Abstract
Background:
The burden of musculoskeletal trauma is increasing worldwide, especially in low-income countries such as Malawi. Ankle fractures are common in Malawi and may receive suboptimal treatment due to inadequate surgical capacity and limited provider knowledge of evidence-based treatment guidelines.
Methods:
This study was conducted in 3 phases. First, we assessed Malawian orthopaedic providers’ understanding of anatomy, injury identification, and treatment methods. Second, we observed Malawian providers’ treatment strategies for adults with ankle fractures presenting to a central hospital. These patients’ radiographs underwent blinded, post hoc review by 3 U.S.-based orthopaedic surgeons and a Malawian orthopaedic surgeon, whose treatment recommendations were compared with actual treatments rendered by Malawian providers. Third, an educational course addressing knowledge deficits was implemented. We assessed post-course knowledge and introduced a standardized management protocol, specific to the Malawian context.
Results:
In Phase 1, deficits in injury identification, ideal treatment practices, and treatment standardization were identified. In Phase 2, 17 (35%) of 49 patients met operative criteria but did not undergo a surgical procedure, mainly because of resource limitations and provider failure to recognize unstable injuries. In Phase 3, 51 (84%) of 61 participants improved their overall performance between the pre-course and post-course assessments. Participants answered a mean of 32.4 (66%) of 49 questions correctly pre-course and 37.7 (77%) of 49 questions correctly post-course, a significant improvement of 5.2 more questions (95% confidence interval [CI], 3.8 to 6.6 questions; p < 0.001) answered correctly. Providers were able to identify 1 more injury correctly of 8 injuries (mean, 1.1 questions [95% CI, 0.6 to 1.6 questions]; p < 0.001) and to identify 1 more ideal treatment of the 7 that were tested (mean, 1.0 question [95% CI, 0.5 to 1.4 questions]; p < 0.001).
Conclusions:
Adult ankle fractures in Malawi were predominantly treated nonoperatively despite often meeting evidence-based criteria for surgery. This was due to resource limitations, knowledge deficits, and lack of treatment standardization. We demonstrated a comprehensive approach to examining the challenges of providing adequate orthopaedic care in a resource-limited setting and the successful implementation of an educational intervention to improve care delivery. This approach can be adapted for other conditions to improve orthopaedic care in low-resource settings.
Trauma is a leading cause of morbidity and mortality worldwide, disproportionately affecting low-income and middle-income countries1–4. Trauma-related disability is especially devastating to poor individuals, as health care-related costs and decreased productivity can worsen impoverishment5,6. Disability can be mitigated with quality surgical care, which remains inaccessible for most of the world’s poorest people7–9.
Malawi is a low-income country in southeastern Africa of 19 million people, 83% living in rural areas, half living below the national poverty line, and 10% living with an untreated surgical condition of the upper or lower extremities10–12. Ankle fractures were found to be the most common adult injury seen in orthopaedic outpatient departments of 4 Malawian public hospitals13.
