centers in the intervention neighborhoods. Additional roles of the youth-leaders included supplementing the BHCK retail food outlet intervention by delivering in-store interactive sessions, generating Facebook and Instagram content for BHCK’s social media intervention, and serving as intervention ‘spokespeople’ in videos, posters and handouts. Each of the 14 recreation center sessions facilitated by youth-leaders involved an icebreaker activity, a brief educational component, a taste test of a healthier food/beverage item, and experiential learning such as interactive games or cooking classes (see supplementary materials). The curriculum focused on four content areas that aligned with other BHCK intervention levels: beverages, snacks, breakfasts, and cooking. Youth-leaders implemented the BHCK nutrition curriculum in each intervention recreation center for one hour every other week, for 6 months in both Waves. On average, teams of 3 youth-leaders delivered each session in the recreation centers.
The BHCK youth-leader component was identical in content across Waves 1 and 2, though Wave 2 tested for sustainability of the program, with youth-leaders being high school students from the community surrounding the intervention recreation centers.40 Youth-leaders were recruited through flyers sent to academic institutions (high schools, colleges, and GED programs), recreation centers, and social media. All youth-leaders lived in Baltimore during the intervention. Many, but not all, of the youth-leaders were recruited from the same communities in which the intervention was taking place.
During Wave 1, a total of 135 applications for the youth-leader position were received, 41 candidates were interviewed, and 16 were selected to be youth-leaders. These 16 were selected based on their age (required to be 18–22 years old during Wave 1), availability, and interest in working with youth around health. In Wave 2, 45 applications were received, 25 were interviewed in-person (required to be 15–18 years old attending high school), and 14 were selected to be youth-leaders. All youth-leaders completed an intensive 12 session (27-hour) training program, which used interactive learning strategies to promote team-building, leadership and communication skills, along with intervention delivery practice and feedback. Wave 1 youth-leaders were paid $10 an hour for an average of 3 hours per week, and Wave 2 youth-leaders received service learning hours and financial small incentives.
Assessment of Youth-leader Characteristics and Description of Intervention Implementation (Research Question 1).
Data Collection and Analysis.
Youth-leader characteristics (age, race, weight status, and educational level) were collected during baseline surveys. Descriptive measures of the youth-led intervention sessions were collected and monitored by the BHCK staff that oversaw implementation at the recreation center. Information collected included: number of recreation center sessions delivered by the youth-leaders; number of youth that the youth-leaders interacted with per session; and youth-leader retention rate. Descriptive statistics were used to analyze these data, and test statistics (t-tests, chi-square tests, and Fisher’s Exact tests) were used to determine differences between groups at baseline among measured characteristics. Additional implementation evaluation measures (reach, dose, fidelity) of the BHCK youth-leader intervention were published elsewhere.41
Assessment of Youth-leader Perceptions of Intervention Impact (Research Question 2)
Data Collection.
A BHCK researcher (initials redacted for review) trained in qualitative research methods conducted in-depth interviews with the 16 youth-leaders in Wave 1. An in-depth interview guide developed for youth-leaders working with low-income, urban youth around nutrition issues was adapted for the purposes of this study. 32 Modifications to the interview guide included tailoring questions to specific study components such as the behavioral theories driving this intervention SLT, 42 SEM, 36 DoI. 37 Additionally, the interview focused on the youth-leaders’ perceived impact of and feedback on the BHCK program. Interviews were conducted one-on-one with the youth-leaders and lasted 45–95 minutes. The interviewer was involved in the youth-leader intervention delivery, and established good rapport with the youth-leaders that carried over into the interviews. Youth-leaders received a $20 gift card after completing the interview. Interviews were audio-recorded and transcribed verbatim. ATLAS.ti software version 7 (ATLAS.ti Scientific Software Development GmbH, Berlin, Germany) was used for data analysis. The BHCK intervention was approved by the [redacted for review] IRB. Informed consent/assent, and parental consent for participants under the age of 18, were obtained prior to the interviews with youth-leaders.
Data Analysis.
Qualitative data analysis was guided by the principles of directed content analysis.43 Coders (initials redacted for review) reviewed the transcripts and generated an initial list of significant themes. These themes, along with a priori codes of constructs from relevant behavioral theories (SLT, 42 SEM,36 DoI 37) and specific research questions, were used to develop a codebook that was iteratively modified and used throughout the coding process. Fifty-six codes were developed (example codes include: relationships between youth-leaders and participants; intervention impact on youth-participants). Coders coded two initial transcripts to resolve discrepancies in code usage, and to refine the codebook. After the initial double-coding, transcripts were coded individually. The researchers took several steps to assure consistent applications of codes, including routine meetings to ensure codes were applied consistently and discuss emerging themes at length. After transcripts were coded, one researcher (initials redacted for review) reviewed all transcripts to confirm consistent use of codes and to add new themes that emerged through the coding process.
Assessment of Intervention Impact on Youth-leader Psychosocial Factors, Dietary Intake, and Leadership Skills (Research Question 3)
Data Collection.
The impact of the intervention on the youth-leaders (baseline n=30; follow-up n= 25) and a cohort of comparison youth (baseline n=21; follow-up n=16) was quantitatively assessed. Comparison youth had applied for the youth-leader position but were not selected for reasons such as schedule conflicts or unmet age criteria. Quantitative measures included a Youth-leader Impact Questionnaire (YIQ) modified from the literature,31,44–47 and the Block 2004 Kids Food Frequency Questionnaire (FFQ).48
The YIQ assessed psychosocial factors related to healthy eating, anthropometrics, food behaviors, dietary intake, and leadership skills. Psychosocial factors for healthy eating included measures of behavioral intentions for making healthier food decisions (an 11-item scale, asking participants to report their intentions for making healthier and less healthy choices in the future); self-efficacy (a 13-item scale, asking participants how confident they were in performing some nutrition-related behaviors); and outcome expectations (a 9-item scale, asking participants whether statements about health-related behaviors were true or false). Social support for healthy and unhealthy eating was measured using a 14-item scale, where participants were asked to report the frequency of receiving social support from their friends and family.
Food behavior measures included a scale that assessed the frequency of sugar-sweetened beverage, non-sugar sweetened beverage, and fruit and vegetable purchases; as well as the use of healthy and unhealthy food preparation methods. Leadership skills were assessed using a 13-item scale that asked youth-leaders to rate their confidence in handling common leadership-related tasks.
