Abstract
Objective:
To examine the extent to which colloquial phrases used to describe opioid-exposed mother-infant dyads affects attitudes towards mothers with opioid use disorder (OUD) to assess the role stigmatizing language may have on the care of mothers with OUD.
Methods:
We employed a randomized, cross-sectional, case vignette of an opioid-exposed dyad, varying on two factors: (1) language to describe newborn (“substance-exposed newborn” v. “addicted baby”); and (2) type of maternal opioid use (injection heroin v. non-medical use of prescription opioids). Participants were recruited using an online survey platform. Substance-related stigma, punitive-blaming, and supportive scales were constructed to assess attitudes. Two-way analyses of variance were conducted to determine mean scale differences by vignette. Post-hoc analyses assessed individual item-level differences.
Results:
Among 1,227 respondents, we found a small statistical difference between language and opioid type factors for the supportive scale only (F=4.31, η2 = .004, p=0.038), with greater agreement with supportive statements when describing injection heroin use, compared to prescription opioid use, for the “substance-exposed newborn” vignette only. In post-hoc analyses, greater than 85% of respondents agreed the mother was “responsible for her opioid use,” her “addiction was caused by poor choices,” and that she “put her baby in danger.”
Conclusion:
We found no major differences in attitudes regardless of vignette received. Overall, respondents supported opportunities for maternal recovery yet blamed women, describing mothers as culpable for causing harm to their newborn, showcasing internally conflicting views. These views could contribute to ongoing stigma and avoidance of care among pregnant women with OUD.
Introduction:
Addiction medicine and public health experts have long urged for use of person-centered, medically accurate terminology to describe people with substance use disorders, including infants born to women with opioid use disorder.1,2 Person-centered language prioritizes describing the individual first rather that a specific disease process, e.g. “a women with an opioid use disorder”, rather than an “addicted woman.”3 Additionally, describing a newborn with in-utero opioid exposure as born “addicted to opioids” is not medically accurate, as addiction involves continued use of a substance despite knowledge of harmful consequences; rather infants experience physiologic dependence after delivery.4,5 Despite this, over the last decade, thousands of news media citations have been published using the phrase “drug addicted baby” or “baby born addicted” to describe newborns exposed in-utero to opioids.6,7 News media coverage using medically inaccurate language can influence public opinion and increase public fear and perception of the severity of an issue.8
A growing body of literature suggests that stigma is perpetuated by negative language which introduces an implicit cognitive bias.1,9 For example, using non-person-centered language (e.g., describing a person with a substance use disorder (SUD) as a “drug addict” or “substance abuser”) is associated with greater perceptions of dangerousness, belief in personal culpability for addiction, and greater support for punitive measures compared with use of person-centered language such as a “person with a substance use disorder.” 10–12 Greater stigma, or negative views held towards individuals with substance use disorder, has been identified as a barrier to substance use treatment.13–16
Pregnant women with substance use disorder commonly report fear of a punitive response by providers as a barrier to treatment.17,18 Use of medically inaccurate language such as “drug addicted baby” may increase perceptions of blame toward the mother, increasing maternal shame and impeding mothers’ disclosure of their OUD. Such increased shame may also inhibit treatment seeking that could ultimately help both the mother and their child.19,20 Despite strong opinion about the use of inaccurate and potentially stigmatizing language describing children newborn to mothers with OUD, little is known from a systematic, empirical standpoint about the extent to which use of different terminology actually influences attitudes toward mothers with an OUD.21
To this end, the current study was designed to inform this discussion about the impact of medically inaccurate language by employing a randomized design. Our principal aim was to examine how colloquial phrases commonly used by the news media affect the endorsement of substance-related stigma, punitive-blaming, or supportive statements. Using the same vignette but substituting different terms to describe an opioid-exposed newborn allowed us to investigate different attitudes that may be uniquely elicited by exposure to each term. Secondarily, given that prescription opioids are socially and medically sanctioned and allied with a positive medical intent (even if used for non-medical purposes) whereas heroin use is considered more clearly socially deviant and thus marginalized, we investigated whether the type of opioid use (i.e., injection heroin use v. non-medical use of prescription opioids) impacts stigmatizing beliefs.
We hypothesized that stigmatizing language (i.e., “addicted baby” and injection heroin use) would be associated with more agreement with statements that support substance-related stigma and align with a punitive-blaming approach to the mother’s OUD when compared to medically accurate language and non-medical use of prescription opioids.
Methods:
Recruitment, survey platform
We used Amazon’s Mechanical Turk (MTurk), an online, crowdsourced marketplace, to recruit individuals ≥ 18 years old living in the United States. Compared to samples from in-person and online study recruitment, MTurk participants have been found to be more representative of the United States population, more attentive, and responses have not significantly differed from those acquired through in-person or other online recruitment.22,23 Potential participants read the description of our study on MTurk and, if they were interested in participating, were directed to our survey hosted on Qualtrics, a secure survey platform.24
The “evenly present elements” tool was utilized within Qualtrics randomizer to ensure an even number of participants were randomized to receive each of the four vignettes.24 Participants first reviewed the vignette, then answered two comprehension questions to ensure participants had read the vignette and had a basic understanding of what opioids are. Next, participants responded to the survey questions and demographic data was collected. The Partners Healthcare Internal Review Board reviewed this study and determined it exempt from full review. All surveys were completed in August of 2018.
