In the last century, children in middle- to high-income countries such as the U.S. adopted a diet that often includes highly processed foods and low intake of fresh fruits, vegetables, and fiber but high intake of saturated fats and refined sugars. Such changes in dietary habits over the last few decades may partly explain the “asthma epidemic” in industrialized nations.
To better understand the impact of diet on asthma, most researchers have focused on studying the effects of individual nutrients or vitamins, with the ultimate goal of recommending a supplement that is easy to administer (e.g., a pill). However, results from experimental studies linking specific dietary components to altered immune responses or airway inflammation have rarely translated into consistent findings from human studies, and none can be currently recommended as a preventive or therapeutic agent for asthma based on consistent results from randomized clinical trials.
As an example of a single-nutrient focus, prenatal supplementation with folic acid (a methyl donor) was previously postulated as a key contributor to the “asthma epidemic,” partly based on a murine model in which administration of methyl donors to pregnant mice led to allergic airway disease in their offspring, perhaps through DNA methylation of genes regulating Th1 and Th2 immunity (1). However, a subsequent body of evidence from observational human studies is not consistent with moderate or strong effects of folate on asthma or allergies in children (2). Similarly, experimental data showed that vitamin D has antioxidant, immune-modulatory, and anti-inflammatory effects, including induction of Tregs and production of IL-10, reduced Th2 and Th17 responses, and upregulation of interferon-mediated antiviral pathways and antimicrobial peptides. Moreover, findings from observational human studies suggested that low intake of vitamin D during pregnancy could lead to childhood asthma, and that vitamin D levels below 30 ng/ml may increase the risk of severe asthma exacerbations in children (3). However, a randomized clinical trial showed that prenatal vitamin D supplementation, while having effects on wheezing by age 3 years, did not prevent asthma by age 6 years (4). Moreover, a recent randomized clinical trial showed no significant effects of vitamin D supplementation on preventing severe exacerbations in school-aged children with asthma and vitamin D levels below 30 ng/ml (3). Although beneficial effects of vitamin D supplementation in mothers or children with very low vitamin D levels require further study, such supplementation is unlikely to benefit individuals with a vitamin D level equal or greater than 20 ng/ml. Other single nutrients or dietary components for which there is insufficient evidence to make clinical recommendations for asthma management include, but are not limited to, omega-3 and omega-6 polyunsaturated fatty acids, and fiber (5).
Given a low yield from studying specific nutrients or vitamins, recent efforts have focused on studying well-validated indices that assess the quality or properties of the whole diet, as nutrients or vitamins could have stronger effects on health when acting additively or synergistically. For example, a cross-sectional U.S. study of 8,175 children and 22,294 adults showed that a higher Energy-adjusted Dietary Inflammatory Index (E-DII, indicating a more pro-inflammatory diet) was associated with current wheeze in adults and in children with an elevated FeNO (fractional exhaled nitric oxide), as well as with reduced FEV1 (forced expiratory volume in 1 second) and FVC (forced vital capacity) in adults without asthma (6). Moreover, a cross-sectional U.S. study including 12,687 Hispanic adults showed that a higher E-DII was associated with increased odds of current asthma, lower FEV1 and lower FVC (7). More recently, a birth cohort study of 862 Irish mother-child pairs showed that a higher maternal E-DII in the first trimester of pregnancy was associated with higher risk of asthma (defined by a physician’s diagnosis or parental report) in their offspring, who were followed up to age 9 years (8). Findings from these studies, though promising, could be due to residual confounding by factors correlated with a pro-inflammatory diet (e.g., an unhealthy lifestyle including tobacco use and no regular exercise, which could worsen asthma symptoms) and thus need to be confirmed in longitudinal studies with high subject retention and a comprehensive assessment of asthma and potential confounders.
Other studies of childhood asthma have focused on a particular diet (e.g., “Mediterranean”, characterized by high content of fruits, vegetables, unsaturated fats, and whole-grains but low intake of saturated fats and red meat) or on analyzing dietary intake of fruits and vegetables. Such studies have shown an inverse association between a “Mediterranean diet” or a high intake of fruits and vegetables and asthma or asthma symptoms, including reduced risk of asthma or wheeze, better asthma control, and improved lung function during childhood (9). Further support for beneficial effects of a healthy diet on asthma is provided by a six-month pilot randomized clinical trial in 90 adults, which showed that a diet rich in fruits, vegetables, and grains but low in saturated fats and sweetened beverages was associated with improved asthma control (10).