The Block 2004 Kids FFQ is a validated, 77-item, semi-quantitative FFQ that assesses the past 7 days of intake. The FFQ was validated with a slightly younger population (ages 10–17) than the youth-leaders of this study (ages 15–22), and thus only select nutritional components (calories, calories from sugar sweetened beverages, fruit and vegetable intake) were used from the FFQ assessment. Detailed descriptions of all measures and scoring can be found in Table 1. Participants received a $30 gift card after completing the questionnaires.
Table 1:
Description of Quantitative Measures Used to Assess Youth-leaders Pre- and Post-Intervention
| Domain | Description |
|---|---|
| Demographics | Demographic measures included self-reported age, gender, race/ethnicity, and education level. |
| Weight Status | Height and weight were measured in duplicate and averaged. In cases where participants refused measurement, self-reported height and weight measures were accepted (8% of measures). Participants were then classified by weight status (normal, overweight/obese) using age-appropriate methods (BMI equation and standard cutoffs for participants >20 years old, and CDC BMI-for-Age percentile and standard cutoffs for participants <20 years old.) |
| Dietary Intake48 | |
| Total Calories, Calories from Sweetened Beverages, Fruit Servings, Vegetable Servings, Total Fat (grams) |
Four measures of dietary intake were assessed: total calories, calories from sweetened beverages, fruit servings, and vegetable servings. These were estimated using the Block 2004 Food Frequency Questionnaire for Kids, which is a 77-item validated semi-quantitative FFQ that assesses the past 7-day intake. |
| Food-related Behavior31,47 | |
| Total Sugar-Sweetened Beverage (SSB) Purchasing (frequency), Total non-SSB Purchasing (frequency) Total FV purchasing (frequency) Healthy Food Purchasing Score Unhealthy Food Purchasing Score Healthy cooking preparation Score |
Frequency of Food Purchasing: food acquired in the previous 7 days from a pre-defined list of 38 healthier (Cronbach’s alpha=0.88) and 28 less healthful foods and beverages (Cronbach’s alpha=0.79). SSB included regular soda, fruit drink, sports drink, energy drink, and sweetened tea. Non-SSB included water, diet soda, low-sugar flavored water, unsweetened tea, 100% fruit juice, and water drink mix. Healthy Cooking Preparation Score: reflects preparation methods used in the previous 7 days. Each food preparation method was assigned the following score based on the healthiness of the method: fried=−1, baked=+1, microwaved=+1, raw=+1, other=0. The total score for each cooking method was averaged and calculated taking into account the number of times food was prepared. The youth food preparation score ranged from −1 to +1, mean=0.46 (SD=0.71). |
| Psychosocial Factors31,46 | |
| Self-efficacy | A 13-item scale asking participants to rate how confident in they are in performing selected nutrition-related behaviors (example statement: I can eat a healthy breakfast even when I am running late for school or work). Participants could respond on a 4-point scale that included: I know I can (3), I think I can (2), I’m not sure I can (1), and I know I can’t (0). Responses were summed to create the scale score (possible range 0–39, Cronbach’s alpha=0.76). |
| Behavioral Intentions | A 11-item scale asking participants to report their intentions to make healthier or less healthy eating choices in the future. Each question had 3 different potential answer choices. Responding with the healthiest choice (i.e., grapes) received 1 point, and all other responses receive 0 points. Points were summed to create the total score (possible range 0–11, Cronbach’s alpha= 0.62). |
| Outcome Expectations | A 9-item scale asking participants to report if they believe statements linking eating behaviors and health outcomes are true or false (example question: I will gain weight if I eat a lot of fatty foods, like potato chips). Participants would respond by saying the statement was true (2 points), mostly true (1 point), mostly false or false (0 points). Points were summed to create the total score (possible range 0–20, Cronbach’s alpha= 0.60). |
| Social Support44 | |
| Social Support for Healthy and Unhealthy Eating | A 14-item questionnaire where youth report the frequency of their caregivers or their friends providing social support for healthy and unhealthy eating behaviors. This questionnaire measures four scales, including: two four-items scales for parent and friend support for healthy eating (example question: How often do your parents/friends give you ideas on how to eat healthier foods?) and two three-item scales measuring parents/friends support for unhealthy eating. Possible responses: never (0), rarely (1), sometimes (2), often (3), very often (4). Scores were summed to create each scale (possible range for healthy eating support scales (0–16), possible range for unhealthy eating support scales (0–12), Cronbach’s alpha’s ranged from 0.70–0.90). |
| Leadership Skills45 | |
| Youth-Leader Skills | Adapted from the youth-leadership literature, this 13-item scale assesses the youth-leaders’ confidence in their abilities to handle common tasks associated with the youth-leader role such as preparing for intervention sessions, problem-solving, and communication. Possible responses were: not at all confident (0), somewhat confident (1), confident (2), and very confident (3). Responses were summed and higher scores indicate higher youth-leader skill levels. (Possible range 0–39, Cronbach’s alpha = 0.94) |
Data Management and Analysis.
The study experienced a 20% attrition rate between baseline and follow-up assessments among youth-leaders in both the intervention and comparison groups. Youth with incomplete impact data were dropped from analyses (n=10), after exploring patterns of missing completely at random mechanism. All other data were complete. To address the non-random assignment of youth-leaders, difference-in-differences analyses were used to assess changes in the groups over time. Difference-in-differences analyses reduce the effect of selection bias by comparing the average change over time in the intervention and comparison groups, and avoids over-estimation of significance levels.49 All analyses were conducted in Stata version 13.1 (Stata Corp LP, College Station, TX). The difference-in-differences analyses used linear regression models with the dependent variable being the outcome of interest, and included independent variables of time, treatment group, and a group*time interaction. Normality assumptions were met in all models. Models controlled for potential confounders (age, sex, and total caloric intake),50 and corrected standard errors for the clustering of repeated measures within individuals. Statistical significance was determined at p<0.05.
RESULTS
Youth-leader Characteristics and Description of Intervention Implementation (Research Question 1)
All youth-leaders were racial or ethnic minorities; most were African-American. There were no differences among groups at baseline in measured demographics, except for a difference in age among youth-leaders in waves 1 and 2, which was the result of the study design (Table 2). Common rationales for youth-leader’s interest in participation included: giving back to the community, passion for working with youth, and gaining professional experience.
Table 2.