Vignettes
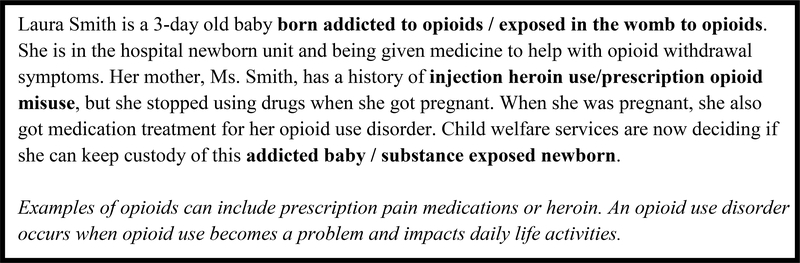
The vignette first describes a newborn with symptoms of opioid withdrawal. Her mother has received medication used to treat OUD throughout her pregnancy. The description specified that the mother did not continue non-prescribed opioid use during their pregnancy. The vignettes differed on two factors each with two levels (i.e., 2 × 2): Language Factor – language used to describe the newborn (stigmatizing description: “addicted baby” vs. medically accurate description: “substance-exposed newborn”); and Opioid type Factor – type of opioid use (injection heroin or non-medical use of prescription opioids). Vignettes were modeled off prior research by Kelly and colleagues depicting a character described as a “substance abuser” or a person with “a substance use disorder.”10 Figure 1 shows the vignette text and the different text options used for each factor. The vignette and survey questions (described in the next section) were beta-tested for face validity, revised based on feedback from 10 individuals with a minimum of bachelor’s level education, and edited by a patient educator for comprehension at an 8th grade reading level.
Figure 1:
Vignette
Surveys
Substance-related stigma items.
Following the vignette, participants rated their agreement using a 6-point Likert scale (“strongly disagree” to “strongly agree”) with four statements about perceived stigma towards addiction. Questions focused on the participants’ own lives and how they would interact with individuals who have a substance use disorder.25
Punitive-Blaming and Supportive items.
Statements were adapted from published and validated survey tools used to assess attitudes towards people with substance use disorders. 10,25–29 The eight punitive-blaming statements focused on maternal culpability, maternal abilities to parent, and whether the mother should receive punishment. The eight supportive statements focused on treatment resources and recovery. The full list of questions are included in Table 4.
Table 4:
Proportion of Any Agreement Across Both Factors (Post-hoc Analysis) (N=1,227)
| “Addicted Baby” | “Substance Exposed” | ||||
|---|---|---|---|---|---|
|
|
|||||
| Total | IV Heroin | Prescription Opioids | IV Heroin | Prescription Opioids | |
| Variable | N = 1227 (%) | n = 298 (%) | n = 308 (%) | n = 309 (%) | n = 312 (%) |
|
| |||||
| N (%) |
% (95% CI) |
% (95% CI) |
%
(95% CI) |
%
(95% CI) |
|
| Substance-related Stigma Sscale (α = .715) | |||||
|
| |||||
| Most people would be willing to date someone who has been treated for substance use | 579 (47.2) |
47.3 (41.7 – 53.0) |
49.7 (44.1 – 55.2) |
43.0 (37.6 – 48.6) |
48.7 (43.2 – 54.3) |
| Most people would willingly accept someone who has been treated for substance use as a close friend | 778 (63.0) |
66.8 (61.2 – 71.9) |
63.3 (57.8 – 68.5) |
58.9 (53.3 – 64.3) |
64.7 (59.3 – 69.9) |
| Most people would hire someone who has been treated for substance use to take care of their children | 346 (28.2) |
26.9 (22.1 – 32.2) |
27.2 (22.6 – 32.5) |
26.9 (22.2 – 32.1) |
31.7 (26.8 – 37.1) |
| Most people think less of a person who has been in treatment for substance use | 1005 (81.9) |
