Abstract
Objective:
Delaying cataract surgery is associated with an increased risk of falls, but it is unknown whether routine preoperative testing delays cataract surgery long enough to cause clinical harm. We sought to determine whether the use of routine preoperative testing leads to harm in the form of delayed surgery and falls in Medicare beneficiaries awaiting cataract surgery.
Design:
Retrospective observational cohort study using 2006-2014 Medicare claims
Participants:
Medicare beneficiaries age 66+ with a CPT claim for ocular biometry
Methods:
We measured the mean and median number of days between ocular biometry and cataract surgery, calculated the proportion of patients waiting >30 days or >90 days for surgery, and determined the odds of having a fall within 90 days of biometry among patients of high-testing physicians (testing performed in ≥75% of their patients) compared to patients of low-testing physicians. We estimated the number of days of delay attributable to high-testing physicians relative to other factors that may determine surgical scheduling.
Main Outcome Measures:
Incidence of falls occurring between biometry and surgery, odds of falling within 90 days of biometry, and estimated delay in days associated with physician testing behavior .
Results:
Of 248,345 beneficiaries, 16.4% were patients of high-testing physicians. More patients of high-testing physicians waited >30 days and >90 days to have cataract surgery (31.4% and 8.2% versus 25.0% and 5.5%, respectively, p<0.0001 for both). Falls before cataract surgery in patients of high-testing physicians increased by 43% within the 90 days following ocular biometry (1.0% vs 0.7%, p<0.0001). The adjusted odds ratio of falling within 90 days of biometry in patients of high-testing physicians versus low-testing physicians was 1.10 (95% CI 1.03-1.19, p=0.008) After adjusting for surgical wait time, the odds ratio decreased to 1.07 (95% CI 1.00-1.15, p=0.06). The delay associated with having a high-testing physician was approximately 8 days (estimate 7.97, 95% CI 6.40-9.55, p<0.0001). Other factors associated with delayed surgery included patient race (non-white), northeast geographic region, ophthalmologist age≤40, and low surgical volume.
Conclusions:
Overuse of routine preoperative medical testing by high-testing physicians is associated with delayed surgery and increased falls in cataract patients awaiting surgery.
PRECIS
Patients of high-testing physicians waited longer for cataract surgery and had 1.10 higher odds of falling while awaiting surgery after adjusting for age, sex, race, and health status.
Over 3.7 million cataract surgeries are performed annually in the United States,1 and approximately 80% of the patients undergoing cataract surgery are covered by Medicare.2 The two key components of modern cataract surgery—the surgical extraction of the clouded lens and the simultaneous correction of any baseline refractive error—dramatically improves patients’ postoperative visual acuity as well as their ability to perform activities of daily living.3-5 More importantly, cataract surgery has been shown to reduce the incidence of significant harms in cataract patients who undergo the procedure. Examples of the harms avoided by undergoing timely cataract surgery include a halving of the rate of motor vehicle accidents during a multiyear follow-up period compared to patients with cataract disease who did not have surgery;3 a reduction in the risk of hip fracture during the first 12 months after surgery (adjusted odds ratio of 0.84 compared to patients with a cataract diagnosis who did not have cataract surgery);6 and a 34% decrease in the fall rate of patients who had cataract surgery within 6 weeks versus patients who waited at least 6 months for the procedure.7 In light of these data, the vast literature on the safety of cataract surgery, and its efficacy in correcting the vision loss associated with senile cataract, it is generally recommended that surgical delays be avoided.4,7
According to clinical guidelines, routine preoperative medical testing is not necessary in advance of cataract surgery8-10 because it neither decreases the incidence of perioperative adverse events nor improves cataract surgery outcomes.11,12 However, testing still occurs frequently in anticipation of this low-risk procedure.13-15 In 2011, 53% of Medicare beneficiaries underwent at least one routine preoperative test within 30 days before their first cataract surgery.14 This finding that approximately half of Medicare cataract surgery patients were undergoing routine preoperative testing was unchanged from a similar study that reviewed Medicare claims from the late-1980’s, before current guidelines were established.13 If a patient undergoes unnecessary testing, even if no abnormality is found, surgery is delayed due to the time it takes to undergo testing and await the results of those tests. Since cataract surgery is usually indicated at the point that the disease impacts vision enough to compromise activities of daily living, delays in surgical scheduling—arising from unnecessary preoperative testing or for other reasons—prolong the period during which these patients with poor vision are at an increased risk of falls and the serious injuries (such as hip fracture) that can result.3-7 To our knowledge, no study has evaluated the impact of routine preoperative testing on the risk of falling in cataract patients awaiting surgery.
