Abstract
Introduction
The COVID-19 pandemic may have negatively impacted children's weight status owing to the closure of schools, increased food insecurity and reliance on ultraprocessed foods, and reduced opportunities for outdoor activity.
Methods
In this interrupted time-series study, height and weight were collected from children (n=1,770 children, mean age=8.7 years, 55.3% male, 64.6% Black) and were transformed into BMI z-score in each August/September from 2017 to 2020. Mixed-effects linear regression estimated yearly BMI z-score change before the COVID-19 pandemic year (i.e., 2017–2019) and during the COVID-19 pandemic year (i.e., 2019–2020). Subgroup analyses by sex, race (i.e., Black, White, other race), weight status (overweight or obese and normal weight), and grade (i.e., lower=kindergarten−2nd grade and upper=3rd−6th grade) were conducted.
Results
Before the COVID-19 pandemic, children's yearly BMI z-score change was +0.03 (95% CI= −0.10, 0.15). Change during the COVID-19 pandemic was +0.34 (95% CI=0.21, 0.47), an acceleration in BMI z-score change of +0.31 (95% CI=0.19, 0.44). For girls and boys, BMI z-score change accelerated by +0.33 (95% CI=0.16, 0.50) and +0.29 (95% CI=0.12, 0.46), respectively, during the pandemic year. Acceleration in BMI z-score change during the pandemic year was observed for children who were Black (+0.41, 95% CI=0.21, 0.61) and White (+0.22, 95% CI=0.06, 0.39). For children classified as normal weight, BMI z-score change accelerated by +0.58 (95% CI=0.40, 0.76). Yearly BMI z-score change accelerated for lower elementary/primary (+0.23, 95% CI=0.08, 0.37) and upper elementary/primary (+0.42, 95% CI=0.42, 0.63) children.
Conclusions
If similar BMI z-score accelerations occurred for children across the world, public health interventions to address this rapid unhealthy BMI gain will be urgently needed.
INTRODUCTION
The coronavirus disease 2019 (COVID-19) pandemic has spread to nearly every country around the world, and as of January 2021, there have been >90,000,000 reported cases and 2,000,000 total deaths worldwide.1 The COVID-19 pandemic has introduced a variety of significant disruptions to individuals’ lifestyles that could negatively impact children's health behaviors and weight status, including but not limited to the following. First, stay-at-home orders may have reduced children's opportunity for outdoor play and increased screen time. Studies have shown that children are less physically active when they are indoors,2 and increased screen time is a risk factor for obesity.3 , 4 Second, food insecurity may have increased dramatically during the COVID-19 pandemic,5 with some estimates indicating that food insecurity has risen as much as 35%,6 , 7 and food insecurity has been linked to increased risk for obesity.8 Third, studies have also indicated that families may have increased their reliance on shelf-stable ultraprocessed foods during the COVID-19 pandemic.9 , 10 Increased consumption of processed foods has been linked to obesity risk in children.11 Finally, the structured days hypothesis12 posits that school exerts a protective influence on children's obesogenic behaviors and, in turn, children's weight status.13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28 Specifically, a large and growing body of evidence indicates that children engage in a greater number of behaviors that lead to increased weight gain on days when they are not in school (e.g., weekends and summer) than on days they attend school. Therefore, it is likely that the closure of school buildings for an extended time had negative impacts on children's health behaviors and weight status.29 , 30 Indeed, a growing body of literature shows that children's BMI gain accelerates during summer vacation from school.31, 32, 33
On the basis of this evidence, a recent simulation indicated that BMI z-score (zBMI) gain would increase by up to 0.20 from April 2020 to March 2021 owing to pandemic-related school closures’ impact on physical activity levels,34 and another study estimated a 4.25-percentage point (95% CI=2.90, 5.60) increase in childhood obesity.29 Furthermore, preliminary, largely self-report studies indicate that children's health behaviors have deteriorated during the COVID-19 pandemic.9 , 35, 36, 37, 38, 39, 40, 41 Thus, the objective of this study is to evaluate the impact of the COVID-19 pandemic on children's zBMI.
METHODS
This study is consistent with an interrupted time-series design. Time-series data consist of a continuous sequence of repeated observations collected at consistent intervals in a sample of participants.42 In an interrupted time-series design, the sequence of repeated observations is interrupted by a naturally occurring intervention at a known timepoint.43 , 44 In this study, the repeated observations consisted of collecting the heights and weights of all the children at 3 participating schools each fall from 2017 to 2020. The intervention that interrupted this time series was the novel COVID-19 pandemic and the associated mitigation strategies. The participating schools closed on March 16, 2020 and did not reopen until the following school year (i.e., September 9, 2020), and a stay-at-home order was issued by the governor of the state in which the schools are located on April 7, 2020 and was lifted on May 4, 2020.
Across the 3 schools, there were 2 groups of participants in this study. The first group included children who had their heights and weights collected before and during the COVID-19 pandemic (i.e., children with pandemic measures, n=182). The second group was children who only had measures before the COVID-19 pandemic (i.e., children without pandemic measures, n=1,588). In this study, the second group (i.e., children without pandemic measures) served as a control to ascertain whether children in Group 1 (i.e., children with pandemic measures) systematically differed from other children in the schools before the COVID-19 pandemic. The number of children measured during each measurement wave is presented in Table 1 .
