Abstract
We showed previously that susceptibility testing for Mycobacterium tuberculosis labeled with fluorescein diacetate could be accomplished rapidly by using flow cytometry. However, safety was a major concern because mycobacteria were not killed prior to flow cytometric analysis. In this study, we developed a biologically safe flow cytometric susceptibility test that depends on detection and enumeration of actively growing M. tuberculosis organisms in drug-free and antimycobacterial agent-containing medium. The susceptibilities of 17 clinical isolates of M. tuberculosis to ethambutol, isoniazid, and rifampin were tested by the agar proportion and flow cytometric methods. Subsequently, all flow cytometric susceptibility test samples were inactivated by exposure to paraformaldehyde before analysis with a flow cytometer. Agreement between the results from the two methods was 98%. In addition, the flow cytometric results were available 72 h after the initiation of testing. The flow cytometric susceptibility assay is safe, simple to perform, and more rapid than conventional test methods, such as the BACTEC system and the proportion method.
In the last decade, the resurgence of tuberculosis and increases in the resistance of Mycobacterium tuberculosis to antimycobacterial agents (1, 3–5, 11) has emphasized the importance of implementing and maintaining effective public health approaches to prevent transmission of the disease. Rapid and accurate susceptibility testing of M. tuberculosis was recommended by the Centers for Disease Control and Prevention (CDC) as essential for controlling tuberculosis (3). Unfortunately, susceptibility testing of M. tuberculosis has been seriously limited by the time required to obtain results primarily because of the slow growth of the organism (2, 7, 9). Even the most frequently used method, BACTEC-460, requires 4 to 12 days of incubation before results are available (6, 9, 13).
We showed previously that susceptibility testing of clinical isolates of M. tuberculosis labeled with fluorescein diacetate (FDA) could be accomplished more rapidly by using a flow cytometer (7, 10). Results of tests were available 24 h after M. tuberculosis cells were incubated with antimycobacterial agents. Furthermore, the multiplication of mycobacteria in the drug-free controls was not required. Although the FDA-dependent flow cytometric susceptibility method is accurate, reproducible, and rapid (7, 10), it is possible that aerosolization of droplet nuclei containing viable M. tuberculosis could occur at several points in the procedure, including during sample aspiration, ejection of the sample from the nozzle inside the flow chamber, and decontamination. Therefore, the procedure is suitable only for public health laboratories or large reference laboratories with a biosafety level 3 tuberculosis facility and experience with biosafety level 3 precautions.
In this study, we developed a flow cytometric susceptibility test that addressed the biosafety concern. M. tuberculosis isolates were determined to be susceptible or resistant to antimycobacterial agents via a bacterial enumeration method. In addition, viable mycobacteria were inactivated by treatment with paraformaldehyde prior to flow cytometric analysis. Results from this method were available 72 h after the initiation of testing.
MATERIALS AND METHODS
Antimycobacterial agents.
Ethambutol (EMB), isoniazid (INH), and rifampin (RIF) were obtained from Sigma Chemical Co., St. Louis, Mo. Stock solutions of EMB and INH were prepared at 10,000 μg/ml in distilled water and sterilized by filtration with a 0.2-μm-pore-size filter (Nalgene Labware Division, Rochester, N.Y.). Aliquots of 1 ml of the sterilized antituberculosis agents were then frozen at −70°C until used. RIF was also prepared at 10,000 μg/ml, but dissolved in dimethyl sulfoxide (Sigma).
Mycobacteria and preparation.
Seventeen clinical isolates of M. tuberculosis that varied in their resistance to antimycobacterial agents were obtained from the CDC. Initially, each isolate was grown in 7H9 broth (Difco, Detroit, Mich.) at 37°C for several days until the turbidity of the suspensions was equivalent to a McFarland 1.0 standard. Each suspension was then dispensed in 1.0-ml aliquots and stored at −70°C until used. Subsequently, aliquots of 50 μl of each isolate were taken from thawed stocks and used to inoculate 10 ml of 7H9 broth in sterile 50-ml polypropylene screw-cap tubes (Sarstedt, Newton, N.C.). Cultures were incubated for approximately 5 to 17 days at 37°C in the presence of 5% CO2. When the turbidity of the cultures was equivalent to a McFarland 1.0 standard, they were used for susceptibility testing.