Baseline Anthropometric and Sociodemographic Characteristics of the BHCK Youth-leader Intervention and Comparison Samples (n=41)
| Wave 1 | Wave 2 | Total n=41 | |||
|---|---|---|---|---|---|
|
|
|||||
| Intervention n=16 | Comparison n=9 | Intervention n=9 | Comparison n=7 | ||
|
| |||||
| Gender, n (%)§ | |||||
| Female | 12(75%) | 6(60%) | 7(78%) | 5(71%) | 30(71%) |
|
| |||||
| Age (M±SD)1‡ | 19.7±1.4a* | 17.5±1.9b | 17.5±2.1 | 17.3±2.7 | 18.3±2.1 |
|
| |||||
| Race, n (%)¶ | |||||
| Black, African American | 14(88%) | 9(90%) | 9 (100%) | 7 (100%) | 39(92%) |
| Pacific Islander | 1(6%) | 0(0%) | 0(0%) | 0(0%) | 1(3%) |
| Other or Mixed Race | 1(6%) | 1(10%) | 0(0%) | 0(0%) | 2(5%) |
| Ethnicity, n (%) | |||||
| Hispanic / Latino | 1(6%) | 0(0%) | 0(0%) | 0(0%) | 1(2%) |
|
| |||||
| BMI Category, n (%)2¶ | |||||
| Normal weight | 8(50%) | 6(60%) | 6 (67%) | 5(72%) | 25(60%) |
| Overweight | 6(38%) | 4(40%) | 2 (22%) | 1(14%) | 13(31%) |
| Obese | 2(12%) | 0(0%) | 1(11%) | 1(14%) | 4(9%) |
|
| |||||
| Education Level, n (%)3¶ | |||||
| High school student | 2(12%) | 5(50%) | 8(89%) | 6(85%) | 21(50%) |
| Completed high school degree | 4(25%) | 2(20%) | 0(0%) | 6(14%) | |
| College Student | 10(63%) | 3(30%) | 1(11%) | 1(15%) | 15(36%) |
Age at baseline, M±SD = Mean±Standard deviation
Weight status at intervention start. Classified by BMI-for-Age percentiles from CDC growth charts for youth <20 years old, and on standard cut offs for youth >20 years old
Education level represents student status at baseline
Statistical significant difference between groups (P<.05)
Pearson Chi-square to compare the groups (2-sided)
2-tailed t-test
Fisher’s Exact Test to compare the groups (2-sided)
In each Wave, youth-leaders delivered 98 sessions in the recreation centers, which equaled 100% of the planned intervention sessions. An average of 10 youth-participants (ages 9–15) attended each session. From the recreation center and store intervention sessions combined, youth-leaders had over 1,600 interactions with participants per Wave. Youth-leader retention in the program delivery was high (75%) during Wave 1 and moderate (50%) in Wave 2. Two youth-leaders left the program immediately after training- one due to interpersonal conflicts with other youth-leaders and another due to lack of interest. Another ten youth-leaders chose to leave the study during the intervention due to schedule conflicts, transportation issues, and/or lack of interest.
Youth-leader Perceptions of Intervention Impact (Research Question 2)
Perceived Intervention Impact on Youth-Participants.
Youth-leaders expressed low levels of self-efficacy to influence the youth-participants initially; however, leaders later reported being pleasantly surprised by how well youth-participants responded to the intervention sessions. One youth-leader said “they actually, like, listen and pay attention. I was so shocked they remembered.” Youth-leaders also reported witnessing changes in youth-participants’ behaviors. For example, the same youth-leader went on to explain, “I’ve seen someone change their beverage choice in the stores. I have seen children remember what I said to them last week and tell me what they did that week to make changes to what we talked about.”
Youth-leaders attributed their ability to impact youth-participants to the leader-participant relationships developed over the course of the intervention. One youth-leader said, “we know what to do to reach them, like, to get them to understand and to get them to want to change, and they know that we were once in their shoes. And they kind of want to be like us, so they’re gonna do what they see us doing, they wanna follow our lead.”
Youth-leaders described also feeling that their role was impactful on youth because it provided caring interactions. A youth-leader said, “I get to be that person that I didn’t have when I was a young person. Like, no one really sat down and told me and showed me healthy eating styles and ways. Now I get to do that for somebody else.” In addition, many youth-leaders lived in the intervention communities, and reported having positive interactions with youth outside of the intervention sessions.
Perceived Intervention Impact on Youth-leaders’ Personal Behaviors.
Youth-leaders described that participation in BHCK impacted their health behaviors and life skills. Youth-leaders reported drinking more water/fewer sweetened beverages, reducing fast food consumption, eating appropriate portions, and eating breakfast and fruits and vegetables more frequently. However, youth-leaders often expressed this as a process of change, acknowledging that changes were happening incrementally over time. One youth-leader reported, “sometimes it’s hard, but at the same time, [you] gotta start with baby steps.” Youth-leaders reported avoiding being “hypocrites,” and acknowledged that being consistent with the health messages they were providing youth in the intervention served as motivation. A youth-leader said, “I’m trying, I really am. ‘Cause I always tell myself, I can’t go and talk to children about healthy eating and making healthy choices when I’m not doing it myself.”
Youth-leaders also described gaining communication and leadership skills from the intervention: “I learned new ways to teach and to go about presenting things that can be applied in real life…with children in the rec center, with college presentations, with talking with a little cousin about changing eating habits, everything.” Youth-leaders frequently reported that they were personally benefitting from the intervention, which encouraged their continued engagement.
Perceived Intervention Impact on Individuals Outside of the BHCK intervention.
Youth-leaders frequently described sharing the new knowledge, skills, and strategies learned through the BHCK intervention with others (parents, siblings, friends, and co-workers). One youth-leader described sharing intervention information with her mother, saying “My mother knows what I am doing [as a youth-leader] so she just listens to me. Like when I come home, I always have something from here, I always have something new to tell her.” Another youth-leader described implementing intervention components with his younger siblings: “I’m like the water police at the house. At the house, everybody knows, eight cups of water a day.”
Youth-leaders also identified the youth-participants as potential drivers of change within their social networks. One youth-leader said, “I think kids have the ability of questioning their parents and their parents would just be like ‘who taught you that? Where did you get that from?’ Things like that will spark a change in a whole household.”
Intervention Impact on Psychosocial Factors, Dietary Intake, and Leadership Skills of Youth-leaders (Research Question 3).