Table 1.
Number of Children Measured in Each August/September
| Group | Sample size | 2017 | 2018 | 2019 | 2020 |
|---|---|---|---|---|---|
| Did not meet inclusion criteria (excluded from analyses) | 101 | — | — | — | ● |
| Group 1 (children with a pandemic measure) | 3 | — | ● | — | ● |
| 3 | ● | — | ● | ● | |
| 38 | — | — | ● | ● | |
| 5 | ● | — | — | ● | |
| 5 | ● | ● | — | ● | |
| 59 | — | ● | ● | ● | |
| 69 | ● | ● | ● | ● | |
| Group 2 (comparison) | 179 | — | ● | ● | — |
| 193 | — | ● | — | — | |
| 205 | ● | ● | — | — | |
| 27 | ● | — | ● | — | |
| 300 | — | — | ● | — | |
| 340 | ● | — | — | — | |
| 344 | ● | ● | ● | — |
On the basis of this study design, the following hypotheses were generated:
-
1.
Children with and without pandemic measures would have similar yearly changes in zBMI before the COVID-19 pandemic (2017–2019).
-
2.
Children with pandemic measures would experience accelerations in zBMI change during the COVID-19 pandemic (2019–2020) compared with that during the previous years (2017–2019).
Study Sample
A total of 3 schools in a single school district in 1 southeastern U.S. state participated in this study. All the children at the participating schools were eligible to participate in this study. Data collection was conducted each in August/September from 2017 to 2020. Before each data collection wave, a letter with information about the study and data collection protocols was sent home with instructions on how parents could opt for their children not to participate. Children provided verbal assent before each measurement occasion. All protocols were approved by the University of South Carolina IRB. A total of 1,883 unique children attended the participating schools during the 4 years of the study. Children who did not have a measure before the COVID-19 pandemic (n=101) and whose parents opted them out of the study (n=12) were not included, resulting in a final analytic sample of 1,770 children.
Measures
During regularly scheduled physical education classes, the heights (nearest 0.1 cm) and weights (nearest 0.01 lbs) of the children at the participating schools were measured within the first 3 weeks of the school year (i.e., August/September) 2017, 2018, 2019, and 2020 using a portable stadiometer (Model S100, Ayrton Corp., Prior Lake, MN) and a digital scale (Model 500KL, Health-o-Meter, McCook, IL). Children were instructed to remove their shoes and any heavy outer clothing (i.e., jackets, sweaters). BMI was calculated (BMI=kg/m2) and transformed into age- and sex-specific z-scores according to the WHO BMI for age growth charts.45 zBMI is a measure of relative BMI, adjusted for child age and sex, compared with a reference standard (i.e., in this case, it was compared with the WHO BMI for age growth charts). zBMI is necessary for children because they are naturally gaining BMI (i.e., gaining weight and height) as their bodies develop and mature. Thus, a change in zBMI of 0 would indicate that a child has maintained their BMI over time, relative to other children of the same age and sex during the same timeframe, whereas an increase would indicate that their BMI gain has increased more rapidly, and a negative change would indicate that a child's BMI gain has increased less rapidly than those of their same age and sex peers in the reference sample.
Statistical Analysis
All analyses were completed in Stata, version 16.1, during December 2020. Before completing the primary analyses, descriptive means and SDs of school and child characteristics were examined. Children who met the inclusion criteria and had ≥1 valid measure of BMI at any timepoint were included.46, 47, 48 All primary and secondary analyses used maximum likelihood estimators to account for missing data.49 , 50 Because data were collected for 2 years before the COVID-19 pandemic (2017–2019), zBMI change was annualized to represent yearly change. Primary analyses were designed to test the yearly change in zBMI before (August/September 2017–August/September 2019) and during the COVID-19 pandemic (August/September 2019–August/September 2020). Multilevel mixed-effects models with measures nested within children and children nested within school were estimated. The dependent variable was yearly zBMI change, and time was the independent variable. Time was dichotomized into before (2017–2019) and during (2019–2020) the COVID-19 pandemic. Secondary logistic regression analyses with the same nesting structure estimated the odds of children being classified as overweight or obese during the year of the COVID-19 pandemic compared with that during the previous years. Sensitivity analyses following the same modeling techniques but restricted to only children with measures at all timepoints in Groups 1 and 2 (n=69 with all measures before and during the COVID-19 pandemic, n=344 with all measures before the COVID-19 pandemic only) were also conducted. All analyses controlled for sex, age, race, and baseline level of zBMI. Multiple comparisons were controlled for through the Benjamini–Hochberg procedure with a false discovery rate of 10%.51
RESULTS
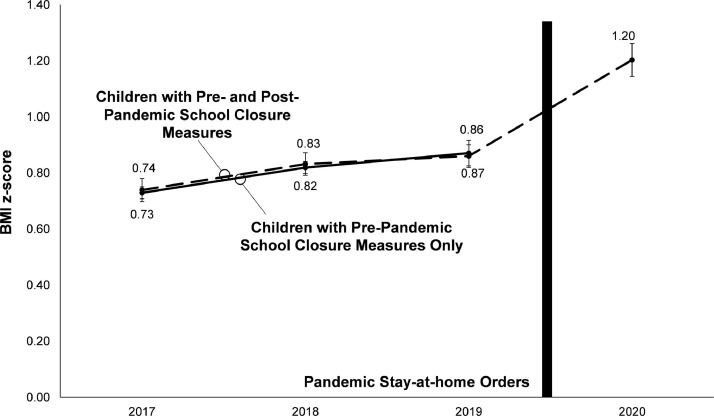
Descriptive data for the participating schools and children are presented in Table 2 . The mean age of the participating children was 8.8 (SD=2.0) years. The sample was primarily Black (63.4%) and was eligible for free or reduced lunches (85.9%). Sensitivity analyses restricted to children with complete data did not differ from the results of the primary and secondary analyses. Therefore, full sample analyses are presented and discussed. Findings from the regression analyses are presented in Figure 1 and Table 3 .