Paraformaldehyde treatment.
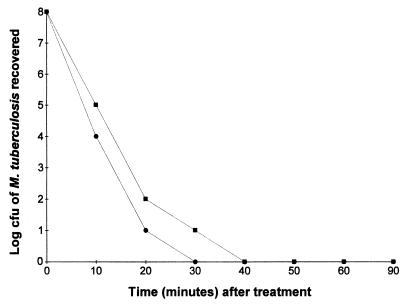
Aliquots (2 ml) of each of three isolates of M. tuberculosis containing 108 organisms/ml were placed in 5-ml round-bottom polystyrene tubes (Becton Dickinson Labware, Lincoln Park, N.J.) containing 134 or 300 μl of an 8% solution of paraformaldehyde to yield final concentrations of 0.5 and 1% paraformaldehyde, respectively. After incubation for 0, 10, 20, 30, 40, 50, 60, and 90 min, 25 μl of the paraformaldehyde-treated M. tuberculosis suspensions were filtered through sterile 0.2-μm-pore-size filters (Millipore Corp., Bedford, Mass.) and washed three times with 100 μl of sterile phosphate-buffered saline (pH 7.4). Each filter was placed on a fresh Middlebrook 7H10 agar plate, sealed in a plastic bag, and incubated at 37°C in the presence of 5% CO2 for 3 weeks. The number of colony forming units (CFU) was then determined.
Agar proportion susceptibility testing.
The agar proportion method, as recommended by the National Committee for Clinical Laboratory Standards (9), was performed to determine the percentage of M. tuberculosis organisms resistant to each of the concentrations of antimycobacterial agents tested. Briefly, 7H10 agar medium (Difco) was prepared, autoclaved at 121°C at 15 lb/in2 for 15 min, and cooled to 50 to 56°C. INH, RIF, and EMB were added to the medium to yield final concentrations of 0.2, 1.0, and 5.0 μg of INH/ml, 1.0 μg of RIF/ml, and 5.0 μg of EMB/ml. Subsequently, 5.0 ml of each concentration of antimycobacterial-containing medium was dispensed into labeled quadrants of sterile petri dishes. One quadrant per plate was reserved for 7H10 medium free of any antimycobacterial agent to serve as a growth control. Upon solidification of the medium, the plates were inoculated with 0.1 ml of 10−2 and 10−4 dilutions of a suspension of each M. tuberculosis isolate equivalent to a McFarland 1.0 standard. The inoculated plates were then incubated at 37°C in the presence of 5% CO2 for 3 weeks. An isolate was considered susceptible to an antimycobacterial agent if the number of colonies growing in the presence of the antimycobacterial agent was <1% of the colonies growing on the drug-free control. An isolate was reported as resistant if the number of colonies growing on the drug-containing medium was greater than or equal to 1% of the colonies growing on the control.
Flow cytometric susceptibility testing.
Aliquots of 0.9 ml of each actively growing M. tuberculosis isolate were transferred to 2.0-ml polypropylene screw-cap microtubes (Sarstedt). The tubes were inoculated with 0.1 ml of 500, 400, 200, 100, 50, 10, and 2.0 μg of INH/ml; 100, 50, and 20 μg of EMB/ml; and 500, 400, 200, 100, 50, and 10 μg of RIF/ml. Drug-free controls of M. tuberculosis were also prepared by inoculating them with 0.1 ml sterile phosphate-buffered saline (pH 7.4). Subsequently, the suspensions were incubated for 24, 48, or 72 h at 37°C in an environment of 5% CO2. After incubation, 0.2 ml of each assay suspension was removed and placed in a sterile 2.0-ml screw-cap microtube containing 30 μl of 8% paraformaldehyde (pH 7.4). Samples were then mixed and held at room temperature for 40 min before being analyzed with a Bryte HS flow cytometer with WinBryte software (Bio-Rad Laboratories, Hercules, Calif.).