Our prior work showed that the strongest predictor of which patients undergo routine preoperative testing is the identity of the ophthalmologist, which we used as a proxy for the group of physicians managing the preoperative medical work up.14 Individual physician practice patterns vary in that some physicians always order routine preoperative testing, and others rarely do.14 We hypothesized that patients of physicians who frequently order preoperative tests (“high-testing physicians”) are more likely to experience delayed surgery and fall-related injuries compared to patients of physicians who do not (“low-testing physicians”). Using a 5% sample of Medicare claims from 2006 to 2014, we sought to determine whether a physician’s decision to order routine preoperative tests before cataract surgery caused harm to patients in the form of surgical delay and fall-related injuries while awaiting surgery. To accomplish this, we measured the time between ocular biometry (a diagnostic procedure performed in cataract patients when the ophthalmologist has made the decision to operate)16,17 and cataract surgery.15 We determined whether patients of high-testing physicians had a longer time interval between biometry and surgery than patients of low-testing physicians. We then examined whether patients of high-testing physicians had a higher risk of fall in the 90 days after ocular biometry.
METHODS
This study was approved by the University of California, San Francisco and the San Francisco Veterans Affairs Medical Center (IRB#1415035).
Data source
We obtained research identifiable files from the VA Information Resource Center for a 5% sample of Medicare beneficiaries. For each beneficiary, we obtained Outpatient, Carrier, MedPAR, and Master Beneficiary Summary files representing all claims from January 1, 2006 through December 31, 2014.
Study cohort
We identified Medicare beneficiaries with a claim for ocular biometry using CPT18 codes (76516, 76519, 92136) between 2007-2013. We included patients aged 66+ who were enrolled in the Medicare fee-for-service program, without a concurrent HMO plan, and had at least 12 months of eligibility before and after their initial biometry claim. We excluded patients with CPT codes or ICD-9-CM19 diagnosis codes indicating that they had already had cataract surgery between 2006 and their first biometry claim (66982-66984; V43.1, V45.61, 379.31). In patients with multiple biometry claims, we assumed that the first claim signaled the earliest indication that an ophthalmologist had planned to schedule cataract surgery.
Index surgery
We defined each beneficiary’s cataract surgery date as the first date of a claim submitted by an ophthalmologist for routine cataract surgery (CPT codes 66982-66984) appearing after the first biometry claim. Only cataract surgery on the first eye (the “index surgery”) was included for each patient.
Baseline characteristics
For each patient, we examined characteristics including age, sex, race, and health status using the Quan modification of the Charlson Comorbidity Index.20
Definition of high-testing physician
To assess physician preoperative testing behavior, we assigned the operating ophthalmologist to represent the group of physicians (e.g., the ophthalmologist, primary care physician, and anesthesiologist) responsible for managing the patient’s preoperative evaluation.14 Using only ophthalmologists who performed ≥10 cataract surgeries between 2007-2013, we stratified physicians into two groups. Ophthalmologists who carried out routine preoperative testing in ≥75% of their patients in the 30 days before surgery were categorized as “high-testing physicians.” All other ophthalmologists were designated as “low-testing physicians.” The preoperative tests used to stratify ophthalmologists are listed in eTable 1 (available at http://www.aaojournal.org).
Definition of falls and fall-related injuries
We applied the 4-step fall algorithm described by Kim et al. to identify falls and fall-related injuries.21,22 Briefly, the algorithm uses Medicare claims to improve the ability to detect unique fall episodes among Medicare patients by hierarchically organizing different types of claims submitted for a range of fall-related injuries into distinct fall events. The claims we reviewed to identify falls included the Medicare MedPAR, Outpatient and Carrier Files, which the authors demonstrated were adequate to identify the vast majority of fall episodes that occurred among Medicare patients.22 Fall-related injuries were grouped into the following broad categories: head injury, hip fracture, other fracture, and joint dislocation. Patients who had more than one type of injury were assigned to the injury group with the highest severity.
Statistical analysis
Statistical analyses were performed using SAS version 9.3 (SAS Institute Inc, Cary, NC).
Descriptive statistics were used to describe the baseline characteristics of all patients who had a biometry claim during the study period, as well as patients stratified by physician testing behavior. Chi-squared tests were used to assess differences in categorical variables, and Student’s t-tests were used for continuous variables. We measured the number of days between a patient’s first biometry claim and index cataract surgery claim. Patients whose cataract surgery occurred more than 360 days after biometry or who did not have a surgery claim following biometry were assigned an interval of 360 days. We determined the mean and median number of days between biometry and surgery and the percent of patients having cataract surgery within 30 days, 31-60 days, 61-90 days and greater than 90 days of biometry. We calculated the incidence of having a fall within 90 days after the biometry claim as well as the incidence of falls that occurred after biometry but prior to the date of surgery. We described the incidence of fall-related injuries grouped in order of decreasing severity as follows: head injury, hip fracture, other fracture, and joint dislocation. To determine the association of routine preoperative testing and falls in patients during the 90 days following ocular biometry, we created a logistic regression model to account for patient characteristics, physician preoperative testing behavior, and timing of surgery in relation to ocular biometry. To confirm that the association of routine preoperative testing and falls while awaiting surgery was not a reflection of other underlying differences between patients of high-testing and low-testing physicians, we created a second multivariate logistic regression model to assess whether having a high-testing physician was associated with an increased risk of falls in the 360 days preceding biometry. Finally, we created a multiple linear regression model to determine how physician testing behavior might impact the timing of surgery in the context of other factors that might influence surgical scheduling. Instead of falls, our primary outcome of interest in this model was the number of days between biometry and surgery. For this model only, patients were analyzed using the actual number of days that elapsed between biometry and surgery, while patients who did not have a surgery claim following biometry were assigned an interval of 365 days.