Table 2.
Demographic Characteristics of Participating Schools and Children
| Characteristics | Participants with prepandemic measures only | Participants with prepandemic and during-pandemic measures |
|---|---|---|
| School characteristics | ||
| Total students | 1,883 | — |
| % Male | 52.6 | — |
| Grades | K‒6 | — |
| Race | ||
| % White non-Hispanic | 23.9 | — |
| % Black | 63.4 | — |
| % Other race (including all races other than Black or White) | 12.7 | — |
| % Free or reduced-price lunch | 85.9 | — |
| Participant characteristics | ||
| Overall number of participants | 1,588 | 182 |
| % Male | 50.1 | 57.1 |
| Mean grade (SD) | 3.2 (2.0) | 3.0 (1.7) |
| Mean age (SD) | 8.9 (2.1) | 8.5 (1.7) |
| Race | ||
| % White non-Hispanic | 26.1 | 29.2 |
| % Black | 65.2 | 60.3 |
| % Other race (including all races other than Black or White) | 8.7 | 10.5 |
| Mean BMI z-score | ||
| Fall 2017 (SD) | 0.80 (1.20) | 0.78 (1.25) |
| Fall 2018 (SD) | 0.80 (1.18) | 0.78 (1.20) |
| Fall 2019 (SD) | 0.80 (1.21) | 0.80 (1.28) |
| Fall 2020 (SD) | — | 1.16 (1.20) |
| % overweight or obese | ||
| Fall 2017 | 44.4 | 41.5 |
| Fall 2018 | 42.2 | 46.7 |
| Fall 2019 | 42.9 | 47.3 |
| Fall 2020 | — | 58.8 |
K‒6, kindergarten–Grade 6.
Figure 1.
Model estimated the BMI z-score of participants before and after the pandemic school closures.
Table 3.
Yearly Change in zBMI and OWOB in the Overall Sample and by Subgroup
| Children with pre-pandemic measures only |
Children with pre-pandemic and during-pandemic measures |
Between group (before pandemic) |
Within group (during pandemic compared with before pandemic)a |
|||
|---|---|---|---|---|---|---|
| Variable | Before pandemic (SE) | Before pandemic (SE) | During pandemic (SE) | Diff (95% CI) | Diff (95% CI) | Odds of OWOB (95% CI) |
| Overall sample | 0.03 (0.05) | 0.03 (0.06) | 0.34 (0.11) | 0.00 (−0.09, 0.08) | 0.31 (0.19, 0.44) | 1.80 (1.40, 2.33) |
| Sex | ||||||
| Male | 0.08 (0.08) | 0.05 (0.09) | 0.34 (0.16) | −0.03 (−0.15, 0.09) | 0.29 (0.12, 0.46) | 1.97 (1.30, 2.98) |
| Female | −0.04 (0.07) | −0.02 (0.09) | 0.31 (0.16) | 0.02 (−0.11, 0.14) | 0.33 (0.16, 0.50) | 1.71 (1.25, 2.35) |
| Race | ||||||
| Black | 0.10 (0.03) | 0.08 (0.06) | 0.49 (0.13) | −0.02 (−0.14, 0.10) | 0.41 (0.21, 0.60) | 2.57 (1.58, 4.19) |
| White | 0.05 (0.04) | 0.03 (0.06) | 0.25 (0.13) | −0.02 (−0.15, 0.10) | 0.22 (0.06, 0.39) | 2.79 (1.07, 7.24) |
| Other race | 0.03 (0.10) | 0.13 (0.15) | 0.37 (0.28) | 0.10 (−0.21, 0.40) | 0.24 (−0.10, 0.59) | 1.24 (0.85, 1.79) |
| Weight status | ||||||
| Normal weight | 0.01 (0.09) | 0.00 (0.10) | 0.58 (0.18) | −0.01 (−0.15, 0.12) | 0.58 (0.40, 0.76) | 7.50 (3.09, 18.16) |
| OWOB | −0.05 (0.07) | −0.06 (0.08) | −0.05 (0.15) | −0.01 (−0.11, 0.10) | 0.00 (−0.14, 0.15) | 1.44 (0.44, 4.78) |
| Grade | ||||||
| Lower elementary (K‒2nd grade) | −0.01 (0.08) | 0.02 (0.09) | 0.24 (0.16) | 0.03 (−0.08, 0.13) | 0.23 (0.08, 0.37) | 1.65 (1.18, 2.29) |
| Upper elementary (3rd–6th grade) | 0.11 (0.08) | 0.05 (0.10) | 0.47 (0.18) | −0.06 (−0.21, 0.09) | 0.42 (0.22, 0.63) | 2.13 (1.46, 3.12) |
Note: Boldface indicates statistical significance (p≤0.05).