After paraformaldehyde treatment, M. tuberculosis cells were detected and differentiated from non-M. tuberculosis particles in 7H9 medium by using forward and side angle light scatter signals. Electronic noise and background particles in the 7H9 medium were excluded from analysis by adjusting the threshold monitor listed on the WinBryte software program. Forward- and side-angle light scattering was then used to analyze M. tuberculosis cells that were incubated with or without antimycobacterial agents. For each sample acquired, the flow cytometer provided a histogram profile relating to the number of M. tuberculosis organisms in each of 2,048 logarithmic channels of increasing light scattering, a measurement of the number of M. tuberculosis events/microliter and a contour plot of forward- versus side-angle light scattering. Five thousand events were acquired for each sample. In addition, 2.5-μm polystyrene beads (Molecular Probes, Eugene, Oreg.) were used daily for the calibration of the instrument and as an internal control to monitor sampling error.
Assessment of susceptibility by using flow cytometry.
An isolate was considered susceptible by the flow cytometric method if the number of M. tuberculosis organisms (events) in the drug-containing medium was reduced 25, 45, and 50% or more after exposure to EMB, INH, and RIF, respectively, compared to the number of tubercle bacilli in the drug-free control. The number of M. tuberculosis organisms/milliliter was obtained as part of the flow cytometric statistical analysis and was dependent upon the establishment of gates to eliminate electronic noise and background particles from the medium.
Statistical analysis.
A t test was used to determine significant differences between the number of mycobacteria in the drug-free and drug-containing medium. The alpha level was set at 0.05 before the experiments were started.
RESULTS
Effects of paraformaldehyde on the viability of M. tuberculosis.
To show that cultures of M. tuberculosis organisms could be sterilized before analysis by flow cytometry, individual suspensions of three isolates of M. tuberculosis containing 108 cells/ml were incubated for 0, 10, 20, 30, 40, 50, 60, or 90 min in the presence of 0.5 or 1.0% paraformaldehyde. No viable M. tuberculosis organisms were recovered from the suspensions 30 or 40 min after treatment with 1.0 or 0.5% paraformaldehyde, respectively (Fig. 1). Subsequently, 14 isolates of M. tuberculosis were exposed to paraformaldehyde for 40 min. Similarly, no viable mycobacteria were recovered from the paraformaldehyde-treated susceptibility assays. When these studies were partially replicated with other mycobacterial isolates, including one isolate of M. tuberculosis H37Ra, four isolates of Mycobacterium avium, and two isolates each of Mycobacterium gordonae, Mycobacterium kansasii, Mycobacterium fortuitum, and Mycobacterium phlei, no viable mycobacteria were recovered from the suspensions treated for 40 min with 1.0% paraformaldehyde, even after several weeks of incubation. Based on these findings, we treated all assay suspensions with 1.0% paraformaldehyde for 40 min before proceeding with flow cytometric analysis.
FIG. 1.
Effects of duration of treatment with 0.5% (■) and 1.0% (●) paraformaldehyde on the viability of an isolate of M. tuberculosis. The experimental standard error was ±0.5. Similar results were obtained with other isolates of M. tuberculosis.
Effects of antimycobacterial agents on M. tuberculosis and detection by flow cytometry.
