ABSTRACT
Gallbladder perforation and stone spillage is a common intraoperative problem during laparoscopic cholecystectomy. Most of these stones are retrieved intraoperatively. The incidence of lost or unretrieved stones is approximately 2%, and very few patients may develop complication. Most common complication of dropped or spilled gallstones is abscess, particularly around the abdominal wall port sites and in the perihepatic space. We report a case of dropped stone-related right subhepatic and parietal wall abscess 39 months after laparoscopic cholecystectomy. The patient was treated successfully by operative drainage of the abscess along with complete removal of stones. The patient was asymptomatic at 6-month follow-up.
INTRODUCTION
Gallbladder perforation with stone spillage is one of the most common intraoperative problems during laparoscopic cholecystectomy (LC). This complication ranges from 6%–40% in LC.1,2 Most of these stones are retrieved intraoperatively, but fragmented and inaccessible stones are left in the peritoneal cavity in a small subset of patients. Very few patients with unretrieved stones may develop a complication. A meta-analysis of 8 studies on lost gallstones during LC showed that the incidence of lost or unretrieved stones is about 2% and these stones caused complications 8.5% of the time.3 The most common complication of dropped gallstones is abscess—either in the perihepatic space or of the abdominal wall.3–5 We report a case of dropped stone-related right subhepatic and parietal wall abscess after LC.
CASE REPORT
A 48-year-old man with a history of LC 39 months back presented with right upper abdominal pain, low-grade fever, and swelling in the right hypochondrium around the right axillary port site for 12 days. He was evaluated by a local physician with transabdominal ultrasound (US) of upper abdomen and was diagnosed as a case of parietal wall abscess. US-guided aspiration of 55 mL of purulent material was performed. He was treated with oral antibiotics based on culture-sensitivity report with partial resolution of symptoms. Four weeks later, he came to our institution with similar symptoms. The medical records and operative notes were reviewed, and there was no description of gallbladder perforation or spillage of stones. Abdominal examination showed a tender swelling in the right hypochondrium close to previous axillary port site. Preliminary laboratory investigations were within normal limits except elevated white blood count of 13.4 × 1,000 cells/μL.
Transabdominal US (Figure 1) showed a collection in the right subhepatic space with few calculi. Abdominal contrast-enhanced computed tomography scan (CECT) (Figure 2) revealed a collection in the right subhepatic space extending into the anterior abdominal wall. The right hepatic flexure of the colon was densely adhered to the abscess cavity. After preoperative bowel preparation, operative drainage of right subhepatic and parietal wall abscess was performed through a right subcostal incision. On entry into the abscess cavity, 200 mL of purulent material was evacuated. Multiple stones were found in the depth of the abscess cavity. After removal of all stones and necrosis, the abscess cavity was irrigated with copious amount of warm normal saline. Then a closed-suction drain was placed within the abscess cavity. Fascial layer was closed with No-1 polypropyline suture. Skin and subcutaneous tissues were left open for delayed primary closure. The drain was removed on the fifth postoperative day. Skin and subcutaneous tissue were closed on the sixth postoperative day. The patient had an uneventful recovery and was well at 6-month follow-up.
Figure 1.
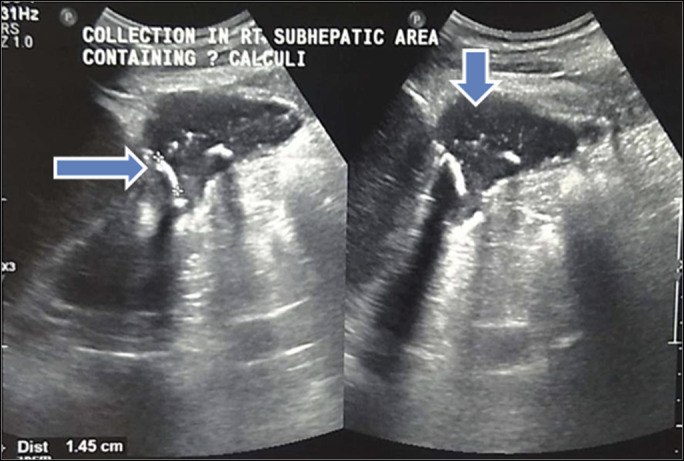
Transabdominal ultrasound showing subhepatic collection (vertical arrow) with stones (transverse arrow) imparting distal acoustic shadow.