Table 3 presents the mean changes in youth-leaders’ food-related behaviors, psychosocial characteristics and leadership skills at baseline and post-intervention in the difference-in-differences analyses. Over time, youth-leaders increased their intentions for healthy eating, while the comparison group decreased their intentions to eat healthfully (β=2.0, Robust SE=0.9, p=0.04). Youth-leaders reported decreased friend support for healthy eating over the course of the intervention, while the comparison sample reported increased friend support (β=−3.5, Robust SE=1.3, p=0.01). Significantly different changes over time between the groups were not found in dietary intake, leadership skills, or other psychosocial factor measures.
Table 3:
Mean Scores for Dietary Intake, Food Purchasing and Cooking Behavior, Psychosocial, and Leadership Measures among Youth-leaders and Comparison Youth at Baseline and Post-Intervention (n=41)
| Measuresab | Scale Range | Intervention | Comparison | Adjusted Difference-in-differencesc | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Baseline | Post-Int. | Change over time | Baseline | Post-Int. | Change over time | |||
|
| ||||||||
| Dietary Intakeb | (n=25) | (n=25) | (n=16) | (n=16)c | ||||
|
| ||||||||
| Total Calories | n/a | 1413.9±154.4 | 1243.7±157.9 | −170.2 | 1739.8±183.6 | 1286.9±167.2 | −452.9 | 282.7 |
| Calories from Sweetened Beverages | n/a | 171.8±55.2 | 160.1±46.1 | −11.8 | 104.1±67.1 | 99.1±49.1 | −5.0 | 6.8 |
| Total Grams of Fat | n/a | 6.7±3.2 | 4.5±3.3 | −2.2 | 7.8±4.1 | 4.5±3.4 | −3.3 | −1.1 |
| Fruit Serving | n/a | 1.1±0.3 | 0.7±0.3 | −0.4 | 0.7±0.2 | 0.6±0.2 | −0.1 | −0.3 |
| Vegetable Servings | n/a | 1.1±0.3 | 0.6±0.3 | −0.5 | 0.6±0.5 | 0.5±0.4 | −0.1 | −0.4 |
|
| ||||||||
| Food-related Behavior | ||||||||
|
| ||||||||
| Total SSB Purchasing (frequency) | n/a | 2.7±0.6 | 1.8±0.6 | −0.9 | 2.7±0.7 | 2.5±0.6 | −0.2 | −0.7 |
| Total non-SSB Purchasing (frequency) | n/a | 2.3±0.6 | 1.7±0.6 | −0.6 | 2.8±1.1 | 1.4±1.7 | −1.4 | 0.8 |
| Total FV purchasing (frequency) | n/a | 2.2±0.8 | 1.9±0.6 | −0.3 | 1.6±0.9 | 2.1±0.8 | −0.5 | −0.8 |
| Healthy Food Purchasing Score | 0; 40 | 4.8±1.3 | 4.8±1.1 | 0.0 | 2.9±1.4 | 6.0±1.8 | 3.1 | −3.1 |
| Unhealthy Food Purchasing Score | 0; 18 | 5.3±1.0 | 4.1±1.0 | −1.2 | 4.6±1.1 | 5.1±0.9 | 0.5 | −1.7 |
| Healthy cooking preparation Score | −1; 1 | 0.3±0.2 | 0.4±0.2 | 0.1 | 0.3±0.2 | 0.3±0.2 | 0.0 | 0.1 |
|
| ||||||||
| Psychosocial Factorsb | (n=25) | (n=25) | (n=17) | (n=16)c | ||||
|
| ||||||||
| Self-efficacy | 0; 39 | 29.0±4.0 | 28.0±4.2 | −1.0 | 26.5±4.4 | 26.4±4.3 | −0.1 | −0.9 |
| Behavioral Intentions | 0; 10 | 6.1±1.0 | 7.0±0.9 | 0.9 | 4.9±1.0 | 3.8±0.7 | −1.1 | 2.0* |
| Outcome Expectations | 0; 20 | 16.1±0.9 | 17.5±0.7 | 1.4 | 16.0±2.2 | 16.2±2.6 | 0.2 | 1.2 |
| Parent Support for Healthy Eating | 0; 16 | 9.4±1.8 | 7.2±1.6 | −2.2 | 8.1±2.0 | 8.3±1.6 | 0.3 | −1.9 |
| Friend Support for Healthy Eating | 0; 16 | 4.5±1.1 | 2.2±0.9 | −2.3 | 1.4±1.2 | 2.6±0.9 | 1.2 | −3.5* |
| Parent Support for Unhealthy Eating | 0; 12 | 3.3±0.9 | 3.8±0.9 | 0.5 | 2.9±1.0 | 3.6±0.9 | 0.7 | −0.2 |
| Friend Support for Unhealthy Eating | 0; 12 | 5.5±0.8 | 5.9±0.8 | 0.4 | 5.0±1.1 | 6.3±0.9 | 1.3 | −0.9 |
|
| ||||||||
| Leadership Skillsb | ||||||||
|
| ||||||||
| Youth-leader Skills | 0–39 | 44.7±16.6 | 44.5±17.8 | 0.2 | 43.1±14.7 | 44.9±15.3 | 1.8 | −2.1 |
Abbreviations: SSB (sugar sweetened beverages); FV (fruits and vegetables)
Statistically significant (p<0.05) difference in changes between groups over time
All measures are expressed at mean±standard error (robust), Higher scores represent higher levels of each measure
Dietary intake measures, assessed by the Block Kids FFQ48; self-efficacy, behavioral intentions, outcome expectations46; support for healthy and unhealthy eating scales44; leadership skills45
Difference-in-difference analysis with robust standard error estimation, clustered at the individual-level (repeated measures), controlled for age and sex. Dietary intake and psychosocial factor analyses were controlled for age, sex, and total caloric intake.
DISCUSSION
This is one of the few studies that specifically evaluates the impact of a youth-led intervention on the youth-leaders themselves. To our knowledge, this is the first study to use multiple research methods to evaluate the characteristics of youth-leaders, to assess their perceptions of intervention impact, and to examine the impact of the intervention on their own dietary intake, psychosocial factors, food behaviors, and leadership skills. The BHCK youth-leaders successfully carried out the intervention, and the BHCK program had a high level of youth-leader retention, demonstrating improvement from previous studies conducted by the research team.31
Youth-leaders described the impact of the intervention on themselves, the youth-participants and others not directly involved in the intervention. In the qualitative assessment component, youth-leaders described making efforts to change their personal eating habits to be consistent with the nutrition messages that they were promoting, and emphasized the importance of the interpersonal relationships they were able to make with the youth-participants. These results are consistent with key themes in another study that qualitatively assessed youth-leader perceptions. 32 Youth-leaders also reported extending the impact of the intervention to their own social networks by sharing information with siblings, family members, friends, and co-workers. This is consistent with another youth-led intervention where nearly all (96%) of youth-leaders reported talking to others about their respective intervention.24
The results of the difference-in-differences analyses showed that youth-leaders’ intentions to eat healthfully increased more than comparison youths’. This is consistent with the literature that demonstrates improvements in youth-leaders’ psychosocial factors.24,33 The behavioral intentions for healthy eating also triangulates with the qualitative and quantitative results in this study. Youth-leaders described wanting to make changes via “baby steps” in their eating and activity habits, and acknowledged that making those changes could be difficult.