In high-income countries such as the United States, a surgical procedure is recommended for many displaced and/or unstable ankle fractures14–16. However, access to surgical procedures remains inadequate in Malawi. Orthopaedic care is provided in 24 district hospitals and 4 urban central hospitals. Over 90% of orthopaedic trauma care is delivered by orthopaedic clinical officers (OCOs), who are non-physician clinicians trained in nonoperative care17,18. Patients with ankle fractures are usually evaluated by OCOs, who triage patients to nonoperative treatment or refer patients to an orthopaedic surgeon for a surgical procedure. At the time of this writing, 10 orthopaedic surgeons were practicing in Malawi, roughly 1 per 1.9 million Malawians. All are board-certified, fellowship-trained, and stationed at central hospitals, where orthopaedic surgical procedures are available. However, surgeons must consider resource availability and each patient’s unique circumstances when recommending a surgical procedure. Implants are entirely donated, with frequent shortages; patients often present late and face challenges to follow-up13,19,20. In this context, we examined how ankle fractures are managed in Malawi and the barriers to evidence-based care.
Materials and Methods
Overview
Our study had 3 phases. In Phase 1, we assessed orthopaedic providers’ knowledge of ankle anatomy, injury classification, and ideal treatment methods. We surveyed providers on actual treatment practices and their rationale. In Phase 2, we observed Malawian providers’ treatment strategies for adult ankle fractures over 5 weeks at Kamuzu Central Hospital (KCH), the only public referral hospital in central Malawi. In Phase 3, we implemented an educational course addressing knowledge deficits and introducing a standardized protocol for ankle fracture management in Malawi. All phases were approved by the College of Medicine Research Ethics Committee (COMREC-P.03/19/2628,P.03/19/2629) in Malawi and by the institutional review board at Brigham and Women’s Hospital in the United States. Statistical analyses were performed with SAS version 9.4 (SAS Institute).
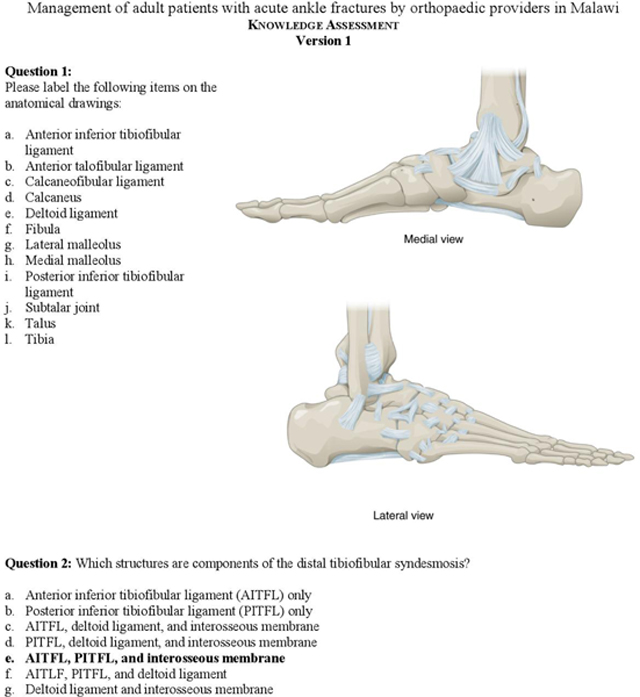
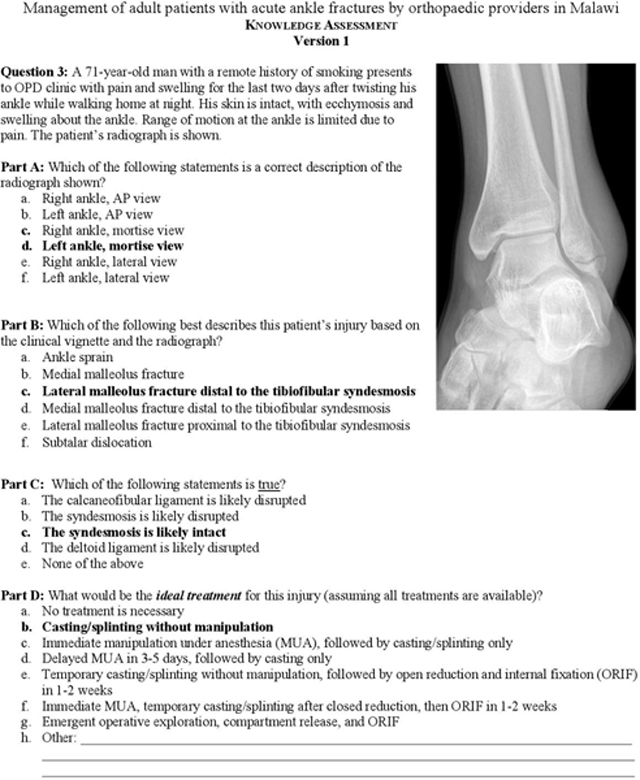
Phase 1: Knowledge Assessment
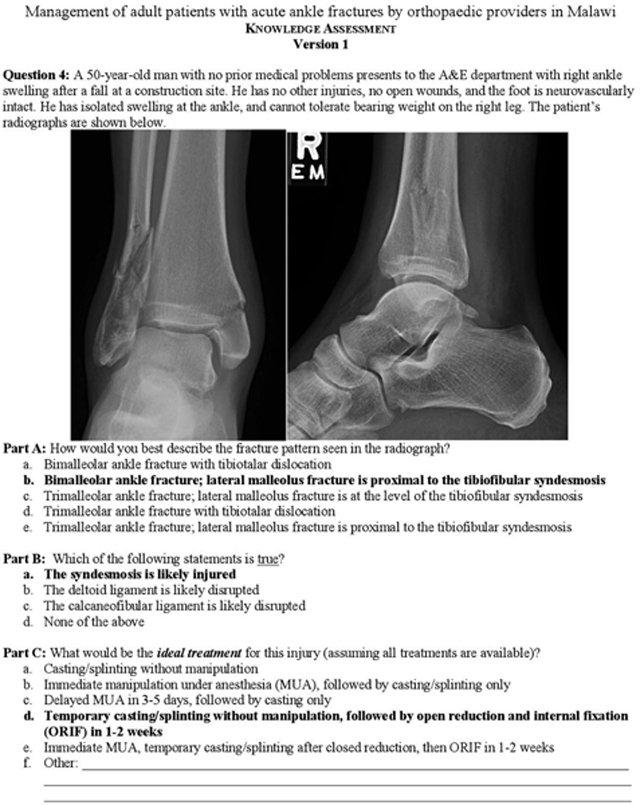
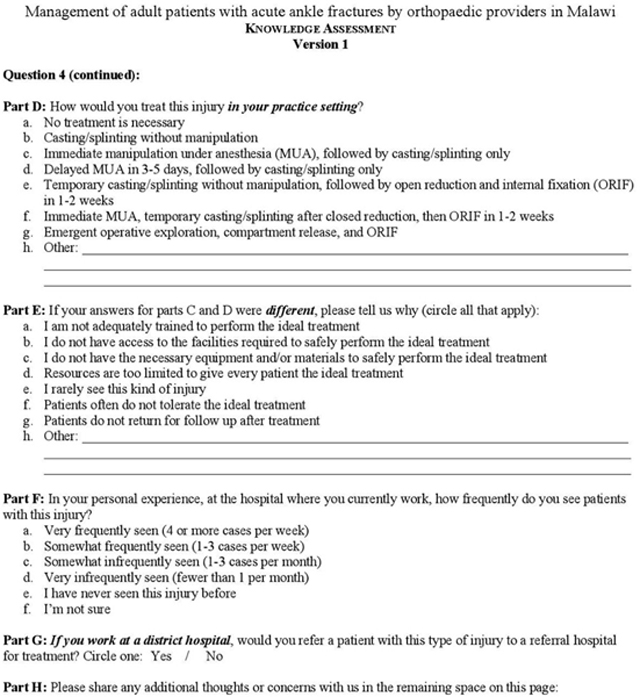
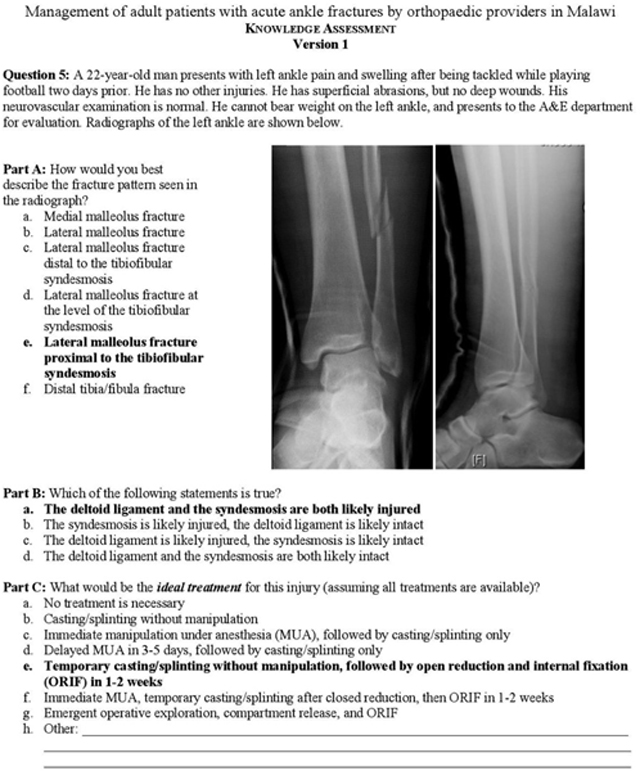
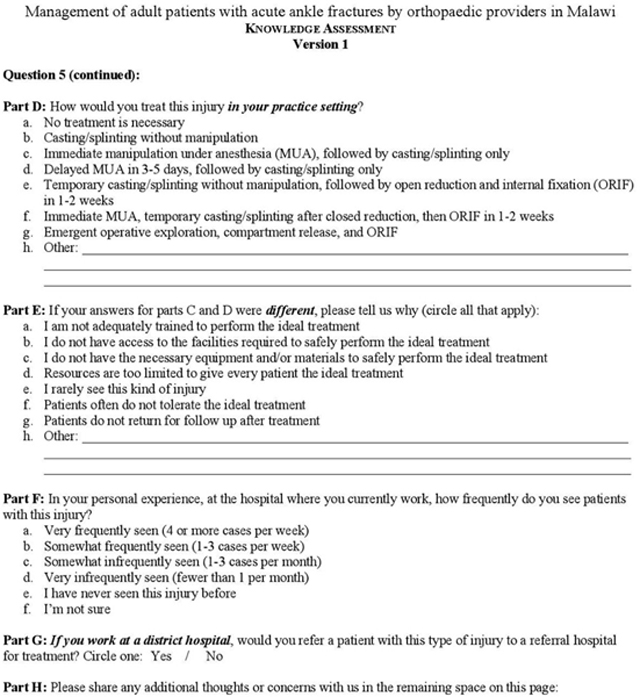
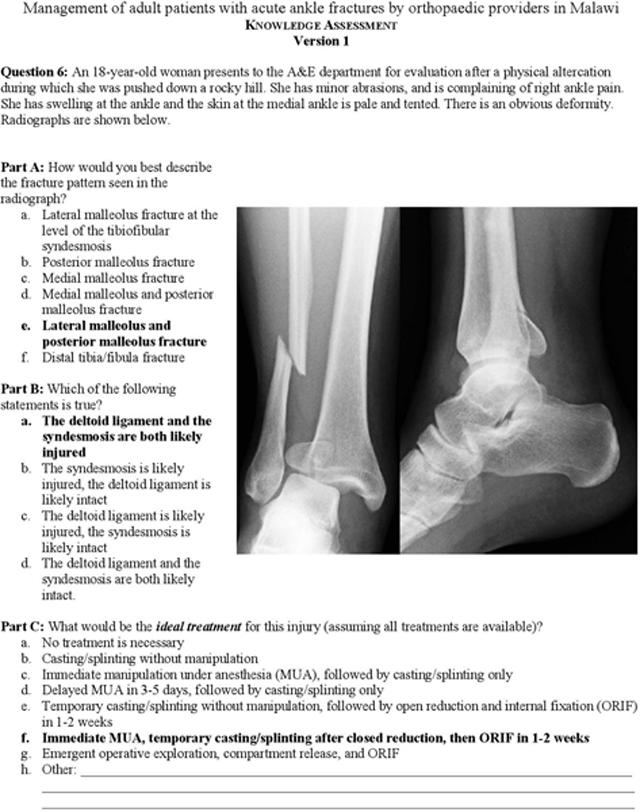
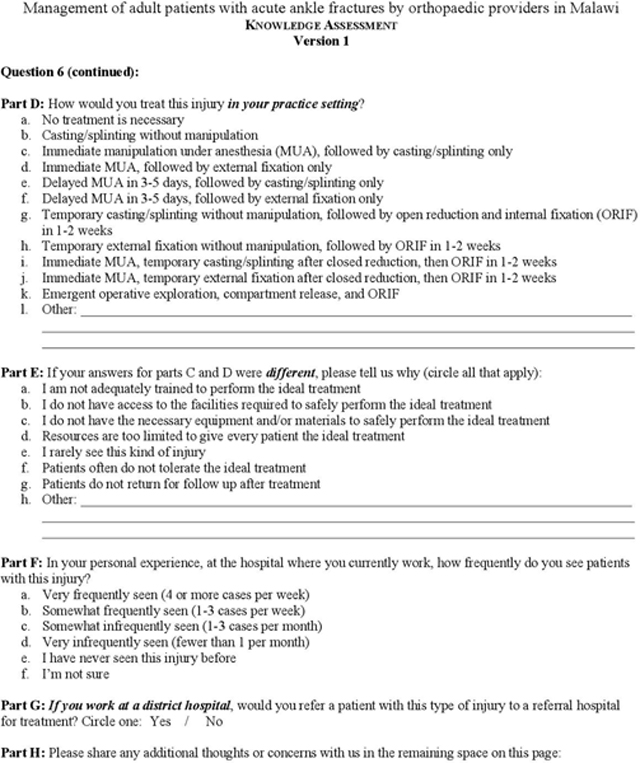
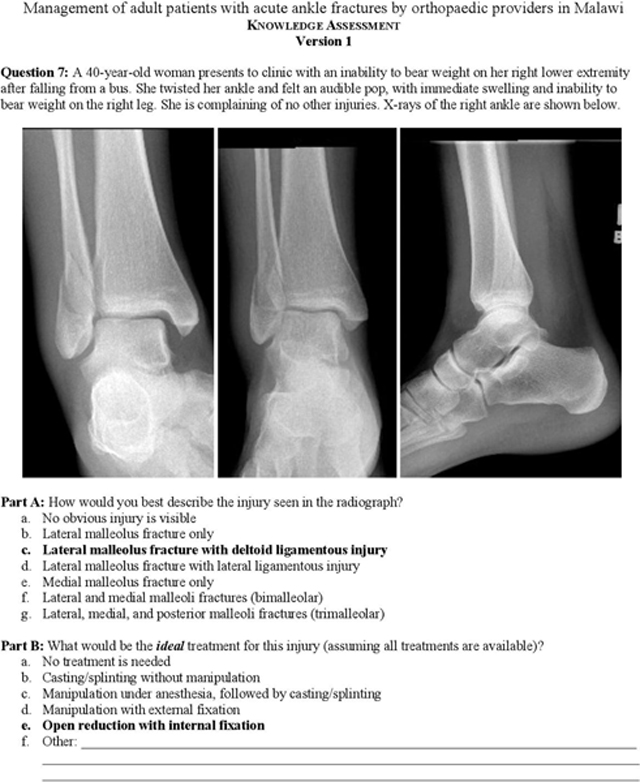
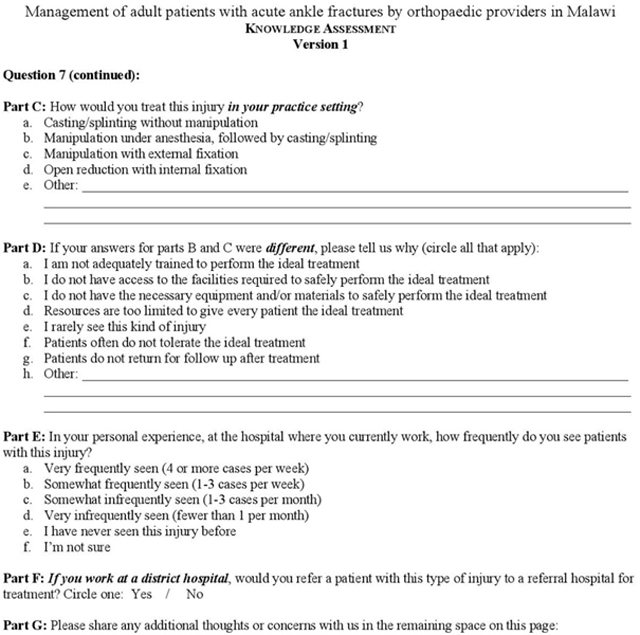
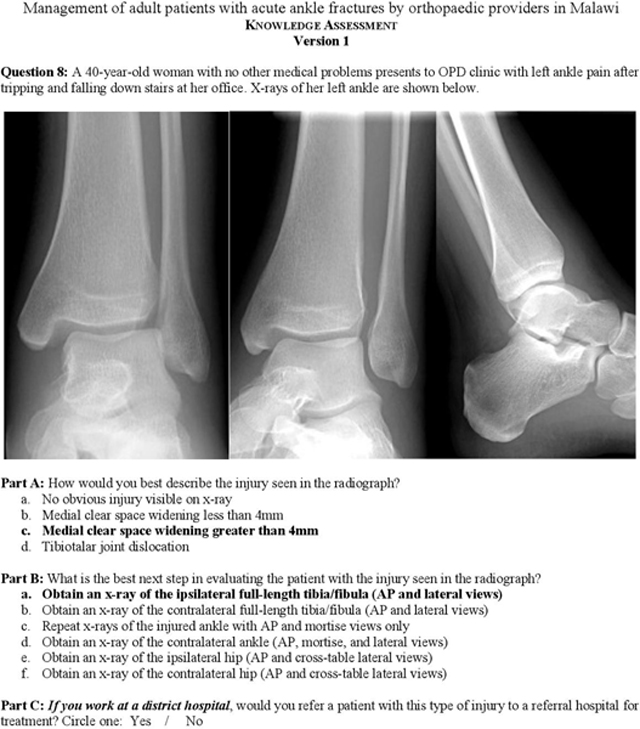
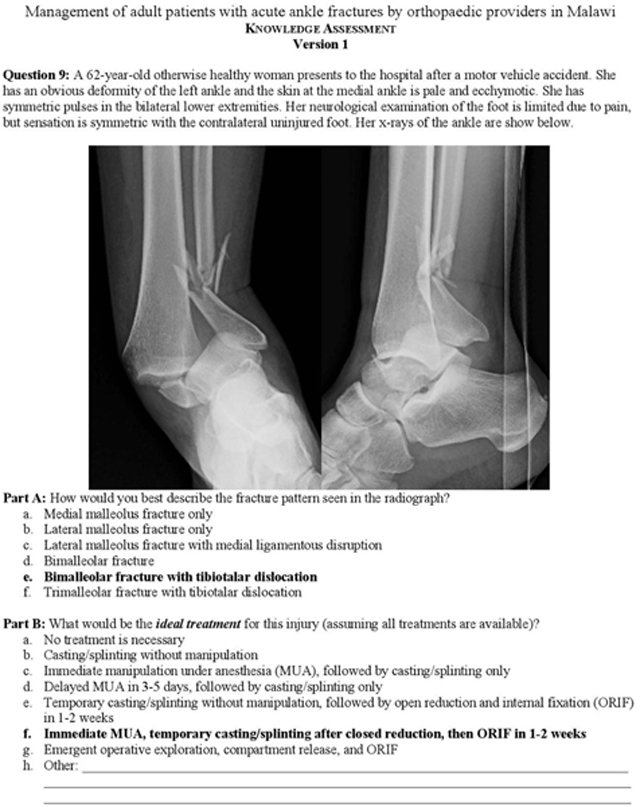
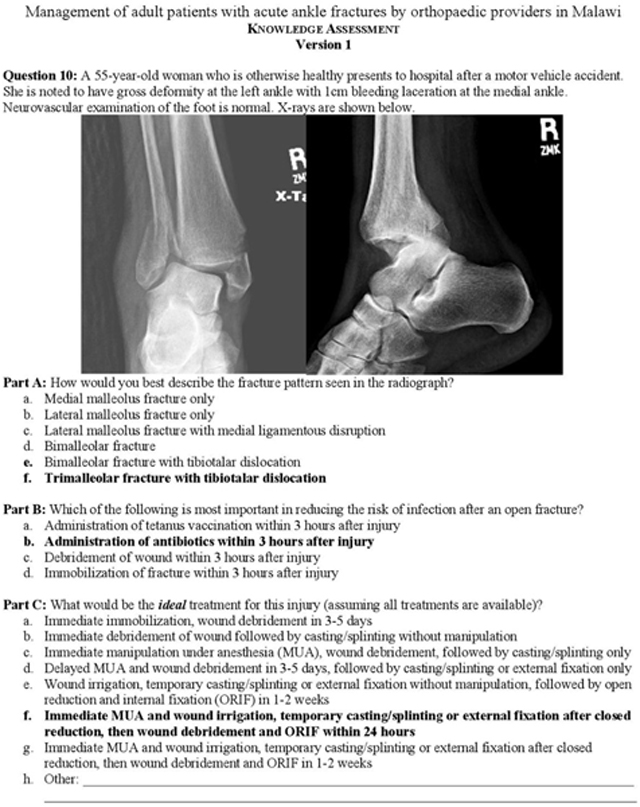
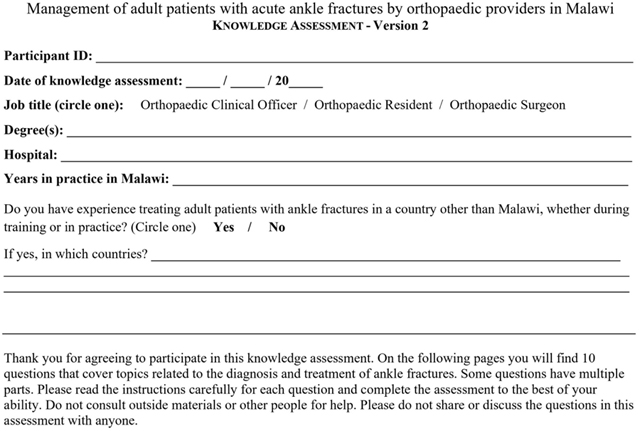
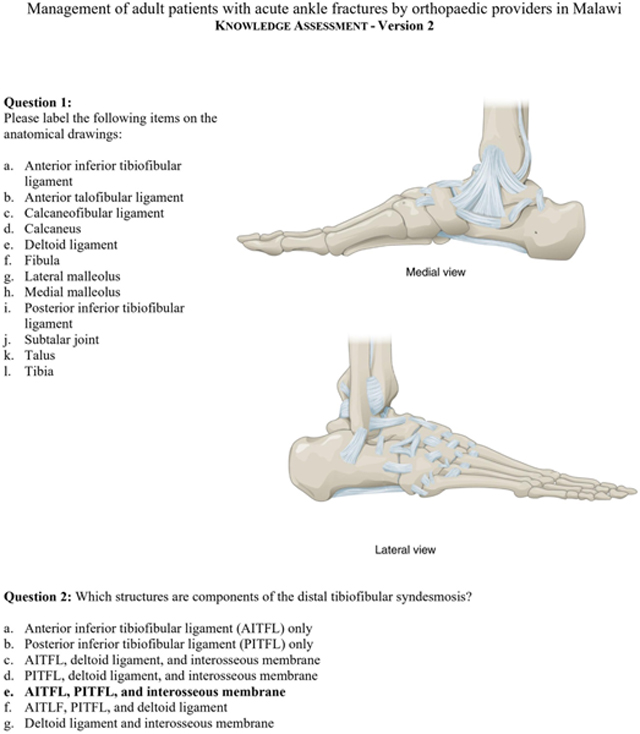
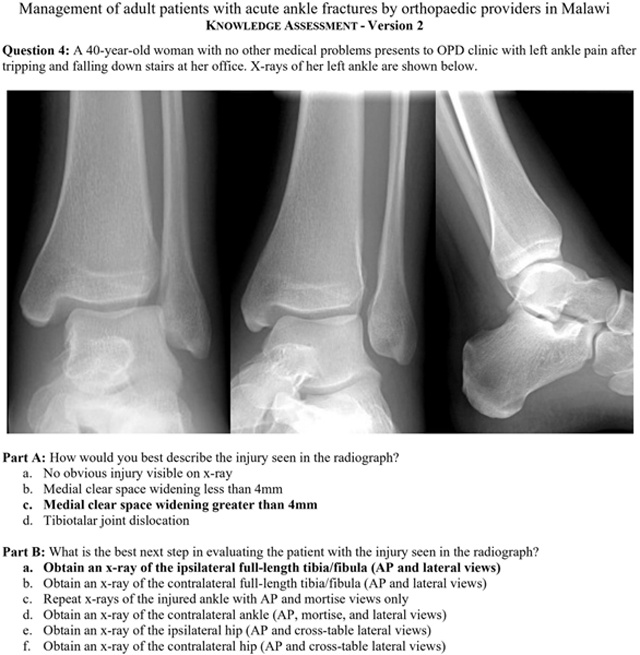
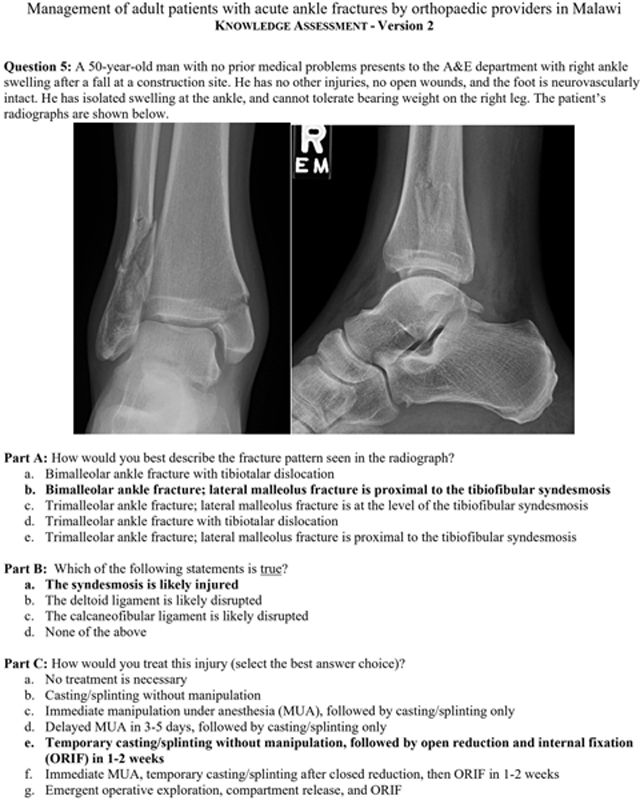
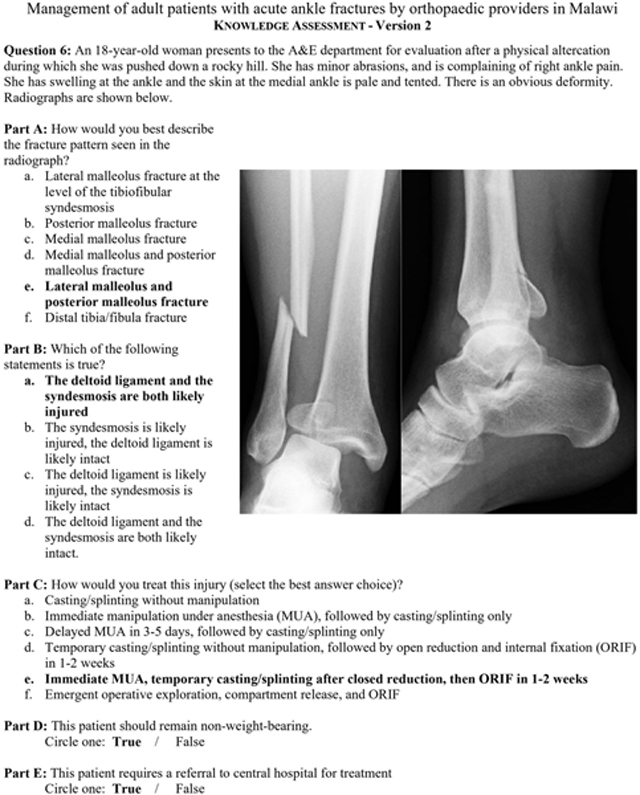
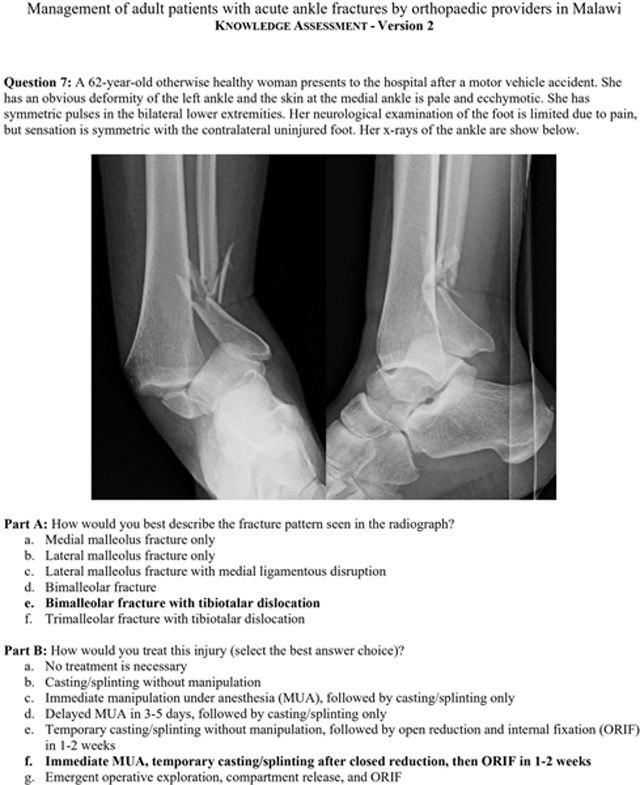
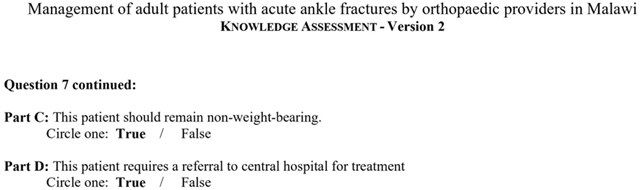
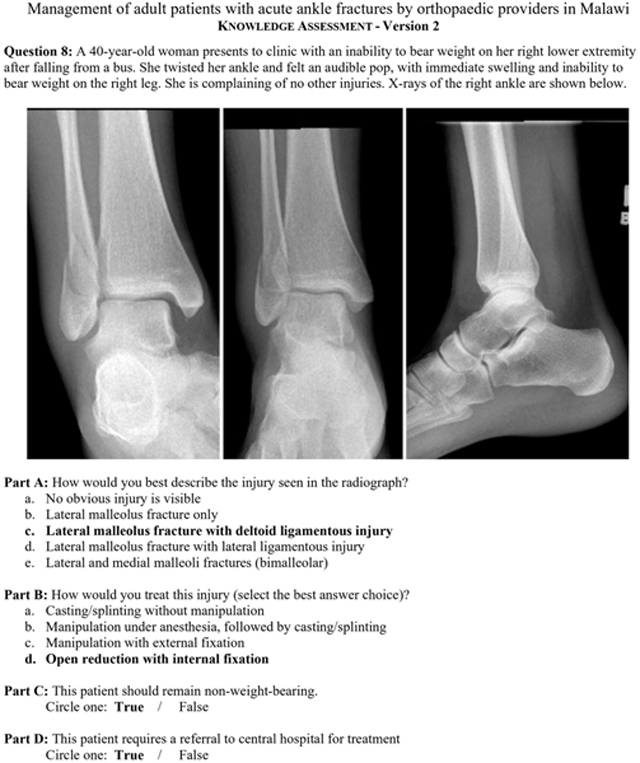
We designed a paper-based knowledge assessment (Appendix A) in English, the language of medical instruction in Malawi. This included a figure of ankle osseous and ligamentous anatomy to label, a multiple-choice question on syndesmosis anatomy, and 8 clinical vignettes with radiographs demonstrating the following fractures: Weber A lateral malleolar, Weber C lateral malleolar, bimalleolar, trimalleolar, lateral malleolar with increased medial clear space (bimalleolar-equivalent), ligamentous Maisonneuve, bimalleolar fracture-dislocation, and open trimalleolar fracture-dislocation. Multiple-choice questions tested injury identification and knowledge of ideal treatment methods. We additionally surveyed actual treatment methods used by participants. When ideal and actual treatments differed, we solicited participants’ explanations.
All orthopaedic providers working at or near KCH were invited to participate. We disclosed the subject matter immediately prior to participation, obtained informed consent, and served as proctors to ensure that external resources and peers were not consulted. No identifying information was solicited; only participants’ job titles and degrees were recorded. All participants received $10 cash compensation paid in Malawian kwacha.