81.8 (77.1 – 85.9) |
84.4 (79.9 – 88.1) |
82.5 (77.9 – 86.4) |
78.9 (74.0 – 83.0) |
|
| |||||
| Punitive-Blaming Scale (α = .828) | |||||
|
| |||||
| Ms. Smith has acted selfishly in becoming pregnant given her opioid use disorder. | 773 (63.0) |
64.4 (58.8 – 69.7) |
64.9 (59.4 – 70.1) |
62.1 (56.6 – 67.4) |
60.6 (55.1 – 65.9) |
| Ms. Smith is responsible for her opioid use. | 1096 (89.3) |
90.6 (86.7 – 93.4) |
86.4 (82.1 – 89.8) |
91.3 (87.6 – 93.9) |
89.1 (85.1 – 92.1) |
| Ms. Smith’s addiction is caused by poor choices she has made. | 1043 (85.0) |
85.6 (81.1 – 89.1) |
84.1 (79.6 – 87.8) |
89.0 (85.0 – 92.0) |
81.4 (76.7 – 85.4) |
| Ms. Smith should be required to provide a urine sample to evaluate for current drug use. | 1077 (87.8) |
90.3 (86.3 – 93.2) |
87.0 (82.8 – 90.3) |
88.7 (84.6 – 91.8) |
85.3 (80.9 – 88.8) |
| Ms. Smith should be punished for her history of opioid use. | 448 (36.5) |
37.6 (32.3 – 43.2) |
38.3 (33.1 – 43.9) |
32.0 (27.1 – 37.5) |
38.1 (32.9 – 43.7) |
| Child protective services should require Ms. Smith to attend a drug treatment program. | 1099 (89.6) |
92.3 (88.7 – 94.8) |
87.3 (83.1 – 90.6) |
91.2 (87.6 – 93.9) |
87.5 (83.4 – 90.7) |
| Ms. Smith has put her baby in danger. | 1078 (87.9) |
88.6 (84.5 – 91.7) |
87.7 (83.5 – 90.9) |
88.7 (84.6 – 91.8) |
86.5 (82.3 – 89.9) |
| Ms. Smith should not be allowed to keep custody of her baby. | 406 (33.1) |
38.9 (33.6 – 44.6) |
34.1 (29.0 – 39.4) |
26.2 (21.6 – 31.4) |
33.3 (28.3 – 38.8) |
|
| |||||
| Supportive Scale (α = .835) | |||||
|
| |||||
| Ms. Smith has an illness. | 994 (81.0) |
80.9 (76.0 – 85.0) |
81.2 (76.4 – 85.2) |
83.5 (78.9 – 87.2) |
78.5 (73.6 – 82.7) |
| Ms. Smith could benefit from seeing a therapist. | 1129 (92.0) |
91.3 (87.5 – 94.0) |
90.9 (87.2 – 93.7) |
96.4 (93.7 – 98.0) |
89.4 (85.5 – 92.4) |
| Ms. Smith can recover from her addiction. | 1135 (92.5) |
91.3 (87.5 – 94.0) |
94.5 (91.3 – 96.5) |
93.2 (89.8 – 95.5) |
91.0 (87.3 – 93.7) |
| Ms. Smith should be offered parenting classes to help care for her baby. | 1117 (91.0) |
91.6 (87.9 – 94.3) |
90.6 (86.8 – 93.4) |
91.9 (88.3 – 94.5) |
90.1 (86.2 – 92.9) |
| Ms. Smith should receive support getting treatment while her newborn is being monitored for withdrawal symptoms. | 1147 (93.5) |
94.0 (90.6 – 96.2) |
93.8 (90.5 – 96.0) |
95.8 (92.9 – 97.5) |
90.4 (86.6 – 93.2) |
| Ms. Smith should get help continuing her medication treatment after giving birth. | 1138 (92.7) |
93.0 (89.4 – 95.4) |
91.9 (88.3 – 94.5) |
95.5 (92.5 – 97.3) |
90.7 (86.9 – 93.5) |
| Ms. Smith can be a good mother even with her history of drug use. | 1023 (83.4) |
83.9 (79.3 – 87.6) |
82.1 (77.5 – 86.0) |
86.1 (81.8 – 89.5) |
81.4 (76.7 – 85.4) |
| Mothers like Ms. Smith can successfully raise children. | 1006 (82.0) |
82.2 (77.5 – 86.2) |
80.5 (75.7 – 84.6) |
83.5 (78.9 – 87.2) |
81.7 (77.1 – 85.6) |
n.b.
indicates α = Cronbach alpha for each scale
Demographics.
Information regarding age, gender, marital status, education level, income, and employment was collected. Participants were asked two questions about experiences with addiction themselves or among their close friends and family. The full list of items is included in Table 1.
