Abstract
While dietary supplements are generally “safe,” they must be appropriately consumed as they have different regulatory standards than traditional pharmaceutical medications and require oversight to ensure that a good thing does not become harmful.
Keywords: AKI, acute kidney injury, dietary supplements
While dietary supplements are generally “safe,” they must be appropriately consumed as they have different regulatory standards than traditional pharmaceutical medications and require oversight to ensure that a good thing does not become harmful.

1. INTRODUCTION
Individuals utilize dietary supplements to further optimize one's health. A 71‐year‐old female who consumed 30+ dietary supplements in a complex regimen four times a day presented with AKI requiring dialysis. Patient discontinued her supplement regimen, renal function improved and no longer required dialysis.
2. BACKGROUND
Dietary supplements are widely available and utilized with the intention of optimizing well‐being and/or supplementing nutrition from diet through dietary ingredients (vitamin, mineral, herb or botanical, amino acid, a concentrate, constituent, extract or combination of the ingredients).
3. PURPOSE
To report one of the first cases in the medical literature highlighting the combined toxicity of multiple dietary supplements exacerbating patient's underlying sickness.
4. CASE REPORT
A 71‐year‐old female with a history of hypertension and hypothyroidism was admitted for acute kidney injury, atrial fibrillation with rapid ventricular response, and numerous electrolyte abnormalities. History obtained from the patient's son was noteworthy for her owning a health store and consuming 30+ dietary supplements (DS) in a complex regimen four times daily as depicted in Table 1 and Figure 1, respectively. Patient is reported to have been on this regimen for over 1 year. On admission, white blood cell was elevated (25.3 K/μL), bicarbonate was low (7 mmol/L), blood urea nitrogen was elevated (130 mg/dL), and creatinine markedly elevated (6.2 mg/dL) from her baseline (0.8 mg/dL) checked 6 weeks prior. Electrolytes, phosphorous (6.4 mg/dL), potassium (5.3 mg/dL), and magnesium (5.9 mg/dL), were markedly elevated. Selenium was on the upper level of normal at 154 μg/L (reference 63‐160 μg/L). The patient was compliant with her prescription medicines hydrochlorothiazide, valsartan, and lisinopril for treatment of her hypertension which likely further compounded her acute kidney injury.
Table 1.
Patient's dietary supplement usage per day
| Supplement | Amount consumed daily |
|---|---|
| Raspberry Ketone | 2000 mg |
| Tyrosine (L‐Tyrosine) | 500 mg |
| Ginkgo Biloba | 80 mg |
| Vitamin A | 25 000 IU |
| Selenium | 200 μg |
| Vitamin K2 | 100 μg |
| Chromium | 200 μg |
| Prasterone | 50 mg |
| Green tea leaf extract | 1450 mg |
| St. John's Wort | 1600 mg |
| Glucosamine & Chondroitin Capsule | 3 capsules |
| L‐Carnitine | 1000 mg |
| Rutin | 1350 mg |
| Omega‐3 fish oil | 6000 mg |
| 5‐Hydroxytryptophan | 200 mg |
| Vanadyl sulfate | 10 mg |
| Fenugreek seed extract | 2440 mg |
| Milk thistle seed extract | 300 mg |
| Turmeric root extract | 1600 mg |
| Magnesium oxide | 1000 mg |
| Alpa lipoic acid | 300 mg |
| Lutein | 20 mg |
| Hyaluronic acid | 200 mg |
| Dong Quai | 520 mg |
| Goldenseal root | 500 mg |
| Thiamine B‐1 tablet | 400 mg |
| Methylsulfonylmethane | 4000 mg |
| Super enzyme capsule | 4 Capsules |
| Pyridoxine HCl (Vitamin B6) | 300 mg |
| Cholecalciferol (Vitamin D3) | 10 000 Unit |
Figure 1.
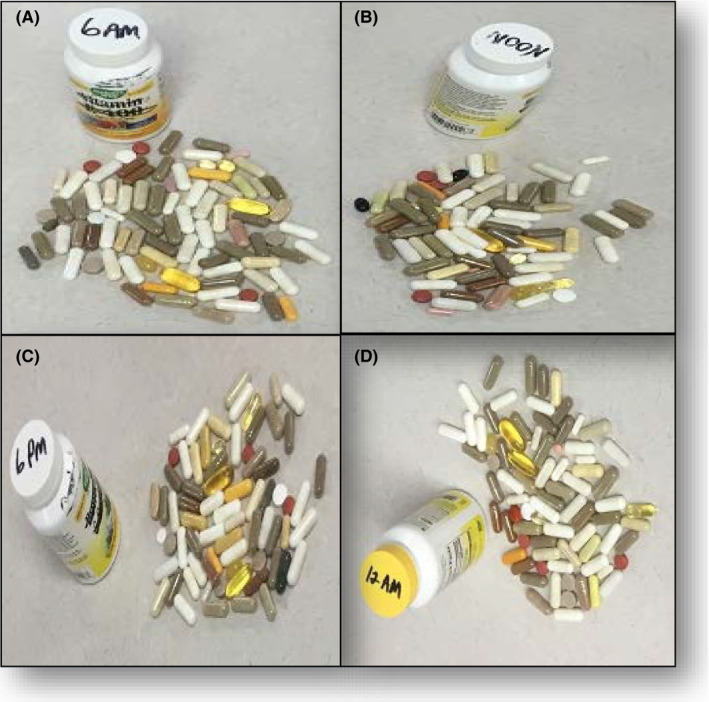
Patient’s supplement consumptions at (A) 06:00, (B) 12:00, (C) 18:00, and (D) 00:00
Hours after admission, patient's urine output decreased becoming anuric. Coupled with her continued acidosis (pH 7.16) that did not respond to a sodium bicarbonate drip, emergent dialysis was initiated. During her hospitalization, her other comorbidities including atrial fibrillation, urinary tract infection, electrolyte abnormalities, and altered mental status resolved. Though her kidney function improved while hospitalized, she required dialysis on discharge. Patient was also recommended to discontinue use of her supplements, and patient agreed.
