Abstract
Therapy-responsive immune thrombocytopenia and anemia shortly after the second dose of an mRNA-based SARS-CoV-2 vaccine, which was complicated by symptomatic bleeding within a pre-existing brainstem cavernoma, has not been reported.
The patient is a 68yo male who experienced gait disturbance and hypoesthesia of the left face and left upper extremity two days after the second dose of the mRNA-based SARS-CoV-2 vaccine BNT162b2 (Tozinameran). Clinical neurologic exam revealed hypoesthesia of the left face and the left upper extremity and ataxic gait. Blood tests revealed macrocytic anemia and marked thrombocytopenia, interpreted as vaccination induced immune thrombocytopenia (ITP). Cerebral MRI revealed subacute bleeding within a pre-existing solitary cavernoma located in the right cerebellar peduncle. With proceeding resorption of the bleeding, symptoms gradually regressed.
This case shows that SARS-CoV-2 vaccinations may be followed by ITP and bleeding in pre-existing vascular malformations. In order to avoid cavernoma bleeding in patients with SARS-CoV-2 vaccination associated ITP and thrombocyte dysfunction, urgent treatment of ITP is warranted. In order to identify patients at risk for experiencing SARS-CoV-2 vaccination induced ITP, further studies are urgently warranted.
Keywords: Bleeding, Cavernoma, Coagulopathy, SARS-CoV-2 vaccination, Adverse reaction
1. Introduction
Though severe, acute respiratory syndrome coronavirus type-2 (SARS-CoV-2) vaccinations are usually well tolerated, some patients experience side effects. An increasingly recognized complication of SARS-CoV-2 vaccinations is the development of immunologic disorders, such as thyroiditis, transverse myelitis, Guillain-Barre syndrome, Parsonage-Turner syndrome, pancreatitis, or immune thrombocytopenia (ITP).1 Though ITP is thrombogenic, it may also go along with bleedings.2 We report a patient who experienced therapy-responsive ITP and anemia shortly after the second dose of an mRNA-based SARS-CoV-2 vaccine, which itself was complicated by symptomatic bleeding of a brainstem cavernoma.
2. Case description
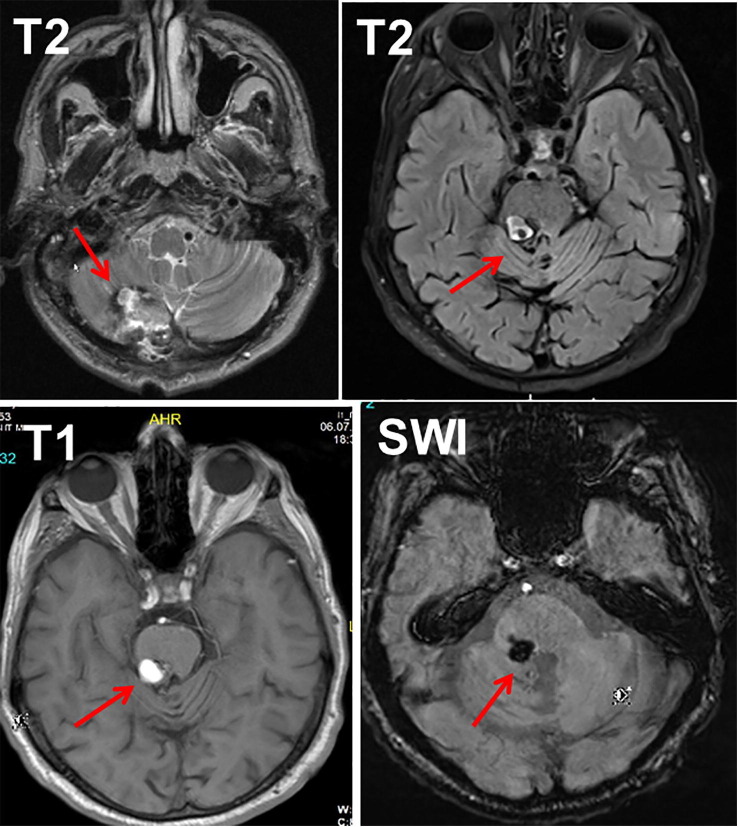
The patient is a 68 years old male who experienced gait disturbance and hypoesthesia of the left face and left upper extremity two days after the second dose of an mRNA-based SARS-CoV-2 vaccine BNT162b2 (Tozinameran). His previous history was positive for resection of a right cerebellar cavernoma 19y earlier, and smoking (80cig/d). Individual and family history was negative for bleeding, thrombocytopenia, or a coagulopathy. He did not take anticoagulants. Clinical neurologic exam revealed hypoesthesia of the left face and the left upper extremity, mild dysarthria, and ataxic gait but was otherwise normal. Electrocardiogram (ECG) and blood pressure were normal. Blood tests revealed macrocytic anemia (erythrocyte count 1.80 T/L (n,4.00–5.65), hemoglobin 8.0 g/dL (n, 12.5–17.2), hematocrit 22.9 % (n, 37.0–49.0%), median cell volume 127.2 fL (n, 80.0–101.0), median cell haemoglobin 44.4 pg (n, 27.0–34.0 pg), thrombocytopenia (91 G/L (n, 160–370 G/L)), folic acid deficiency, and vitamin-B12 deficiency, The thrombocyte count further decreased during hospitalisation to a nadir of 60 G/L six days after admission. Iron levels were normal. Transferrin levels were mildly reduced. The prothrombin time was 88% (n, 70–140%) and the partial thromboplastin time was 29 s (n, 25.1–36.5 s) on admission and remained normal throughout hospitalisation. Unfortunately, the patient was not tested for vWF or factor VIII. Magnetic resonance imaging (MRI) of the brain revealed subacute bleeding of a solitary cavernoma located in the right cerebellar peduncle (Fig. 1 ). Malignoma screening revealed a colonic adenoma, which was successfully resected, and multiple intrapulmonary lesions, too small for immediate biopsy. Under supplementation of folic acid and vitamin-B12, physiotherapy, and speech therapy since admission, neurological deficits steadily improved without any relapse until discharge. Follow-up CT 10 days after admission showed gradual resorption of the bleeding, The patient was recommended to undergo a second cavernoma resection but he did not consent with this proposal so far.