Change in zBMI of 0 would indicate that a child has maintained their BMI over time, relative to that in other children of the same age and sex during the same timeframe, whereas an increase would indicate that their BMI gain has increased more rapidly, and a negative change score would indicate that a child's BMI gain has increased less rapidly than that of their same age and sex peers in the reference sample.
Diff in yearly zBMI change during pandemic compared with that before the pandemic in children with both prepandemic and during-pandemic measures.
Diff, difference; K‒2nd grade, kindergarten–Grade 2; OWOB, overweight or obesity; zBMI, BMI z-score.
Consistent with Hypothesis 1, before the COVID-19 pandemic, children with and those without pandemic measures experienced the same mean yearly zBMI change of 0.03 in the years preceding the pandemic (difference=0.00, 95% CI= −0.09, 0.08). Furthermore, there were no statistically significant or clinically meaningful52 , 53 differences between children with and those without pandemic measures in yearly zBMI change before the COVID-19 pandemic by weight status, race, grade, or sex. The remaining analyses were conducted among the sample of children with pandemic measures.
Consistent with Hypothesis 2, children showed a 0.34 increase in zBMI during the COVID-19 pandemic. This represented an acceleration in zBMI change of 0.31 (95% CI=0.19, 0.44) compared with their mean yearly change in zBMI before the pandemic. Correspondingly, children were 1.80 (95% CI=1.40, 2.33) times more likely to be overweight or obese during the COVID-19 pandemic than in previous years.
Next, accelerated zBMI gain by age and sex was examined. Male and female children experienced a 0.29 (95% CI=0.12, 0.46) and 0.33 (95% CI=0.16, 0.50) acceleration in zBMI change during the pandemic, respectively, compared with that in the previous years and were 1.97 (95% CI=1.30, 2.98) and 1.71 (95% CI=1.25, 2.35) times more likely to be overweight and obese during the COVID-19 pandemic, respectively.
Accelerated zBMI gain by race was then examined. Children who are Black experienced a 0.41 (95% CI=0.21, 0.60) acceleration in zBMI change during the pandemic compared with that in the previous years and were 2.57 (95% CI=1.58, 4.19) times more likely to be overweight and obese during the COVID-19 pandemic. Similarly, children who are White experienced a 0.22 (95% CI=0.06, 0.39) acceleration in zBMI change during the pandemic compared with that in the previous years and were 2.79 (95% CI=1.07, 7.24) times more likely to be overweight and obese during the COVID-19 pandemic. Children who were identified by their parents to be of other race gained 0.24 (95% CI= −0.10, 0.59) more zBMI during the pandemic than in the previous years and were 1.24 (95% CI=0.85, 1.79) times more likely to be overweight and obese during COVID-19 pandemic.
Accelerated zBMI gain by weight status was examined next. Children who were normal weight before the COVID-19 pandemic experienced a 0.58 (95% CI=0.40, 0.76) acceleration in zBMI change during the pandemic compared with that in the previous years and were 7.50 (95% CI=0.40, 0.76) times more likely to be overweight or obese during the pandemic. Children who were overweight or obese before the COVID-19 pandemic did not experience accelerated zBMI gain during the pandemic.
Finally, accelerated zBMI gain by grade level was estimated. Lower and upper elementary school children experienced a 0.23 (95% CI=0.08, 0.37) and 0.42 (95% CI=0.22, 0.63) acceleration in zBMI change during the pandemic, respectively, compared with that in the years before the pandemic and were 1.65 (95% CI=1.18, 2.29) and 2.13 (95% CI=1.46, 3.12) more likely to be overweight and obese during the COVID-19 pandemic, respectively.
DISCUSSION
This study examined the impact of the COVID-19 pandemic on children's zBMI through an interrupted time-series study design. Children's zBMI change was approximately 10 times greater during the COVID-19 pandemic than in the previous years. Acceleration in zBMI gain was observed across children of different racial groups, grade levels, and sexes. Notably, whereas children who were normal weight experienced significant acceleration in zBMI change, children who were overweight or obese did not. Finally, the accelerated changes in zBMI translated into an increased risk of overweight or obesity.
Although there are a variety of reasons that children's BMI gain increased during the COVID-19 pandemic, the closure of the school buildings was likely a major driver of these increases. The structured days hypothesis posits that the structure (i.e., preplanned, compulsory, adult-supervised activities) provided by schools exerts a positive impact on children's weight-related behaviors (e.g., sleep, diet, physical activity, screen time).12 During the COVID-19 pandemic, children lost access to regularly scheduled, compulsory physical activity opportunities such as recess and physical education. Furthermore, children no longer had access to meals served at school, which likely increased food insecurity,6 , 7 a known risk factor for obesity.8 Finally, the lack of the school day likely led to variable and later sleep schedules, both of which have been linked to increased risk for overweight or obesity.54 , 55
Preliminary and largely self-reported evidence from around the world indicates that during the pandemic, children were more sedentary, engaged in more screen time35 and less physical activity,9 , 36 , 37 ate more unhealthy and fewer healthy foods,9 , 38 and experienced later and more variable sleep schedules.39 , 40 Engagement in similar behaviors is likely the behavioral mechanism responsible for the accelerated BMI gain in this study.