Patient was transferred to subacute care, and over the next one month, patient's renal function improved. Her creatinine plateaued in the low 3s allowing the patient to discontinue dialysis.
5. DISCUSSION
Dietary supplement (DS) usage has increased to 69.7% adults over the age of 60 with nearly 29% taking 4 or more DS daily and is closely associated with increased utilization when taking ≥3 prescription medicines.1 Motivations for taking a DS include improving overall physical and mental well‐being and for targeted optimization of musculoskeletal and heart health.1 It is well established that DS is utilized to help meet nutritional needs (vitamin D) that cannot be achieved through a well‐balanced diet and are often prescribed similarly to pharmaceutical medications. A recent study found that of those patients taking supplements, only about 5% had all their supplements discussed and documented during an outpatient visit with their primary care provider2 highlighting the widespread passive rather than active management of DS.
In addition, DS is marketed as “natural” which is often perceived to be safe by the public.3 However, numerous herbal and dietary supplements including St. John's wort, echinacea, chromium, glucosamine, vitamins A/C/D, and selenium (all of which our patient consumed) have been associated with acute kidney injury.4 Furthermore, our patient's borderline selenium toxicity likely altered native selenoproteins further exacerbating patient's underlying kidney failure.5 In addition to certain DS being possibly nephrotoxic, supplements can interact with pharmaceutical medications impacting the true therapeutic efficacy such as the case of L‐Tyrosine interacting with levothyroxine. Furthermore, it is less well established how different DS interacts with each other in part due to variable quality and formulations.
Supplements are treated differently than traditional pharmaceutical drugs.6 Dietary Supplements Health and Education Act allows DS to not be regulated as drugs but rather as food with minimal oversight from the Food and Drug Administration (FDA).3 While the FDA requires safety and efficacy documentation prior to market entry for drugs, DS is not held to the same standard and can be brought to the market with relative ease.3 The FDA can remove a DS from the market if the DS provides a danger to public health, but that process requires considerable time and resources to prove danger allowing for questionable products to remain on the market.6 In addition to safety, quality is also not enforced. By law, pharmaceutical companies are required to meet or exceed quality standards established by the nonprofit, private entity, United States Pharmacopeia (USP), whereas manufacturers of DS are only required to exceed USP standards if the manufacturer reports that they follow USP standards.6 More simply, DS does not have to exceed a certain quality threshold.
In conclusion, the widespread usage of DS warrants careful monitoring at all levels to ensure that the goal of trying to maximize one's well‐being does not become deleterious.
CONFLICT OF INTEREST
All authors do not have any conflict of interest.
AUTHOR CONTRIBUTIONS
NM: cared for the patient during patient's hospitalization, contributed to study design, data collection and data interpretation, and literature search, and wrote the first draft of the manuscript including securing the patient consent; MG: cared for the patient during patient's hospitalization, and reviewed and edited the manuscript; LQ: was admitting attending for the patient and cared for the patient during patient's hospitalization, contributed study design, data collection, and data interpretation, and reviewed and edited the manuscript.
ETHICAL APPROVAL
Our institution does not require ethical approval for reporting individual cases or case series.
ACKNOWLEDGMENT
Published with written consent of the patient.
Mehta N, Germain MS, Quiel L. Dietary supplements: When too much of a good thing becomes harmful. Clin Case Rep. 2021;9:e03614. 10.1002/ccr3.3614
REFERENCES
- 1.Gahche J, Bailey R, Potischman N, et al. Dietary supplement use was very high among older adults in the United States in 2011–2014. J Nutr. 2017;147:1968‐1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jang DJ, Tarn DM. Infrequent older adult‐primary care provider discussion and documentation of dietary supplements. J Am Geriatric Soc. 2014;62(7):1386‐1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sax J. Dietary supplements are not all safe and not all food: how the low cost of dietary supplements preys on the consumer. Am J Law Med. 2015;41(2–3):374‐394. [DOI] [PubMed] [Google Scholar]
- 4.Brown A. Kidney toxicity related to herbs and dietary supplements: Online table of case reports. Part 3 of 5 series. Food Chem Toxicol. 2017;107(Pt A):502‐519. [DOI] [PubMed] [Google Scholar]
- 5.Holben D, Smith A. The diverse role of selenium within selenoproteins. A review. J Am Diet Assoc. 1999;99(7):836‐843. [DOI] [PubMed] [Google Scholar]
- 6.Cohen P, Brandt S, Sarma N, et al. Dietary supplements quality analysis tools from the United States Pharmacopeia. Drug Test Anal. 2016;8(3–4):418‐423. [DOI] [PMC free article] [PubMed] [Google Scholar]


