Abstract
Background
Health care workers (HCWs) during the COVID-19 pandemic experience numerous psychological problems, including stress and anxiety. These entities can affect their sleep quality and predispose them to insomnia. The aim of the present study was to investigate the prevalence of insomnia among HCWs during the COVID-19 crisis via an umbrella review.
Methods
The PRISMA guideline was used to conduct this review. By searching relevant keywords in databases of Scopus, PubMed, Web of Science, and Google Scholar, studies that reported the prevalence of insomnia among HCWs during the COVID-19 pandemic (January 2020 to the end of January 2021) and had been published in English were identified and evaluated. The random effects model was used for meta-analysis, and the I2 index was used to assess heterogeneity. The Egger test was used to determine publication bias. Based on the results of the primary search, 96 studies were identified, and ultimately 10 eligible studies entered the meta-analysis phase.
Results
The results of the umbrella review of meta-analyses showed that the prevalence of insomnia among HCWs during the COVID-19 pandemic was 36.36% (95% CI: 33.36–39.36, I2 = 59.6%, p = 0.006).
Conclusions
The results of this umbrella review of meta-analyses showed a relatively high prevalence of insomnia among HCWs during the COVID-19 pandemic. As insomnia can be associated with other psychological problems, policymakers and health managers should regularly screen HCWs for psychological disorders as well as a possible tendency for suicide. Furthermore, by treating insomnia, one can reduce the incidence of these psychological disorders.
Keywords: COVID-19, Health care workers, Sleep disorder, Mental health, Insomnia
1. Introduction
In December of 2019, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged in Wuhan, China and rapidly spread worldwide, causing the World Health Organization (WHO) declared a pandemic a few months later [1,2]. This pandemic has been associated with an increased prevalence of psychological health issues, in addition to the more obvious physical health consequences [3,4]. The disease affects different aspects of people's lives and different communities in the society, including health care workers (HCWs) [5,6]. HCWs, due to frequent contact with COVID-19 patients, are at high risk of infection transmission. In addition, they have grappled with higher workloads, frustration, discrimination, fatigue, isolation from their families, and shortages of personal protective equipment (PPE) within a high pressure, high stress work environment. Despite their resilience, a significant number of HCWs have experienced various physical and psychological problems [5,7]. It has been noted that due to high stress, HCWs engaged in caring for COVID-19 patients are at an increased risk of depression, anxiety, insomnia [8,9], burnout, and post-traumatic stress disorder (PTSD) [10]. Stress has been shown to be one of the main factors contributing to HCW insomnia. The change in normal daily routine, economic uncertainty, and concerns about contracting the COVID-19 have all contributed to increased HCW insomnia [11,12]. According to studies during the COVID-19 pandemic, HCWs serving on the front-line experience more sleep disorders and poorer sleep quality as compared with non-HCWs [13]. The results of a study in Turkey showed that the prevalence of depression, anxiety, and insomnia among HCWs were 77.6%, 60.2, and 50.4%, respectively [14]. The results of another study in China revealed that about one-third of HCWs experienced insomnia during the COVID-19 pandemic. Education level, isolated environment, occupational concerns, and worries about the consequences of COVID-19 have been associated with an increased risk of insomnia among HCWs [15]. As HCWs have been on the frontline of caring for patients affected by COVID-19 since its emergence, they seem to be vulnerable to different psychological consequences. Numerous systematic reviews and meta-analyses have been conducted on the mental health outcomes, especially insomnia, among HCWs during this pandemic, but no single study has combined these results to identify overarching trends or conclusions. Therefore, the present umbrella review of meta-analyses aims to serve as the first and most comprehensive study in this regard. This umbrella review assesses all meta-analyses conducted on the prevalence of insomnia among HCWs around the world to estimate the prevalence of insomnia in this population. The results of this study can serve as a resource for policy-makers or health managers to implement appropriate plans to improve the mental health of HCWs around the world.
2. Materials and methods
In order to conduct this review, we used the Preferred Reporting Items for Systematic Reviews and Meta-analyzes (PRISMA) guidelines [16]. The review protocol was registered and is accessible at the PROSPERO database under the code of CRD42021238985.