Figure 2.
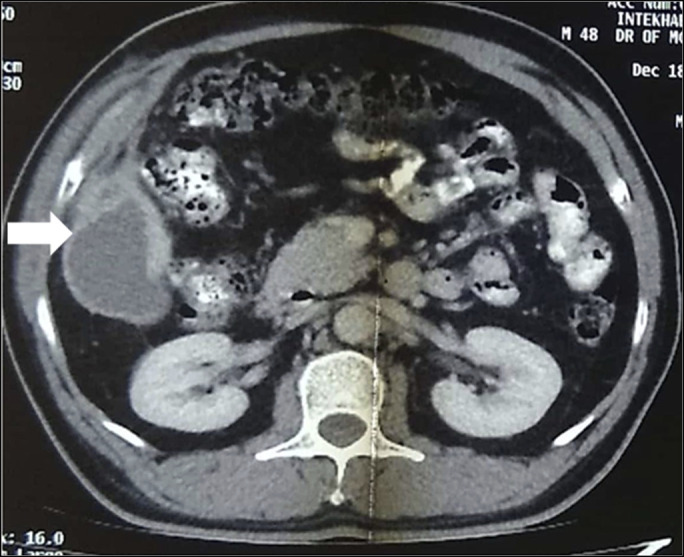
Abdominal computed tomography showing right subhepatic collection (white arrow) extending into the parietal wall.
DISCUSSION
Abscess formation caused by spilled gallstones may manifest weeks to months or even years after LC.4,5 The diagnosis of dropped gallstones causing abscesses can be extremely challenging for 3 reasons: (i) Presentation is often remote from the time of the procedure4,5; (ii) in most cases, the occurrence of stone spillage or lost stones was not mentioned in the operative notes3,4,6; and (iii) standard imaging may not detect dropped stones.5
US and CECT are valuable diagnostic tools in this scenario. CECT will reveal the site of septic lesion and even the presence of a radio opaque gallstone. However, in most cases, the CECT may be unable to delineate the presence of stone in the abscess cavity.7 Possible explanations include radiolucency due to water attenuation of cholesterol stones, low-calcium density tiny gallstone fragments, and obscuration of calcium attenuation by adjacent inflammatory enhancement on CECT.5 Transabdominal US may be more sensitive for low calcium-density stone or radiolucent dropped stone embedded in enhancing inflammatory tissue8 by detecting the hyperechoic acoustic signals from these stones and may depict calculi invisible in CECT. US is more cost-effective and should be regarded as the first-line imaging in this scenario. In our patient also, US showed few calculi in the depth of the abscess cavity not visualized in CECT abdomen.
Prevention of stone spillage is the best way to avoid this complication. The primary means of preventing dropped gallstones is the surgical removal of an intact gallbladder. Careful dissection, aspiration of bile from the tense gallbladder, and use of an endobag for gallbladder removal can avoid stone spillage and reduce the incidence of septic complication after LC. If gallstones have spilled into the peritoneal cavity, every attempt should be made to retrieve them with suctioning, forceps, and irrigation. Because complications from spilled stones are the exception rather than the rule, conversion to open procedure in the event of unretrieved stones is not recommended. A good policy is to document the event and to inform the patient for medicolegal reasons, to alert them to the possibility of future complications, and to avoid misinterpretation of subsequent imaging findings.5,6
There are several options for the management of dropped gallstone-related abscess such as percutaneous technique, laparoscopy, and laparotomy.5,9,10 Laparoscopy is less invasive, and the procedure can be performed through the retroperitoneal approach.10 In many cases, laparoscopic and percutaneous technique may not be feasible because of the inaccessible location of the abscess and surrounding dense adhesions. An open approach therefore is preferable. Regardless of the approach, the main stay of treatment is drainage of purulent material and complete removal of all stones. Antibiotic therapy and drainage of abscess without stone removal may result in recurrent abscess.3,5 Similarly in our patient, abscess recurred after percutaneous aspiration of purulent material and antibiotic therapy. Complete recovery was achieved only after operative drainage of purulent material with complete stone removal.
