Abstract
The neurological manifestations of SARS-CoV-2 are wide-ranging from simple headache to severe demyelinating brain disease. This is a review of collected case reports of patients with SARS-CoV-2 with neurological manifestations presenting to the Pakistan Institute of Medical Sciences (PIMS). Neurological manifestations associated with SARS-CoV-2 such as encephalitis, acute cerebrovascular disease, encephalitis with chorea, post-COVID myositis and Guillain-Barré Syndrome (GBS) are of great concern but are often overlooked in the presence of life-threatening abnormal vital signs in severely ill SARS-CoV-2 patients. There is a need to diagnose these manifestations at the earliest opportunity to limit long-term consequences and complications. Much research is needed to explore the role of SARS-CoV-2 in causing these neurological manifestations by isolating it either from the cerebrospinal fluid (CSF) or the brain tissue of the deceased on autopsy. We also recommend exploring the risk factors that lead to the development of these neurological manifestations.
Keywords: Covid-19, Stroke, Encephalitis, Guillian Barre Syndrome, Polymyositis
1. Background
SARS-CoV-2 emerged in Wuhan city, China, in December 2019, and rapidly spread to more than 200 countries as a global health pandemic. As of today, there are more than 120 million confirmed cases and more than 2.6 million deaths worldwide.1 SARS-CoV-2 primarily presents as a disease of the respiratory tract, but involvement of many other systems has been reported either in isolation or as a complex multisystem involvement. Mao et al. described a set of relatively common neurological manifestations. The most-frequently reported symptoms included headache and dizziness2 followed by encephalopathy and delirium. Among the complications reported were cerebrovascular accident (CVA), Guillain-Barré syndrome (GBS), acute transverse myelitis, and acute encephalitis. The most common peripheral manifestation was hyposmia. This article presents a narrative review of the collected neurological manifestations and complications of SARS-CoV-2 seen in a single leading tertiary care hospital.
2. Neurological presentations in sars-cov-2 pneumonia
2.1. Guillain-Barré Syndrome
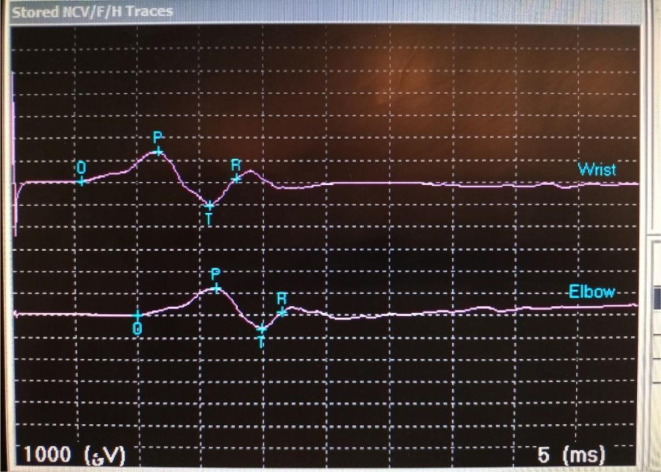
A 45-year-old male with a smoking history of 10 pack years and no other comorbidities presented with 5 days’ history of high-grade fever, cough, body aches, fatigue and shortness of breath (SOB). At presentation in the emergency room (ER), he had a fever of 103.5 °F, a pulse of 112 beats/min, a blood pressure of 110/65 mmHg, and his respiratory rate was 32 breaths/min. Examination findings and high-resolution computed tomography (HRCT) chest (Fig. 1 ) was suggestive of lower respiratory tract infection (LRTI) and reverse transcription polymerase chain reaction (RT-PCR) for SARS-CoV-2 was positive. The relevant treatment was started but on the 3rd day of admission, the patient started showing a weakness in the lower limbs. Examination findings at this time were suggestive of ascending polyneuropathy. A lumbar puncture was refused by his family as the patient was hemodynamically unstable. The weakness further progressed, and nerve conduction studies were performed (Fig. 2 ). A diagnosis of acute inflammatory demyelinating polyneuropathy was made, and the patient was given the treatment options of intravenous immunoglobulin vs plasmapheresis. The patient died on the 4th day of admission despite mechanical ventilation and ICU care. Both GBS and SARS-CoV-2 can lead to respiratory failure requiring mechanical ventilation. In our case, severe SARS-CoV-2 pneumonia exacerbated the patient’s condition and eventually contributed to the cause of death.