Seeing increases in behavioral intentions for healthy eating, but not changes in actual behavior (dietary intake) reflects the difficulties in changing behaviors that youth-leaders described. This finding is consistent with a meta-analysis of studies on health behavior change51. The meta analysis described that when individuals have high levels of perceived and actual control over a behavior, then their behavioral intentions and actual behaviors are closely linked; however, when health behaviors are more complex and difficult, such as eating a healthier diet, behavioral intentions may be high, but actual, measurable health behavior change may be lower51. Often youth, including youth-leaders, have limited control over their dietary intake due to factors such parents providing most of their foods/beverages, and limited income and time available to purchase/prepare their own food/beverages. Physical activity (and/or sedentary behavior) on the other hand, may be an important factor to intervene on and assess, as youth-leaders may have more behavioral control in those areas, and valid subjective52 and objective physical activity measures53 are readily available.
Despite this discrepancy in changing behavioral intentions versus actual behaviors identified in this study, other youth-led interventions have reported significant changes in actual dietary consumption behaviors of youth-leaders or youth that are highly engaged in the intervention.24,30 We hypothesized that the BHCK youth-leader intervention would passively impact the youth-leaders’ psychosocial factors and diet-related behaviors, however, there were not specific behavior change intervention components or health-related goals directed at the youth-leaders, which may have limited the impact of the intervention on the youth-leaders dietary intake. Incorporating multi-pronged participatory research strategies to help youth-leaders address their personal health behaviors, such as diet and physical activity levels, in addition to delivering the intervention to younger youth could strengthen the impact of this intervention on youth-leaders health behaviors.
Youth-leaders also experienced a decrease in perceived support for healthy eating from friends, while comparison youth reported an increase in perceived support. This finding was interesting, as it had not been previously investigated in the published literature. We hypothesize that the decrease in youth-leader’s perceived support from their friends may have been related to the extensive support they received from their youth-leader peers and the BHCK program staff, which could have made any support from friends outside the program seem insufficient relative to their newly developed expectations. An alternative explanation for this decrease in support seen among youth-leaders could be that youth-leaders had high expectations for friends’ support prior to starting the study, and these expectations were not met once youth-leaders began making changes to their dietary habits over the course of the study. Given that this is the first study to report on the impact of a youth-led intervention on youth-leaders’ perceptions of social support for healthy and unhealthy eating, future studies need to further explore the relationship between social support and youth-led interventions.
The limitations of this research should be noted. The limited number of statistically significant changes observed between the youth-leaders and comparison youth may be attributed to small sample size (25 youth-leaders, 16 comparison youth). This study was conducted as an exploratory approach to impact evaluation, as the youth-leader component was not designed to provide definitive evidence for a treatment effect, but to inform the design of larger and more comprehensive youth-led programs.
Another limitation is that while this study utilized several rigorous evaluation methods, additional measures of interest could have been included, such as additional measures of health behaviors such as assessment of physical activity and/or sedentary behavior (the current study only focused on dietary behaviors), and assessment of other psychosocial constructs grounded in the theoretical frameworks used to develop this intervention, such as role modeling and observational learning. Additionally, enhanced measures of the psychosocial factors included in this study (self-efficacy, behavioral intentions, and outcome expectations) could also be included, as a limitation of this study was that some of the included scales used had Cronbach’s alpha scores slightly below the ideal threshold,54 which may have precluded the ability to detect differences among groups and limited the interpretability of these findings. Finally, other factors of interest that could have been assessed include things such as community engagement/civic participation55, and mental/social health factors such as mental health screeners56, and social network analysis57. Despite these limitations in sample size and evaluation methods, this study provides valuable new insight to the perceived and actual impacts of youth-led interventions on the youth-leaders themselves.
Strengths of this study include the utilization of multiple methods of data collection and analysis. This study provides a novel, intensive analysis of a youth-led intervention conducted in a specific high-risk population (urban, African-American youth). The high-risk, nutritionally vulnerable nature of this study population highlights the importance of researching the best methods to address obesity-related behaviors in this Baltimore-based community. This study adds to the promising results seen from other research done on youth-led nutrition interventions. While much of the literature focuses on the impact of such interventions on program participants, this study assessed the impact on the youth-leaders themselves, using a novel multi-method analytical approach.
The results of this study have implications for both researchers and nutrition practitioners working in the field of obesity prevention. For researchers conducting youth-led obesity prevention interventions, this study provides evidence that measurement of intervention effects on youth-leaders themselves is an important component of overall intervention evaluation. For nutrition practitioners and public health program developers, this study provides evidence to support the incorporation of youth as partners in obesity prevention, due to both feasibility and co-benefits to both children and the youth-leaders. Inclusion of youth-leaders into programming could be done in multiple ways, including in the intervention development and delivery; in identifying and understanding health issues of interest to the population58; and/or empowering youth to engage in local policy development and advocacy efforts59. For example, youth-leaders could be invited to serve on a neighborhood-level or city-level youth advisory board to provide feedback on food policy strategies being considered at the local level (such as sugar sweetened beverage taxes, and food advertising restrictions), which have been shown to be successful and cost-effective 60
Another emerging area that youth-leaders could participate in would be social media interventions. Recent reviews articles indicate that incorporation of social media and other electronic platforms show promising results for enhancing nutrition-related outcomes in youth populations, however, many acknowledge that the technology often used in these studies is basic and dated (i.e., discussion boards and blogs)61,62. B’More Healthy Communities for Kids, the parent study to this youth-leader intervention, did include a novel and effective social media intervention component, where the youth leaders helped generate social media content related to the promotion of healthier eating, however, this component was targeted toward parents/caregivers rather than youth63,64. Involving youth-leaders in social media intervention delivery to youth participants may be a way to support the development of interventions using platforms that youth are comfortable with and actively engaging in, and further enhance intervention impact on both youth-leaders and youth participants.