Although the impact of the COVID-19 pandemic on children's zBMI was not unexpected, the magnitude of the acceleration in change is alarming. Two recent studies have projected the impact of the COVID-19‒related school closures on children's zBMI.30 , 34 The first study used a microsimulation to estimate the change in zBMI of a nationally representative cohort of kindergarteners from April 2020 to March 2021. In the worst-case scenario (i.e., school closures of 6 months and a 10% reduction in physical activity during the months of summer), the study projected an acceleration in zBMI gain of 0.20 compared with that in the control. The second study took a simpler approach and simply multiplied the mean monthly gain in obesity prevalence of 0.85 percentage points per month (95% CI=0.58, 1.12) observed in a large nationally representative data set33 and multiplied it by 5 (i.e., the number of months schools were closed). This approach yielded an increase of 4.25 percentage points (95% CI=2.90, 5.60). This study indicates that the accelerations are markedly worse than projected, with an acceleration in zBMI gain of 0.31 from August 2020 to August 2021. This discrepancy may be because both studies only considered the impact of the removal of the school day and did not consider other impacts that the COVID-19 pandemic had on families (i.e., increase in food insecurity, stay-at-home orders, increased reliance on processed foods). Furthermore, the microsimulation study only considered the impact of reduced physical activity while neglecting to consider the impact of the school closures on children's sleep and diet. Past studies also indicate that school closures and natural disasters disproportionately impact children from minority and low-income households.56, 57, 58 This may partially explain the large magnitude of acceleration in zBMI change in this study given that majority of the sample were from low-income and minority households. Nonetheless, although the magnitude is greater, the acceleration in zBMI gain observed in this study is consistent with simulated projections about the impacts of limited access to school.
Notably, children who were normal weight experienced acceleration in zBMI change, whereas children who were overweight or obese did not. It is possible that children with overweight or obesity were already engaging in risky obesogenic behaviors before the pandemic; thus, behavioral changes were not as dramatic as in children with normal weight, and in turn, BMI gain did not increase as dramatically. However, because behavioral data were not collected, this is speculative. Future studies examining the changes in behavior patterns of children by weight status over the course of this time period might elucidate the mechanisms driving these differences. Furthermore, children who were Black experienced greater accelerations in BMI gain than their White counterparts. The reasons for this are unclear; however, differences in SES may be a mechanism that is driving this difference. Because of structural racism, children from minoritized households are from low-income households at a higher rate than their White counterparts.59 , 60 Thus, their families might have been impacted by COVID-19 to a greater degree than the families of children from higher-income and White households for the reasons discussed previously (i.e., school closing and natural disasters disproportionately impact children from minority and low-income households). However, because this study did not collect data on the SES of individuals, it is impossible to disentangle the impact of race and SES on BMI gain in this sample of children during the COVID-19 pandemic.
This study has several strengths that heighten its public health impact. A key strength of this study is the time-series design (i.e., 4 years of measures) and the objective measurement of zBMI. Although several studies examining the impacts of the COVID-19 pandemic have been published in recent months, the vast majority have relied on self-report questionnaires and surveys to measure health behaviors and weight status. The interrupted time-series design also allows for stronger causal inferences to be drawn about the impact of COVID-19 pandemic on the zBMI of children. Furthermore, this study included a large proportion of the children at the participating schools. Thus, the findings are likely representative of the changes in zBMI in these schools and are due to the COVID-19 pandemic.
Limitations
Results from this study should also be interpreted in the context of its limitations. This study was conducted in a convenience sample of 3 schools in 1 southeastern U.S. state and included schools that primarily serve children who are Black and from low-income families; thus, the findings may reflect the significant impact of COVID-19‒related school closures on the most vulnerable sector of the population. However, study findings may not generalize to children of other races/ethnicities or from higher-income populations. Furthermore, only 182 children had measures before and during the COVID-19 pandemic. Although repeated and objective measurement of zBMI is a relative strength of this study, it is worth noting that this study is limited by the lack of contextual measures beyond zBMI. Changes in BMI are driven by a complex web of behavioral, environmental, and biological factors. The lack of such measures does not allow for this study to examine the mechanisms responsible for these dramatic changes in zBMI. However, given the recent proliferation in COVID-19 studies published in the past year, it is likely that additional high-quality research regarding the behavioral impacts of COVID-19 will help contextualize the findings of this study.
CONCLUSIONS
The findings from this study indicate that children's zBMI gain increased dramatically during the COVID-19 pandemic. These findings are alarming given the magnitude of change in zBMI and underscore the urgent need for public health interventions to address overweight and obesity, especially in children from minority and low-income families.
ACKNOWLEDGMENTS
The content of this study is solely the responsibility of the authors and does not necessarily represent the official views of NIH.