Diet could help prevent or improve asthma through direct and indirect effects. With regard to direct effects, a healthy maternal diet during pregnancy could positively impact fetal lung and immune system development, thus reducing the risk of childhood asthma. Moreover, the antioxidant properties of fruits, vegetables, and whole grains could reduce systemic and airway inflammation in subjects with asthma (2)(5). Conversely, a pro-inflammatory diet with high intake of saturated fats, red meat, and refined sugars but low intake of fruits and vegetables may lead to increased production of reactive oxygen species, enhanced Th2 immune responses, and activation of factor NF-kB (5). With regard to indirect effects, a “Western diet” with high intake of processed foods, sweetened beverages, and saturated fats can lead to weight gain and obesity, a risk factor for asthma. Moreover, such diet can alter the gut microbiota, leading to reduced production of short-chain fatty acids, which have been shown to have immune-regulatory and anti-inflammatory effects (5). In addition, there is preliminary evidence of potential protective effects of a Mediterranean diet or a diet rich in fruits and vegetables against the detrimental effects of pollutants such as ozone on asthma.
In summary, current evidence suggests that healthy dietary patterns emphasizing intake of fruits and vegetables, whole grains, fiber, and unsaturated fats may help prevent and treat asthma. Although challenging, well-designed clinical trials of “full dietary interventions” are needed to understand both the mechanisms and effects of such interventions on asthma and asthma control. Because of known effects on overall health, a healthy and balanced diet should be recommended for all children and adults with asthma.
Supplementary Material
Figure 1.
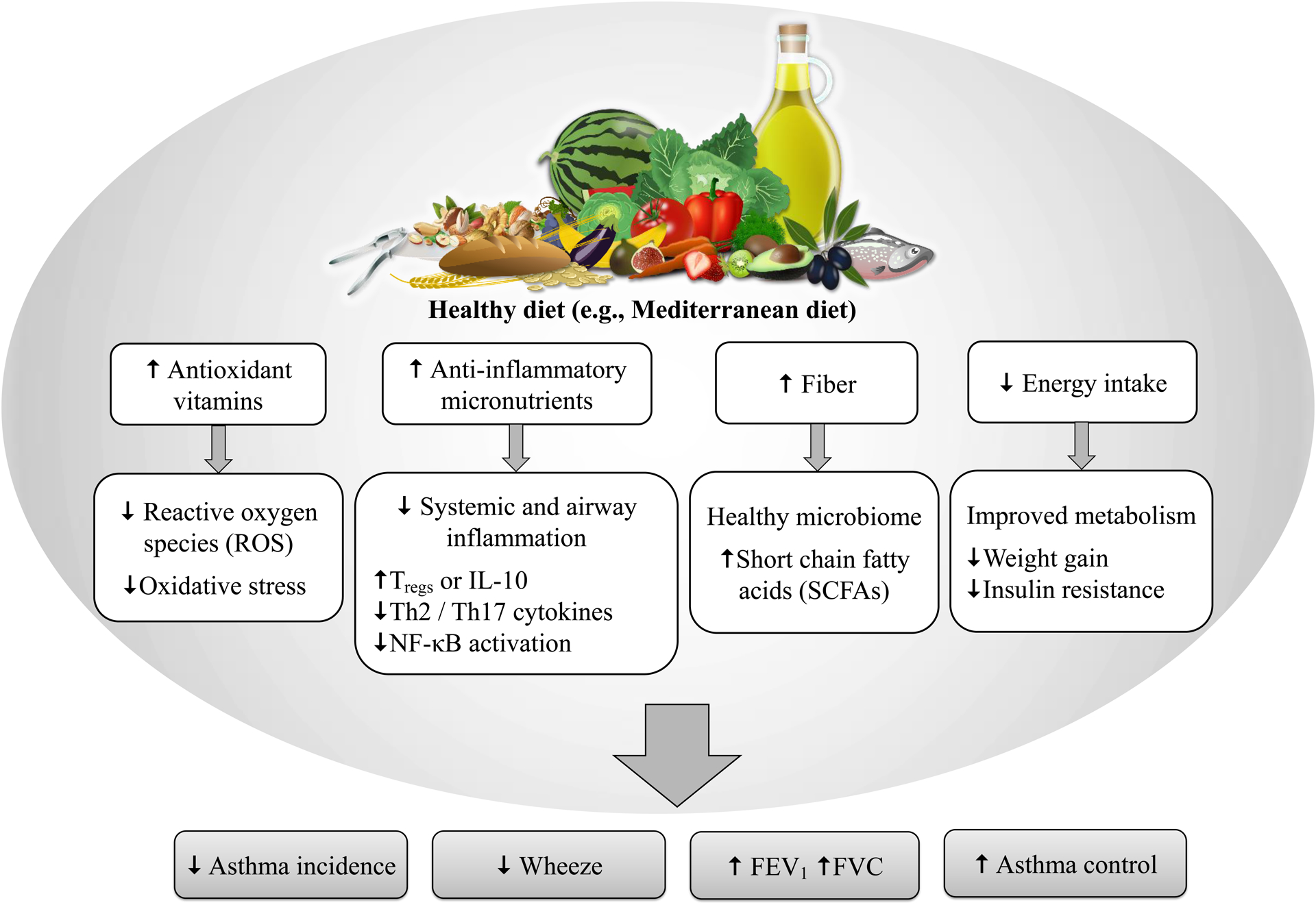
Potential beneficial effects of a healthy diet on asthma and lung function.