The present analysis begins to assess important, additional aspects of impact of youth-led programs (i.e., impact on the youth-leaders), and in doing so brings us one step closer to achieving a viable and effective option for addressing childhood obesity in urban, African American communities. There is consensus in the literature that culturally tailored, multi-level, multi-component interventions that include policy components, similar to the BHCK study are the most successful and cost effective for addressing obesity and nutrition-related chronic diseases65,66. However multi-component, multi-level interventions that do not put an emphasis on comprehensive assessments and analyses of all components of the intervention, including multiple factors of youth-led interventions, such as the impact on youth participants, the youth-leaders, and members of both groups’ social networks, may be missing important outcomes.
Supplementary Material
Acknowledgements:
The authors would like to acknowledge to additional members of the B’More Healthy Communities for Kids (BHCK) research team who contributed to this work, as well as the youth-leaders who participated in the BHCK intervention.
Source of Funding: The project described was primarily supported by Grant Number U54HD070725 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD). The project is co-funded by the NICHD and the Office of Behavioral and Social Sciences Research (OBSSR). Additional funding for the youth-leader intervention was obtained from the Academy of Nutrition and Dietetics Champions for Healthy Kids, PepsiCo New Lifestyles Innovation Grants and NE- Regional Nutrition Education Center of Excellence. The funders had no role in the design, writing, or analysis of this article. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NICHD or OBSSR.
Footnotes
Institution at which work was conducted: Johns Hopkins Bloomberg School of Public Health, Global Obesity Prevention Center, Address: 615 N Wolfe Street, 21205, Baltimore City, Maryland
Conflict of Interest Statement: The authors declare that they have no conflict of interest..
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, et al. Trends in Obesity Prevalence Among Children and Adolescents in the United States, 1988–1994 Through 2013–2014. JAMA. 2016;315(21):2292–2299. doi: 10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wabitsch M, Moss A, Kromeyer-Hauschild K. Unexpected plateauing of childhood obesity rates in developed countries. BMC Med. 2014;12:17. doi: 10.1186/1741-7015-12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Robbins JM, Mallya G, Polansky M, Schwarz DF. Prevalence, disparities, and trends in obesity and severe obesity among students in the Philadelphia, Pennsylvania, school district, 2006–2010. Prev Chronic Dis. 2012;9:E145. doi: 10.5888/pcd9.120118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eagle TF, Sheetz A, Gurm R, Woodward AC, Kline-Rogers E, Leibowitz R et al. Understanding childhood obesity in America: linkages between household income, community resources, and children’s behaviors. Am Heart J. 2012;163(5):836–843. doi: 10.1016/j.ahj.2012.02.025. [DOI] [PubMed] [Google Scholar]
- 6.Kershaw KN, Pender AE. Racial/Ethnic Residential Segregation, Obesity, and Diabetes Mellitus. Curr Diab Rep. 2016;16(11):108. doi: 10.1007/s11892-016-0800-0. [DOI] [PubMed] [Google Scholar]
- 7.Wang Y, Wu Y, Wilson RF, Bleich S, Cheskin L, Weston C, et al. Childhood Obesity Prevention Programs: Comparative Effectiveness Review and Meta-Analysis. Comp Eff Rev. 2013;115. http://www.ncbi.nlm.nih.gov/books/NBK148737/.Accessed April 11, 2019. [PubMed] [Google Scholar]
- 8.Campbell R, Starkey F, Holliday J, Audrey S, Bloor M, Parry-Langdon N, et al. An informal school-based peer-led intervention for smoking prevention in adolescence (ASSIST): a cluster randomised trial. Lancet. 2008;371(9624):1595–1602. doi: 10.1016/S0140-6736(08)60692-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maticka-Tyndale E, Barnett JP. Peer-led interventions to reduce HIV risk of youth: a review. Eval Program Plann. 2010;33(2):98–112. doi: 10.1016/j.evalprogplan.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 10.Black MM, Hager ER, Le K, Anliker J, Arteaga SS, DiClemente C, et al. Challenge! Health promotion/obesity prevention mentorship model among urban, black adolescents. Pediatrics. 2010;126(2):280–288. doi: 10.1542/peds.2009-1832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bogart LM, Cowgill BO, Elliott MN, Klein DJ, Hawes-Dawson J, Uyeda K, et al. A randomized controlled trial of students for nutrition and eXercise: a community-based participatory research study. J Adolesc Health. 2014;55(3):415–422. doi: 10.1016/j.jadohealth.2014.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cawley J, Cisek-Gillman L, Roberts R, Cocotas C, Smith-Cook T, Bouchard M, et al. Effect of HealthCorps, a High School Peer Mentoring Program, on Youth Diet and Physical Activity. Childhood Obesity. 2011;7(5):364–371. doi: 10.1089/chi.2011.0022. [DOI] [Google Scholar]
- 13.French SA, Story M, Fulkerson JA, Hannan P. An environmental intervention to promote lower-fat food choices in secondary schools: outcomes of the TACOS Study. Am J Public Health. 2004;94(9):1507–1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lo E, Coles R, Humbert ML, Polowski J, Henry CJ, Whiting SJ. Beverage intake improvement by high school students in Saskatchewan, Canada. Nutr Res. 2008;28(3):144–150. doi: 10.1016/j.nutres.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 15.Siega-Riz AM, El Ghormli L, Mobley C, Gillis B, Stadler D, Hartstein J, et al. The effects of the HEALTHY study intervention on middle school student dietary intakes. Int J Behav Nutr Phys Act. 2011;8(1):7. doi: 10.1186/1479-5868-8-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stock S, Miranda C, Evans S, Plessis S, Ridley J, Yeh S, et al. Healthy Buddies: a novel, peer-led health promotion program for the prevention of obesity and eating disorders in children in elementary school. Pediatrics. 2007;120(4):e1059–68. doi: 10.1542/peds.2006-3003. [DOI] [PubMed] [Google Scholar]