Fig. 1.
High Resolution computed tomography (CT) chest scan showing a bilateral ground glass appearance with septal thickening and opacities.
Fig. 2.
Nerve conduction study (NCS) findings showing a distal motor latency.
2.2. Ischemic cerebrovascular vascular accident (CVA)
Case 1: A 67-year-old male, with multiple comorbidities, a doctor by profession, and with no recent travel history, presented to ER complaining of SOB with a mild cough and low-grade fever (undocumented). His vitals on admission were normal with 92% oxygen saturation on room air. The neurological examination at presentation was unremarkable. Based on chest examination and chest x-ray (CXR) findings, PCR confirmed the presence of SARS-CoV-2 infection. Total leukocyte count (TLC) showed a marked lymphopenia and a slight elevation of inflammatory markers. The patient was started on all the relevant treatment (ceftriaxone, azithromycin, methylprednisolone, omeprazole, multivitamin, vitamin D supplementation). On the 4th day, the patient’s GCS suddenly deteriorated to 10/10 (E4 M6 V0) with aphasia and left sided hemiparesis with ipsilateral extensor (upgoing) plantar reflex, and unable to maintain saturation on room air, so patient was immediately put-on oxygen (Nasal Cannula @5L). Initial CT Brain (Fig. 3 ) confirmed middle cerebral artery (MCA) infarct. Upon further deterioration of GCS to 6/15 the next day, a repeat CT brain without contrast demonstrated total anterior circulation infract (TACI). Patient’s life could not be sustained after 12 days in isolation.
Fig. 3.
CT brain scan showing right-sided middle cerebral artery infarct (MCA).
Case 2: A 62-year-old female with a previous history of ischemic heart disease (IHD), type 2 diabetes mellitus (T2DM) and osteoarthritis (OA), presented in ER with SOB and drowsiness. Vitals at presentation were normal with oxygen saturation of 94% on room air. Chest examination findings, CXR and HRCT were all suggestive of a severe LRTI. SARS CoV-2 PCR was positive. Patient was admitted in isolation. Total leucocyte count (TLC) along with inflammatory markers were all raised. Her condition deteriorated progressively and despite dual oxygen therapy, saturation dropped to 82%. She developed hemiplegia on the 6th day of admission and an acute MCA infarct was confirmed on CT. She was given 300 mg of aspirin via nasogastric tube and was moved to ICU and mechanical ventilation was commenced along with the rest of the treatment (ceftriaxone, azithromycin, methylprednisolone, omeprazole, multivitamin, vitamin D supplementation). Due to her poor functional status, the patient was deemed not to be a good candidate for any neurologic intervention or thrombolysis. Despite all efforts, the patient died on the 11th day of hospitalization. As cerebrovascular accidents typically increase the risk of additional infections, especially pneumonia contracted through aspiration, it was assumed that severe SARS-CoV-2 pneumonia together with the added complication of the cerebrovascular accident ultimately led to the demise of the patient.