In conclusion, abscess formation due to dropped gallstones is a rare event that can manifest itself many months to years after the initial operation. As it is a preventable complication, meticulous preventive measures should be adopted to prevent a spilled gallstone. It is vital to document and communicate the presence of dropped gallstones to the patients to alert them for future complications. High index of suspicion is essential for prompt diagnosis, and the main stay of treatment is drainage of purulent material and complete removal of all stones.
DISCLOSURES
Author contributions: S. Ray wrote and edited the manuscript, approved the final manuscript, and is the article guarantor. D. Kumar wrote the manuscript, reviewed the literature, revised the manuscript for intellectual content, and approved the final manuscript. D. Garai and S. Khamrui reviewed the literature, revised the manuscript for intellectual content, and approved the final manuscript.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
Contributor Information
Dilip Kumar, Email: dcompanyoo5@gmail.com.
Dibyendu Garai, Email: dibyendugarai.dg@gmail.com.
Sujan Khamrui, Email: skpapam@rediffmail.com.
REFERENCES
- 1.Brockmann JG, Kocher T, Senninger NJ, Schürmann GM. Complications due to gallstones lost during laparoscopic cholecystectomy. Surg Endosc. 2002;16(8):1226–32. [DOI] [PubMed] [Google Scholar]
- 2.Schäfer M, Suter C, Klaiber C, Wehrli H, Frei E, Krähenbühl L. Spilled gallstones after laparoscopic cholecystectomy. A relevant problem? A retrospective analysis of 10,174 laparoscopic cholecystectomies. Surg Endosc. 1998;12(4):305–9. [DOI] [PubMed] [Google Scholar]
- 3.Zehetner J, Shamiyeh A, Wayand W. Lost gallstones in laparoscopic cholecystectomy: All possible complications. Am J Surg. 2007;193(1):73–8. [DOI] [PubMed] [Google Scholar]
- 4.Dobradin A, Jugmohan S, Dabul L. Gallstone-related abdominal abscess 8 years after laparoscopic cholecystectomy. JSLS. 2013;17(1):139–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ramamurthy NK, Rudralingam V, Martin DF, Galloway SW, Sukumar SA. Out of sight but kept in mind: Complications and imitations of dropped gallstones. AJR Am J Roentgenol. 2013;200(6):1244–53. [DOI] [PubMed] [Google Scholar]
- 6.Mullerat J, Cooper K, Box B, Soin B. The case for standardisation of the management of gallstones spilled and not retrieved at laparoscopic cholecystectomy. Ann R Coll Surg Engl. 2008;90(4):310–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Manukyan MN, Demirkalem P, Gulluoglu BM, et al. Retained abdominal gallstones during laparoscopic cholecystectomy. Am J Surg. 2005;189(4):450–2. [DOI] [PubMed] [Google Scholar]
- 8.Viera FT, Armellini E, Rosa L, et al. Abdominal spilled stones: Ultrasound findings. Abdom Imaging. 2006;31(5):564–7. [DOI] [PubMed] [Google Scholar]
- 9.Thomson B, Kawa B, Rabone A, et al. Ultrasound-guided percutaneous retrieval of a dropped gallstone following laparoscopic cholecystectomy. BJR Case Rep. 2018;4(3):20180002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Villar del Moral JM, Villegas-Herrera MT, Medina-Benítez A, Ramia-Angel JM, Garrote-Lara D, Ferrón-Orihuela JA. Retroperitoneoscopy to extract dropped gallstones after laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A. 2006;16(3):290–3. [DOI] [PubMed] [Google Scholar]