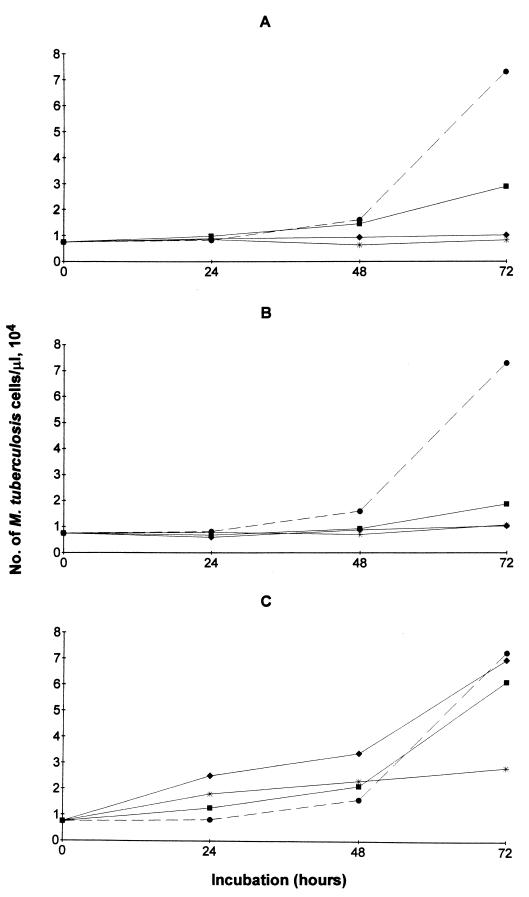
Viable M. tuberculosis cells were incubated in the presence or absence of 0.06, 0.25, and 1.0 μg of INH/ml (Fig. 2A) or RIF (Fig. 2B) and 0.25, 1.0, and 5.0 μg of EMB/ml (Fig. 2C) and incubated for 24, 48, or 72 h. M. tuberculosis organisms incubated for 24 or 48 h in the presence of antituberculosis agents did not show a significant decrease in events compared to untreated controls when analyzed by flow cytometry. However, significant differences (P < 0.01) were detected at 72 h. The number of M. tuberculosis cells/microliter increased from 104 to 8 × 104 in the drug-free controls, while 2.5 × 104 or less mycobacteria/microliter were detected in the drug-treated suspensions containing EMB, INH, or RIF. When these experiments were repeated with other isolates of M. tuberculosis, similar results were obtained. Subsequent studies used 72 h to determine the susceptibility or resistance of isolates of M. tuberculosis to antimycobacterial agents.
FIG. 2.
Number of M. tuberculosis cells (events)/microliter detected by flow cytometry with or without (●) exposure to 0.06 (■), 0.25 (⧫), or 1.0 (∗) μg of INH/ml (A) or RIF (B) or 0.25 (■), 1.0 (⧫), or 5.0 (∗) μg of EMB/ml (C) for 24, 48, or 72 h. The experimental standard error was ±0.21.
Susceptibility of clinical isolates of M. tuberculosis to antimycobacterial agents.
Seventeen clinical isolates obtained from the CDC were tested for susceptibility or resistance to EMB, INH, or RIF by the flow cytometric and proportion methods (Table 1). Overall, there was agreement between the two methods for 83 of the 85 total tests (98%). Two of the isolates, 352 and 368 were resistant to 0.2 μg of INH/ml by the proportion method but susceptible to this concentration of INH by flow cytometry. When higher concentrations (1.0 and 5.0 μg/ml) were tested, the same susceptibility results were obtained by the proportion and flow cytometric methods. When isolates were tested for susceptibility or resistance to EMB or RIF, no discrepancies between the methods were detected.
TABLE 1.