Phase 2: Observations of Treatment Strategies
Between May 27 and June 28, 2019, a research assistant (A.K.) shadowed providers at KCH and invited all adults with ankle fractures encountered during routine care to participate in the study. All patients with open and closed injuries and those with acute, subacute, and chronic injuries were included. Pediatric patients (<18 years of age) and patients with polytrauma were excluded. Written informed consent was obtained in the Malawian language Chichewa and English. Patients were compensated $10 paid in Malawian kwacha.
Age, sex, residence, comorbidities, occupation, education, injury mechanism, and prior treatments were recorded for each patient using a secure smartphone-based tool (CommCare; Dimagi). The Malawian provider caring for each patient classified the injury and gave his or her intended treatment plan and rationale. Providers were not identified; only job titles and degrees were recorded.
Deidentified radiographs for each patient were collected and were analyzed post hoc by 3 U.S.-based foot and ankle fellowship-trained orthopaedic surgeons and 1 trauma fellowship-trained Malawian senior orthopaedic surgeon. Blinded to Malawian providers’ classifications and treatment plans, the reviewers independently classified each injury and gave treatment recommendations. The percent agreement and Fleiss kappa coefficient of agreement were calculated between U.S. surgeons. The differences between U.S. surgeons were discussed and were reconciled by consensus. We then compared classification and treatment recommendations between the Malawian providers, the Malawian surgeon, and U.S. surgeons, calculating the percent agreement and Cohen kappa coefficient of agreement.
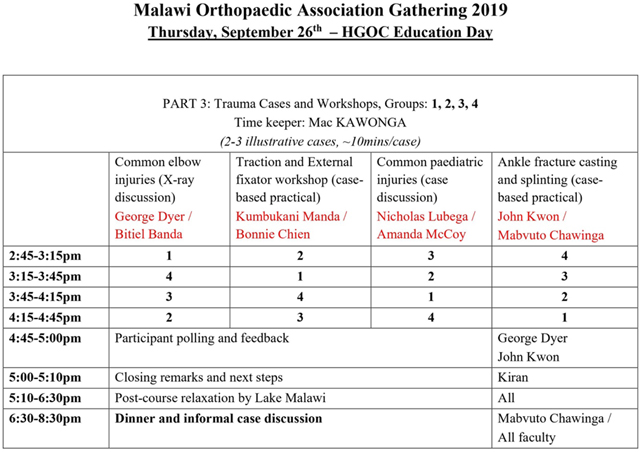
Phase 3: Educational Course
Based on Phases 1 and 2, a team of Malawian and U.S. faculty, including the study investigators, designed an educational course to review anatomy and injury classification, to review evidence-based treatment guidelines, and to present a standardized protocol for ankle fracture management feasible in Malawi (Appendix B). Jointly implemented by Malawian and U.S. faculty, the course took place on September 26, 2019, during the annual Malawi Orthopaedic Association gathering for continuing professional development. It included lectures, case-based discussions, and practical skills training (Appendix C).
Resembling the assessment in Phase 1, pre-course assessments were performed on the morning prior to the course and post-course assessments were performed on the morning after the course (Appendix D). All providers in attendance were invited to participate and written informed consent was obtained. Course instructors served as proctors to ensure that assessments were completed without the help of external resources or peers. No identifying information was solicited; only participants’ job titles and degrees were recorded. Unique participant numbers were used to match pre-course and post-course assessments, and change in performance was analyzed using paired t tests. All participants were compensated $10 paid in Malawian kwacha.
Results
Phase 1: Knowledge Assessment
Fifteen OCOs, 2 orthopaedic residents, and 1 attending physician participated. Practice experience ranged from 5 months to 29 years (median, 9.5 years [interquartile range (IQR), 5 to 11 years]). Overall, of the 35 questions, the median score was 61% (IQR, 49% to 70%) (21 questions), and performance varied widely, with participants answering 37% (13 questions) to 91% (32 questions) correctly.