Table 1:
Survey Participant Characteristics, N = 1227
| Total Sample N = 1227 (%) |
“Addicted Baby” | “Substance Exposed” | p-value | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||
| IV Heroin | Prescription Opioids | IV Heroin | Prescription Opioids | ||||||||
| Variable | n = 298 (%) | n = 308 (%) | n = 309 (%) | n = 312 (%) | |||||||
|
|
|||||||||||
| Age | .170 | ||||||||||
| 18 – 24 | 121 | (9.9) | 25 | (8.4) | 33 | (10.7) | 35 | (11.3) | 28 | (9.0) | |
| 25 – 34 | 554 | (45.2) | 135 | (45.3) | 151 | (49.2) | 131 | (42.4) | 137 | (43.9) | |
| 35 – 44 | 279 | (22.8) | 57 | (19.1) | 66 | (21.5) | 80 | (25.9) | 76 | (24.4) | |
| 45+ | 272 | (22.2) | 81 | (27.2) | 57 | (18.6) | 63 | (20.4) | 71 | (22.8) | |
| Missing | 1 | 1 | |||||||||
| Gender | .764 | ||||||||||
| Men | 601 | (49.0) | 150 | (50.3) | 142 | (46.1) | 152 | (49.2) | 157 | (50.3) | |
| Women | 624 | (50.9) | 148 | (49.7) | 165 | (53.6) | 156 | (50.5) | 155 | (49.7) | |
| Other | 2 | (.2) | 0 | (.0) | 1 | (.3) | 1 | (.3) | 0 | (.0) | |
| Marital Status | .297 | ||||||||||
| Married or in a domestic partnership | 624 | (50.9) | 160 | (53.7) | 149 | (48.4) | 148 | (47.9) | 167 | (53.5) | |
| Single, separated, divorced, or widowed | 603 | (49.1) | 138 | (46.3) | 159 | (51.6) | 161 | (52.1) | 145 | (46.5) | |
| Education | .521 | ||||||||||
| High school graduate or less | 141 | (11.5) | 36 | (12.1) | 43 | (14.0) | 34 | (11.0) | 28 | (9.0) | |
| College graduate, some college, associates | 859 | (70.0) | 211 | (70.8) | 207 | (67.2) | 221 | (71.5) | 220 | (70.5) | |
| Some graduate school, graduate degree | 227 | (18.5) | 51 | (17.1) | 58 | (18.8) | 54 | (17.5) | 64 | (20.5) | |
| Income | .689 | ||||||||||
| Less than 29999 | 408 | (33.3) | 100 | (33.6) | 104 | (33.8) | 103 | (33.3) | 101 | (32.4) | |
| 30000–59999 | 462 | (37.7) | 109 | (36.6) | 125 | (40.6) | 118 | (38.2) | 110 | (35.3) | |
| More than 60000 | 357 | (29.1) | 89 | (29.9) | 79 | (25.6) | 88 | (28.5) | 101 | (32.4) | |
| Employment Status | .838 | ||||||||||
| Not working or prefer not to answer | 170 | (13.9) | 41 | (13.8) | 39 | (12.7) | 47 | (15.2) | 43 | (13.8) | |
| Working | 1057 | (86.1) | 257 | (86.2) | 269 | (87.3) | 262 | (84.8) | 269 | (86.2) | |
| Personal Experience with Drug Problem (Yes) | 170 | (13.9) | 44 | (14.8) | 40 | (13.0) | 33 | (10.7) | 53 | (17.0) | .134 |
| Family or Friend Experience with a Drug Problem (Yes) | 587 | (47.8) | 142 | (47.7) | 141 | (45.8) | 145 | (46.9) | 159 | (51.0) | .604 |
n.b. p-value for chi-square tests
Analysis
The frequencies of each demographic characteristic were calculated for participants receiving each of the 4 vignettes and compared using Pearson’s chi-square tests to evaluate randomization. For each scale, participant responses were averaged to produce a single mean scale score. Correlation between the three scales was assessed using a Pearson product-moment correlation. Scores were compared using two-way analyses of variance (ANOVA) to assess the effect of each factor and their potential interaction. Internal consistency of each scale was assessed using Cronbach’s alpha.30 To address the potential impact of skewing in the scale distributions, we also assessed the data with the punitive-blaming scale scores inverse log transformed and the supportive scale scores log transformed. Because there was no difference in the pattern of results, the non-transformed results are presented to ease interpretability. Finally, in addition to potential differences in the mean scale scores we examined potential differences in responses to individual questions in post-hoc analysis. To extend the work from Kelly and colleagues31 who dichotomized their Likert scale responses, we characterized each statement response as either in agreement or disagreement and effects of the two factors and their potential interaction were assessed using factorial logistic regression. SAS Version 9.4 was used for statistical analyses.32
Results:
Cohort Characteristics
There were 1,527 participants who participated in the survey. Participants who missed either of the two comprehension questions, did not complete the survey or completed the survey in under 100 seconds were excluded from the analysis (n =300). The final analytic sample included 1,227 participants (Supplemental Figure 1).
Overall, 45.2% of the participants were between 25–34 years of age, 70.2% had some college education, 86.2% reported some type of employment, 33% made less than $30,000, and there was an even breakdown of participants by gender and marital status. In our sample 13.9% reported having ever had an alcohol or drug problem and 47.8% reported family or close friends have had one. There were no significant differences between participants across vignette received, indicating that the randomization across demographic variables was adequate (Table 1).
Survey Properties
The substance-related stigma scale had adequate reliability (α = .715). The punitive-blaming (α = .828) and supportive (α = .835) scales had good reliability. The three scale scores were very weakly correlated using Pearson correlation (stigma/punitive R=0.036, stigma/supportive R=0.048, supportive/punitive R=−0.044).