- 17.Smith LH, Holloman C. Comparing the effects of teen mentors to adult teachers on child lifestyle behaviors and health outcomes in Appalachia. J Sch Nurs. 2013;29(5):386–396. doi: 10.1177/1059840512472708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bergmann L, Clifford D, Wolff C. Edutainment and teen modeling may spark interest in nutrition & physical activity in elementary school audiences. J Nutr Educ Behav. 2010;42(2):139–141. doi: 10.1016/j.jneb.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 19.Forneris T, Fries E, Meyer A, Buzzard M, Uguy S, Ramakrishnan R, et al. Results of a rural school-based peer-led intervention for youth: goals for health. J Sch Health. 2010;80(2):57–65. doi: 10.1111/j.1746-1561.2009.00466.x. [DOI] [PubMed] [Google Scholar]
- 20.Wilson DB, Jones RM, McClish D, Westerberg AL, Danish S. Fruit and vegetable intake among rural youth following a school-based randomized controlled trial. Prev Med (Baltim). 2012;54(2):150–156. doi: 10.1016/j.ypmed.2011.11.005. [DOI] [PubMed] [Google Scholar]
- 21.Jones S, Spence M, Hardin S, Clemente N, Schoch A. Youth Can! results of a pilot trial to improve the school food environment. J Nutr Educ Behav. 2011;43(4):284–287. doi: 10.1016/j.jneb.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 22.Yip C, Gates M, Gates A, Hanning RM. Peer-led nutrition education programs for school-aged youth: a systematic review of the literature. Health Educ Res. 2016;31(1):82–97. doi: 10.1093/her/cyv063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Linton LS, Edwards CC, Woodruff SI, Millstein RA, Moder C. Youth advocacy as a tool for environmental and policy changes that support physical activity and nutrition: an evaluation study in San Diego County. Prev Chronic Dis. 2014;11:E46. doi: 10.5888/pcd11.130321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bogart LM, Elliott MN, Uyeda K, Hawes-Dawson J, Klein DJ, Schuster MA. Preliminary healthy eating outcomes of SNaX, a pilot community-based intervention for adolescents. J Adolesc Health. 2011;48(2):196–202. doi: 10.1016/j.jadohealth.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lytle LA, Murray DM, Perry CL, Story M, Birnbaum AS, Kubik MY, et al. School-based approaches to affect adolescents’ diets: results from the TEENS study. Health Educ Behav. 2004;31(2):270–287. doi: 10.1177/1090198103260635. [DOI] [PubMed] [Google Scholar]
- 26.Smith LH. Piloting the use of teen mentors to promote a healthy diet and physical activity among children in Appalachia. J Spec Pediatr Nurs. 2011;16(1):16–26. doi: 10.1111/j.1744-6155.2010.00264.x. [DOI] [PubMed] [Google Scholar]
- 27.Story M, Lytle LA, Birnbaum AS, Perry CL. Peer-led, school-based nutrition education for young adolescents: feasibility and process evaluation of the TEENS study. J Sch Health. 2002;72(3):121–127. doi: 10.1111/j.1746-1561.2002.tb06529.x [DOI] [PubMed] [Google Scholar]
- 28.Ronsley R, Lee AS, Kuzeljevic B, Panagiotopoulos C. Healthy BuddiesTM reduces body mass index z-score and waist circumference in Aboriginal children living in remote coastal communities. J Sch Health. 2013;83(9):605–613. doi: 10.1111/josh.12072. [DOI] [PubMed] [Google Scholar]
- 29.Santos RG, Durksen A, Rabbanni R, Chanoine JP, Lamboo MA, Mayer T, et al. Effectiveness of Peer-Based Healthy Living Lesson Plans on Anthropometric Measures and Physical Activity in Elementary School Students: A Cluster Randomized Trial. JAMA Pediatr. 2014; 168(4):330–337. doi: 10.1001/jamapediatrics.2013.3688. [DOI] [PubMed] [Google Scholar]
- 30.Birnbaum AS, Lytle LA, Story M, Perry CL, Murray DM. Are Differences in Exposure to a Multicomponent School-Based Intervention Associated with Varying Dietary Outcomes in Adolescents? Heal Educ Behav. 2002;29(4):427–443. doi: 10.1177/109019810202900404. [DOI] [PubMed] [Google Scholar]
- 31.Shin A, Surkan PJ, Coutinho AJ, Suratkar SR, Campbell RK, Rowan M, et al. Impact of Baltimore Healthy Eating Zones: An Environmental Intervention to Improve Diet Among African American Youth. Heal Educ Behav. 2015;42(1 Suppl):97S–105S. doi: 10.1177/1090198115571362. [DOI] [PubMed] [Google Scholar]
- 32.Black MM, Arteaga SS, Sanders J, Hager E, Anliker J, Gittelsohn J, et al. College mentors: a view from the inside of an intervention to promote health behaviors and prevent obesity among low-income, urban, African American adolescents. Health Promot Pract. 2012;13(2):238–244. doi: 10.1177/1524839910385899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hamdan S, Story M, French SA, Fulkerson JA, Nelson H. Perceptions of adolescents involved in promoting lower-fat foods in schools: associations with level of involvement. J Am Diet Assoc. 2005;105(2):247–251. doi: 10.1016/j.jada.2004.11.030. [DOI] [PubMed] [Google Scholar]
- 34.Gittelsohn J, Anderson Steeves E, Mui Y, Kharmats AY, Hopkins LC, Dennis D. B’More Healthy Communities for Kids: design of a multi-level intervention for obesity prevention for low-income African American children. BMC Public Health. 2014;14:942. doi: 10.1186/1471-2458-14-942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice-Hall; 1977. [Google Scholar]
- 36.Bronfenbrenner U. The Ecology of Human Development: Experiements by Nature and by Design .Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- 37.Rogers EM. Diffusion of Innovations. 5th ed. New York: Simon and Schuster; 2003. [Google Scholar]
- 38.Story M, Neumark-Sztainer D, French S. Individual and environmental influences on adolescent eating behaviors. J Am Diet Assoc. 2002;102(3 Suppl):S40–51. doi: 10.1016/S0002-8223(02)90421-9 [DOI] [PubMed] [Google Scholar]
- 39.Forsyth R, Purcell C, Barry S, Simpson S, Hunter R, McDaid L, et al. Peer-led intervention to prevent and reduce STI transmission and improve sexual health in secondary schools (STASH): protocol for a feasibility study. Pilot feasibility Stud. 2018;4:180. doi: 10.1186/s40814-018-0354-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Trude ACB, Anderson Steeves E, Shipley C, Surkan P, Sato PM, Estep T, et al. A Youth-Leader Program in Baltimore City Recreation Centers: Lessons Learned and Applications. Health Promot Pract. 2017;19(1):75–85. doi: 10.1177/1524839917728048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sato PM, Steeves EA, Carnell S, Checkin LJ, Trude AC, Shipley C, et al. A youth mentor-led nutritional intervention in urban recreation centers: a promising strategy for childhood obesity prevention in low-income neighborhoods. Health Educ Res. 2016;31(2):195–206. doi: 10.1093/her/cyw011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1985. [Google Scholar]