2.1. Search strategy in databases
In this study, the search was performed in Scopus, PubMed, Web of Science, and Google Scholar databases using relevant keywords including:
“Insomnia”, “Primary Insomnia”, “Transient Insomnia”, “Secondary Insomnia”, “Sleep Initiation Dysfunction”, Sleeplessness,“Insomnia Disorder”, “Chronic Insomnia”, “Psychophysiological Insomnia”, “Mental Health Disorder”, “Psychiatric Disorder”, “2019 Novel Coronavirus Disease” COVID19, “COVID-19 Pandemic”, “SARS-CoV-2 Infection”, “COVID-19 virus disease”, “2019 Novel Coronavirus Infection”, “2019-nCoV Infection”, “Coronavirus Disease 2019”, “2019-nCoV Disease”, “COVID-19 Virus Infection”, “Health Personnel”, “Health Care Provider,” “Health worker,” “Healthcare Provider,” “Healthcare Worker,” “Health Care Professional,” “Medical Staff,” “Medical worker,” “Systematic Review,” “Meta-Analysis,” “Meta-Analytic”.
At first, using the keywords, search fields, and operators, a search strategy was designed for PubMed. Subsequently, according to the designed strategy, searches were also performed in the other databases. The searches were conducted to obtain studies published in English from January 2020 until the end of January 2021. The following is an example of the search strategy in PubMed. Strategies employed in other databases are noted in Appendix 1.
An example of the search strategy in PubMed:
((insomnia* OR “Primary Insomnia” OR “Transient Insomnia” OR “Secondary Insomnia” OR “Sleep Initiation Dysfunction*” OR Sleeplessness OR “Insomnia Disorder*” OR “Chronic Insomnia” OR “Psychophysiological Insomnia” OR “Mental health Disorder*” OR “Psychiatric Disorder*”) AND (“2019 novel coronavirus disease” OR COVID19 OR “COVID-19 pandemic” OR “SARS-CoV-2 infection” OR “COVID-19 virus disease” OR “2019 novel coronavirus infection” OR “2019-nCoV infection” OR “Coronavirus disease 2019” OR “2019-nCoV disease” OR “COVID-19 virus infection”) AND (“Health Personnel” OR “Health Care Provider*” OR “Health worker*” OR “Healthcare Provider*” OR “Healthcare Worker*” OR “Health care professional*” OR “medical staff” OR “Medical worker*”) AND (“Systematic review”) AND (“meta-analysis” OR “meta-analytic”))
2.2. Eligibility criteria
All meta-analyses reporting the prevalence of insomnia among HCWs during the COVID-19 pandemic were included. The studies addressing the prevalence of sleep disorders in people other than HCWs or those focusing on sleep disorders other than insomnia were excluded.
2.3. Study selection
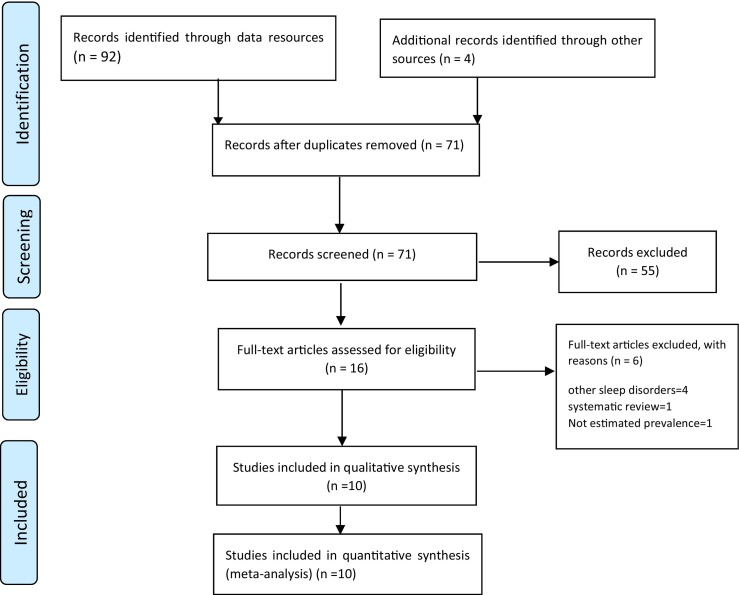
Initially, all 96 studies found in the primary search were inserted into EndNote X7 software. After excluding duplicate articles, 71 studies were screened. The full texts of 16 possibly related studies were independently reviewed by two of the researchers (AS, MG). Ultimately, 10 studies were selected for quality assessment. Fig. 1 demonstrates the steps of study selection.