Fig. 1.
T1- and T2-weighted and SWI cerebral MRI images (upper right, lower left and right) on admission showing a subacute bleeding within a cavernoma located in the right cerebellar peduncle. The MRI of the upper left panel shows the condition after resection of right cerebellar cavernoma.
3. Discussion
The presented patient is interesting for bleeding of a cavernoma presumably triggered by a SARS-CoV-2 vaccination induced ITP and thrombocyte dysfunction. Bleeding has been repeatedly reported as a complication of SARS-CoV-2 vaccinations.3 The EudraVigilance European database listed 33 respectively 151 serious adverse events (SAE) with regard to ITP bleeding per one million doses in the BNT162b2 vaccine.4 The number of SAEs related to cerebral or splanchnic venous thrombosis or ITP amounted to 4 SAEs and 0.4 deaths/1 million doses of the BNT162b2 vaccine.4 The pathophysiology background of bleeding after SARS-CoV-vaccinations is poorly understood but it is speculated that antibodies directed against thrombocyte surface proteins may impair their function why they are progressively removed from the blood. In addition to ITP, the generation of coagulation factors may be decreased, such as with acquired Willebrand disease5 or acquired hemophilia-A.6 Bleeding in the index patient was most likely due to a combination of immune-mediated thrombocytopenia, thrombocyte dysfunction, and possibly reduced levels of coagulation factors as other possible causes were excluded. Vitamin-B12 deficiency was largely excluded as the cause of thrombocytopenia as previous blood tests showed anemia but normal thrombocyte counts and because thrombocytopenia declined during hospitalization despite vitamin-B12 supplementation.
In conclusion, this case shows that SARS-CoV-2 vaccinations may be followed by ITP and bleeding in pre-existing vascular malformations. To avoid cavernoma bleeding in patients with SARS-CoV-2 vaccination associated ITP and thrombocyte dysfunction, urgent treatment of ITP is warranted. In order to identify patients at risk for experiencing SARS-CoV-2 vaccination induced ITP, further studies are urgently warranted.
Declarations
Author contribution: corresponding author: design, literature search, discussion, first draft, critical comments.
Funding: No funding was received.
Informed consent: was obtained.
The study was approved by the institutional review board.
Financial disclosures: none.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Suvvari T.K., Rajesh E., D Silva R.G., Corriero A.C., Kutikuppala L.V.S. SARS-CoV-2 vaccine-induced prothrombotic immune thrombocytopenia: Promoting awareness to improve patient-doctor trust. J Med Virol. 2021 doi: 10.1002/jmv.27176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Helms J.M., Ansteatt K.T., Roberts J.C., et al. Severe, Refractory Immune Thrombocytopenia Occurring After SARS-CoV-2 Vaccine. J Blood Med. 2021;Volume 12:221–224. doi: 10.2147/JBM.S307047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gessler F., Schmitz A.K., Dubinski D., et al. Neurosurgical Considerations Regarding Decompressive Craniectomy for Intracerebral Hemorrhage after SARS-CoV-2-Vaccination in Vaccine Induced Thrombotic Thrombocytopenia-VITT. J Clin Med. 2021;10(13):2777. doi: 10.3390/jcm10132777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cari L., Fiore P., Naghavi Alhosseini M., Sava G., Nocentini G. Blood clots and bleeding events following BNT162b2 and ChAdOx1 nCoV-19 vaccine: An analysis of European data. J Autoimmun. 2021;122:102685. doi: 10.1016/j.jaut.2021.102685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Portuguese A.J., Sunga C., Kruse-Jarres R., Gernsheimer T., Abkowitz J. Autoimmune- and complement-mediated hematologic condition recrudescence following SARS-CoV-2 vaccination. Blood Adv. 2021;5(13):2794–2798. doi: 10.1182/bloodadvances.2021004957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Radwi M., Farsi S. A case report of acquired hemophilia following COVID-19 vaccine. J Thromb Haemost. 2021;19(6):1515–1518. doi: 10.1111/jth.15291. [DOI] [PMC free article] [PubMed] [Google Scholar]