RESULTS
We identified 248,345 patients meeting inclusion criteria; 40,829 (16.4%) were patients of high-testing physicians (n=1,513), while 207,516 (83.6%) were patients of low-testing physicians (n=5,445) (Table 1). Patients of high-testing physicians were slightly older, more likely to be female, non-white, and have poorer health status (p<0.0001 for all), although the vast majority of patients had a Charlson score of 0 or 1 (72.0% vs 74.9% of low-testing physicians, respectively). The mean and median number of days between biometry and surgery in patients of high-testing physicians was 54.3 days and 21.0 days, respectively, compared to 41.2 days and 16.0 days in patients of low-testing physicians.
Table 1:
| All patients (n=248,345) |
Patients of low- testing physicians (n=207,516) |
Patients of high- testing physicians (n=40,829) |
p-value | |
|---|---|---|---|---|
| Age | <0.0001 | |||
| 66-70 | 52,166 (21.0%) | 44,711 (21.5%) | 7,455 (18.3%) | |
| 71-75 | 66,884 (26.9%) | 56,657 (27.3%) | 10,227 (25.1%) | |
| 76-80 | 63,601 (25.6%) | 52,974 (25.5%) | 10,627 (26.0%) | |
| 80+ | 65,657 (26.4%) | 53,141 (25.6%) | 12,516 (30.7%) | |
| Sex | <0.0001 | |||
| Male | 89,292 (36.0%) | 75,087 (36.2%) | 14,205 (34.8%) | |
| Female | 159,053 (64.0%) | 132,429 (63.8%) | 26,624 (65.2%) | |
| Ethnicity | <0.0001 | |||
| White | 219,521 (88.4%) | 184,680 (89.0%) | 34,841 (85.3%) | |
| Black | 11,927 (4.8%) | 9,731 (4.7%) | 2,196 (5.4%) | |
| Other | 16,897 (6.8%) | 13,105 (6.3%) | 3,792 (9.3%) | |
| Charlson comorbidity index | <0.0001 | |||
| 0-1 | 184,935 (74.5%) | 155,532 (74.9%) | 29,403 (72.0%) | |
| 2 | 27,460 (11.1%) | 22,627 (10.9%) | 4,833 (11.8%) | |
| 3+ | 35,950 (14.5%) | 29,357 (14.1%) | 6,593 (16.1%) | |
| Time between biometry and surgery | ||||
| Mean +/− SD (in days) | 43.3 +/−80.9 | 41.1 +/−78.4 | 54.3 +/−92.2 | <0.0001 |
| Median (in days) | 17 | 16 | 21 | |
| <30 days | 176,538 (71.1%) | 150,147 (72.4%) | 26,391 (64.6%) | <0.0001 |
| 31-60 days | 39,637 (16.0%) | 32,251 (15.5%) | 7,386 (18.1%) | |
| 61-90 days | 10,305 (4.1%) | 8,230 (4.0%) | 2,075 (5.1%) | |
| >90 days | 21,865 (8.8%) | 16,918 (8.2%) | 4,977 (12.2%) |
To account for outliers, patients whose claim for surgery was more than 360 days after biometry (n=5,096) or who did not have a claim for surgery within 360 days of biometry (n=7,108) were assigned as having surgery at 360 days.
All physicians (n=6,958); high-testing physicians (n=1,513); low-testing physicians (n=5,445)
Fewer patients of high-testing physicians underwent surgery within 30 days of biometry compared to patients of low-testing physicians (64.6% vs 72.4%, p<0.0001, Figure 1). Correspondingly, more patients of high-testing physicians waited longer than 30 days (31.4% vs 25.0%) and 90 days (8.2% vs 5.5%) after biometry to undergo surgery. Approximately 4.0% of patients of high-testing physicians did not have any claim for cataract surgery during the study period compared to 2.6% of patients of low-testing physicians (p<0.0001 for all).