Results of susceptibility tests by the flow cytometric or proportion method for isolates of M. tuberculosis exposed to INH, RIF, or EMBa
| Isolate | Result obtained by:
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Flow cytometric method
|
Proportion method
|
|||||||||
| INH (μg/ml)
|
RIF (μg/ml)
|
EMB (μg/ml)
|
INH (μg/ml)
|
RIF (μg/ml)
|
EMB (μg/ml)
|
|||||
| 0.2 | 1 | 5 | 1 | 5 | 0.2 | 1 | 5 | 1 | 5 | |
| 017 | R | S | S | S | S | R | S | S | S | S |
| 132 | S | S | S | R | S | S | S | S | R | S |
| 135 | S | S | S | R | S | S | S | S | R | S |
| 212 | S | S | S | R | S | S | S | S | R | S |
| 223 | R | R | S | S | S | R | R | S | S | S |
| 226 | R | R | R | S | S | R | R | R | S | S |
| 289 | R | S | S | S | S | R | S | S | S | S |
| 292 | S | S | S | R | S | S | S | S | R | S |
| 323 | R | R | S | S | S | R | R | S | S | S |
| 348 | R | S | S | S | S | R | S | S | S | S |
| 352 | S | S | S | S | S | R | S | S | S | S |
| 368 | S | S | S | S | S | R | S | S | S | S |
| 621 | R | S | S | S | S | R | S | S | S | S |
| 642 | R | R | R | S | R | R | R | R | S | R |
| 897 | R | S | S | S | R | R | S | S | S | R |
| 982 | S | S | S | R | S | S | S | S | R | S |
| 992 | S | S | S | R | S | S | S | S | R | S |
Isolates of M. tuberculosis were exposed to 0.2, 1.0, or 5.0 μg of INH/ml, 1.0 μg of RIF/ml, and 5.0 μg of EMB/ml using the proportion and flow cytometric methods. The isolates marked S for the proportion method showed less than 1% of the growth seen on drug-free control plates after 3 weeks of incubation. The isolates marked S for flow cytometry contained 25, 45, and 50% less mycobacteria in suspensions containing EMB, INH, or RIF, respectively, than the drug-free control 72 h after incubation. Isolates marked R for both methods were considered resistant.
DISCUSSION
Our results show that accurate susceptibility testing of M. tuberculosis can be accomplished by the enumeration of mycobacterial cells with a flow cytometer. Results of tests were available 72 h after M. tuberculosis organisms were incubated with EMB, INH, and RIF. Most importantly, the method is safe. Mycobacteria were killed by exposure to paraformaldehyde before susceptibility samples were analyzed with the flow cytometer.
The flow cytometric susceptibility test depends on multiplication of M. tuberculosis organisms. Although M. tuberculosis grows slowly, with cell division occurring every 15 to 24 h, small but significant increases in the numbers of mycobacteria can be accurately detected and quantified by flow cytometric analysis. Within 72 h after the initiation of testing procedures, the number of mycobacteria in the drug-free and drug-containing assays could be compared. A decrease in the number of M. tuberculosis cells of 45, 50, or 25% in suspensions containing INH, RIF, or EMB, respectively, was required to accurately predict the same results as those obtained by the agar proportion method. The proportion method is the “gold standard” for susceptibility testing of M. tuberculosis (9).
We tested 17 isolates of M. tuberculosis for susceptibility or resistance to EMB, INH, and RIF by the flow cytometric and proportion methods. Agreement between the results from the two methods was 97, 100, and 100% for INH, EMB, and RIF, respectively. Overall, agreement was 98%. Two discrepancies were detected among the 85 tests performed. These isolates were susceptible to 0.2 μg of INH/ml by the flow cytometric test but resistant to this concentration of INH by the proportion method. When higher concentrations (1.0 and 5.0 μg/ml) of INH were tested, identical susceptibility results were obtained by both the flow cytometric and proportion methods. A likely explanation for these discrepancies is the cutoff value. We arbitrarily set the cutoff value for defining susceptibility to INH at 45%. This required the detection of 45% less M. tuberculosis cells in the drug-containing assay compared to the number of M. tuberculosis cells detected in the drug-free controls. The value could have been 30, 35, or 40% or any numerical value within these numbers. Determination of the best-fit cutoff value will require evaluation of multiple isolates of M. tuberculosis by several laboratories. Another possible explanation is the bactericidal activity of INH. The flow cytometric results were obtained during an interval (72 h) of high bactericidal activity for INH. It has been reported that INH bactericidal activity decreases rapidly in medium after 7 days of incubation due to formation of isonicotinic acid and other metabolites (14, 15). Therefore, mycobacteria that survived inactivation at a low concentration (0.2 μg/ml) of INH would be considered resistant to INH by the proportion method after the recommended incubation period of 3 weeks. When higher concentrations of INH (1.0 and 5.0 μg/ml) were tested by the flow cytometric and proportion methods, the same susceptibility results were obtained.