Differences across scales
Two-way ANOVAs were conducted to examine the independent effect of each factor on scale means. There was a statistically significant interaction between the Language Factor and Opioid type Factor for the supportive scale only, p = .038, η2 = .004. Comparing across those receiving the “addicted baby” vignette, there was no difference when participants received either type of opioid use (Estimated Marginal Mean (EMM) = 4.8, SE = .04 for both heroin and prescription opioids). Among those receiving the “substance exposed” vignette, participants who also received the prescription opioid as opioid type (EMM = 4.7, SE = .04) endorsed less agreement with supportive statements compared to participants who received injection heroin as opioid type (EMM = 4.9, SE = .04). There were no other significant interactions when comparing the substance-related stigma scale and punitive-blaming scale (Table 2).
Table 2:
Two-way ANOVA Results Comparing Stigma Scale Means by Factor (N=1,227)
| Scales | F * | partial η2 | p-value |
|---|---|---|---|
| a. Substance-related Stigma | |||
| Language Factor | .01 | <.001 | .942 |
| Opioid type Factor | 1.52 | .001 | .218 |
| Language Factor x Opioid type Factor | 1.79 | .001 | .181 |
|
| |||
| b. Punitive-Blaming | |||
| Language Factor | 2.88 | .002 | .090 |
| Opioid type Factor | 1.01 | .001 | .315 |
| Language Factor x Opioid type Factor | .13 | <.001 | .714 |
|
| |||
| c. Supportive | |||
| Language Factor | .28 | <.001 | .600 |
| Opioid type Factor | 1.42 | .001 | .233 |
| Language Factor x Opioid type Factor | 4.31 | .004 | .038 |
n.b.
Degrees of Freedom = 1, 1223;
Language Factor - language used to describe the newborn (Addicted Baby or Substance Exposed Infant); Opioid type Factor - type of opioid use (IV Heroin or Prescription Opioid)
Post-hoc exploratory item-level analysis
Overall, less than 30% of participants agreed that most people would hire someone who had been treated for their substance use disorder to take care of their children. Just over half agreed that that most people would be willing to date someone who has been treated for substance use disorder. More than 85% of the respondents were in agreement that Ms. Smith was “responsible for her opioid use”, that her “addiction is caused by poor choices”, that “child welfare services should require her to attend drug treatment”, that she “should be required to provide a urine sample”, and that she has “put her baby in danger.” These responses were in contrast to over 80% of respondents agreeing that Ms. Smith has “an illness,” that she “can recover from her addiction,” she “can be a good mother even with her history of drug use,” and can “successfully raise children” (Table 4).
Agreement with the statement that “Ms. Smith should not be allowed to keep custody of her baby” was low across vignettes (33.1% in agreement). For this question there was a statistically significant interaction between the Language Factor and Opioid type Factor, Wald χ2 = 5.07, p = 0.024. (Supplemental Table). Looking at those who received the injection heroin as type of opioid use, agreement that the mother should lose custody was greatest in the “addicted baby” (38.9%) compared to “substance exposed newborn” and injection heroin vignette (26.2%) as shown in Table 4.
For type of OUD, individuals who received the vignette where the mother had a history of injection heroin use were more likely to agree with the following statements: Ms. Smith’s addiction was caused by poor choices she has made, she would benefit from seeing a therapist, she should receive support getting treatment during newborn hospitalization, and that she should get help continuing her medication treatment after delivery (p < .05). (Data shown in Supplemental Table). There was a statistically significant interaction between the Language Factor and Opioid type Factor for the question of whether Ms. Smith would benefit from seeing a therapist, Wald χ2 = 5.98, p = 0.015. Among those receiving the substance-exposed newborn vignette, 96.4% of those receiving the injection heroin use language were in agreement that a therapist would be beneficial compared with 89.4% of those receiving the prescription opioids language.
Discussion:
This study examined the impact of exposure to randomly assigned terms describing a mother who received medications to treat her OUD during pregnancy that varied by description of the newborn and the type of maternal opioid use. In our primary analysis, the type of language used to describe opioid-exposed infants did not significantly impact respondent views across our three scales. For individuals receiving the “substance exposed newborn” vignette, we identified a small, but statistically greater agreement with supportive statements among those who also received injection heroin as the type of opioid used compared with non-medical use of prescription opioids. This was not supported across the other two scales, and was contrary to our hypothesis that prescription opioid use would garner more supportive responses than injection heroin use. In responses to the item-level questions, the overwhelming majority of individuals agreed with the supportive statements such as engaging in recovery and parenting supports for a mother with opioid use disorder, yet at the same time they endorsed agreement with punitive-blaming views such as mandated treatment and a personal responsibility for her disease of addiction.