Fig. 1.
Flowchart of the selection of studies based on PRISM.
2.4. Quality assessment and data extraction
Qualitative evaluation of the selected studies' methodology was independently performed by two researchers using the Assessment of Multiple Systematic Reviews, version 2 (AMSTAR-2) [17]. In order to extract the data, the two researchers independently extracted the required data (the first author's name, the location, the number of subjects, the degree of heterogeneity, and publication) using a checklist designed in Microsoft Word 2016.
2.5. Statistical analysis
The random effects model was used to conduct the meta-analysis of selected studies. The I2 index was used to evaluate the heterogeneity among the studies. The indices of <25%, 25–50%, 50–75%, and > 75% indicate no, moderate, high, and very high heterogeneity, respectively [18]. Publication bias was assessed by the Egger's test, and the data was analyzed using STATA (version 14) software.
3. Results
Overall, 187,506 HCWs were analyzed in this umbrella review. Table 1 shows the specifications and data related to each study.
Table 1.
The Specifications of Studies Included in the Umbrella Review.
| First author | Country | Sample Size (HCWs) |
Prevalence of insomnia | Heterogeneity% I2 | Publication bias | Survey Instrument | Group study |
|---|---|---|---|---|---|---|---|
| Batra [29] | USA | 18,546 | 27.8% (21.4–35.3) | 98.1% | Egger (P = 0.01) Begg (P = 0.03) |
ISI, AIS, PSQI | Doctors and Nurses |
| Krishnamoorthy [30] | India | NA | 37% (32–42) | 92.6% | NA | ISI, AIS | HCWs |
| Pappa [31] | United Kingdom | 33,062 | 34·32% (27·45–41·54) | 98%) | NA | ISI, AIS | Physicians, nurses Other HCWs |
| de Pablo [32] | United Kingdom | 60,458 | 44.5% (38.2–50.9) | 93.179 | NA | Not reported | Nurses, physicians, medical students, social workers |
| Cénat [33] | Canada | 7379 | 36.52(32.99–40.20) | 89.45 | funnel plot (No asymmetric) | ISI.AIS, PSQI | HCWs |
| Luo [34] | China | NA | 32% (25–39) | NA | NA | ISI, PSQI, AIS | HCWs |
| Wu [35] | China | 13,375 | 47.3 (38.8–55.8) | 98.7 | Egger (p = 0.223) | PSQI, ISI | Nurses and physicians |
| Wu [35] | China | 1380 | 31.8 (27.2–36.5) | 37.5 | Egger (p = 0.223) | PSQI, ISI | Other medical staff |
| Dutta [36] | India | 34,021 | 35.8% (28.3–48.1) | 99.2% | NA | ISI, PSQI | Doctors and Nurses, other HCWs |
| Mahmud [37] | Bangladesh | 19,285 | 40.52%. (31.19–49.86) | 99.47% | Egger P = 0.38 |
ISI, AIS, PSQI, PHQ-9 | HCWs |
| Maqbali [38] | Oman | NA | 36 (30-43) | 95% | NA | ISI, AIS, PHQ-15 | Nurses |
NA = Not Applicable, NR = Not reported, HCWs = Healthcare workers, ISI: Insomnia Severity Index, AIS: Athens insomnia scale, PSQI: Pittsburgh sleep quality index, PHQ: Patient Health Questionnaire.