Research reported in this publication was supported in part by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of NIH under Award Number R21HD095164 and the National Institute of General Medical Sciences Award Numbers P20GM130420 and T32-GM081740.
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.WHO coronavirus (COVID-19) dashboard. WHO. https://covid19.who.int/. Updated June 14, 2021. Accessed January 18, 2021.
- 2.Zheng C, Feng J, Huang W, Wong SH-S. Associations between weather conditions and physical activity and sedentary time in children and adolescents: a systematic review and meta-analysis. Health Place. 2021;69 doi: 10.1016/j.healthplace.2021.102546. [DOI] [PubMed] [Google Scholar]
- 3.Ramsey Buchanan L, Rooks-Peck CR, Finnie RKC. Reducing recreational sedentary screen time: a Community Guide systematic review [published correction appears in Am J Prev Med. 2016;50(6):809] Am J Prev Med. 2016;50(3):402–415. doi: 10.1016/j.amepre.2015.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stiglic N, Viner RM. Effects of screentime on the health and well-being of children and adolescents: a systematic review of reviews. BMJ Open. 2019;9(1) doi: 10.1136/bmjopen-2018-023191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gundersen C, Hake M, Dewey A, Engelhard E. Food insecurity during COVID-19. Appl Econ Perspect Policy. 2021;43(1):153–161. doi: 10.1002/aepp.13100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Niles MT, Bertmann F, Belarmino EH, Wentworth T, Biehl E, Neff R. The early food insecurity impacts of COVID-19. Nutrients. 2020;12(7):2096. doi: 10.3390/nu12072096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adams EL, Caccavale LJ, Smith D, Bean MK. Food insecurity, the home food environment, and parent feeding practices in the era of COVID-19. Obesity (Silver Spring) 2020;28(11):2056–2063. doi: 10.1002/oby.22996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Metallinos-Katsaras E, Must A, Gorman K. A longitudinal study of food insecurity on obesity in preschool children. J Acad Nutr Diet. 2012;112(12):1949–1958. doi: 10.1016/j.jand.2012.08.031. [DOI] [PubMed] [Google Scholar]
- 9.Ruíz-Roso MB, de Carvalho Padilha P, Matilla-Escalante DC. Changes of physical activity and ultra-processed food consumption in adolescents from different countries during COVID-19 pandemic: an observational study. Nutrients. 2020;12(8):2289. doi: 10.3390/nu12082289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.White M, Nieto C, Barquera S. Good deeds and cheap marketing: the food industry in the time of COVID-19. Obesity (Silver Spring) 2020;28(9):1578–1579. doi: 10.1002/oby.22910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Costa CS, Del-Ponte B, Assunção MCF, Santos IS. Consumption of ultra-processed foods and body fat during childhood and adolescence: a systematic review. Public Health Nutr. 2018;21(1):148–159. doi: 10.1017/S1368980017001331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brazendale K, Beets MW, Weaver RG. Understanding differences between summer vs. school obesogenic behaviors of children: the structured days hypothesis. Int J Behav Nutr Phys Act. 2017;14(1):100. doi: 10.1186/s12966-017-0555-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beck J, Chard CA, Hilzendegen C, Hill J, Stroebele-Benschop N. In-school versus out-of-school sedentary behavior patterns in U.S. children. BMC Obes. 2016;3(1):34. doi: 10.1186/s40608-016-0115-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Atkin AJ, Sharp SJ, Harrison F, Brage S, Van Sluijs EM. Seasonal variation in children's physical activity and sedentary time. Med Sci Sports Exerc. 2016;48(3):449–456. doi: 10.1249/MSS.0000000000000786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Riddoch CJ, Mattocks C, Deere K. Objective measurement of levels and patterns of physical activity. Arch Dis Child. 2007;92(11):963–969. doi: 10.1136/adc.2006.112136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Comte M, Hobin E, Majumdar SR. Patterns of weekday and weekend physical activity in youth in 2 Canadian provinces. Appl Physiol Nutr Metab. 2013;38(2):115–119. doi: 10.1139/apnm-2012-0100. [DOI] [PubMed] [Google Scholar]
- 17.Nyberg GA, Nordenfelt AM, Ekelund U, Marcus C. Physical activity patterns measured by accelerometry in 6- to 10-yr-old children. Med Sci Sports Exerc. 2009;41(10):1842–1848. doi: 10.1249/MSS.0b013e3181a48ee6. [DOI] [PubMed] [Google Scholar]
- 18.Gilbey H, Gilbey M. The physical activity of Singapore primary school children as estimated by heart rate monitoring. Pediatr Exerc Sci. 2010;7(1):26–35. doi: 10.1123/pes.7.1.26. [DOI] [Google Scholar]
- 19.Blader JC, Koplewicz HS, Abikoff H, Foley C. Sleep problems of elementary school children. A community survey. Arch Pediatr Adolesc Med. 1997;151(5):473–480. doi: 10.1001/archpedi.1997.02170420043007. [DOI] [PubMed] [Google Scholar]
- 20.Snell EK, Adam EK, Duncan GJ. Sleep and the body mass index and overweight status of children and adolescents. Child Dev. 2007;78(1):309–323. doi: 10.1111/j.1467-8624.2007.00999.x. [DOI] [PubMed] [Google Scholar]
- 21.Gulliford MC, Price CE, Rona RJ, Chinn S. Sleep habits and height at ages 5 to 11. Arch Dis Child. 1990;65(1):119–122. doi: 10.1136/adc.65.1.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Matheson DM, Killen JD, Wang Y, Varady A, Robinson TN. Children's food consumption during television viewing. Am J Clin Nutr. 2004;79(6):1088–1094. doi: 10.1093/ajcn/79.6.1088. [DOI] [PubMed] [Google Scholar]