A major concern with use of the flow cytometer for susceptibility testing of M. tuberculosis is biosafety. A single tubercle bacillus is infectious for humans. Because the flow cytometer operates under a pressurized system, generation of a small number of infectious particles (5 μm) is possible. Previously, we showed that susceptibility testing of M. tuberculosis could be accomplished by flow cytometry in 24 h. The rapidity of the method was dependent upon addition of FDA to differentiate viable from nonviable mycobacteria after treatment with antimycobacterial agents (7). Unfortunately, attempts to inactivate or kill the mycobacteria and still maintain the differential effects of FDA failed. Therefore, viable mycobacteria with or without exposure to antimycobacterial agents were processed with the flow cytometer. Although this FDA-dependent assay is accurate, rapid (24 h), and reproducible, most clinical laboratories do not have the facilities or expertise to carry out the procedure safely.
In this study, we developed a flow cytometric procedure that greatly reduced the risk of infection to the health care worker using the flow cytometer. All assay suspensions were treated with 1.0% paraformaldehyde before processing with the instrument. Viable tubercle bacilli were not recovered from the drug-containing or drug-free suspensions 40 min after treatment with paraformaldehyde. Increasing the duration of exposure of suspensions of M. tuberculosis organisms to paraformaldehyde also did not alter the results of the susceptibility tests. Accurate susceptibility results could still be obtained if paraformaldehyde treated samples were analyzed 24 to 72 h after exposure to paraformaldehyde. This step further augments the biosafety of the procedure. However, tubercle bacilli trapped in the lips or caps of the susceptibility tubes could have escaped treatment with paraformaldehyde. Therefore, processing samples outside a biosafety level 3 tuberculosis facility is not recommended unless exquisite care is taken to assure that samples are treated properly.
The flow cytometric susceptibility assay also has another advantage besides increased biosafety. The assay does not depend on use of FDA (7) for obtaining results. Instead, the numbers of mycobacteria in the assay suspensions with or without exposure to antimycobacterial agents are determined 72 h after initiation of testing. Although the requirement for enumeration of mycobacteria delays the reporting of results by 48 h compared to the FDA-dependent flow cytometric susceptibility assay, this biologically safer procedure is still more rapid than the BACTEC-460 system (6, 8, 9, 12, 13).
Other advantages of the flow cytometric assay are its simplicity and low cost. The materials required to perform the test include 7H9 broth, microtubes, and the antimycobacterial agents. In addition, samples can be rapidly processed by the flow cytometer (under 60 s). If results are indeterminate, the flow cytometric susceptibility tests can be reanalyzed after incubation for 24 h. Technician time for performing the flow cytometric susceptibility test is similar to that required by the radiometric proportion method. Furthermore, the cost of the flow cytometric test is considerably less than the cost incurred by the radiometric proportion method. The actual test components cost less than 3 dollars. Although the cost of the flow cytometer is high, when the high cost of supplies for performing susceptibility testing by the radiometric instrument is considered, the cost of a flow cytometer is justifiable, especially if a refurbished instrument is obtained.
In conclusion, the flow cytometric method is safe for performing susceptibility testing on clinical isolates of M. tuberculosis. The assay is extremely simple to perform and can be completed in 72 h after the initiation of testing.
ACKNOWLEDGMENTS
We thank Bio-Rad Laboratories in cooperation with the Gundersen Lutheran Medical Foundation, Inc., LaCrosse, Wis., for support.
We greatly appreciate the support of Adolf L. Gundersen and Mark Connelly along with Herbert M. Heili. We also thank Louise Kubista, David Fett, Michelle Myrdal, and Daniel Muller for excellent advice and assistance.