Figure 1:
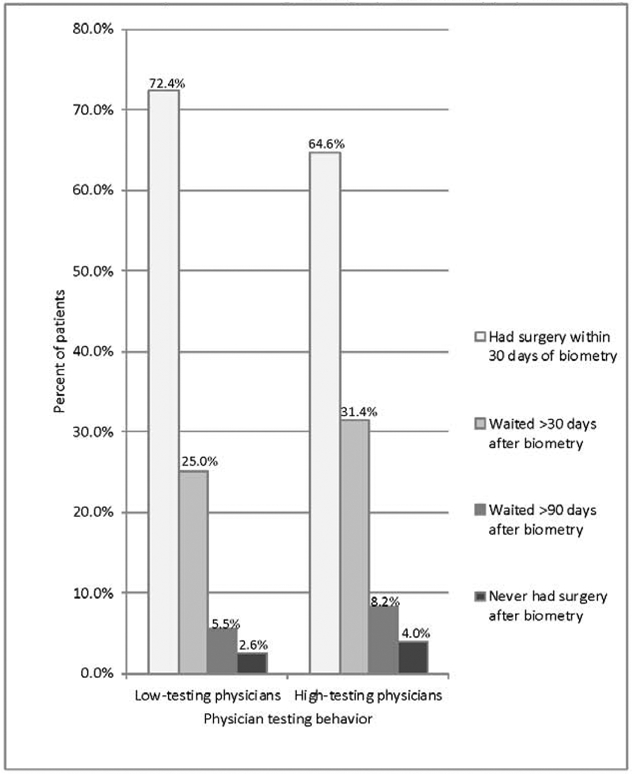
Percent of patients waiting for surgery, stratified by physician testing behavior
When we assessed the incidence of falls stratified by physician testing behavior, we found that 2.2% of patients of high-testing physicians experienced at least one fall within 90 days after biometry, compared to 2.0% of patients of low-testing physicians, regardless of the timing of cataract surgery (p=0.0002, Figure 2a). In other words, there was a 10% increase in fall events in patients of high-testing physicians in the 90 days following ocular biometry. Fall-related injuries were also more common among patients of high-testing physicians during this period, including head injury (0.07% vs 0.06%), hip fracture (0.33% vs 0.27%), other fracture (1.4% vs 1.2%), and joint dislocation (0.5% vs 0.4%, p<0.003 across all injury categories).
Figure 2a. Falls and fall-related injuries within 90 days of biometry, stratified by physician testing behavior1,2.
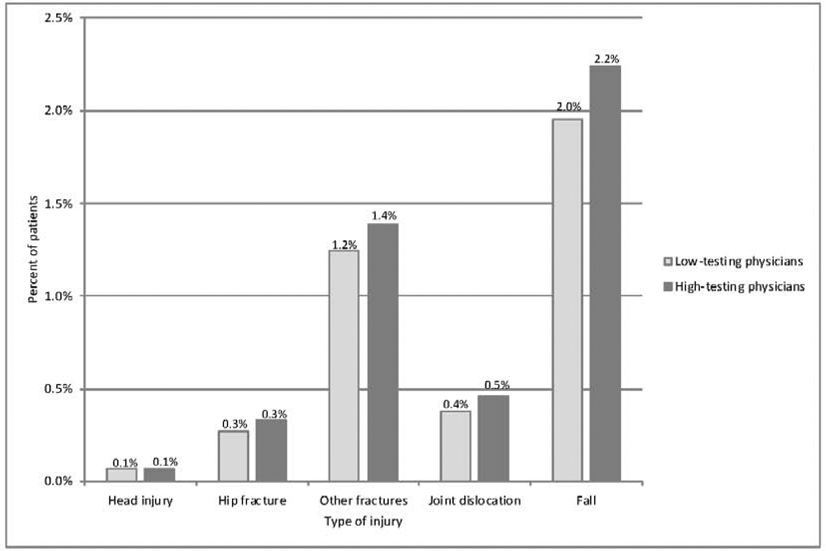
1) Falls in Figure 2a occurred before or after surgery, within 90 days of biometry.
2) n=40,829 and 207,516 for patients of high-testing physicians and low-testing physicians, respectively.
When we focused on falls that occurred before cataract surgery was performed (still within 90 days after biometry), there was a 43% increase in fall events in patients of high-testing physicians (1.0% vs 0.7%, p<0.0001, Figure 2b). The overall incidence of fall-related injuries occurring before cataract surgery was lower than the incidence of injuries occurring during the full 90-day period following biometry. However, with the exception of head injury (0.02% vs 0.02%), the difference in the incidence of fall-related injuries between the two groups remained consistent and statistically significant (p<0.0001 across all injury categories).
Figure 2b. Falls and fall-related injuries within 90 days of biometry that occurred prior to cataract surgery, stratified by physician testing behavior1,2.