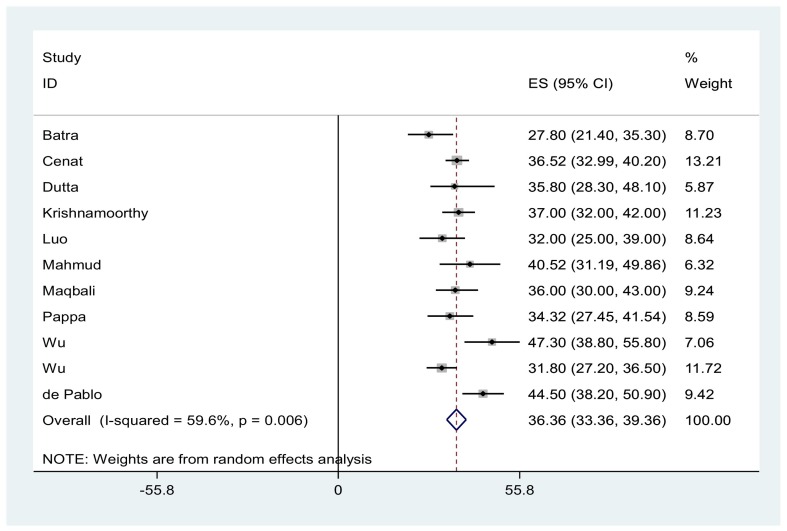
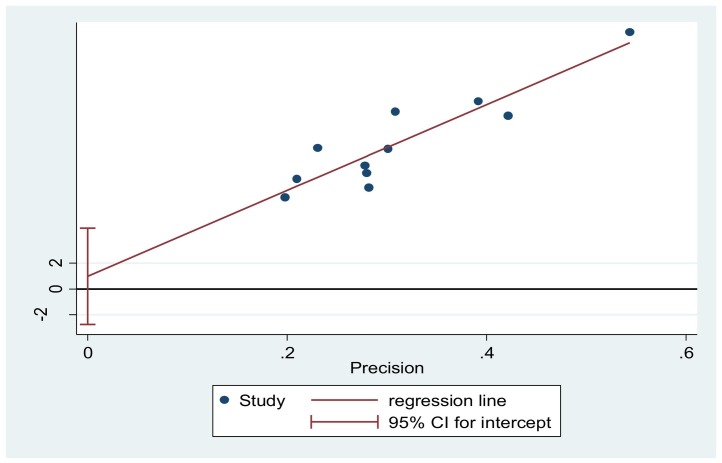
The prevalence of insomnia among HCWs during the COVID-19 pandemic was 36.36% (95% CI: 33.36–39.36, I2 = 59.6%, p = 0.006, Fig. 2 ). The I2 index showed a high heterogeneity between the studies. Based on the results of the Egger's test (p = 0.571), publication bias was insignificant (Fig. 3 ).
Fig. 2.
The forest plot of overall and individual prevalence of insomnia in the Included studies with 95% confidence interval.
Fig. 3.
Publication bias based on Egger Test.
4. Discussion
Based on the findings of this umbrella review, the prevalence of insomnia among HCWs during the COVID-19 pandemic was 36.36% (95% CI: 33.36–39.36). A review by Jahrami et al. [19] showed that the prevalence of sleep disorders was higher in HCWs as compared with the general population (36%vs. 32.3%). The results of a study by Zhou et al. [20] showed that frontline HCWs suffered more from mental disorders than the general population during the COVID-19 pandemic. These findings are consistent with the results of this umbrella review, indicating that the COVID-19 pandemic has been a source of significant psychological stress for HCWs as compared with the general population. In cases of traumatic stress, acute stress suppresses rapid eye movement (REM) sleep and increases the duration of non-REM sleep, which is followed by restorative sleep compensation, increased sleep time and increased REM sleep. However, persistent or repeated chronic stress exposure like COVID-19 may have a more negative impact on sleep, resulting in the presentation of sleep disorders, insomnia and other problems. In the presence of an active the hypothalamic-pituitary-adrenal (HPA) axis, individuals may experience a lighter sleep, increasing awakenings and sleep fragmentation [21].Glucocorticoids are the end-hormones of the HPA axis. Their secretion is regulated by the brain and reflects the overall activity of the stress system which includes the HPA axis, and the arousal and autonomic nervous systems. Activation of the stress system is associated with a repertoire of functions that collectively constitute the “stress syndrome”. Fragmented sleep can subsequently excite the sympathetic catecholamine system and elevate cortisol levels, which eventually results in persistent insomnia [21,22].