2.3. Encephalitis3
A 45-year-old male patient with hypertension was brought to ER with generalized tonic-clonic seizures. The patient had a history of high-grade fever (up to 103 °F), headache, dry cough, and altered level of consciousness for the previous 5 days. Neurology was consulted and the patient was noted to have a fever of 102 °F, tachypnoea, tachycardia, and BP of 100/80. Chest examination revealed bilateral coarse crepitation and wheeze and neurological examination reported a GCS of E3M4V3 with all four limbs moving, bilateral extensor plantar reflex, and pupils bilaterally symmetrical but sluggish response to light. Motor and sensory examinations were limited due to the irritability of the patient. SARS-CoV-2 PCR was positive, and HRCT showed bilateral ground glass appearance with extensive opacities (Fig. 4 ). CSF PCR analysis for SARS-CoV-2 was also positive. Empirical treatment ((ceftriaxone, acyclovir, omeprazole, dexamethasone, multivitamin, vitamin D supplementation) for viral encephalitis along with antiepileptic medication (levetiracetam 500 mg BD) were started in an isolation ward. Inflammatory markers were all raised, subsequently the patient continues to deteriorate and was moved onto continuous positive airway pressure (CPAP), but the patient died eventually after 4 days despite all efforts. Deaths due to viral encephalitis are relatively uncommon, but due to the novelty of this virus, it could not be determined whether the cause of death was due to severe SARS-CoV-2 pneumonia or to the spread of the infection to the central nervous system (CNS).
Fig. 4.
CT chest scan showing the typical signs of SARS-CoV-2 pneumonia; bilateral ground glass appearance with septal thickening.
2.4. Encephalitis with chorea4
A 58 year-old male with known hypertension and no travel history was brought to ER with complaints of abnormal movements of the hands and feet and an inability to talk properly for the previous 2 days. His current symptoms were preceded by high grade fever (up to 102 °F), dry cough and headache for 4 days. I/V midazolam was given due to irritability. At presentation the patient was febrile and had tachypnoea with tachycardia. GCS was 15 and he was moving all four limbs. The sensory and motor examination was limited due to persistent abnormal movements. HRCT chest was suggestive of LRTI, and PCR was positive for SARS-CoV-2. Magnetic resonance imaging (MRI) brain with contrast demonstrated no gross lesions except mild periventricular ischemic changes (FAZEKA-II grade), as shown in ( Fig. 5 ). Routine CSF analysis was unremarkable, as were oligoclonal bands (OCBs) and autoimmune profile, but PCR analysis of CSF was positive for SARS-CoV-2. Patient was moved to an isolation ward and the relevant treatment (ceftriaxone, acyclovir, dexamethasone, risperidone, omeprazole) was started. The patient improved daily in terms of oxygen saturation, encephalopathy and abnormal choreiform movement. The patient was discharged from isolation after 14 days with a GCS of E4M6V5 and a Modified Rankin Score of 2.
Fig. 5.
Magnetic resonance imaging (MRI) brain using a FLAIR sequence, showing no changes and reported as microvascular changes.
2.5. Post COVID Myositis
A 19-year-old male, presented with mild flu-like symptoms and generalized body weakness secondary to positive PCR for SARS-CoV-2 from a nasopharyngeal swab. His PCR for SARS-CoV-2 was negative on the 14th day of illness, but 4 days following this, he developed pain in both thighs. After a further 3 days, he developed moderate-to-severe pain in both arms that was persistent but relieved temporarily by painkillers (acetaminophen tablets). After almost 4 weeks, he reported bilateral proximal muscle weakness in both upper and lower limbs. After 3 months, muscular weakness worsened to such an extent that he was unable to stand unaided. Examination revealed decreased power grade 3/5 in bilateral lower limbs. His Creatine phosphokinase (CPK) was 6,338 IU/L and all other laboratory analyses including autoimmune profile were negative. MRI showed hyperintense signals suggesting active myositis in the muscles of the thighs and buttocks (hamstrings and quadriceps), while nerve conduction studies were normal, and electromyography showed fibrillations and sharp waves along with early recruitment and myopathic units in the proximal muscles of the upper and lower limbs. Myopathic changes with focal lymphocytic inflammatory infiltrate were observed on histopathological examination of a biopsy specimen taken from the quadricep. Echocardiography and abdominal ultrasound were normal. He was put on oral folic acid 5 mg/OD, methotrexate 2.5 mg 6tab/week, and prednisolone 5 mg 6tab/BD, along with vitamin D and calcium supplements, and his symptoms improved gradually.