- 43.Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 44.Fitzgerald A, Heary C, Kelly C, Nixon E, Shevlin M. Self-efficacy for healthy eating and peer support for unhealthy eating are associated with adolescents’ food intake patterns. Appetite. 2013;63:48–58. doi: 10.1016/j.appet.2012.12.011. [DOI] [PubMed] [Google Scholar]
- 45.Jenkinson KA, Naughton G, Benson AC. The GLAMA (Girls! Lead! Achieve! Mentor! Activate!) physical activity and peer leadership intervention pilot project: a process evaluation using the RE-AIM framework. BMC Public Health. 2012;12(1):55. doi: 10.1186/1471-2458-12-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kramer RF, Coutinho AJ, Vaeth E, Christiansen K, Suratkar S, Gittelsohn J. Healthier home food preparation methods and youth and caregiver psychosocial factors are associated with lower BMI in African American youth. J Nutr. 2012;142(5):948–954. doi: 10.3945/jn.111.156380. [DOI] [PubMed] [Google Scholar]
- 47.Sattler M, Hopkins L, Anderson Steeves E, Cristello A, McCloskey M, Gittelsohn J, et al. Characteristics of Youth Food Preparation in Low-Income, African American Homes: Associations with Healthy Eating Index Scores. Ecol Food Nutr. 2015:54(4):380–96. doi: 10.1080/03670244.2014.1001982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cullen KW, Watson K, Zakeri I. Relative reliability and validity of the Block Kids Questionnaire among youth aged 10 to 17 years. J Am Diet Assoc. 2008;108(5):862–866. doi: 10.1016/j.jada.2008.02.015. [DOI] [PubMed] [Google Scholar]
- 49.Villa J. Simplifying the Estimation of Difference in Differences Treatment Effects with Stata. Manchester, UK; 2012. [Google Scholar]
- 50.Willett WC, Howe GR, Kushi LH. Adjustment for total energy intake in epidemiologic studies. Am J Clin Nutr. 1997;65(4 Suppl):1220S–1228S. doi: 10.1093/ajcn/65.4.1220S [DOI] [PubMed] [Google Scholar]
- 51.Armitage CJ, Conner M. Efficacy of the Theory of Planned Behaviour: a meta-analytic review. Br J Soc Psychol. 2001;40(Pt 4):471–499. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- 52.Centers for Disease Control and Prevention. Physical Activity Surveillance Systems. https://www.cdc.gov/physicalactivity/data/surveillance.htm. Published 2017. Accessed November 2, 2018.
- 53.Clemes SA, Biddle SJH. The use of pedometers for monitoring physical activity in children and adolescents: measurement considerations. J Phys Act Health. 2013;10(2):249–262. [DOI] [PubMed] [Google Scholar]
- 54.Tavakol M, Dennick R. Making sense of Cronbach’s alpha. Int J Med Educ. 2011;2:53–55. doi: 10.5116/ijme.4dfb.8dfd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Millstein RA, Woodruff SI, Linton LS, Edwards CC, Sallis JF. Development of measures to evaluate youth advocacy for obesity prevention. Int J Behav Nutr Phys Act. 2016;13:84. doi: 10.1186/s12966-016-0410-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl Psychol Assess. 1977;1(3):385–4-1. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 57.de la Haye K, Robins G, Mohr P, Wilson C. Obesity-related behaviors in adolescent friendship networks. Soc Networks. 2010;32(3):161–167. doi: 10.1016/j.socnet.2009.09.001. [DOI] [Google Scholar]
- 58.Johnson KA, Steeves EA, Gewanter ZR, Gittelsohn J. Food in my neighborhood : Exploring the food environment through photovoice with urban, African American youth. J Hunger Environ Nutr. 2016;12(3):394–405. doi: 10.1080/19320248.2016.1227751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Millstein RA, Sallis JF. Youth advocacy for obesity prevention: the next wave of social change for health. Transl Behav Med. 2011;1(3):497–505. doi: 10.1007/s13142-011-0060-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gortmaker SL, Long MW, Resch SC, Ward ZJ, Cradock AL, Barrett JL, et al. Cost Effectiveness of Childhood Obesity Interventions: Evidence and Methods for CHOICES. Am J Prev Med. 2015;49(1):102–111. doi: 10.1016/j.amepre.2015.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hsu MSH, Rouf A, Allman-Farinelli M. Effectiveness and Behavioral Mechanisms of Social Media Interventions for Positive Nutrition Behaviors in Adolescents: A Systematic Review. J Adolesc Health. 2018;63(5):531–545. doi: 10.1016/j.jadohealth.2018.06.009. [DOI] [PubMed] [Google Scholar]
- 62.Chau MM, Burgermaster M, Mamykina L. The use of social media in nutrition interventions for adolescents and young adults—A systematic review. Int J Med Inform. 2018;120:77–91. doi: 10.1016/j.ijmedinf.2018.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Trude AC, Surkan PJ, Anderson Steeves E, Pollack Porter K, Gittelsohn J. The impact of a multilevel childhood obesity prevention intervention on healthful food acquisition, preparation, and fruit and vegetable consumption on African-American adult caregivers. Public Health Nutr. 2019;22(7):1300–1315. doi: 10.1017/S1368980018003038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Loh IH, Schwendler T, Trude ACB, Anderson Steeves ET, Checskin LJ, Lange S, et al. Implementation of Text-Messaging and Social Media Strategies in a Multilevel Childhood Obesity Prevention Intervention: Process Evaluation Results. Inquiry. 2018; 55:1–9. doi: 10.1177/0046958018779189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lobstein T, Jackson-Leach R, Moodie ML, Hall KD, Gortmaker SL, Swinburn BA, et al. Child and adolescent obesity: part of a bigger picture. Lancet. 2015; 385(9986):2510–20. doi: 10.1016/S0140-6736(14)61746-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Roberto CA, Swinburn B, Hawkes C, Huang TT, Costa SA, Ashe M, et al. Patchy progress on obesity prevention: emerging examples, entrenched barriers, and new thinking. Lancet. 2015;385(9985)2400–9. doi: 10.1016/S0140-6736(14)61744-X. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.