This may account for the higher prevalence of sleep disorders among HCWs. These results argue for the urgent implementation of support systems to prevent the psychological distress among HCWs and increase their resilience during this time. Supportive measures that are useful and necessary to reduce job stress include: creating a suitable environment for effective communication, reducing the hours of work shifts and workload, hiring new staff, providing adequate personal protective equipment (PPE) for staff, using mental health professionals for counseling, and setting up counseling lines for easy access to a psychiatrist. Health care workers are encouraged to express their feelings by talking, drawing, singing, exercising, and communicating with colleagues with similar experiences or feelings. They can understand each other better and help out dealing with the problem [23,24]. Previous research has demonstrated a direct correlation between COVID-19-related anxiety, insomnia severity, and suicidality. The likelihood of suicidal ideation has been directly linked to the severity of insomnia [25]. In addition to their association with anxiety and depression, sleep disorders are risk factors for suicidal ideation, attempt, and completion. Accordingly, addressing sleep disorders is vital to reducing suicide and psychiatric disorders among HCWs [26]. The results of an umbrella review by Sahebi et al. [24] showed that the prevalence of anxiety and depression among HCWs were 24.92% and 21.41%, respectively. The results of other studies further support the assertion that the HCWs engaged in caring for COVID-19 patients are more prone to psychiatric disorders such as anxiety, depression, insomnia, and stress compared with other occupational groups. HCWs should be screened for insomnia and other psychological problems and regularly followed up to reduce the risk of suicide. This research demonstrates that mental health resources should be prioritized for HCWs during this pandemic [27,28].
4.1. Limitations
The most important limitation of this study was the high heterogeneity among the selected studies. This was because various studies used different tools and cut-off points. Another limitation of the present study was the lack of reporting the number of participants by some studies. Finally, because the prevalence of insomnia was not separately reported in men and women by most of the studies, it was not possible for us to report the prevalence of insomnia by gender.
5. Conclusion
The results of the present study showed relatively high prevalence of insomnia among HCWs. As insomnia can be associated with other psychological disorders, policymakers and administrators should consider regularly screening for insomnia, as well as other psychological disorders and suicidal ideation, among HCWs. By implementing appropriate supportive measures and timely treatment, it is possible to reduce the incidence of more serious psychological disorders and decrease the incidence of suicide within this population.
Funding
None.
Authors contributions
AS, SM, MT, and MG designed the review, developed the inclusion criteria, screened titles and abstracts, appraised the quality of included papers, and drafted the manuscript. AS, SM, KA, MT, and MG reviewed the study protocol and inclusion criteria and provided substantial input to the manuscript. AS, MG, KA, SM, and MS reviewed the study protocol. AS and MG read and screened articles for inclusion. All authors critically reviewed drafts and approved the final manuscript.
Conflicts of interest statement
The authors declare that they have no competing interests.
Ethical considerations
Not applicable.
Acknowledgments
None.
Appendix 1. Appendix
Table A1.
Using database-appropriate syntax, with parentheses, Boolean operators, and field codes.