REFERENCES
- 1.Bloch A B, Cauthen G M, Onorato I M, Dansbury K G, Kelly G D, Driver C R, Snider D E., Jr Nationwide survey of drug-resistant tuberculosis in the United States. JAMA. 1994;271:665–671. [PubMed] [Google Scholar]
- 2.Canetti G, Frosman S, Grosset J H, Hauduroy P, Langerova M, Mahler H T, Meissner G, Mitchison D A, Sula L. Mycobacteria: laboratory methods for testing drug sensitivity and resistance. Bull W H O. 1963;29:565–578. [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Tuberculosis morbidity—United States, 1995. Morbid Mortal Weekly Rep. 1996;45:365–370. [PubMed] [Google Scholar]
- 4.Cohn D L, Bustreo F, Raviglione M C. Drug-resistant tuberculosis: review of the worldwide situation and the WHO/IUATLD global surveillance project. Clin Infect Dis. 1997;24(Suppl. 1):S121–S130. doi: 10.1093/clinids/24.supplement_1.s121. [DOI] [PubMed] [Google Scholar]
- 5.Daniel T M, Debanne S M. Estimation of the annual risk of tuberculosis infection for white men in the United States. J Infect Dis. 1997;175:1535–1537. doi: 10.1086/516495. [DOI] [PubMed] [Google Scholar]
- 6.Heifets L B, Iseman M D, Cook J L, Lindholm-Levy P J, Drupa I. Determination of in vitro susceptibility of Mycobacterium tuberculosis to cephalosporins by radiometric and conventional methods. Antimicrob Agents Chemother. 1985;27:11–15. doi: 10.1128/aac.27.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kirk S M, Schell R F, Moore A V, Callister S M, Mazurek G H. Flow cytometric testing of susceptibilities of Mycobacterium tuberculosis isolates to ethambutol, isoniazid, and rifampin in 24 hours. J Clin Microbiol. 1998;36:1568–1573. doi: 10.1128/jcm.36.6.1568-1573.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee C, Heifets L B. Determination of minimal concentrations of antituberculosis drugs by radiometric and conventional methods. Am Rev Respir Dis. 1987;136:349–352. doi: 10.1164/ajrccm/136.2.349. [DOI] [PubMed] [Google Scholar]
- 9.National Committee for Clinical Laboratory Standards. Antimycobacterial susceptibility testing for Mycobacterium tuberculosis. Proposed standard M24-T. Villanova, Pa: National Committee for Clinical Laboratory Standards; 1995. [Google Scholar]
- 10.Norden M A, Kurzynski T A, Bounds S E, Callister S M, Schell R F. Rapid susceptibility testing of Mycobacterium tuberculosis (H37Ra) by flow cytometry. J Clin Microbiol. 1995;33:1231–1237. doi: 10.1128/jcm.33.5.1231-1237.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Raviglione M C, Snider D E, Jr, Kochi A. Global epidemiology of tuberculosis: morbidity and mortality of a worldwide epidemic. JAMA. 1995;273:220–226. [PubMed] [Google Scholar]
- 12.Roberts G D, Goodman N L, Heifets L, Larsh H W, Lindner T H, McClatchy J K, McGinnis M R, Siddiqi S H, Wright P. Evaluation of the BACTEC radiometric method for recovery of mycobacteria and drug susceptibility testing of Mycobacterium tuberculosis from acid-fast smear-positive specimens. J Clin Microbiol. 1983;18:689–696. doi: 10.1128/jcm.18.3.689-696.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Siddiqi S H, Hawkins J E, Laszio A. Interlaboratory drug susceptibility testing of Mycobacterium tuberculosis by a radiometric procedure and two conventional methods. J Clin Microbiol. 1985;22:919–923. doi: 10.1128/jcm.22.6.919-923.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wimpenny J W T. Effect of isoniazid on biosynthesis in Mycobacterium tuberculosis var. bovis BCG. J Gen Microbiol. 1967;47:379. doi: 10.1099/00221287-47-3-379. [DOI] [PubMed] [Google Scholar]
- 15.Youatt J. A review of the action of isoniazid. Am Rev Respir Dis. 1969;99:729–749. doi: 10.1164/arrd.1969.99.5.729. [DOI] [PubMed] [Google Scholar]