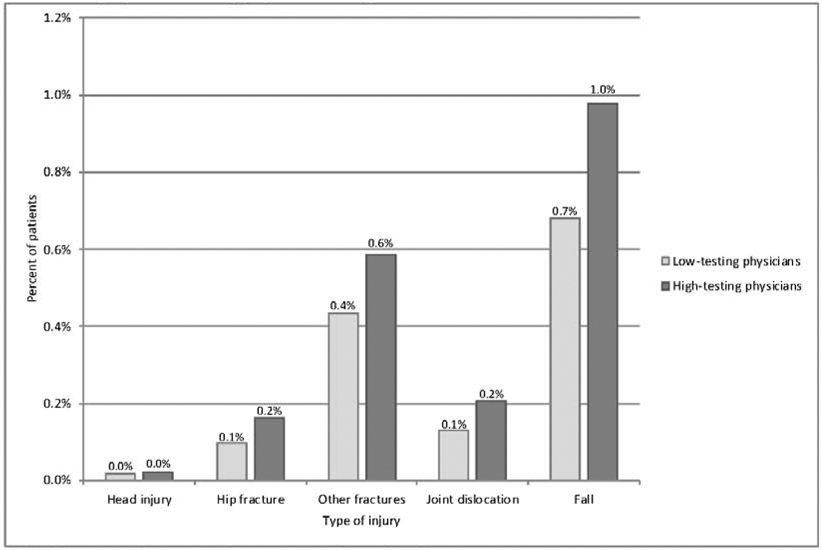
1) All Falls in Figure 2b occurred before surgery, within 90 days of biometry.
2) n=40,829 and 207,516 for patients of high-testing physicians and low-testing physicians, respectively.
The unadjusted odds ratio of having a fall within 90 days after biometry for patients of high-testing physicians compared to low-testing physicians was 1.15 (95% CI 1.07-1.24, p=0.0002, Table 2). When we adjusted for patient characteristics including age, sex, race, and health status, the odds of having a fall remained higher in patients of high-testing physicians (AOR 1.10 (95% CI 1.03-1.19, p=0.008). After accounting for the elapsed time between biometry and surgery, the odds of having a fall in patients of high-testing physicians decreased to 1.07 (95% CI 1.00-1.15, p=0.06). We found no difference in the odds of falling during the 360 days preceding biometry in patients of high-testing vs low-testing physicians (AOR 1.03, 95% CI 0.99-1.08, p=0.11, eTable 2) after adjusting for the same patient characteristics that we included in our primary model (i.e., age, sex, race, and health status). In our multiple linear regression model, after adjusting for patient, ophthalmologist, and health system characteristics, we found that having a high-testing physician increased the number of days between biometry and surgery by approximately 8 days compared to having a low-testing physician (estimate 7.97, 95% CI 6.40-9.55, p<0.0001, eTable 3). Other factors associated with a longer interval between biometry and surgery included race (8.94 and 7.14 additional days for black and other/unknown patients, respectively, compared to white patients), receiving care in the Northeast region (10.19 to 13.02 additional days compared to other regions), being cared for by a younger ophthalmologist (9.83 additional days for ≤40 versus ≥61 years old), lower annual surgical volume (5.63 additional days in lowest quartile compared to highest quartile), and surgical setting (2.29 additional days for hospital outpatient department compared to ambulatory surgery center). All of these comparisons were statistically significant. (eTable 3).
Table 2:
Predictors of falling within 90 days of ocular biometry
| Unadjusted OR (95% CI) |
p-value | Adjusted OR1 (95% CI) |
p-value | Adjusted OR2 (95% CI) |
p-value | |
|---|---|---|---|---|---|---|
| Age (mean +/− SD) | 1.03 (1.02-1.03) | <0.0001 | 1.02 (1.02-1.03) | <0.0001 | 1.02 (1.02-1.03) | <0.0001 |
| Sex | ||||||
| Male | Ref | Ref | Ref | |||
| Female | 1.67 (1.56-1.78) | <0.0001 | 1.73 (1.62-1.85) | <0.0001 | 1.72 (1.61-1.83) | <0.0001 |
| Race | ||||||
| White | Ref | Ref | Ref | |||
| Black | 0.55 (0.46-0.65) | <0.0001 | 0.50 (0.42-0.60) | <0.0001 | 0.49 (0.41-0.58) | <0.0001 |
| Other | 1.11 (1.00-1.23) | 0.05 | 1.02 (0.91-1.13) | 0.76 | 0.99 (0.89-1.10) | 0.84 |
| Charlson comorbidity index | ||||||
| 0-1 | Ref | Ref | Ref | |||
| 2 | 1.37 (1.26-1.49) | <0.0001 | 1.41 (1.29-1.54) | <0.0001 | 1.41 (1.29-1.53) | <0.0001 |
| 3+ | 1.85 (1.73-1.99) | <0.0001 | 1.93 (1.80-2.07) | <0.0001 | 1.92 (1.79-2.06) | <0.0001 |
| Time between biometry and surgery | ||||||
| <30 days | Ref | - | - | Ref | ||
| 31-60 days | 1.02 (0.94-1.10) | 0.67 | - | - | 1.00 (0.93-1.09) | 0.91 |
| 61-90 days | 1.35 (1.19-1.54) | <0.0001 | - | - | 1.32 (1.16-1.50) | <0.0001 |
| >90 days | 1.80 (1.66-1.96) | <0.0001 | - | - | 1.73 (1.59-1.88) | <0.0001 |
| Physician preop testing behavior | ||||||
| Low-testing physicians | Ref | Ref | Ref | |||
| High-testing physicians | 1.15 (1.07-1.24) | 0.0002 | 1.10 (1.03-1.19) | 0.008 | 1.07 (1.00-1.15) | 0.06 |
Adjusted for age, sex, race and health status.