| pubmed | ((insomnia* OR “Primary Insomnia” OR “Transient Insomnia” OR “Secondary Insomnia” OR “Sleep Initiation Dysfunction*” OR Sleeplessness OR “Insomnia Disorder*” OR “Chronic Insomnia” OR “Psychophysiological Insomnia” OR “Mental health Disorder*” OR “Psychiatric Disorder*”) AND (“2019 novel coronavirus disease” OR COVID19 OR “COVID-19 pandemic” OR “SARS-CoV-2 infection” OR “COVID-19 virus disease” OR “2019 novel coronavirus infection” OR “2019-nCoV infection” OR “Coronavirus disease 2019” OR “2019-nCoV disease” OR “COVID-19 virus infection”) AND (“Health Personnel” OR “Health Care Provider*” OR “Health worker*” OR “Healthcare Provider*” OR “Healthcare Worker*” OR “Health care professional*” OR “medical staff” OR “Medical worker*”) AND (“Systematic review”) AND (“meta-analysis”[tiab] OR “meta-analytic”)) |
12 |
|---|---|---|
| Scopus | ((ALL(insomnia*) OR ALL(“Primary Insomnia”) OR ALL(“Transient Insomnia”) OR ALL(“Secondary Insomnia”) OR ALL(“Sleep Initiation Dysfunction*”) OR ALL(Sleeplessness) OR ALL(“Insomnia Disorder*”) OR ALL(“Chronic Insomnia”) OR ALL(“Psychophysiological Insomnia”) OR ALL(“Mental health Disorder*”) OR ALL(“Psychiatric Disorder*”)) AND (ALL(“2019 novel coronavirus disease”) OR ALL(COVID19) OR ALL(“COVID-19 pandemic”) OR ALL(“SARS-CoV-2 infection”) OR ALL(“COVID-19 virus disease”) OR ALL(“2019 novel coronavirus infection”) OR ALL(“2019-nCoV infection”) OR ALL(“Coronavirus disease 2019”) OR ALL(“2019-nCoV disease”) OR ALL(“COVID-19 virus infection”)) AND (ALL(“Health Personnel”) OR ALL(“Health Care Provider*”) OR ALL(“Health worker*”) OR ALL(“Healthcare Provider*”) OR ALL(“Healthcare Worker*”) OR ALL(“Health care professional*”) OR ALL(“medical staff”) OR ALL(“Medical worker*”)) AND (ALL(“Systematic review”)) AND (TITLE-ABS(“meta-analysis”) OR ALL(“meta-analytic”))) | 77 |
| Web of science | ((TS = (insomnia*) OR TS = (“Primary Insomnia”) OR TS = (“Transient Insomnia”) OR TS = (“Secondary Insomnia”) OR TS = (“Sleep Initiation Dysfunction*”) OR TS = (Sleeplessness) OR TS = (“Insomnia Disorder*”) OR TS = (“Chronic Insomnia”) OR TS = (“Psychophysiological Insomnia”) OR TS = (“Mental health Disorder*”) OR TS = (“Psychiatric Disorder*”)) AND (TS = (“2019 novel coronavirus disease”) OR TS = (COVID19) OR TS = (“COVID-19 pandemic”) OR TS = (“SARS-CoV-2 infection”) OR TS = (“COVID-19 virus disease”) OR TS = (“2019 novel coronavirus infection”) OR TS = (“2019-nCoV infection”) OR TS = (“Coronavirus disease 2019”) OR TS = (“2019-nCoV disease”) OR TS = (“COVID-19 virus infection”)) AND (TS = (“Health Personnel”) OR TS = (“Health Care Provider*”) OR TS = (“Health worker*”) OR TS = (“Healthcare Provider*”) OR TS = (“Healthcare Worker*”) OR TS = (“Health care professional*”) OR TS = (“medical staff”) OR TS = (“Medical worker*”)) AND (TS = (“Systematic review”)) AND (Ti = (“meta-analysis”) OR TS = (“meta-analytic”))) | 3 |
References
- 1.Lin Y., Hu Z., Alias H., Wong L.P. Quarantine for the coronavirus disease (COVID-19) in Wuhan city: support, understanding, compliance and psychological impact among lay public. J. Psychosom. Res. 2021;144:110420. doi: 10.1016/j.jpsychores.2021.110420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vardanjani A.E., Moayedi S., Golitaleb M. COVID-19 pandemic hemoperfusion therapy versus plasma exchange therapy in intensive care. Iranian Journal of Allergy, Asthma and Immunology. 2020:7–9. doi: 10.18502/ijaai.v19i(s1.r1).2848. [DOI] [PubMed] [Google Scholar]
- 3.Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shanbehzadeh S., Tavahomi M., Zanjari N., Ebrahimi-Takamjani I., Amiri-Arimi S. Physical and mental health complications post-COVID-19: scoping review. J. Psychosom. Res. 2021;110525 doi: 10.1016/j.jpsychores.2021.110525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Badahdah A., Khamis F., Al Mahyijari N., Al Balushi M., Al Hatmi H., Al Salmi I., et al. The mental health of health care workers in Oman during the COVID-19 pandemic. Int. J. Soc. Psychiatry. 2020;67(1):90–95. doi: 10.1177/0020764020939596. 0020764020939596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu C., Pan W., Li L., Li B., Ren Y., Ma X. Prevalence of depression, anxiety, and insomnia symptoms among patients with COVID-19: a meta-analysis of quality effects model. J. Psychosom. Res. 2021:110516. doi: 10.1016/j.jpsychores.2021.110516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rana W., Mukhtar S., Mukhtar S. Mental health of medical workers in Pakistan during the pandemic COVID-19 outbreak. Asian J. Psychiatr. 