Similar to prior survey research on stigma and OUD in the general population, we found that a high proportion of respondents held negative and stigmatizing views towards people with addiction, such as endorsing that a mother who used drugs is “responsible for her opioid use” (89.4%).33,34 We found that less than one third of people would hire someone who has been treated for a substance use disorder to care for their children whereas only approximately half would befriend or date such a person. This deep stigma towards individuals with a history of addiction was similar to college students’ replies to the same questions in a psychometric study assessing the perceived stigma scale.35 Unique to our vignette, and regardless of descriptive terms used, we found there was also strong support for the biomedical model of addiction and the belief that recovery is possible. However, when substance-use recovery intersected with parenting, views were at times contradictory. Most respondents felt the mother – who in our vignette ceased using non-prescribed opioids when she found out she was pregnant and received medication for her opioid use disorder – was “putting her baby in danger.” One third of individuals felt that the mother should not be allowed to keep custody of her newborn and more than half felt she had acted selfishly in becoming pregnant. Our findings suggest that pregnant and parenting women in recovery face a unique social stigma, rooted in both external and internal pressures to meet societal expectations of the ideal mother.
We were surprised that there were no differences across scales when assessing our two primary factors of interest separately and only a small significant difference when comparing the interaction of our two factors in the supportive scale. These findings are a departure from recent research that have found differences when using stigmatizing language to describe adults with substance use disorder.11,31,36 We propose several possible hypotheses to explain this finding. First, the use of person-centered, medically accurate language to describe infants may not have been sufficient to overcome the cognitive dissonance respondents expressed with both punitive-blaming and supportive views towards mothers and recovery. Next, there may have been idiosyncrasies in the sample who completed the survey. The participants in our cohort may not be truly representative of the general public, with more than 70% obtaining some college-level education or greater. While there are many advantages to using MTurk to quickly gather data from a large number of participants, users have consistently been found to be more educated than the general public, which may have led to greater knowledge and education around substance use disorder impacting the responses.37,38 Future research looking at health care and substance use treatment providers who work closely with women with OUD would be valuable. Furthermore, one in seven individuals endorsed a personal history of having a drug or alcohol problem and almost half had a family member or close friend with a history of a drug or alcohol problem. These personal experiences may have contributed to a greater understanding of the chronic relapsing nature of addiction, decreasing, while still harboring, negative views towards individuals who use drugs.39,40 While the majority of questions either came from previously published studies or validated scales, the questions we used were not from formally validated survey instruments. The questions that we selected may have been too similar to detect subtle differences in individual perceptions based on which vignette they received.
Limitations
There are important limitations to this study that may have impacted our findings. As highlighted above, we adapted our vignette and survey questions from previously published studies, but the specific language we compared and the question scales were not validated independently prior to this study. Next, our study is subject to social desirability bias, where participants may have felt that there was a “right” response to certain questions. This bias may have overridden the subtler effects attributable to our factors of interest. Additionally, given high agreement with both punitive-blaming and supportive statements that at times appear contradictory, the quality of participant responses may be subject to acquiescence bias. We intentionally included comprehension checks and eliminated survey responses under 100 seconds to reduce this effect, but this may have been inadequate to completely eliminate the threat of such biases. Finally, given the large number of statistical tests we performed, the cumulative error rate is high, suggesting that our significant results may in fact be due to chance. Further research would benefit from rigorously controlling the number of tests to reduce this error rate.
Conclusion:
In a randomized vignette study assessing the role of language describing opioid-exposed newborns and type of opioid use in pregnant women, we identified no clinically significant differences in respondents views, regardless of type of vignette received. Overall, participants wanted mothers to recover and do well, yet they also blamed them, felt they were personally responsible, and caused harm to their newborn. By endorsing both punitive-blaming and supportive views, respondents showcased cognitive dissonance which may contribute to ongoing stigma towards mothers with OUD. Future work is needed to better understand the internal conflict in responses received, and whether responses among health care providers working with families impacted by OUD carry different beliefs than the general public.
Supplementary Material
Table 3:
Estimated Marginal Mean Scores for Survey Scales from Two-Way ANOVA (N=1,227)
| Substance-related Stigma | Punitive-Blaming | Supportive | ||
|---|---|---|---|---|
|
| ||||
| Estimated Marginal Means (SE) | ||||
|
| ||||
| Overall | 3.8 (.02) | 4.3 (.02) | 4.8 (.02) | |
|
| ||||
| Language Factor | Opioid type Factor | |||
|
| ||||
| “Addicted Baby” | IV Heroin | 3.8 (.05) | 4.4 (.05) | 4.8 (.04) |
| Prescription Opioids | 3.8 (.05) | 4.3 (.05) | 4.8 (.04) | |
| “Substance Exposed” | IV Heroin | 3.9 (.05) | 4.3 (.05) | 4.9 (.04) |
| Prescription Opioids | 3.8 (.05) | 4.2 (.05) | 4.7 (.04) | |
n.b.
‘Scales are from 1 (=“strongly disagree”) to 6 (=“strongly agree”) on a Likert scale’; ANOVA= analysis of variance; SE= standard error; Language Factor - language used to describe the newborn (Addicted Baby or Substance Exposed Infant); Opioid type Factor - type of opioid use (IV Heroin or Prescription Opioid)
Acknowledgements:
The authors thank Dr. Sarah Wakeman for her input on vignette and survey tool development.
