Abstract
This cohort study assesses whether adding premature menopause status to pooled cohort equations improves risk prediction of atherosclerotic cardiovascular disease among women.
Contemporary practice guidelines recommend using pooled cohort equations (PCEs)1 to predict 10-year risk of atherosclerotic cardiovascular disease (ASCVD). In 2019, the American College of Cardiology (ACC) and the American Heart Association (AHA)2 issued an updated primary prevention guideline for cardiovascular disease. To personalize patient-clinician discussions of ASCVD risk, the ACC/AHA guideline recognized premature menopause as a risk-enhancing factor among women younger than 40 years.2 Conventional ASCVD risk calculations currently do not include premature menopause. Thus, the extent to which premature menopause may quantitatively change risk prediction of ASCVD, beyond traditional risk factors such as diabetes, hyperlipidemia, hypertension, and obesity, is unknown. This cohort study assessed whether adding premature menopause status to PCEs improves risk prediction of ASCVD among women.
Methods
We pooled individual-level participant data from Black and White postmenopausal women aged 40 to 79 years from 7 US population-based cohorts. These cohorts included the Atherosclerosis Risk in Communities Study, the Cardiovascular Health Study, the Coronary Artery Risk Development in Young Adults Study, the Framingham Heart Study, the Framingham Offspring Study, the Multi-ethnic Study of Atherosclerosis, and the Women’s Health Initiative. We excluded women with a history of ASCVD. We defined premature menopause as age younger than 40 years based on the 2019 ACC/AHA guideline.2 ASCVD was defined as fatal or nonfatal coronary heart disease or stroke. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline. Informed consent was waived because the data were deidentified, and this study was deemed not human subjects research by the Northwestern University Feinberg School of Medicine Institutional Review Board. We used Cox proportional hazards regression models to define the association between premature menopause and ASCVD, adjusting for traditional risk factors such as diabetes, hyperlipidemia, hypertension, and obesity. We used the C statistic, Greenwood-Nam-D’Agostino χ2 statistic, and categorical net reclassification improvement (NRI) based on a lipid-lowering therapy clinical threshold (7.5%) to assess PCE model performance in 10-year risk predictions of incident ASCVD among women with or without premature menopause. We performed 3 sensitivity analyses for the following: (1) women with natural menopause only (given heterogeneity in ascertainment of surgical menopause), (2) women with surgical menopause only, and (3) women aged 40 to 54 years. All analyses were stratified by self-reported race.
Results
Of the 5466 Black women and 10 584 White women in this study, Black women were older and had a higher prevalence of hypertension, obesity, and diabetes (Table). Premature menopause was more common among Black women (17.4%) compared with White women (9.8%). In addition, premature menopause was significantly associated with ASCVD independent of traditional risk factors, with hazard ratios of 1.24 (95% CI, 1.03-1.49) and 1.28 (95% CI, 1.13-1.45) for Black and White women, respectively. The PCEs demonstrated good discrimination and calibration for both groups (Figure). However, there was no incremental benefit in ASCVD risk predictions when premature menopause was added to the PCEs, with categorical NRI values of 0.0007 (P = .91) and 0.003 (P = .37) for Black and White women, respectively. In sensitivity analyses, similar findings in model performance were observed for women with only natural menopause, for women with only surgical menopause, and for women aged 40 to 54 years.
Table. Baseline Characteristics for the Cohort of Black and White Women With or Without Premature Menopausea.