2020;51:102080. doi: 10.1016/j.ajp.2020.102080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rossi R., Socci V., Pacitti F., Di Lorenzo G., Di Marco A., Siracusano A., et al. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Network Open. 2020;3(5) doi: 10.1001/jamanetworkopen.2020.10185. e2010185-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rashid H., Katyal J. COVID-19 impact on health care workers: revisiting the metrics. Brain, Behavior, and Immunity. 2021;92(2021):205–206. doi: 10.1016/j.bbi.2020.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chirico F., Nucera G., Magnavita N. Protecting the mental health of healthcare workers during the COVID-19 emergency. BJPsych International. 2021;18(1) [Google Scholar]
- 11.Zitting K.-M., Lammers-van der Holst H.M., Yuan R.K., Wang W., Quan S.F., Duffy J.F. Google trends reveals increases in internet searches for insomnia during the 2019 coronavirus disease (COVID-19) global pandemic. J. Clin. Sleep Med. 2021;17(2):177–184. doi: 10.5664/jcsm.8810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Olagunju A.T., Bioku A.A., Olagunju TO, Sarimiye F.O., Onwuameze O.E., Halbreich U. Psychological distress and sleep problems in healthcare workers in a developing context during COVID-19 pandemic: implications for workplace wellbeing. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2021;110:110292. doi: 10.1016/j.pnpbp.2021.110292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.San Martin A.H., Serrano J.P., Cambriles T.D., Arias E.M.A., Méndez J.M., del Yerro Álvarez M.J., et al. Sleep characteristics in health workers exposed to the COVID-19 pandemic. Sleep Med. 2020;75:388–394. doi: 10.1016/j.sleep.2020.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Şahin M.K., Aker S., Şahin G., Karabekiroğlu A. Prevalence of depression, anxiety, distress and insomnia and related factors in healthcare workers during COVID-19 pandemic in Turkey. J. Community Health. 2020;45(6):1168–1177. doi: 10.1007/s10900-020-00921-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang C., Yang L., Liu S., Ma S., Wang Y., Cai Z., et al. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Frontiers in Psychiatry. 2020;11:306. doi: 10.3389/fpsyt.2020.00306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moher D., Liberati A., Tetzlaff J., Altman D.G., Group T Linee guida per il reporting di revisioni sistematiche e meta-analisi: il PRISMA Statement. PLoS Med. 2009;6(7) [Google Scholar]
- 17.Shea B.J., Reeves B.C., Wells G., Thuku M., Hamel C., Moran J., et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. bmj. 2017:358. doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Orlewski J., Orlewska E. Effects of genetic polymorphisms of glutathione S-transferase genes (GSTM1, GSTT1, GSTP1) on the risk of diabetic nephropathy: a meta-analysis. Pol. Arch. Med. Wewn. 2015;125(9):649–658. doi: 10.20452/pamw.3045. [DOI] [PubMed] [Google Scholar]
- 19.Jahrami H., BaHammam A.S., Bragazzi N.L., Saif Z., Faris M., Vitiello M.V. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J. Clin. Sleep Med. 2021;17(2):299–313. doi: 10.5664/jcsm.8930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhou Y., Wang W., Sun Y., Qian W., Liu Z., Wang R., et al. The prevalence and risk factors of psychological disturbances of frontline medical staff in China under the COVID-19 epidemic: workload should be concerned. J. Affect. Disord. 2020;277:510–514. doi: 10.1016/j.jad.2020.08.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhuo K., Gao C., Wang X., Zhang C., Wang Z. Stress and sleep: a survey based on wearable sleep trackers among medical and nursing staff in Wuhan during the COVID-19 pandemic. General Psychiatry. 2020;33(3) doi: 10.1136/gpsych-2020-100260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chrousos G.P., Meduri G.U. Critical COVID-19 disease, homeostasis, and the “surprise” of effective glucocorticoid therapy. Clinical Immunology (Orlando, Fla) 2020;219:108550. doi: 10.1016/j.clim.2020.108550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Magnavita N., Tripepi G., Di Prinzio R.R. Symptoms in health care workers during the COVID-19 epidemic. A cross-sectional survey. International Journal of Environmental Research and Public Health. 