Adjusted for age, sex, race, health status, and time to surgery
DISCUSSION
In this first ever study of the impact of routine preoperative medical testing on delayed surgery and fall events in Medicare beneficiaries awaiting cataract surgery, we found that patients of high-testing physicians wait longer for surgery and experience more falls and fall-related injuries than patients of low-testing physicians.
Despite guidelines stating that routine preoperative testing is not necessary before cataract surgery,8-10,23 such testing is frequently performed in these older adults,13-15 and many physicians order tests on nearly all of their patients regardless of clinical indication.14 However, aside from the inconvenience to patients and the cost to patients and Medicare, it was not previously known whether routine preoperative testing caused clinical harm. Although the magnitude of effect of having a high-testing physician was limited compared to some of the other risk factors for falling that we accounted for in our analysis, our study still demonstrates that patients of high-testing physicians experience more falls and fall-related injuries during the brief but potentially avoidable surgical delay that accompanies the deployment of routine preoperative testing. The lack of association between physician testing behavior and falls in the 360 days preceding biometry supports our hypothesis that the falls that occur after a patient begins preparing for surgery are associated with the routine use of preoperative testing, rather than from other underlying differences in patients of high-testing physicians compared to patients of low-testing physicians.
Fall-related injuries in older adults are a major public health concern because of their prevalence, the associated morbidity and mortality, and their cost to the healthcare system.24,25 The link between routine preoperative testing, surgical delays, and falls is strengthened by our finding that there is an estimated difference in time to surgery of approximately 8 days between patients of high-testing and low-testing physicians after adjusting for other factors that may impact surgical scheduling. However, we found that factors such as patient race, geographic region, ophthalmologist age, surgical volume and surgical setting also play a role in determining the timing of surgery in relation to biometry. Since our study did not directly evaluate the association between these other factors and the risk of falls, we cannot give definitive recommendations regarding the ideal timing of cataract surgery that would best minimize fall risk. Nevertheless, given the mechanism by which we believe routine preoperative testing contributes to falls in this patient population, we can extrapolate that any reduction in the duration of time a patient awaits cataract surgery has the potential to help lower the risk of falls that can arise from the visual disturbances caused by advanced cataract disease. This includes the elimination of surgical delays attributable to the time spent undergoing routine preoperative testing or managing the incidental findings that sometimes result from performing unnecessary tests, as well as expediting other aspects of surgical scheduling to allow patients to undergo surgery as soon as possible once the decision to proceed with surgery has been made.
There are many reasons that routine preoperative testing persists in this patient population. Most cataract patients are of advanced age and have multiple coexisting chronic illnesses. As a result, many providers have concerns about patient safety as well as worries about the medicolegal risks of not performing a thorough preoperative evaluation.13,26 Attitudes towards preoperative testing itself also perpetuates its continued use: for the most part, both doctors and patients consider routine preoperative testing to be a harmless intervention, aside from the time, inconvenience, and cost borne by patients who have to undergo “preoperative clearance.”27 Finally, patients undergoing surgery at ambulatory surgery centers (ASC) were historically required by the Centers for Medicare and Medicaid Services (CMS) to have a history and physical performed by a physician within the 30 days preceding surgery, which was often accompanied by cardiac and laboratory testing. With the recent change to allow ASCs to customize history and physical requirements according to the expected risk of the planned procedure or the underlying health risks of the surgical patient, combined with the evidence for potential harm arising from routine preoperative medical testing presented in our current study, we anticipate that the use of routine testing among cataract surgery patients will continue to fall.28
This study has several limitations. First, we used retrospective data relying on a surrogate marker (ocular biometry) to determine the timing of surgical delay. Although we have previously shown that biometry can accurately reflect the start of a surgical episode of care,15 in actual clinical practice, the timing of cataract surgery in relation to biometry may vary depending on when the biometry claim was submitted by the ophthalmologist. In addition, our study did not account for all the factors that may be associated with delays in surgical scheduling. Variables such as patient preference, unexpected illness, and operating room availability may also play a role in determining the timing of surgery in relation to biometry. Second, our study only assessed Medicare cataract surgery patients, which may limit the generalizability of our findings to non-Medicare patients. Other limitations related to the use of administrative claims data, including the inability to assert causality because of the retrospective observational study design, also apply. Third, we categorized physicians according to their use of routine preoperative testing in the 30 days prior to surgery. Some of these tests could have been ordered for reasons other than for routine preoperative testing, and therefore physicians may have been miscategorized. In addition, since we were working with a 5% sample of Medicare beneficiaries, the routine preoperative testing behavior of each physician was assessed across multiple years (in contrast to the single year of data we used in our prior work).14 However, based on current preoperative testing guidelines, we feel confident that physicians who test 75-100% of their cataract patients are demonstrating overuse of routine preoperative medical testing. Fourth, Kim’s algorithm to detect fall events has not been externally validated, and patients with minor falls may not present to medical care. However, we found this algorithm to be the most robust methodologic approach available in the literature to detect fall events using Medicare claims data.21,22 Finally, although the falls themselves could have delayed surgery in patients of high-testing physicians, since the incidence of falls was rare, this would not fully explain the difference in surgical wait time between the two groups.