- 23.Baranowski T, Smith M, Hearn MD. Patterns in children's fruit and vegetable consumption by meal and day of the week. J Am Coll Nutr. 1997;16(3):216–223. doi: 10.1080/07315724.1997.10718677. [DOI] [PubMed] [Google Scholar]
- 24.Au LE, Rosen NJ, Fenton K, Hecht K, Ritchie LD. Eating school lunch is associated with higher diet quality among elementary school students. J Acad Nutr Diet. 2016;116(11):1817–1824. doi: 10.1016/j.jand.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 25.Hart CN, Raynor HA, Osterholt KM, Jelalian E, Wing RR. Eating and activity habits of overweight children on weekdays and weekends. Int J Pediatr Obes. 2011;6(5–6):467–472. doi: 10.3109/17477166.2011.590204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cullen KW, Lara KM, de Moor C. Children's dietary fat intake and fat practices vary by meal and day. J Am Diet Assoc. 2002;102(12):1773–1778. doi: 10.1016/s0002-8223(02)90380-9. [DOI] [PubMed] [Google Scholar]
- 27.Hanson KL, Olson CM. School meals participation and weekday dietary quality were associated after controlling for weekend eating among U.S. school children aged 6 to 17 years. J Nutr. 2013;143(5):714–721. doi: 10.3945/jn.112.170548. [DOI] [PubMed] [Google Scholar]
- 28.Tanasescu M, Ferris AM, Himmelgreen DA, Rodriguez N, Pérez-Escamilla R. Biobehavioral factors are associated with obesity in Puerto Rican children. J Nutr. 2000;130(7):1734–1742. doi: 10.1093/jn/130.7.1734. [DOI] [PubMed] [Google Scholar]
- 29.Rundle AG, Park Y, Herbstman JB, Kinsey EW, Wang YC. COVID-19–related school closings and risk of weight gain among children. Obesity (Silver Spring). 2020;28(6):1008‒1009. https://doi.org/10.1002/oby.22813. [DOI] [PMC free article] [PubMed]
- 30.Workman J. How much may COVID-19 school closures increase childhood obesity? Obesity (Silver Spring) 2020;28(10):1787. doi: 10.1002/oby.22960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Franckle R, Adler R, Davison K. Accelerated weight gain among children during summer versus school year and related racial/ethnic disparities: a systematic review. Prev Chronic Dis. 2014;11:E101. doi: 10.5888/pcd11.130355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weaver RG, Beets MW, Brazendale K, Brusseau TA. Summer weight gain and fitness loss: causes and potential solutions. Am J Lifestyle Med. 2018;13(2):116–128. doi: 10.1177/1559827617750576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.von Hippel PT, Workman J. From kindergarten through second grade, U.S. children's obesity prevalence grows only during summer vacations. Obesity (Silver Spring) 2016;24(11):2296–2300. doi: 10.1002/oby.21613. [DOI] [PubMed] [Google Scholar]
- 34.An R. Projecting the impact of the coronavirus disease-2019 pandemic on childhood obesity in the United States: a microsimulation model. J Sport Health Sci. 2020;9(4):302–312. doi: 10.1016/j.jshs.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schmidt SCE, Anedda B, Burchartz A. Physical activity and screen time of children and adolescents before and during the COVID-19 lockdown in Germany: a natural experiment. Sci Rep. 2020;10(1):21780. doi: 10.1038/s41598-020-78438-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lu C, Chi X, Liang K. Moving more and Sitting less as healthy lifestyle behaviors are protective factors for insomnia, depression, and anxiety among adolescents during the COVID-19 pandemic. Psychol Res Behav Manag. 2020;13:1223–1233. doi: 10.2147/PRBM.S284103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ozturk Eyimaya A, Yalçin Irmak A. Relationship between parenting practices and children's screen time during the COVID-19 pandemic in Turkey. J Pediatr Nurs. 2021;56:24–29. doi: 10.1016/j.pedn.2020.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dondi A, Candela E, Morigi F, Lenzi J, Pierantoni L, Lanari M. Parents’ perception of food insecurity and of its effects on their children in Italy six months after the COVID-19 pandemic outbreak. Nutrients. 2020;13(1):121. doi: 10.3390/nu13010121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lim MTC, Ramamurthy MB, Aishworiya R. School closure during the coronavirus disease 2019 (COVID-19) pandemic-impact on children's sleep. Sleep Med. 2021;78:108–114. doi: 10.1016/j.sleep.2020.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Okely A, Kariippanon KE, Guan H. Global effect of COVID-19 pandemic on physical activity, sedentary behaviour and sleep among 3- to 5-year-old children: a longitudinal study of 14 countries. BMC Public Health. 2021;21(1):940. doi: 10.1186/s12889-021-10852-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bates LC, Zieff G, Stanford K. COVID-19 Impact on behaviors across the 24-hour day in children and adolescents: physical activity, sedentary behavior, and sleep. Children (Basel) 2020;7(9):138. doi: 10.3390/children7090138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McDowall D, McCleary R, Bartos BJ. Oxford University Press; Oxford, United Kingdom: 2019. Interrupted Time Series Analysis. [DOI] [Google Scholar]
- 43.Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial [published correction appears in Int J Epidemiol. 2020;49(4):1414] Int J Epidemiol. 2017;46(1):348–355. doi: 10.1093/ije/dyw098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lopez Bernal J, Cummins S, Gasparrini A. The use of controls in interrupted time series studies of public health interventions. Int J Epidemiol. 2018;47(6):2082–2093. doi: 10.1093/ije/dyy135. [DOI] [PubMed] [Google Scholar]
- 45.BMI-for-age (5-19 years). WHO. https://www.who.int/tools/growth-reference-data-for-5to19-years/indicators/bmi-for-age. Accessed January 17, 2021.