2020;17(14):5218. doi: 10.3390/ijerph17145218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sahebi A., Nejati B., Moayedi S., Yousefi K., Torres M., Golitaleb M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: an umbrella review of meta-analyses. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2021;110247 doi: 10.1016/j.pnpbp.2021.110247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Killgore W.D., Cloonan S.A., Taylor E.C., Fernandez F., Grandner M.A., Dailey N.S. Suicidal ideation during the COVID-19 pandemic: the role of insomnia. Psychiatry Res. 2020;290:113134. doi: 10.1016/j.psychres.2020.113134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sher L. COVID-19, anxiety, sleep disturbances and suicide. Sleep Med. 2021;4(1):103–108. doi: 10.1016/j.sleep.2020.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.da Silva F.C.T., Neto M.L.R. Psychiatric symptomatology associated with depression, anxiety, distress, and insomnia in health professionals working in patients affected by COVID-19: a systematic review with meta-analysis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2020;110057 doi: 10.1016/j.pnpbp.2020.110057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sasaki N., Kuroda R., Tsuno K., Kawakami N. The deterioration of mental health among healthcare workers during the COVID-19 outbreak: a population-based cohort study of workers in Japan. Scand. J. Work Environ. Health. 2020;46(6):639–644. doi: 10.5271/sjweh.3922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Batra K., Singh T.P., Sharma M., Batra R., Schvaneveldt N. Investigating the psychological impact of COVID-19 among healthcare workers: a Meta-analysis. Int. J. Environ. Res. Public Health. 2020;17(23):9096. doi: 10.3390/ijerph17239096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Krishnamoorthy Y., Nagarajan R., Saya G.K., Menon V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2020;293:113382. doi: 10.1016/j.psychres.2020.113382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain, Behavior, and Immunity. 2020;88(2020):901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.de Pablo G.S., Serrano J.V., Catalan A., Arango C., Moreno C., Ferre F., et al. Impact of coronavirus syndromes on physical and mental health of health care workers: systematic review and meta-analysis. J. Affect. Disord. 2020;275(2020):48–57. doi: 10.1016/j.jad.2020.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cénat J.M., Blais-Rochette C., Kokou-Kpolou C.K., Noorishad P.-G., Mukunzi J.N., McIntee S.-E., et al. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2020;113599 doi: 10.1016/j.psychres.2020.113599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Luo M., Guo L., Yu M., Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public–a systematic review and meta-analysis. Psychiatry Res. 2020;113190 doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wu T., Jia X., Shi H., Niu J., Yin X., Xie J., et al. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J. Affect. Disord. 2020;281(2021):91–98. doi: 10.1016/j.jad.2020.11.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dutta A., Sharma A., Torres-Castro R., Pachori H., Mishra S. 2020. Mental Health Outcomes Among Healthcare Workers Dealing with COVID-19/SARS-CoV-2 Pandemic: A Systematic Review and Meta-Analysis. Available at SSRN 3633225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mahmud S., Hossain S., Muyeed A., Islam M.M., Mohsin M. 2021. The Global Prevalence of Depression, Anxiety, Stress, and, Insomnia and Its Changes Among Health Professionals During Covid-19 Pandemic: A Rapid Systematic Review and Meta-Analysis. Mahmud, Sultan and Hossain, Sorif and Muyeed, Abdul and Islam, Md Mynul and Mohsin, Md, The Global Prevalence of Depression, Anxiety, Stress, and, Insomnia and Its Changes Among Health Professionals During Covid-19 Pandemic: A Rapid Systematic Review and Meta-Analysis (January 20, 2021) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Al Maqbali M., Al Sinani M., Al-Lenjawi B. Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: a systematic review and meta-analysis. J. Psychosom. Res. 2020;110343 doi: 10.1016/j.jpsychores.2020.110343. [DOI] [PMC free article] [PubMed] [Google Scholar]