| Characteristic | Black women | White women | ||
|---|---|---|---|---|
| Premature menopause (n = 951) | Menopause (n = 4515) | Premature menopause (n = 1039) | Menopause (n = 9545) | |
| Premature menopause | 17.4 | 9.8 | ||
| Age, y | 59.7 (8.4) | 60.5 (8.0) | 57.4 (10.5) | 58.0 (10.1) |
| Blood pressure, mm Hg | ||||
| SBP | 132.3 (20.9) | 130.9 (19.6) | 125.1 (21.3) | 125.4 (21.2) |
| DBP | 77.7 (10.4) | 76.9 (10.2) | 72.4 (11.8) | 72.8 (11.4) |
| BMI | 31.0 (6.6) | 30.4 (6.4) | 26.5 (5.4) | 26.2 (5.0) |
| Cholesterol, mg/dL | ||||
| Total | 218.7 (45.7) | 216.7 (42.6) | 224.8 (43.8) | 220.1 (43.0) |
| HDL | 59.2 (16.0) | 58.3 (15.7) | 56.6 (16.3) | 57.9 (16.5) |
| Glucose, mg/dL | 108.1 (44.9) | 105.1 (40.7) | 98.9 (30.5) | 97.6 (26.0) |
| Current smoking | 17.0 | 14.2 | 33.0 | 22.6 |
| Hypertension treatment | 53.0 | 48.9 | 25.5 | 23.6 |
| Cholesterol treatment | 12.9 | 13.8 | 5.4 | 5.0 |
| Diabetes history | 17.8 | 15.9 | 8.1 | 5.9 |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); DBP, diastolic blood pressure; HDL, high-density lipoprotein; SBP, systolic blood pressure.
SI conversion factors: To convert total and HDL cholesterol to mmol/L, multiply by 0.0259; glucose to mmol/L, by 0.0555.
Data are presented as percentages or means (SD) unless otherwise stated. Individual-level pooled data are from participants from 7 US population-based cohorts, including the Atherosclerosis Risk in Communities Study, the Cardiovascular Health Study, the Coronary Artery Risk Development in Young Adults Study, the Framingham Heart Study, the Framingham Offspring Study, the Multi-ethnic Study of Atherosclerosis, and the Women’s Health Initiative. Participants comprised 5466 Black women (34%) and 10 584 White women (66%). Women with premature menopause were younger than 40 years, whereas those with menopause were 40 years or older.
Figure. Model Performance of the Original Pooled Cohort Equation for Black Women and White Women With or Without Premature Menopause.
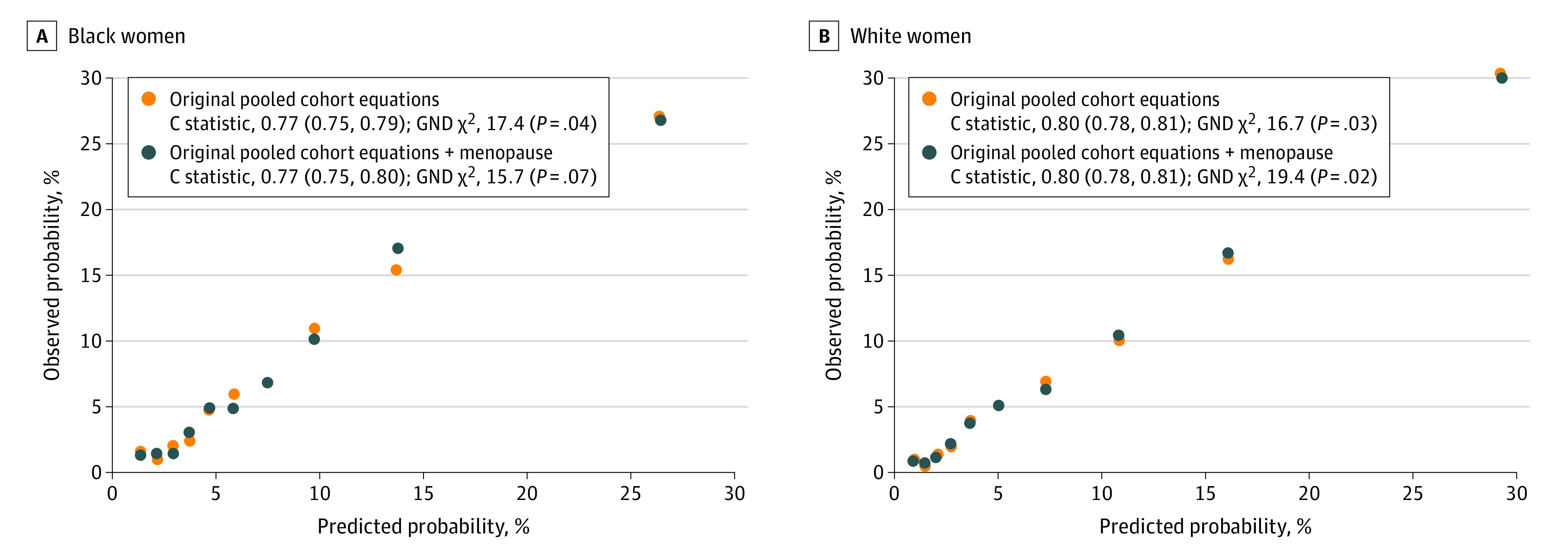
Individual-level pooled data are for Black women (A) and White women (B) from 7 US population-based cohorts, including the Atherosclerosis Risk in Communities Study, the Cardiovascular Health Study, the Coronary Artery Risk Development in Young Adults Study, the Framingham Heart Study, the Framingham Offspring Study, the Multi-ethnic Study of Atherosclerosis, and the Women’s Health Initiative. P < .05 represents suboptimal calibration. GND indicates Greenwood-Nam-D’Agostino.