Funding Support: Dr. Schiff was supported by NIDA (K12 DA043490 and K23DA048169). Ms. Myers was supported by the Case Western Reserve School of Medicine Summer Research Program. Dr. Kelly was supported by NIAAA (K24AA022136).
Footnotes
Conflicts of Interest:
Dr. Timothy Wilens is or has been a consultant for Arbor, Otsuka, Ironshore, KemPharm and Vallon. Dr. Wilens has a licensing agreement with Ironshore (BSFQ Questionnaire). He serves as a clinical consultant to the US National Football League (ERM Associates), U.S. Minor/Major League Baseball; Gavin Foundation and Bay Cove Human Services. No other coauthors have any financial conflicts of interest to report.
Literature Cited
- 1.Botticelli MP & Koh HK Changing the Language of Addiction. JAMA 316, 1361 (2016). [DOI] [PubMed] [Google Scholar]
- 2.Kelly JF, Wakeman SE & Saitz R Stop talking ‘dirty’: clinicians, language, and quality of care for the leading cause of preventable death in the United States. Am. J. Med 128, 8–9 (2015). [DOI] [PubMed] [Google Scholar]
- 3.Kumar R & Chattu V What is in the name? Understanding terminologies of patient-centered, person-centered, and patient-directed care! J. Fam. Med. Prim. Care 7, 487 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. What Is Addiction? Psychiatric News 53, appi.pn.2018.5a24 (2018). [Google Scholar]
- 5.Substance Use Disorders | SAMHSA - Substance Abuse and Mental Health Services Administration. Available at: https://www.samhsa.gov/disorders/substance-use. (Accessed: 30th July 2018)
- 6.Rappleye H, McHugh R & Farrow R Born Addicted: The Number of Opioid-Addicted Babies Is Soaring. Available at: https://www.nbcnews.com/storyline/americas-heroin-epidemic/born-addicted-number-opioid-addicted-babies-soaring-n806346. (Accessed: 19th July 2018)
- 7.Klaric M Drug-addicted babies: Wailing, gnashing of teeth | News | sharonherald.com. Available at: http://www.sharonherald.com/news/drug-addicted-babies-wailing-gnashing-of-teeth/article_661dd279-7ae3-5f5f-833e-dab768971dd0.htm. (Accessed: 19th July 2018)
- 8.McGinty EE, Stone EM, Kennedy-Hendricks A & Barry CL Stigmatizing language in news media coverage of the opioid epidemic: Implications for public health. Prev. Med. (Baltim). 124, 110–114 (2019). [DOI] [PubMed] [Google Scholar]
- 9.McGinty EE, Goldman HH, Pescosolido B & Barry CL Portraying mental illness and drug addiction as treatable health conditions: Effects of a randomized experiment on stigma and discrimination. Soc. Sci. Med 126, 73–85 (2015). [DOI] [PubMed] [Google Scholar]
- 10.Kelly JF, Dow SJ & Westerhoff C Does Our Choice of Substance-Related Terms Influence Perceptions of Treatment Need? An Empirical Investigation with Two Commonly Used Terms. J. Drug Issues 40, 805–818 (2010). [Google Scholar]
- 11.Goodyear K, Haass-Koffler CL & Chavanne D Opioid use and stigma: The role of gender, language and precipitating events. Drug Alcohol Depend. 185, 339–346 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ashford RD, Brown AM & Curtis B The Language of Substance Use and Recovery: Novel Use of the Go/No–Go Association Task to Measure Implicit Bias. Health Commun. 1–7 (2018). doi: 10.1080/10410236.2018.1481709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kennedy-Hendricks A et al. Social Stigma Toward Persons With Prescription Opioid Use Disorder: Associations With Public Support for Punitive and Public Health–Oriented Policies. Psychiatr. Serv. 68, 462–469 (2017). [DOI] [PubMed] [Google Scholar]
- 14.McGinty EE et al. Criminal Activity or Treatable Health Condition? News Media Framing of Opioid Analgesic Abuse in the United States, 1998–2012. Psychiatr. Serv 67, 405–411 (2016). [DOI] [PubMed] [Google Scholar]
- 15.National Academies of Sciences Engineering and Medicine. Medications for Opioid Use Disorder Save Lives. (2019). doi: 10.17226/25310. [DOI] [PubMed]
- 16.Volkow ND Stigma and the toll of addiction. New England Journal of Medicine 382, 1289–1290 (2020). [DOI] [PubMed] [Google Scholar]
- 17.Stone R Pregnant women and substance use: fear, stigma, and barriers to care. Heal. Justice 3, 2 (2015). [Google Scholar]
- 18.Cleveland LM & Bonugli R Experiences of mothers of infants with neonatal abstinence syndrome in the neonatal intensive care unit. J Obs. Gynecol Neonatal Nurs 43, 318–329 (2014). [DOI] [PubMed] [Google Scholar]