In conclusion, we found that patients of high-testing physicians are more likely to experience delayed surgery and falls while awaiting cataract surgery compared to patients of low-testing physicians. This is the first study to show that a physician’s decision to order routine preoperative testing is associated with clinical harm. This study reinforces the importance of following longstanding guidelines that recommend that patients should not undergo routine preoperative testing prior to cataract surgery.
Supplementary Material
Acknowledgments
Funding:
This research was supported by UCSF Anesthesia Research Support, the Foundation for Anesthesia Education and Research (FAER; Schaumburg, IL), and by an NIH training grant to the Department of Anesthesia and Perioperative Care at the University of California, San Francisco (T32 GM008440, PI: Hellman). SDM has an unrestricted grant from Research to Prevent Blindness (New York City). UCSF Anesthesia Research Support, FAER, NIGMS, and Research to Prevent Blindness had no role in the design or conduct of the study; the collection, management, analysis and interpretation of the data; the preparation, review or approval of the manuscript; or the decision to submit the manuscript for publication. Support for VA/CMS data provided by the Department of Veterans Affairs, VA Health Services Research and Development Service, VA Information Resource Center (Project Numbers SDR 02-237 and 98-004).
Footnotes
Disclosures/Conflicts of Interest:
AWG reports personal fees as a consultant for Masimo Inc and Haisco Pharmaceuticals, unrelated to the submitted work. The other authors have no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ianchulev T, Litoff D, Ellinger D, Stiverson K, & Packer M. Office-based cataract surgery: Population health outcomes study of more than 21 000 cases in the United States. Ophthalmology 123, 723–728, doi: 10.1016/j.ophtha.2015.12.020 [doi] (2016). [DOI] [PubMed] [Google Scholar]
- 2.Schein OD, Cassard SD, Tielsch JM & Gower EW. Cataract surgery among Medicare beneficiaries. Ophthalmic epidemiology 19, 257–264, doi: 10.3109/09286586.2012.698692 [doi] (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Owsley C, McGwin G, Sloane M, Wells J, Stalvey B T, Gauthreaux S. Impact of cataract surgery on motor vehicle crash involvement by older adults. JAMA 288, 841–849, doi: 10.1001/jama.288.7.841 (2002). [DOI] [PubMed] [Google Scholar]
- 4.Hodge W, Horsley T, Albiani D, et al. The consequences of waiting for cataract surgery: A systematic review. Canadian Medical Association Journal 176, 1285–1290, doi: 10.1503/cmaj.060962 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iroku-Malize T & Kirsch S. Eye conditions in older adults: Cataracts. FP Essentials 445, 17–23 (2016). [PubMed] [Google Scholar]
- 6.Tseng V, Yu F, Lum F, Coleman AL. Risk of fractures following cataract surgery in Medicare beneficiaries. JAMA 308, 493–501, doi: 10.1001/jama.2012.9014 (2012). [DOI] [PubMed] [Google Scholar]
- 7.Harwood RH, Foss JE, Osborn F, Gregson RM, Zaman A, Masud T. Falls and health status in elderly women following first eye cataract surgery: a randomised controlled trial. British Journal of Ophthalmology 89, 53–59, doi: 10.1136/bjo.2004.049478 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Apfelbaum JL, Connis RT, Nickinovich DG, et al. Practice advisory for preanesthesia evaluation: An updated report by the American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Anesthesiology 116, 522–538, doi: 10.1097/ALN.0b013e31823c1067 [doi] (2012). [DOI] [PubMed] [Google Scholar]
- 9.Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Developed in collaboration with the American College of Surgeons, American Society of Anesthesiologists, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Anesthesiologists, and Society of Vascular Medicine Endorsed by the Society of Hospital Medicine. Journal of nuclear cardiology : Official publication of the American Society of Nuclear Cardiology 22, 162–215, doi: 10.1007/s12350-014-0025-z [doi] (2015). [DOI] [PubMed] [Google Scholar]
- 10.American Academy of Ophthalmology. Routine pre-operative laboratory testing for patients scheduled for cataract surgery, Clinical Statement, <http://www.aao.org/clinical-statement/routine-preoperative-laboratory-testing-patients-s> [Google Scholar]