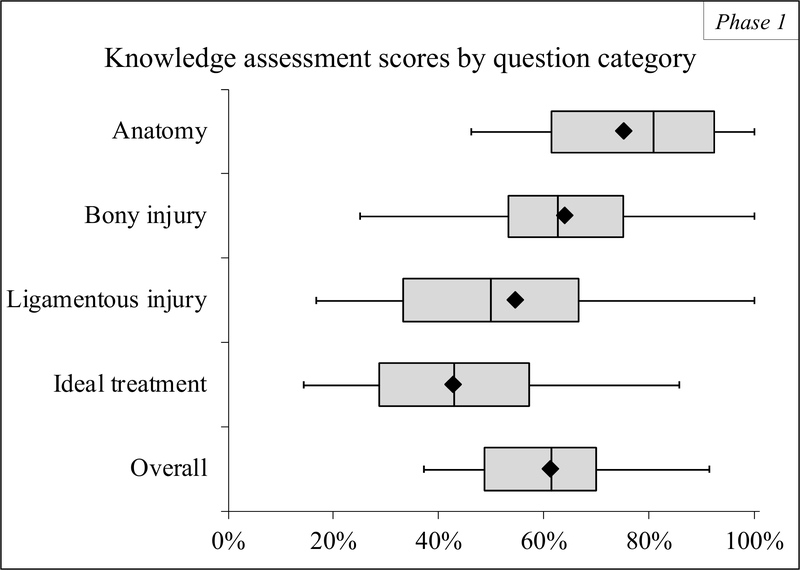
Participants scored highest in anatomy (median, 81% [IQR, 62% to 92%]), identifying a median of 6 of 7 osseous structures and 4 of 5 ligamentous structures correctly. Eight participants (44%) correctly identified syndesmotic anatomy. Participants correctly answered a median of 63% (IQR, 53% to 75%) of questions on osseous injury identification and 50% (IQR, 33% to 67%) of questions on ligamentous injury identification. Participants scored lowest in the knowledge of ideal treatment (median, 43% [IQR, 29% to 57%]) (Fig. 1).
Fig. 1.
Phase-1 knowledge assessment scores by question category. Scores for each participant were calculated as the percentage of questions answered correctly, by question category and overall. Questions were categorized as pertaining to anatomy, osseous injury identification, ligamentous injury identification, and knowledge of ideal treatment principles. In the box-and-whisker plots, the left-most boundary of the box indicates the 25th percentile, the black line within the box marks the median, the diamond marks the mean, and the right-most boundary of the box indicates the 75th percentile. Whiskers to the left and right indicate the minimum and maximum.
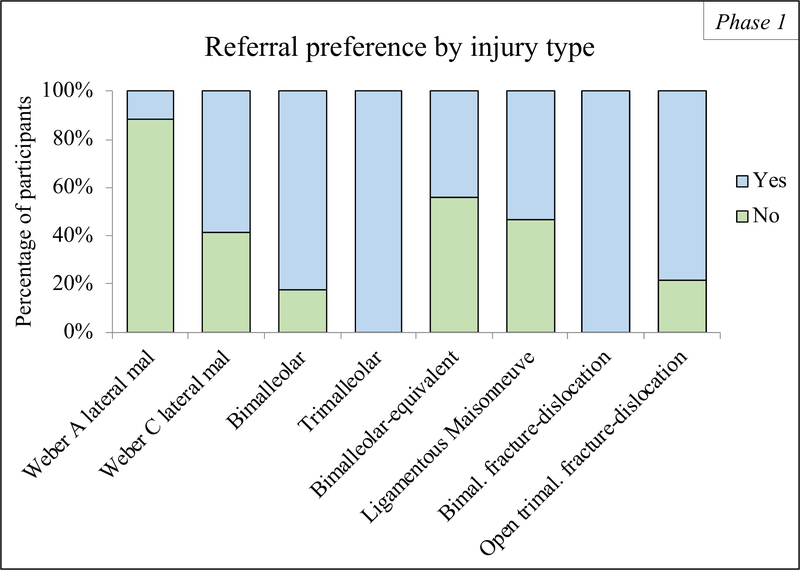
With regard to actual treatment practices, for 1 injury type (the bimalleolar-equivalent fracture), 12 (67%) of 18 participants agreed on the same treatment (manipulation under anesthesia, followed by casting or splinting). For the other 6 of the 7 injury types, there was no majority agreement (>9 of the 18 participants) on the actual treatment practice. Participants demonstrated no consensus on whether the following injuries required referral for a surgical procedure: Weber C, bimalleolar-equivalent, and ligamentous Maisonneuve (Fig. 2). Participants also identified several challenges in providing ideal treatment, most commonly resource limitations (17 [94%] of 18 participants) and inadequate training (13 [72%] of 18 participants) (Table I).
Fig. 2.
Phase-1 participants’ referral preferences for specific ankle fracture types. The percentage of participants who would (yes) or would not (no) refer a patient to central hospital for a surgical procedure is presented for each ankle fracture type tested in the knowledge assessment.
TABLE I.
Phase 1: Challenges in Delivering Ideal Treatment
| Challenge* | No. of Participants (N = 18) |
|---|---|
| Resources are too limited to give every patient the ideal treatment | 17 (94%) |
| I am not adequately trained to perform the ideal treatment | 13 (72%) |
| I do not have the necessary equipment and/or material to safely perform the ideal treatment | 8 (44%) |
| I do not have access to the facilities required to safely perform the ideal treatment | 3 (17%) |
| I rarely see this kind of injury | 1 (6%) |
Challenges denote reasons that actual treatment practices differed from ideal treatment.
For additional results, including participant demographic characteristics, performance on identifying specific injury types and their ideal treatment, and actual treatment preferences, see Appendix E.
Phase 2: Observations of Treatment Strategies
We observed treatment of 52 adults with ankle fractures, all treated by OCOs with diplomas in clinical orthopaedics as their highest qualification. The mean age was 42.6 years; 60% were male, and 92% of patients came from the Lilongwe district. Patient characteristics are summarized in Table II.
TABLE II.
Phase 2: Patient Characteristics*
| Characteristic | Value |
|---|---|
| No. of patients | 52 |
| Age* (yr) | 42.6 ± 10.4 |
| Sex† | |
| Female | 21 (40%) |
| Male | 31 (60%) |
| District† | |
| Dowa | 1 (2%) |
| Lilongwe | 48 (92%) |
| Mzimba | 1 (2%) |
| Salima | 2 (4%) |
| Employment type†‡ | |
| Formal | 27 (52%) |
| Informal | 16 (31%) |
| Unemployed, retired, or student | 9 (17%) |
| Occupation† | |
| Farmer | 4 (8%) |
| Housewife | 1 (2%) |
| Laborer | 2 (4%) |
| Office worker | 1 (2%) |
| Other | 20 (38%) |
| Small-scale business | 16 (31%) |
| Student | 1 (2%) |
| Unemployed | 7 (13%) |
| Income level†§ | |
| 0 to 10,000 kwacha/month | 14 (27%) |
| 10,001 to 20,000 kwacha/month | 3 (6%) |
| 20,001 to 30,000 kwacha/month | 7 (13%) |
| 30,001 to 40,000 kwacha/month | 3 (6%) |
| 40,001 to 50,000 kwacha/month | 7 (13%) |
| >50,000 kwacha/month | 18 (35%) |
| Education level† | |
| No schooling | 4 (8%) |
| Primary grade 1 to 4 | 8 (15%) |
| Primary grade 5 to 8 | 13 (25%) |
| Secondary or above | 27 (52%) |
| Medical comorbidities† | |
| Hypertension | 5 (10%) |
| Asthma | 2 (4%) |
| Diabetes | 1 (2%) |
| None | 44 (85%) |
| Time since injury* (days) | 49.3 ± 60.6 |
| Mechanism of injury† | |
| Other | 6 (12%) |
| Assault | 1 (2%) |
| Fall | 26 (50%) |
| Road traffic collision | 19 (37%) |
| Laterality† | |
| Left | 24 (46%) |
| Right | 28 (54%) |
| Neurovascular status† | |
| Intact | 49 (94%) |
| Sensory deficit | 1 (2%) |
| Vascular injury | 2 (4%) |
| Open fracture† | 8 (15%) |
| Referred to KCH† | 27 (52%) |
| Christian Health Association of Malawi hospital | 7 (26%) |
| District hospital | 8 (30%) |
| Health center | 11 (41%) |
| Other | 1 (4%) |
The values are given as the mean and the standard deviation.
The values are given as the number of patients, with the percentage in parentheses.
Formal employment is registered, regulated, and protected by a country’s existing legal or regulatory framework. Formal workers have work contracts, benefits, social protection, and workers’ representation. In contrast, informal employment is defined as self-employment or wage employment that is not registered, regulated, or legally protected. Informal workers do not have formal work contracts, benefits, social protection, or workers’ representation. Informal workers face higher risks of poverty than workers in the formal economy30.
10,000 Malawian kwacha ≈ $13.60 in U.S. dollars.
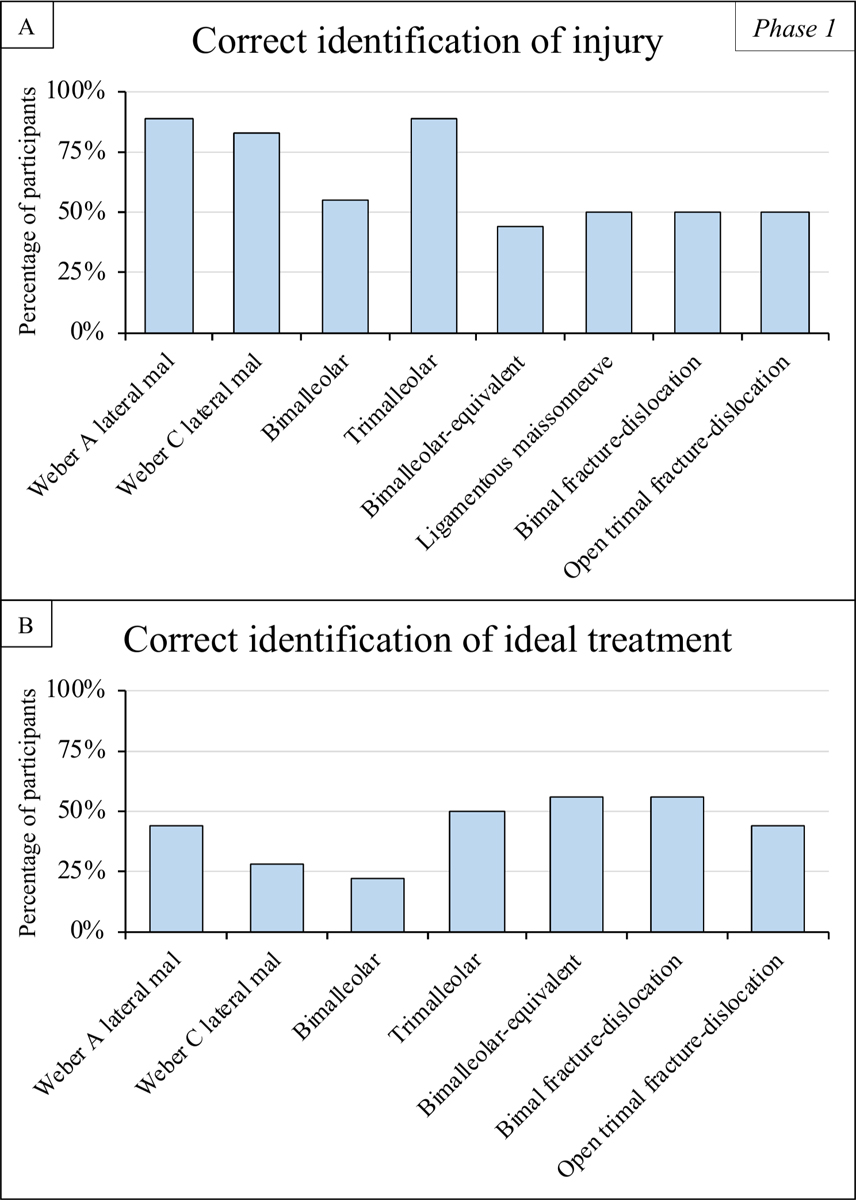
Forty-nine patients (94%) had adequate radiographs for post hoc analysis. There was substantial to near-perfect agreement between U.S. surgeons in injury characterization except syndesmotic injury identification, which had moderate agreement at 57% (Fleiss kappa, 0.35 [95% confidence interval (CI), 0.19 to 0.51]) (Table III). By U.S. surgeon consensus, there were 3 Weber-A fractures (6%), 33 Weber-B fractures (67%), and 13 Weber-C fractures (27%). Isolated lateral malleolar fractures were most common (22 [45%]), followed by bimalleolar fractures (16 [33%]) and then trimalleolar fractures (6 [12%]). Five patients (10%) had fracture-dislocations.
TABLE III.
Phase 2: Agreement in Fracture Characterization and Treatment Recommendations
| Among U.S. Surgeons* | Between Malawian OCOs and U.S. Surgeons† | |||
|---|---|---|---|---|
| Percent Agreement | Fleiss Kappa‡ | Percent Agreement | Cohen Kappa‡ | |
| Injury classification | ||||
| Weber classification | 86% | 0.79 (0.66 to 0.93) | ||
| Osseous injury | 78% | 0.77 (0.67 to 0.87) | ||
| Syndesmotic injury | 57% | 0.35 (0.19 to 0.51) | ||
| Medial clear space | 77% | 0.65 (0.43 to 0.86) | ||
| Fracture characteristics | ||||
| Nondisplaced | 78% | 0.68 (0.52 to 0.84) | 80% | 0.60 (0.38 to 0.82) |
| Displaced | 73% | 0.63 (0.47 to 0.79) | 78% | 0.57 (0.35 to 0.80) |
| Unstable | 88% | 0.83 (0.67 to 0.99) | 65% | 0.38 (0.09 to 0.66) |
| Dislocated | 92% | 0.76 (0.60 to 0.92) | 80% | 0.29 (0 to 0.66) |
| Treatment recommendation (operative vs. nonoperative) | 90% | 0.86 (0.69 to 1.00) | 65% | 0.38 (0.09 to 0.66) |
Three foot and ankle fellowship-trained orthopaedic surgeons examined deidentified radiographs for each patient in Phase 2 and gave blinded, post hoc injury characteristics and treatment recommendations.