- 19.Roberts SCM & Pies C Complex calculations: how drug use during pregnancy becomes a barrier to prenatal care. Matern. Child Health J. 15, 333–41 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jessup MA, Humphreys JC, Brindis CD & Lee KA Extrinsic Barriers to Substance Abuse Treatment among Pregnant Drug Dependent Women. J. Drug Issues 33, 285–304 (2003). [Google Scholar]
- 21.National Advocates for Pregnant Women: Pregnancy and Drug Use: The Facts. Available at: http://www.advocatesforpregnantwomen.org/issues/pregnancy_and_drug_use_the_facts/. (Accessed: 31st July 2018)
- 22.Hauser DJ & Schwarz N Attentive Turkers: MTurk participants perform better on online attention checks than do subject pool participants. Behav. Res. Methods 48, 400–407 (2016). [DOI] [PubMed] [Google Scholar]
- 23.Bartneck C, Duenser A, Moltchanova E & Zawieska K Comparing the Similarity of Responses Received from Studies in Amazon’s Mechanical Turk to Studies Conducted Online and with Direct Recruitment. PLoS One 10, e0121595 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Randomizer - Qualtrics Support. Available at: https://www.qualtrics.com/support/survey-platform/survey-module/survey-flow/standard-elements/randomizer/. (Accessed: 8th August 2020)
- 25.Luoma JB, O’Hair AK, Kohlenberg BS, Hayes SC & Fletcher L The Development and Psychometric Properties of a New Measure of Perceived Stigma Toward Substance Users. Subst. Use Misuse 45, 47–57 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kelly JF & Westerhoff CM Does it matter how we refer to individuals with substance-related conditions? A randomized study of two commonly used terms. Int. J. Drug Policy 21, 202–207 (2010). [DOI] [PubMed] [Google Scholar]
- 27.National Centre for Education and Training on Addiction. A Training Resource Health Professionals’ Attitudes Towards Licit and Illicit Drug Users.
- 28.Chappel JN, Veach TL, •-And ED & Krug RS The Substance Abuse Attitude Survey: An Instrument for Measuring Attitudes*. Journal of Studies on Alcohol 46, (1985). [DOI] [PubMed] [Google Scholar]
- 29.Schiff DM, Zuckerman B, Wachman EM & Bair-Merritt M Trainees’ knowledge, attitudes, and practices towards caring for the substance-exposed mother-infant dyad. Subst. Abus 38, 414–421 (2017). [DOI] [PubMed] [Google Scholar]
- 30.Cortina JM What Is Coefficient Alpha? An Examination of Theory and Applications. J. Appl. Psychol 78, 98–104 (1993). [Google Scholar]
- 31.Kelly JF, Dow SJ & Westerhoff C Does Our Choice of Substance-Related Terms Influence Perceptions of Treatment Need? An Empirical Investigation with Two Commonly Used Terms. J. Drug Issues 40, 805–818 (2010). [Google Scholar]
- 32.SAS 9.4 Software Overview for the Customer Available at: https://support.sas.com/software/94/index.html. (Accessed: 7th December 2020)
- 33.Kennedy-Hendricks A et al. Social stigma toward persons with prescription opioid use disorder: Associations with public support for punitive and public health-oriented policies. Psychiatr. Serv 68, 462–469 (2017). [DOI] [PubMed] [Google Scholar]
- 34.Barry CL, McGinty EE, Pescosolido BA & Goldman HH Stigma, discrimination, treatment effectiveness, and policy: Public views about drug addiction and mental illness. Psychiatr. Serv 65, 1269–1272 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tuliao AP & Holyoak D Psychometric properties of the perceived stigma towards substance users scale: factor structure, internal consistency, and associations with help-seeking variables. Am. J. Drug Alcohol Abuse (2019). doi: 10.1080/00952990.2019.1658198 [DOI] [PubMed] [Google Scholar]
- 36.Sumnall HR, Hamilton I, Atkinson AM, Montgomery C & Gage SH Representation of adverse childhood experiences is associated with lower public stigma towards people who use drugs: an exploratory experimental study. Drugs Educ. Prev. Policy (2020). doi: 10.1080/09687637.2020.1820450 [DOI] [Google Scholar]
- 37.Goodman JK, Cryder CE & Cheema A Data Collection in a Flat World: The Strengths and Weaknesses of Mechanical Turk Samples. J. Behav. Decis. Mak 26, 213–224 (2013). [Google Scholar]
- 38.Follmer DJ, Sperling RA & Suen HK The Role of MTurk in Education Research: Advantages, Issues, and Future Directions. Educational Researcher 46, 329–334 (2017). [Google Scholar]
- 39.Keyes KM et al. Original Contribution Stigma and Treatment for Alcohol Disorders in the United States. 172, (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Adlaf EM, Hamilton HA, Wu F & Noh S Adolescent stigma towards drug addiction: Effects of age and drug use behaviour. (2008). doi: 10.1016/j.addbeh.2008.11.012 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.