- 11.Schein OD, Katz J, Bass EB, et al. The value of routine preoperative medical testing before cataract surgery. Study of Medical Testing for Cataract Surgery. The New England Journal of Medicine 342, 168–175, doi: 10.1056/NEJM200001203420304 [doi] (2000). [DOI] [PubMed] [Google Scholar]
- 12.Imasogie N, Wong DT, Luk K, & Chung F. Elimination of routine testing in patients undergoing cataract surgery allows substantial savings in laboratory costs. A brief report. Canadian Journal of Anaesthesia = Journal Canadien d'Anesthesie 50, 246–248, doi: 10.1007/BF03017792 [doi] (2003). [DOI] [PubMed] [Google Scholar]
- 13.Steinberg EP, Javitt JC, Sharkey PD, et al. The content and cost of cataract surgery. Archives of Ophthalmology 111, 1041–1049 (1993). [DOI] [PubMed] [Google Scholar]
- 14.Chen CL, Lin GA, Bardach NS, et al. Preoperative medical testing in Medicare patients undergoing cataract surgery. The New England Journal of Medicine 372, 1530–1538, doi: 10.1056/NEJMsa1410846 [doi] (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen CL, Clay TH, McLeod S, et al. A revised estimate of costs associated with routine preoperative testing in Medicare cataract patients with a procedure-specific indicator. JAMA Ophthalmol 136, 231–238, doi: 10.1001/jamaophthalmol.2017.6372 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sahin A & Hamrah P. Clinically relevant biometry. Current Opinion in Ophthalmology 23, 47–53, doi: 10.1097/ICU.0b013e32834cd63e [doi] (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sheard R Optimising biometry for best outcomes in cataract surgery. Eye (London, England) 28, 118–125, doi: 10.1038/eye.2013.248 [doi] (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.CPT/Current Procedural Terminology (Professional Edition). 2017 Edition (American Medical Association, 2016). [Google Scholar]
- 19.National Center for Health Statistics. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), <https://www.cdc.gov/nchs/icd/icd9cm.htm>
- 20.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Medical Care 43, 1130–1139, doi:00005650-200511000-00010 [pii] (2005). [DOI] [PubMed] [Google Scholar]
- 21.Hoffman GJ, Hays RD, Shapiro MF, Wallace SP, & Ettner SL. Claims-based identification methods and the cost of fall-related injuries among US older adults. Medical Care 54, 664–671, doi: 10.1097/MLR.0000000000000531 [doi] (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim BS, Zingmond DS, Keeler EB, et al. Development of an algorithm to identify fall-related injuries and costs in Medicare data. Injury Epidemiology 3, 1, doi: 10.1186/s40621-015-0066-z (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Onuoha OC, Arkoosh VA, & Fleisher LA. Choosing wisely in anesthesiology: The gap between evidence and practice. JAMA Internal Medicine, doi: 10.1001/jamainternmed.2014.2309 [doi] (2014). [DOI] [PubMed] [Google Scholar]
- 24.Roudsari BS, Ebel BE, Corso PS, Molinari NM, & Koepsell TD. The acute medical care costs of fall-related injuries among the U.S. older adults. Injury 36, 1316–1322, doi: 10.1016/j.injury.2005.05.024 (2005). [DOI] [PubMed] [Google Scholar]
- 25.Verma SK, Willetts JL, Corns HL, Marucci-Wellman HR, Lombardi DA, & Courtney TK. Falls and fall-related injuries among community-dwelling adults in the United States. - PLoS ONE 11, doi: 10.1371/journal.pone.0150939 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brown SR & Brown J. Why do physicians order unnecessary preoperative tests? A qualitative study. Family medicine 43, 338–343 (2011). [PubMed] [Google Scholar]
- 27.Patey AM, Islam R, Francis JJ, Bryson GL, Grimshaw JM. Anesthesiologists' and surgeons' perceptions about routine pre-operative testing in low-risk patients: application of the Theoretical Domains Framework (TDF) to identify factors that influence physicians' decisions to order pre-operative tests. Implementation science : IS 7, 52, doi: 10.1186/1748-5908-7-52 [doi] (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Department of Health and Human Services Center for Medicare and Medicaid Services. Medicare and Medicaid Programs; Regulatory Provisions To Promote Program Efficiency, Transparency, and Burden Reduction; Fire Safety Requirements for Certain Dialysis Facilities; Hospital and Critical Access Hospital (CAH) Changes To Promote Innovation, Flexibility, and Improvement in Patient Care. https://www.govinfo.gov/content/pkg/FR-2019-09-30/pdf/2019-20736.pdf (2019).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