- 46.Trost SG, Rosenkranz RR, Dzewaltowski D. Physical activity levels among children attending after-school programs. Med Sci Sports Exerc. 2008;40(4):622–629. doi: 10.1249/MSS.0b013e318161eaa5. [DOI] [PubMed] [Google Scholar]
- 47.Beets MW, Wallner M, Beighle A. Defining standards and policies forpromoting physical activity in afterschool programs. J Sch Health. 2010;80(8):411–417. doi: 10.1111/j.1746-1561.2010.00521.x. [DOI] [PubMed] [Google Scholar]
- 48.Beets MW, Huberty J, Beighle A. Healthy Afterschool Program Network. Physical activity of children attending afterschool programs: research- and practice-based implications. Am J Prev Med. 2012;42(2):180–184. doi: 10.1016/j.amepre.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 49.Beets MW, Weaver RG, Moore JB. From policy to practice: strategies to meet physical activity standards in YMCA afterschool programs. Am J Prev Med. 2014;46(3):281–288. doi: 10.1016/j.amepre.2013.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Beets MW, Weaver RG, Turner-McGrievy G. Making policy practice in afterschool programs: a randomized controlled trial on physical activity changes. Am J Prev Med. 2015;48(6):694–706. doi: 10.1016/j.amepre.2015.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Series B Stat Methodol. 1995;57(1):289–300. doi: 10.1111/j.2517-6161.1995.tb02031.x. [DOI] [Google Scholar]
- 52.O'Connor EA, Evans CV, Burda BU, Walsh ES, Eder M, Lozano P. Screening for obesity and intervention for weight management in children and adolescents: evidence report and systematic review for the U.S. Preventive Services Task Force. JAMA. 2017;317(23):2427–2444. doi: 10.1001/jama.2017.0332. [DOI] [PubMed] [Google Scholar]
- 53.Preventive Services Task Force U.S., Grossman DC, Bibbins-Domingo K. Screening for obesity in children and adolescents: U.S. Preventive Services Task Force recommendation statement. JAMA. 2017;317(23):2417–2426. doi: 10.1001/jama.2017.6803. [DOI] [PubMed] [Google Scholar]
- 54.Golley RK, Maher CA, Matricciani L, Olds TS. Sleep duration or bedtime? Exploring the association between sleep timing behaviour, diet and BMI in children and adolescents. Int J Obes (Lond) 2013;37(4):546–551. doi: 10.1038/ijo.2012.212. [DOI] [PubMed] [Google Scholar]
- 55.Stoner L, Beets MW, Brazendale K, Moore JB, Weaver RG. Social jetlag is associated with adiposity in children. Glob Pediatr Health. 2018;5 doi: 10.1177/2333794X18816921. 2333794X18816921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kuhfeld M, Soland J, Tarasawa B, Johnson A, Ruzek E, Liu J. Projecting the potential impact of COVID-19 school closures on academic achievement. Educ Res. 2020;49(8):549–565. doi: 10.3102/0013189X20965918. [DOI] [Google Scholar]
- 57.Goodman J. Flaking out: student absences and snow days as disruptions of instructional time. NBER Work Pap Ser. 2014;(20221) doi: 10.3386/w20221. [DOI] [Google Scholar]
- 58.Sacerdote B. When the saints go marching out: long-term outcomes for student evacuees from Hurricanes Katrina and Rita. Am Econ J Appl Econ. 2012;4(1):109–135. doi: 10.1257/app.4.1.109. [DOI] [Google Scholar]
- 59.LaVeist TA. Disentangling race and socioeconomic status: a key to understanding health inequalities. J Urban Health. 2005;82(2):iii26–iii34. doi: 10.1093/jurban/jti061. (suppl 3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Flores G, Tomany-Korman SC, Olson L. Does disadvantage start at home?Racial and ethnic disparities in health-related early childhood home routines and safety practices. Arch Pediatr Adolesc Med. 2005;159(2):158–165. doi: 10.1001/archpedi.159.2.158. [DOI] [PubMed] [Google Scholar]