Consensus fracture characteristics and treatment recommendations among U.S. surgeons were then compared with the fracture characteristics and intended treatment plans formulated by the Malawian OCOs caring for the patients. Malawian OCOs were not asked to provide a Weber classification or describe the osseous and ligamentous injury on radiographs.
The values are given as the kappa value, with the 95% CI in parentheses.
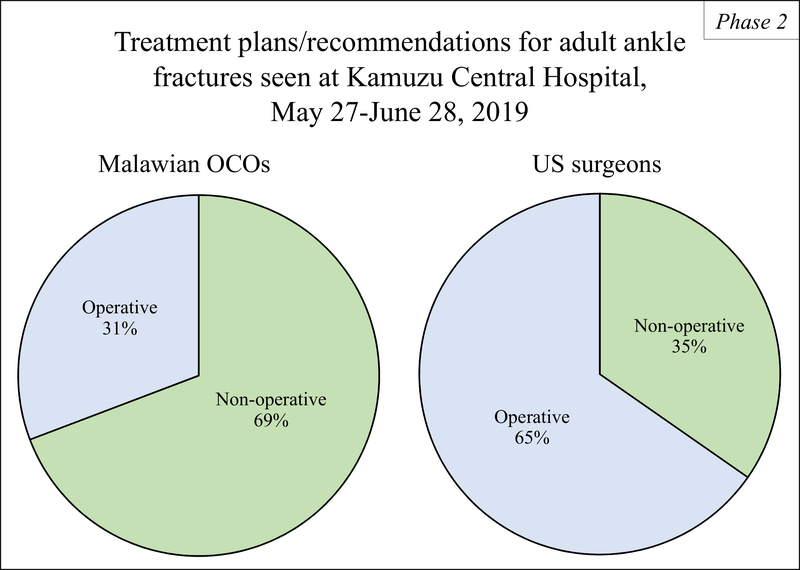
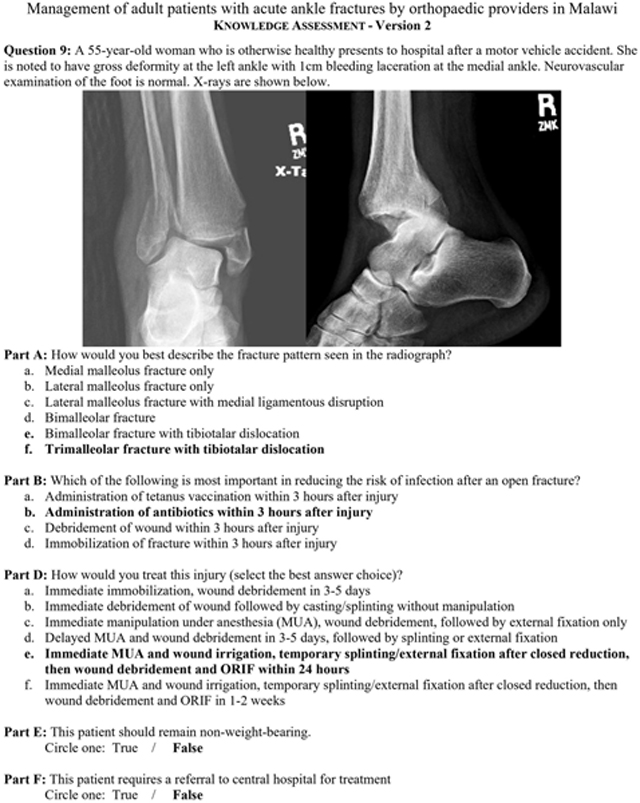
There was moderate agreement between Malawian OCOs and U.S. surgeons when identifying nondisplaced and displaced fractures, fair agreement when identifying unstable and dislocated injuries, and fair agreement when recommending nonoperative treatment compared with operative treatment (Table III). Malawian OCOs planned nonoperative management for 34 patients (69%) and planned to refer 15 patients (31%) for surgery. U.S. surgeons recommended nonoperative treatment without manipulation for 17 patients (35%). All had isolated nondisplaced lateral malleolar fractures. Operative treatment was recommended for 32 patients (65%), all of whom had displaced, unstable, and/or dislocated fractures (Fig. 3). The Malawian surgeon and the U.S. surgeons had near-perfect agreement in treatment recommendations at 94% (Cohen kappa, 0.87 [95% CI, 0.72 to 1.00]).
Fig. 3.
Comparison of Malawian OCOs’ treatment plans and U.S. surgeons’ consensus post hoc treatment recommendations for adult ankle fractures seen at KCH during Phase 2. The Malawian OCO caring for each patient provided the intended treatment plan. Three foot and ankle fellowship-trained orthopaedic surgeons based in the United States, blinded to the treatment plans of the Malawian OCOs, gave post hoc treatment recommendations based on deidentified patient radiographs.
Of the 17 patients for whom treatment recommendations differed between the Malawian OCOs and the U.S. surgeons, all met operative criteria per U.S. surgeons but were treated nonoperatively by Malawian providers. Four were treated with casting or splinting after manipulation, and 13 were treated with casting or splinting only. All were Weber-B or C injuries, classified as displaced or unstable by U.S. providers. Malawian OCOs stated that resources were too limited to provide ideal treatment for 9 (53%) of the 17 patients, including all 4 treated with casting or splinting after closed reduction. One of the 17 patients should have been treated surgically, according to the Malawian OCOs, but nonoperative treatment had already been started at a district hospital and was continued. For 7 (41%) of the 17 patients, Malawian OCOs stated that nonoperative treatment was ideal; however, the Malawian surgeon recommended a surgical procedure for 6 of these 7 patients. None of the 7 fractures were reported as displaced or unstable by Malawian OCOs.
For additional results comparing fracture classification and treatment plans and recommendations made by Malawian OCOs and U.S. surgeons, see Appendix E.
Phase 3: Educational Course
Sixty-one participants completed pre-course and post-course assessments. Fifty-five of these 61 participants were orthopaedic providers and made up 40% of all practicing orthopaedic providers in Malawi at that time. Providers represented 31 hospitals, including all 4 central hospitals and 16 of 25 district hospitals.
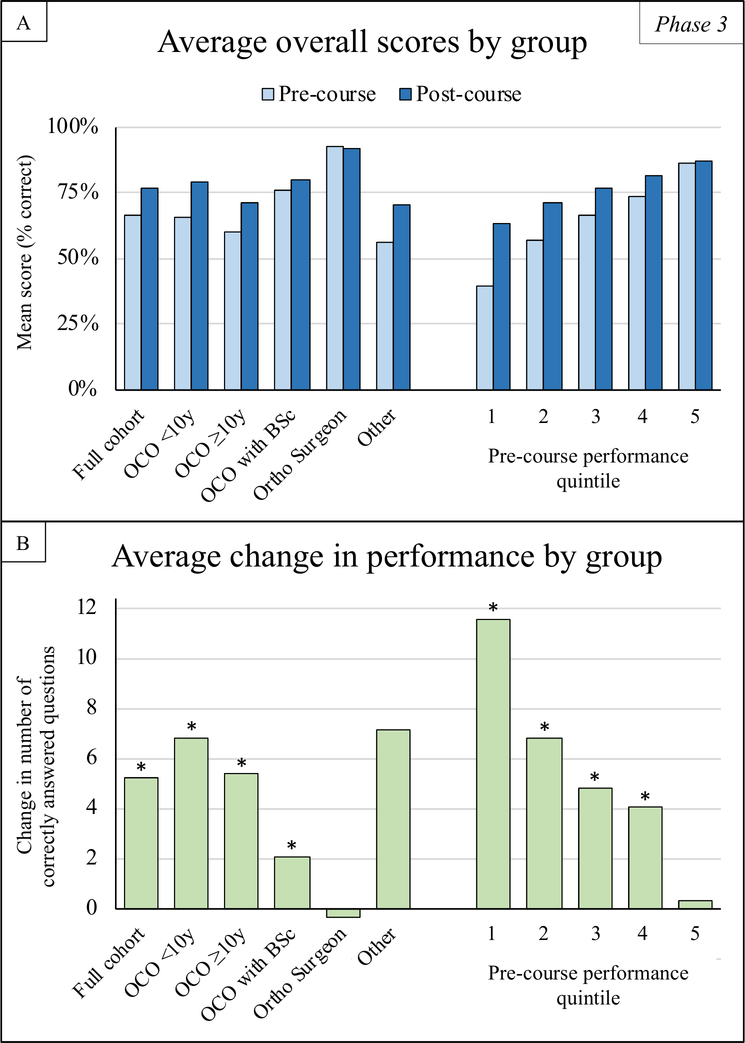
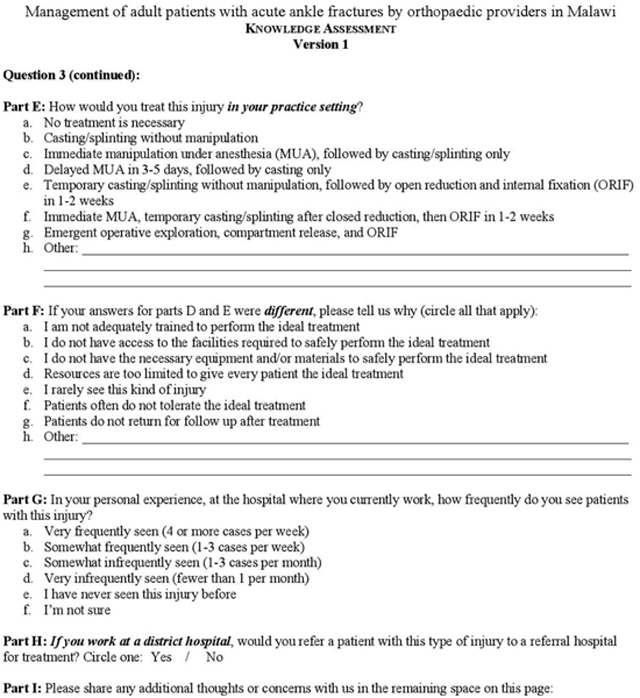
Scores improved for 51 (84%) of 61 participants. The mean overall score improved from 32.4 points (66% of 49 points) pre-course to 37.7 points (77%) post-course (Fig. 4-A). This represented a significant 5.2 additional questions (95% CI, 3.8 to 6.6 questions; p < 0.001) answered correctly. A significant improvement was found for OCOs with <10 years of experience (6.8 questions [95% CI, 4.1 to 9.6 questions]; p < 0.001), OCOs with ≥10 years of experience (5.4 questions [95% CI, 3.3 to 7.5 questions]; p < 0.001), and OCOs with a BSc (2.1 questions [95% CI, 0.4 to 3.8 questions]; p = 0.022). All participants had a significant improvement in performance except for those whose scores before the course were in the top quintile. The largest improvements were seen for those in the pre-course performance quintile 1 (11.6 questions [95% CI, 6.8 to 16.4 questions]; p < 0.001) and quintile 2 (6.8 questions [95% CI, 2.7 to 10.9 questions]; p < 0.001) (Fig. 4-B).
Fig. 4.
Figs. 4-A and 4-B Phase-3 knowledge assessment performance by participant group. Fig. 4-A The mean overall scores. The mean pre-course and post-course assessment scores (percentage of total questions answered correctly) were calculated for the cohort as a whole, by job title or years of experience (OCOs with <10 years of experience, OCOs with ≥10 years of experience, OCOs with a BSc degree, orthopaedic surgeons, and others) and by pre-course performance quintile. Fig. 4-B The mean change in performance. The change in number of questions answered correctly between the pre-course and post-course assessments was calculated for each participant. The mean change in performance was calculated by participant group. The asterisk denotes a significant change (p < 0.05) in mean scores between the pre-course and post-course assessments, calculated using paired t tests.
Overall, the cohort demonstrated a significant improvement in all question categories. The cohort was able to identify 1 more injury correctly of the 8 injuries that were tested (1.1 questions [95% CI, 0.6 to 1.6]; p < 0.001) and to identify 1 more ideal treatment of the 7 that were tested (1.0 question [95% CI, 0.5 to 1.4 questions]; p < 0.001). Greater than two-thirds were able to correctly identify all injuries in the post-course assessment except for bimalleolar fractures (48% pre-course and 54% post-course).
See Appendix E for additional results with regard to participant demographic characteristics, mean change in performance by question category, and performance on identifying specific injury types and their ideal treatment before and after the course.
Discussion
Patients sustaining ankle fractures in Malawi may be treated suboptimally because of resource limitations, knowledge deficits, and lack of treatment standardization. The expansion of surgical capacity is essential if the Malawian health-care system is to meet the needs of a rapidly growing population subject to a high trauma burden19.
In Phases 1 and 2, we found that resource limitations caused providers to deviate from evidence-based treatment practices and treat unstable fractures nonoperatively. In our previous assessment of trauma care capacity in Malawi, we found that most district hospitals lacked basic resources including radiography, likely impeding timely diagnosis and treatment decision-making. Two of 4 central hospitals (the only facilities offering surgical procedures for ankle fractures) reported limited availability of operating rooms, surgeons, and suture19. These resource limitations undoubtedly limit surgical availability and should be addressed nationally through infrastructure development and improved resource procurement and allocation19.
Phases 1 and 2 also identified that important knowledge deficits existed, largely among OCOs who are trained primarily in nonoperative treatment18. This resulted in potentially operative injuries failing to be referred to an orthopaedic surgeon. As gatekeepers to surgical procedures, OCOs must be able to properly assess an injury and determine whether it meets surgical criteria to effectively deliver care. In Phase 3, we addressed these knowledge deficits, especially with regard to the assessment of injury instability and treatment decision-making. Education is critical to building and maintaining surgical capacity21,22. Educational courses collaboratively designed by high-income country and low-income and middle-income country partners have been shown to improve provider knowledge and skills, facilitating improved care and dissemination of knowledge23,24. Participants in our educational course demonstrated an 11% mean score improvement, comparable with the results of similar orthopaedic courses conducted in Haiti24,25. Persistent knowledge deficits, especially with regard to Weber-B lateral malleolar, bimalleolar, and bimalleolar-equivalent fractures, should be addressed in future studies.