Discussion
Our results are consistent with previous studies documenting substantial positive associations between premature menopause and ASCVD.3 Our findings also extend prior work with data supporting premature menopause as a risk-enhancing factor for ASCVD. However, adding premature menopause to the PCEs in this study did not notably improve ASCVD risk prediction. In this analysis and in others examining risk-enhancing factors, it is important to highlight the distinction between a notable association and a meaningful change in risk prediction.4 Although the menopausal transition is well established as one of the dynamic hormonal changes that may contribute to accelerated ASCVD risk, this risk appears to be mediated largely by the interim development of traditional risk factors (eg, diabetes and hypertension) in the causal pathway of ASCVD and is included in the PCEs.5 Conversely, premature menopause may be a marker of underlying risk rather than a contributor to ASCVD development, because studies have reported a positive association between premenopausal cardiovascular health (eg, body mass index, systolic blood pressure, physical activity) and early age at menopause.5 Regardless, clinicians should aim to screen and identify women with a high risk for ASCVD and then offer early detection and treatment of these risk factors soon after the menopausal transition. Self-report of menopausal status is a limitation of this study, and future studies with adjudication are needed.
In conclusion, premature menopause is associated with an increased risk of ASCVD, but adding premature menopause to the PCEs did not meaningfully alter risk predictions of ASCVD for middle-aged women. Traditional risk factors such as hypertension and hyperlipidemia were already present by midlife and provided strong predictive utility within the PCEs, limiting the additive role of premature menopause by midlife.
References
- 1.Stone NJ, Robinson JG, Lichtenstein AH, et al. ; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25)(suppl 2):S1-S45. doi: 10.1161/01.cir.0000437738.63853.7a [DOI] [PubMed] [Google Scholar]
- 2.Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):e596-e646. doi: 10.1161/CIR.0000000000000678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Honigberg MC, Zekavat SM, Aragam K, et al. Association of premature natural and surgical menopause with incident cardiovascular disease. JAMA. 2019;322(24):2411-2421. doi: 10.1001/jama.2019.19191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pepe MS, Janes H, Longton G, Leisenring W, Newcomb P. Limitations of the odds ratio in gauging the performance of a diagnostic, prognostic, or screening marker. Am J Epidemiol. 2004;159(9):882-890. doi: 10.1093/aje/kwh101 [DOI] [PubMed] [Google Scholar]
- 5.El Khoudary SR, Aggarwal B, Beckie TM, et al. ; American Heart Association Prevention Science Committee of the Council on Epidemiology and Prevention; and Council on Cardiovascular and Stroke Nursing . Menopause transition and cardiovascular disease risk: implications for timing of early prevention: a scientific statement from the American Heart Association. Circulation. 2020;142(25):e506-e532. doi: 10.1161/CIR.0000000000000912 [DOI] [PubMed] [Google Scholar]