Declaration of funding and conflicts of interest:
This work was supported by grants HL117191, HL119952, and MD011764 from the U.S. National Institutes of Health (NIH). Dr. Celedón has received research materials from GSK and Merck (inhaled steroids) and Pharmavite (vitamin D and placebo capsules), to provide medications free of cost to participants in NIH-funded studies, unrelated to this work. The other authors have no conflicts of interest to declare.
REFERENCES
- 1.Hollingsworth JW, Maruoka S, Boon K, Garantziotis S, Li Z, Tomfohr J, et al. In utero supplementation with methyl donors enhances allergic airway disease in mice. J Clin Invest 2008; 118: 3462–3469. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 2.Han YY, Blatter J, Brehm JM, Forno E, Litonjua AA, Celedon JC. Diet and asthma: vitamins and methyl donors. Lancet Respir Med 2013; 1: 813–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Forno E, Bacharier LB, Phipatanakul W, Guilbert TW, Cabana MD, Ross K, et al. Effect of Vitamin D3 Supplementation on Severe Asthma Exacerbations in Children With Asthma and Low Vitamin D Levels: The VDKA Randomized Clinical Trial. JAMA 2020; 324: 752–760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Litonjua AA, Carey VJ, Laranjo N, Stubbs BJ, Mirzakhani H, O’Connor GT, et al. Six-Year Follow-up of a Trial of Antenatal Vitamin D for Asthma Reduction. N Engl J Med 2020; 382: 525–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alwarith J, Kahleova H, Crosby L, Brooks A, Brandon L, Levin SM, et al. The role of nutrition in asthma prevention and treatment. Nutr Rev 2020; 78: 928–938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Han YY, Forno E, Shivappa N, Wirth MD, Hebert JR, Celedon JC. The Dietary Inflammatory Index and Current Wheeze Among Children and Adults in the United States. J Allergy Clin Immunol Pract 2018; 6: 834–841 e832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Han YY, Jerschow E, Forno E, Hua S, Mossavar-Rahmani Y, Perreira KM, et al. Dietary Patterns, Asthma, and Lung Function in the Hispanic Community Health Study/Study of Latinos. Ann Am Thorac Soc 2020; 17: 293–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen LW, Lyons B, Navarro P, Shivappa N, Mehegan J, Murrin CM, et al. Maternal dietary inflammatory potential and quality are associated with offspring asthma risk over 10-year follow-up: the Lifeways Cross-Generation Cohort Study. Am J Clin Nutr. 2020;111:440–7. [DOI] [PubMed] [Google Scholar]
- 9.Castro-Rodriguez JA, Forno E, Rodriguez-Martinez CE, Celedon JC. Risk and Protective Factors for Childhood Asthma: What Is the Evidence? J Allergy Clin Immunol Pract 2016; 4: 1111–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ma J, Strub P, Lv N, Xiao L, Camargo CA Jr., Buist AS, et al. Pilot randomised trial of a healthy eating behavioural intervention in uncontrolled asthma. Eur Respir J 2016; 47: 122–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