We also developed and disseminated a standardized protocol for ankle fracture management. Care standardization is essential to improve quality and safety26 and can improve resource utilization by ensuring that patients with injuries that should be treated operatively are reliably referred to central hospitals where surgical procedures are available. Recognizing that this may increase the burden on central hospitals, we designed our protocol to safely treat as many patients nonoperatively as possible. We also standardized referral practices to encourage timely transfer of surgical patients to avoid more challenging and costly treatments associated with delayed care. Our protocol (Appendix B) was intended to exist within the reality of Malawi’s current health-care system and to be revised and adapted in the future. Provider adherence and the protocol’s effects on resource utilization, provider workload, and patient outcomes must be investigated in future studies.
This study had several limitations. First, social desirability bias may have caused respondents to overreport or underreport adherence to evidence-based treatment, assuming that the study investigators desired these responses. Second, Phases 1 and 2 were conducted at KCH only, possibly limiting generalizability. We focused on care delivery at KCH, where high rates of delayed presentation and limited treatment standardization were previously observed13,27, in an effort to examine challenges where they were perhaps greatest, and thus have the greatest impact on care nationally when implementing our educational course. Third, our post hoc treatment recommendations based on radiographic review were subject to personal bias. Although not necessarily representative for all orthopaedic surgeons in high-income countries, operative treatment was recommended for open, unstable, and/or displaced ankle fractures, which was justifiable on the basis of current evidence28. There was substantial to near-perfect agreement between the 3 U.S. surgeons in all domains, except in identification of syndesmotic injury. In the absence of gross diastasis, the diagnosis of subtle syndesmotic injury on radiographs is challenging and preoperative and/or intraoperative stress testing is often required. Stress radiography, which is not commonly performed in Malawi, might have improved interrater agreement when assessing the syndesmosis29.
Fourth, Phase 2 was conducted over a 5-week period during Malawi’s dry season, possibly limiting sample size. Because fewer patients present during the dry season13, resources may have been more available to perform surgical procedures than in the rainy season19. Access to surgery for an ankle fracture may be even lower than what was observed in this study. A retrospective study might have been preferable but was impossible in this setting because detailed patient records are not kept at KCH or at most Malawian public hospitals. Despite the logistical challenges of conducting clinical research in this setting, the information gathered demonstrated important disparities between Malawian and U.S. providers’ recommendations. This underscores the need to conduct clinical research in resource-limited settings to understand why evidence-based guidelines in high-income countries may be incompletely implemented or inapplicable in low-income and middle-income countries.
Lastly, it remains unknown whether knowledge gained by Malawian providers will be retained and will translate to improved care. Further investigation of knowledge retention and adherence to the standardized protocol is necessary.
In conclusion, we demonstrate a comprehensive investigative approach to examining the challenges of providing adequate orthopaedic care for a common injury in a resource-limited country and the successful implementation of an educational intervention to improve care capacity and to standardize treatment for ankle fractures.
Acknowledgments
The authors thank Nancy Mwale, Rajab Wanyawa, and Dr. Cornelius Mukuzunga for their logistical assistance and guidance during the implementation of Phases 1 and 2; Master Yesaya and Mac Kawonga for their logistical assistance in preparation for the educational course in Phase 3; Dr. Nicholas Lubega, Dr. Kumbukani Manda, and Dr. Boston Munthali for serving as faculty for the ankle fracture course; and Dr. George Dyer, Dr. Bonnie Chien, and Dr. Amanda McCoy for making the journey to Malawi and serving as visiting faculty for the ankle fracture course. The authors also thank all the orthopaedic clinical officers, orthopaedic residents, and orthopaedic surgeons of Malawi for their participation and support of this project. Without their commitment to quality improvement, nothing would be possible. The authors especially thank all of the patients with ankle fractures who participated in this study.
Disclosure: This project was supported by a grant from Paragon 28, Inc. K.J.A.-H. and L.N.B. received grant support from the AO Alliance Foundation. K.J.A.-H. was supported by the Clinical Orthopedic and Musculoskeletal Education and Training Program at Brigham and Women’s Hospital (NIH AR-T32-055885). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
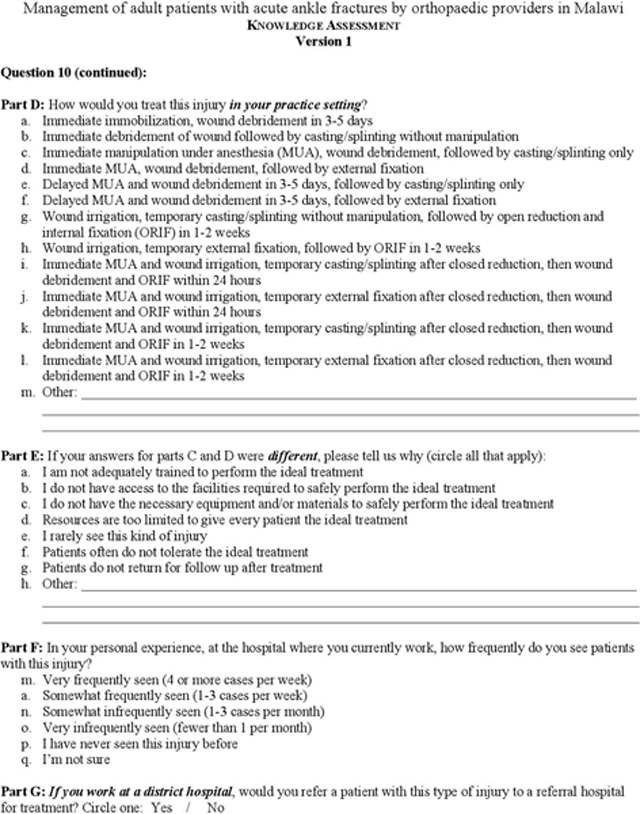
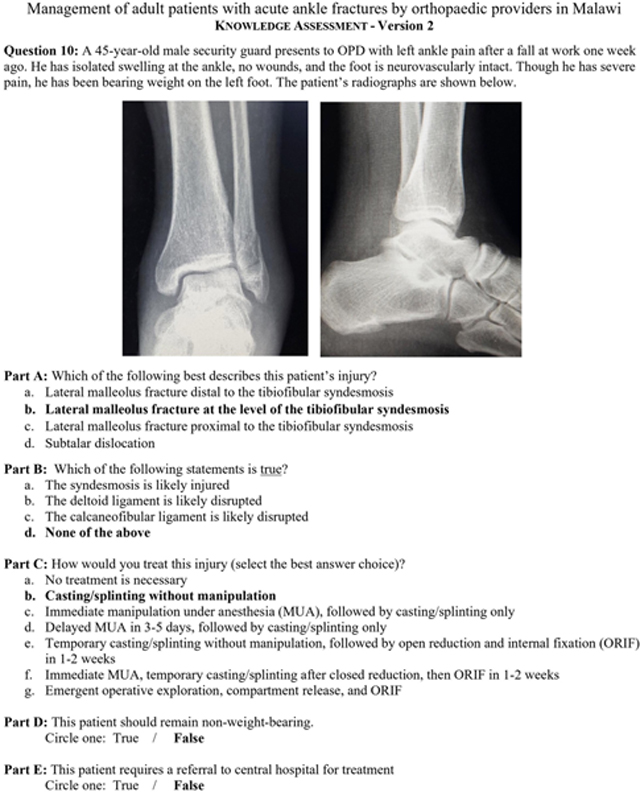
Appendix A –. Phase 1 provider knowledge assessment
Correct answers are indicated in bold, where applicable.
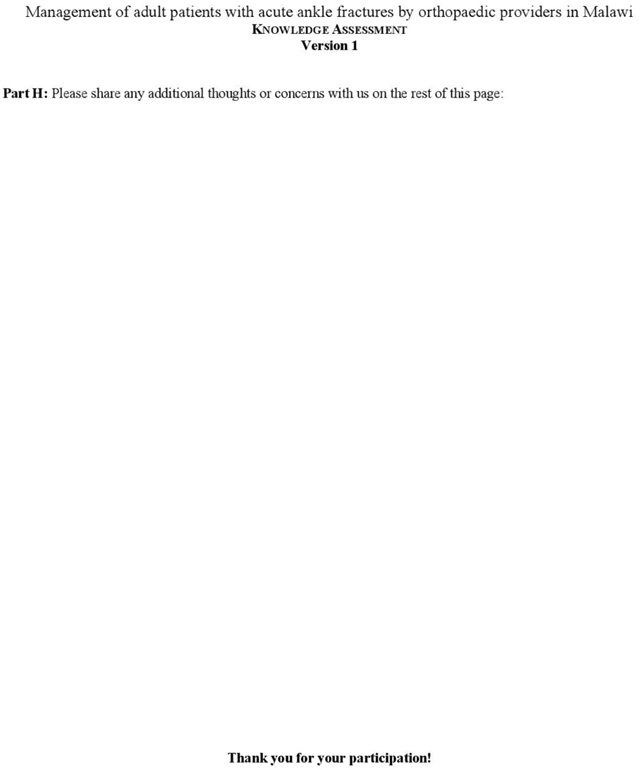
Appendix B –. Standardized protocol for ankle fracture management in Malawi
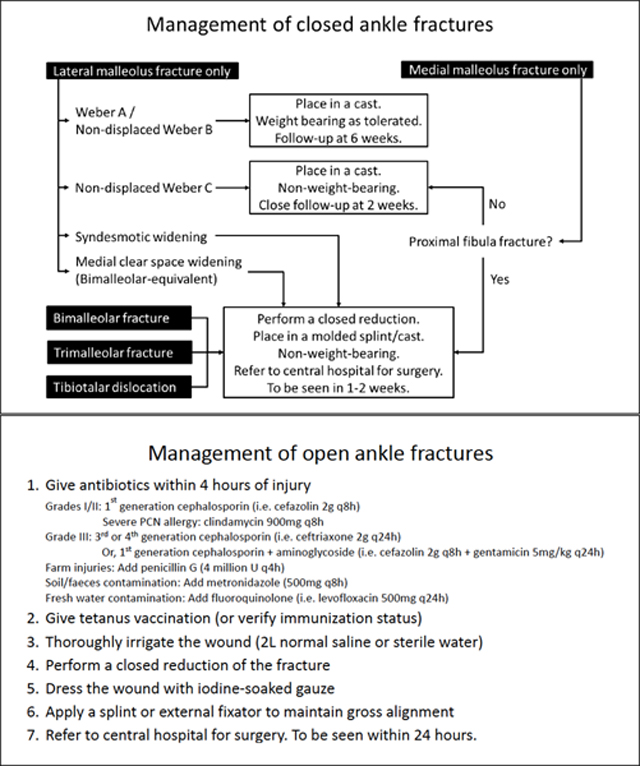
Appendix C –. Ankle fracture educational course agenda
Appendix D –. Phase 3 pre- and post-course participant knowledge assessment
Correct answers are indicated in bold, where applicable.
Appendix E –. Additional results
Phase 1
Table E1:
Phase 1 – Participant demographics
| Total | 18 |
|
| |
| Title | |
| Orthopaedic Clinical Officer | 15 |
| Orthopaedic Resident | 2 |
| Orthopaedic Surgeon | 1 |
|
| |
| Highest Level of Training | |
| Diploma | 13 |
| BSc | 2 |
| MBBS | 2 |
| MD PhD | 1 |
|
| |
| Place of Work | |
| Kamuzu Central Hospital | 10 |
| District hospital | 5 |
| Mission hospital | 2 |
| Kamuzu Barracks | 1 |
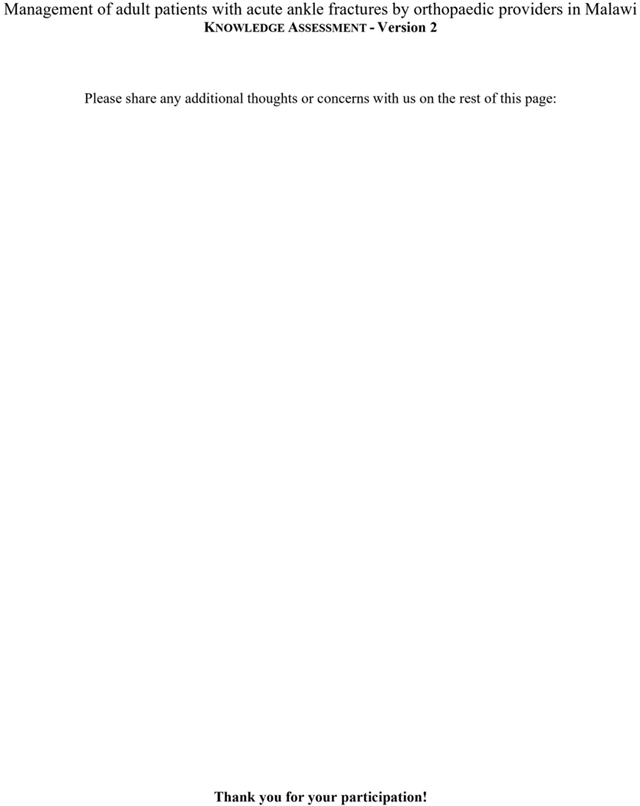
Figure E1: Percentage of phase 1 participants who A) correctly identified specific ankle fracture types, and B) correctly identified the ideal treatment of each fracture type.