3. Discussion
Neurological symptoms associated with SARS-CoV-2 range from mild a headache and anosmia to debilitating rhabdomyolysis, stroke, myopathies, myositis, and encephalopathies. It is crucial to understand the mechanisms through which the neuromuscular system is affected by SARS-CoV-2 infection. The structure of the virus itself resembles a crown, thus the name Corona virus. The virus is enclosed in an envelope, the surface of which is covered in protein spikes that are responsible for interactions with human cells, leading ultimately to infection. Brain glial tissues express angiotensin-converting enzyme 2 (ACE2), which acts as a cellular receptor for this virus and is why the nervous system can become prone to SARS-CoV-2 infection.5 Infiltration of the CNS via the olfactory system has also been suggested. Muscle injuries are thought to be due to extensive release of pro-inflammatory cytokines.6 Pro-inflammatory cytokines may also provide a key pathogenic pathway resulting in encephalopathy.7 Activated macrophage migration to the CNS has also been observed, causing demyelination.8 Despite the absence of extensive lung involvement in SARS-CoV-2, respiratory failure may occur due to neurogenic involvement.9 An urgent CT brain without contrast should be ordered in all confirmed or suspected SARS-CoV-2 patients exhibiting signs or symptoms suggestive of CNS involvement.3 Further testing, such as MRI, carotid doppler, echocardiography, electroencephalography (EEG), nerve conduction velocity (NCV), EMG, and CT angiogram may also be required on a case-by-case basis. CSF analysed including SARS-CoV-2 PCR may be necessary in SARS-CoV-2 patients showing altered consciousness.3
3.1. Learning Points
-
•
The neurological manifestations associated with SARS-CoV-2 are of particular concern, especially if there is focal neurologic deficit.
-
•
In the presence of severe SARS-CoV-2 pneumonia, neurological symptoms are often overlooked, or at least given lower priority.
-
•
Extensive research is needed to understand the role of SARS-CoV-2 in the expression of neurological symptoms either via CSF analyses or autopsy examination.
-
•
An understanding of the risk factors that contribute to neurological manifestations is also needed.
-
•
Neuropsychological testing and MRI should be used to detect possible permanent sequelae following SARS-CoV-2 infection, and to prognosticate the occurrence of long-term deficits.
Funding source
NA.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethical statement
The study was approved by the institutional review board.
Consent for publication
Patients consented for the study and publication.
Acknowledgement
NA.
References
- 1.https://www.worldometers.info/coronavirus/
- 2.Mao L., Jin H., Wang M., et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77(6):683. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hassan M., Syed F., Mustafa F., Mushtaq H.F., Khan N.U., Badshah M. SARS-CoV-2 infection with pneumonia and stroke. Brain Hemorrhages. 2021 doi: 10.1016/j.hest.2020.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hassan M., Syed F., Ali L., et al. Chorea as a presentation of SARS-CoV-2 encephalitis: a clinical case report. J Mov Disord. 2021;14(3):245–247. doi: 10.14802/jmd.20098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yan R., Zhang Y., Li Y., Xia L.u., Guo Y., Zhou Q. Structural basis for the recognition of SARS-CoV-2by full-length human ACE-2. Science. 2020;367(6485):1444–1448. doi: 10.1126/science.abb2762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Najjar S., Najjar A., Chong D.J., et al. Central nervous system complications associated with SARS-CoV-2infection: integrative concepts of pathophysiology and case reports. J Neuroinflamm. 2020;17(1) doi: 10.1186/s12974-020-01896-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moore J.B., June C.H. Cytokine release syndrome in severe COVID-19. Science. 2020;368(6490):473–474. doi: 10.1126/science.abb8925. [DOI] [PubMed] [Google Scholar]
- 8.Kim T.S., Perlman S. Viral expression of CCL2 is sufficient to induce demyelination in RAG1−/− mice infected with a neurotropic coronavirus. J Virol. 2005;79(11):7113–7120. doi: 10.1128/JVI.79.11.7113-7120.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baig A.M., Wasay M. COVID-19 infection; Loss of taste, smell and neurogenic respiratory failure. Pak J Neurol Sci. 2020;15(1):10. [Google Scholar]