The following ankle fracture types were tested: Weber A lateral malleolar, Weber C lateral malleolar, bimalleolar, trimalleolar, lateral malleolar with increased medial clear space (bimalleolar-equivalent), ligamentous Maissonneuve (only injury identification was tested), bimalleolar fracture-dislocation, and open trimalleolar fracture-dislocation.
Participants correctly answered a median of 63% of questions that tested identification of bony injuries (IQR 53-75%), and 50% of questions that tested identification of ligamentous injuries (IQR 33-67%). Sixteen participants (89%) correctly identified Weber A lateral malleolar and trimalleolar fractures, 15 (83%) correctly identified Weber C lateral malleolar fracture, 10 (56%) correctly identified bimalleolar fracture, and 9 (50%) or fewer correctly identified bimalleolar-equivalent, ligamentous Maissoneuve, bimalleolar fracture-dislocation, and open trimalleolar fracture-dislocation on x-ray.
Table E2:
Phase 1 – Actual treatment preferences
| Injury type | Treatment preference | Number of participants (%) |
|---|---|---|
|
| ||
| Weber A lateral malleolus fracture | Casting/splinting without manipulation | 9/18 (50) |
| Immediate MUA, followed by casting/splinting only | 7/18 (39) | |
|
| ||
| Weber C lateral malleolus fracture | Temporary casting/splinting without manipulation, followed by ORIF in 1–2 weeks | 5/18 (28) |
|
| ||
| Bimalleolar fracture | Immediate MUA, temporary casting/splinting after CR, then ORIF in 1–2 weeks | 7/18 (39) |
|
| ||
| Trimalleolar fracture with syndesmotic and deltoid injury | Immediate MUA, temporary casting/splinting after CR, then ORIF in 1–2 weeks | 9/18 (50) |
|
| ||
| Bimalleolar-equivalent fracture | MUA, followed by casting/splinting | 12/18 (67) |
|
| ||
| Bimalleolar fracture-dislocation | Emergent operative exploration, compartment release, and ORIF | 7/18 (39) |
| Immediate MUA, temporary casting/splinting after CR, then ORIF in 1–2 weeks | 6/18 (33) | |
|
| ||
| Open trimalleolar fracture-dislocation | Immediate MUA and wound irrigation, temporary external fixation after CR, then wound debridement and ORIF within 24 hours | 4/18 (22) |
With regards to actual treatment preferences, for eight of the nine injury types presented, no clear consensus was demonstrated, with 9 participants (50%) or fewer reporting the same treatment preference. Only for bimalleolar-equivalent fractures was a clear dominant treatment modality demonstrated, with 12 of the 18 participants reporting preferred treatment with manipulation under anesthesia (MUA) and casting/splinting.
Phase 2
Figure E2: Post-hoc classification of ankle fractures for adult patients seen at Kamuzu Central Hospital during phase 2.
Deidentified x-rays for each patient seen during phase 2 were collected and independently analyzed post-hoc by three Foot and Ankle fellowship-trained orthopaedic surgeons based in the United States. Classification differences were discussed and reconciled to give a uniform classification of each injury representing consensus among the US-based providers.
Table E3:
Phase 2 - Treatment plans/recommendations made by Malawian OCOs and US surgeons
| Treatment plans/recommendations | Malawian providers (ad hoc) | US providers (post-hoc) |
|---|---|---|
|
| ||
| Non-operative | 34 (69) | 17 (35) |
|
| ||
| Casting/splinting without manipulation | 30 (61) | 17 (35) |
| Casting/splinting after closed reduction | 4 (10) | 0 (0) |
|
| ||
| Operative | 15 (31) | 32 (65) |
|
| ||
| Temporary casting/splinting without manipulation | 8 (16) | 15 (35) |
| Temporary casting/splinting after closed reduction | 4 (8) | 17 (31) |
| No temporary immobilization | 3 (6) | 0 (0) |
|
| ||
| External Fixation | 3 (6) | 1 (2) |
| Open reduction and internal fixation | 12 (24) | 31 (63) |
Malawian OCOs planned nonoperative management for 34 patients (69%), which included casting/splinting without manipulation for 30 patients (61%) and after manipulative closed reduction for 4 patients (8%). Operative treatment was planned/performed for 15 patients (31%). Prior to surgery, temporary immobilization by casting/splinting alone was recommended for 8 patients (16%), and casting/splinting after a closed reduction was recommended for 4 patients (10%).
The US surgeons recommended non-operative treatment of casting without manipulation for 17 patients (35%). All had non-displaced fractures of the lateral malleolus only with no syndesmotic or medial clear space widening. This included all three Weber A lateral malleolus fractures, 13 Weber B fractures, and one Weber C fracture. Operative treatment was recommended for 32 patients (65%), all of which had displaced and/or unstable Weber B or C fractures. This included all 18 patients with syndesmotic injuries, and all 5 patients with medial clear space widening. Four had tibiotalar dislocations. Temporary immobilization by casting/splinting alone was recommended for 15 patients (31%), and casting/splinting after a closed reduction was recommended for 17 patients (35%). Definitive treatment with external fixation was recommended for 1 patient with an open bimalleolar fracture with syndesmotic widening and significant bone loss at the medial malleolus. For the remaining 31 patients (63%), definitive treatment with open reduction and internal fixation was recommended.
Figure E3: Percent agreement in fracture classifications by Malawian OCOs and US surgeons.
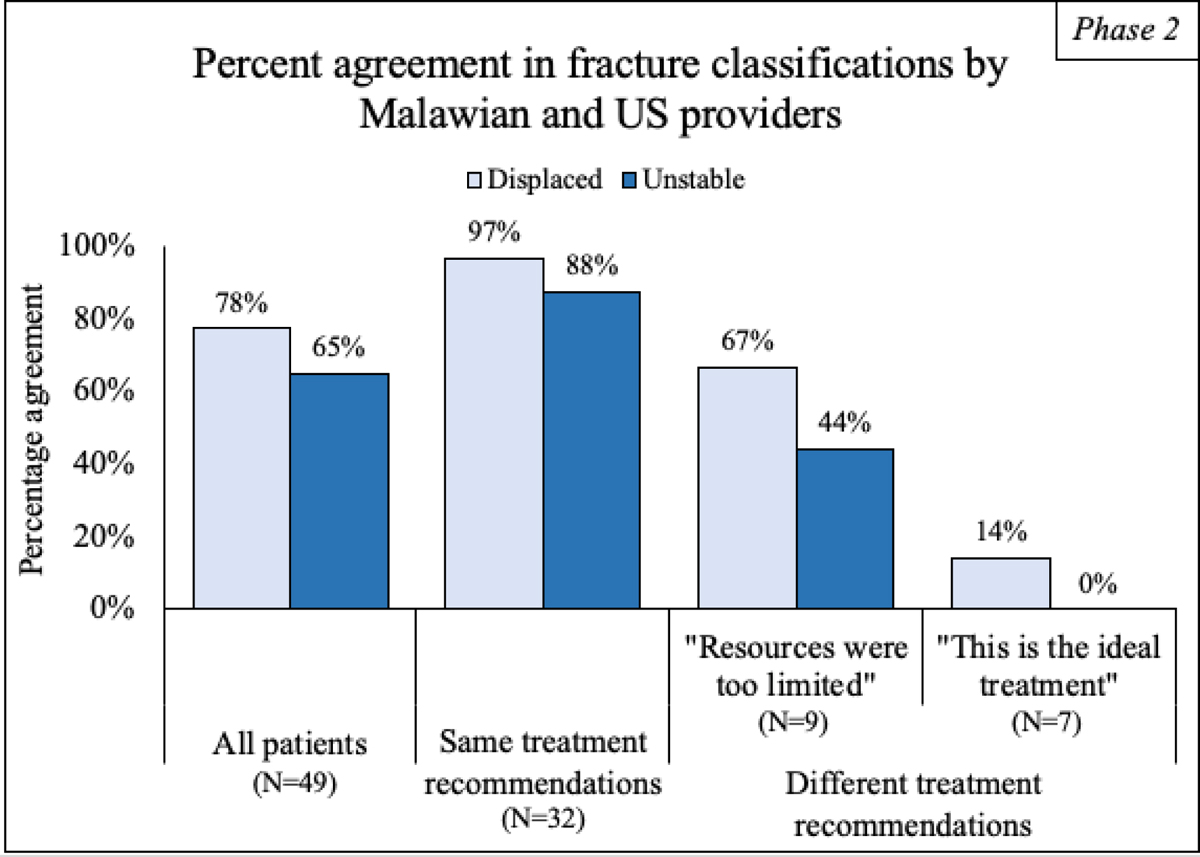
Percent agreement on fracture displacement and instability was examined for all patients, the subset of patients for whom Malawian OCOs and US surgeons made the same treatment recommendation (non-operative vs. operative), and the subset of patients for whom Malawian OCOs and US surgeons made different treatment recommendations. This last subset was further subdivided into patients for whom the Malawian OCOs stated their rationale for treatment was that resources were too limited to provide the ideal treatment, and patient for whom Malawian OCOs felt they were providing the ideal treatment.
For the patients who received the same treatment recommendations by Malawian and US providers, percentage agreement regarding fracture displacement and instability was high – 97% and 88% respectively. For the 9 patients who received different recommendations because Malawian providers felt that resources were too limited, agreement on fracture displacement remained relatively high at 67%, though agreement on fracture instability dropped to 44%. For the 7 patients who received different recommendations because Malawian providers felt non-operative care was the ideal treatment, percent agreement on fracture displacement and instability was 14% and 0%, respectively. All 7 patients’ fractures were characterized as displaced and/or unstable by the US surgeons; none were reported as displaced/unstable by Malawian OCOs.
Phase 3
Table E4:
Phase 3 - Educational course participant demographics
| Total | 61 |
|
| |
| Title | |
| Orthopaedic Clinical Officer | 52 |
| Orthopaedic Surgeon | 3 |
| Other (Prosthetist, Physiotherapist, Student) | 6 |
|
| |
| Highest Level of Training | |
| Diploma | 46 |
| BSc | 12 |
| MBBS | 3 |
|
| |
| Place of Work | |
| Central hospital | 27 |
| District hospital | 22 |
| Mission hospital | 8 |
| Other facilities (barracks, private clinics, health centers) | 4 |
Sixty-one providers completed pre- and post-course assessments. 55/61 were orthopaedic providers and made up 40% of all practicing orthopaedic providers in Malawi at that time. Providers represented 31 hospitals including all four central hospitals and 16/25 district hospitals.
Figure E4: Phase 3 knowledge assessment performance by question category.
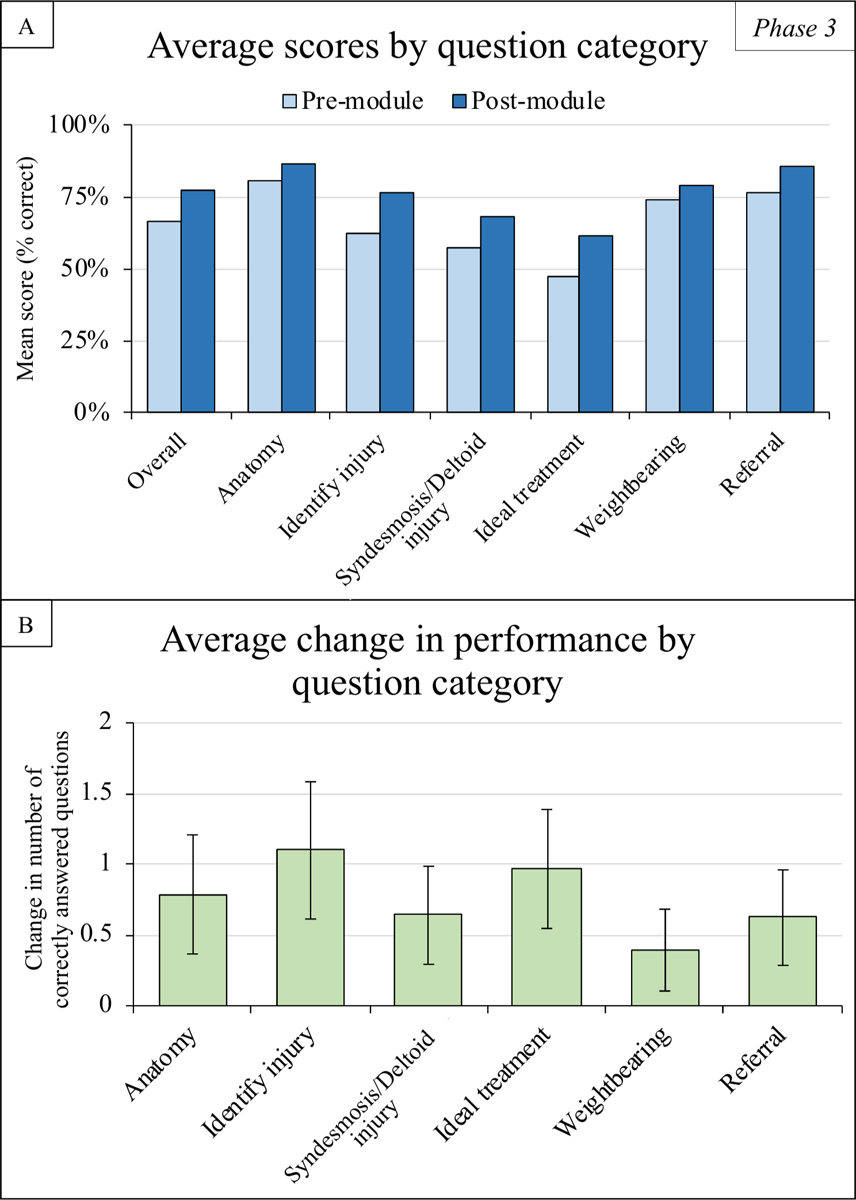
A) Average scores for entire cohort. Scores were calculated as the percentage of questions answered correctly, overall and by question category. Questions were categorized as pertaining to anatomy, injury identification, syndesmotic/deltoid injury identification, knowledge of ideal treatment principles, post-treatment weightbearing recommendations, and referral recommendations. B) Average change in performance. Change in number of questions answered correctly between the pre- and post-course assessments was calculated for each participant. Average change in performance was calculated by question category. Error bars denotes 95% confidence intervals. All changes between the pre- and post-course assessments were statistically significant (p<0.05), as calculated using paired t-tests.
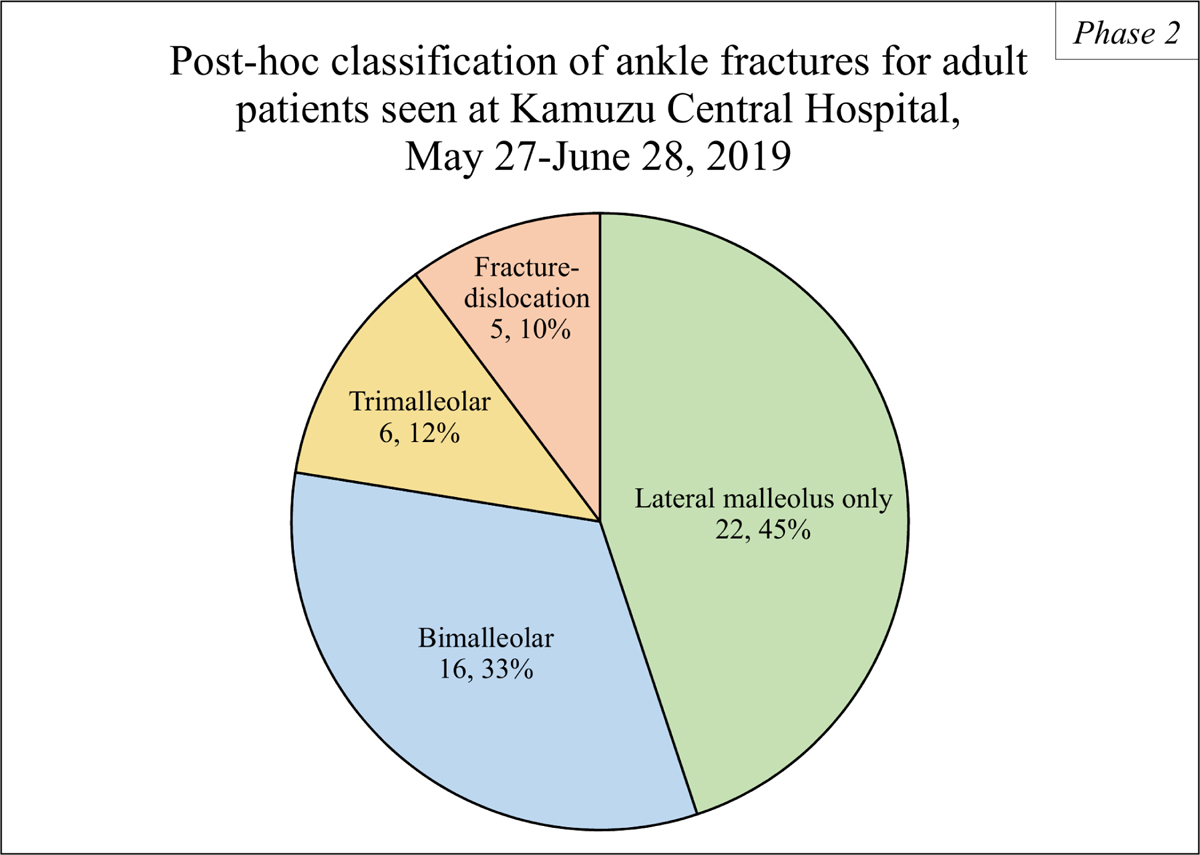
Figure E5: Percentage of phase 3 participants who A) correctly identified specific ankle fracture types, and B) correctly identified the ideal treatment of each fracture type.
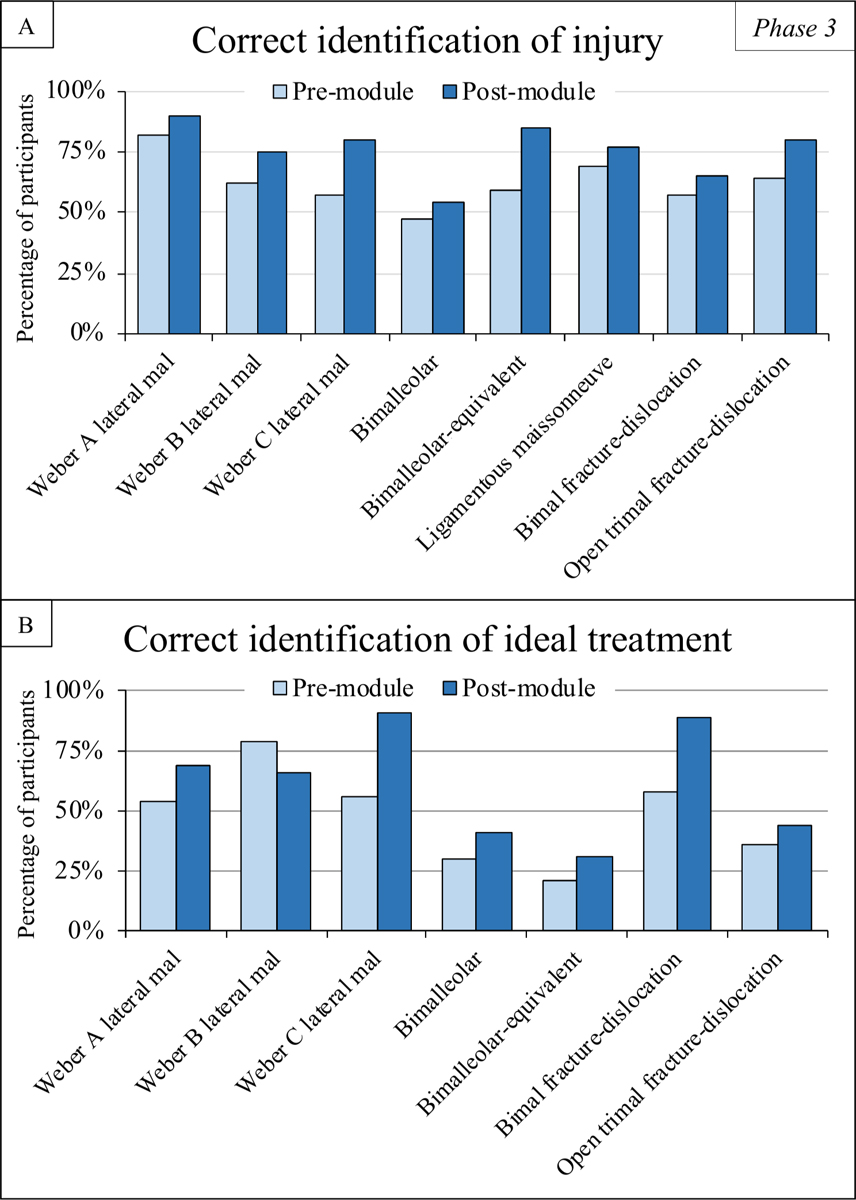
Pre- and post-course performance are demonstrated. The following ankle fracture types were tested: Weber A lateral malleolar, Weber B lateral malleolar, Weber C lateral malleolar, bimalleolar, lateral malleolar with increased medial clear space (bimalleolar-equivalent), ligamentous Maissonneuve (only injury identification was tested), bimalleolar fracture-dislocation, and open trimalleolar fracture-dislocation.
Greater than two-thirds of the cohort was able to correctly identify all injuries in the post-course assessment except for bimalleolar fractures which were identified correctly by 48% pre-course and 54% post-course (Figure E5A). Participants improved in their ability to identify the correct ideal treatment of all injuries except Weber B lateral malleolar fractures, for which 79% of participants identified it correctly pre-course compared to 66% post-course. In the post-course assessment, greater than two-thirds of the cohort was able to correctly identify the ideal treatment of all injuries except bimalleolar, bimalleolar-equivalent, and open trimalleolar fracture-dislocations (Figure E5B).
Footnotes
The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org.
References
- 1.Debas HT, Gosselin R, McCord C, Thind A. Surgery. In: Jamison DT, editor. Disease control priorities in developing countries. 2nd ed. New York: Oxford University Press; 2006. p. 1245–60. [Google Scholar]
- 2.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Barker-Collo S, Bartels DH, Bell ML, Benjamin EJ, Bennett D, Bhalla K, Bikbov B, Bin Abdulhak A, Birbeck G, Blyth F, Bolliger I, Boufous S, Bucello C, Burch M, Burney P, Carapetis J, Chen H, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahodwala N, De Leo D, Degenhardt L, Delossantos A, Denenberg J, Des Jarlais DC, Dharmaratne SD, Dorsey ER, Driscoll T, Duber H, Ebel B, Erwin PJ, Espindola P, Ezzati M, Feigin V, Flaxman AD, Forouzanfar MH, Fowkes FG, Franklin R, Fransen M, Freeman MK, Gabriel SE, Gakidou E, Gaspari F, Gillum RF, Gonzalez-Medina D, Halasa YA, Haring D, Harrison JE, Havmoeller R, Hay RJ, Hoen B, Hotez PJ, Hoy D, Jacobsen KH, James SL, Jasrasaria R, Jayaraman S, Johns N, Karthikeyan G, Kassebaum N, Keren A, Khoo JP, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Lipnick M, Lipshultz SE, Ohno SL, Mabweijano J, MacIntyre MF, Mallinger L, March L, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGrath J, Mensah GA, Merriman TR, Michaud C, Miller M, Miller TR, Mock C, Mocumbi AO, Mokdad AA, Moran A, Mulholland K, Nair MN, Naldi L, Narayan KM, Nasseri K, Norman P, O’Donnell M, Omer SB, Ortblad K, Osborne R, Ozgediz D, Pahari B, Pandian JD, Rivero AP, Padilla RP, Perez-Ruiz F, Perico N, Phillips D, Pierce K, Pope CA 3rd, Porrini E, Pourmalek F, Raju M, Ranganathan D, Rehm JT, Rein DB, Remuzzi G, Rivara FP, Roberts T, De León FR, Rosenfeld LC, Rushton L, Sacco RL, Salomon JA, Sampson U, Sanman E, Schwebel DC, Segui-Gomez M, Shepard DS, Singh D, Singleton J, Sliwa K, Smith E, Steer A, Taylor JA, Thomas B, Tleyjeh IM, Towbin JA, Truelsen T, Undurraga EA, Venketasubramanian N, Vijayakumar L, Vos T, Wagner GR, Wang M, Wang W, Watt K, Weinstock MA, Weintraub R, Wilkinson JD, Woolf AD, Wulf S, Yeh PH, Yip P, Zabetian A, Zheng ZJ, Lopez AD, Murray CJ, AlMazroa MA, Memish ZA. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012December15;380(9859):2095–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kotagal M, Agarwal-Harding KJ, Mock C, Quansah R, Arreola-Risa C, Meara JG. Health and economic benefits of improved injury prevention and trauma care worldwide. PLoS One. 2014March13;9(3):e91862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, Abraham J, Ackerman I, Aggarwal R, Ahn SY, Ali MK, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Bahalim AN, Barker-Collo S, Barrero LH, Bartels DH, Basáñez MG, Baxter A, Bell ML, Benjamin EJ, Bennett D, Bernabé E, Bhalla K, Bhandari B, Bikbov B, Bin Abdulhak A, Birbeck G, Black JA, Blencowe H, Blore JD, Blyth F, Bolliger I, Bonaventure A, Boufous S, Bourne R, Boussinesq M, Braithwaite T, Brayne C, Bridgett L, Brooker S, Brooks P, Brugha TS, Bryan-Hancock C, Bucello C, Buchbinder R, Buckle G, Budke CM, Burch M, Burney P, Burstein R, Calabria B, Campbell B, Canter CE, Carabin H, Carapetis J, Carmona L, Cella C, Charlson F, Chen H, Cheng AT, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahiya M, Dahodwala N, Damsere-Derry J, Danaei G, Davis A, De Leo D, Degenhardt L, Dellavalle R, Delossantos A, Denenberg J, Derrett S, Des Jarlais DC, Dharmaratne SD, Dherani M, Diaz-Torne C, Dolk H, Dorsey ER, Driscoll T, Duber H, Ebel B, Edmond K, Elbaz A, Ali SE, Erskine H, Erwin PJ, Espindola P, Ewoigbokhan SE, Farzadfar F, Feigin V, Felson DT, Ferrari A, Ferri CP, Fèvre EM, Finucane MM, Flaxman S, Flood L, Foreman K, Forouzanfar MH, Fowkes FG, Franklin R, Fransen M, Freeman MK, Gabbe BJ, Gabriel SE, Gakidou E, Ganatra HA, Garcia B, Gaspari F, Gillum RF, Gmel G, Gosselin R, Grainger R, Groeger J, Guillemin F, Gunnell D, Gupta R, Haagsma J, Hagan H, Halasa YA, Hall W, Haring D, Haro JM, Harrison JE, Havmoeller R, Hay RJ, Higashi H, Hill C, Hoen B, Hoffman H, Hotez PJ, Hoy D, Huang JJ, Ibeanusi SE, Jacobsen KH, James SL, Jarvis D, Jasrasaria R, Jayaraman S, Johns N, Jonas JB, Karthikeyan G, Kassebaum N, Kawakami N, Keren A, Khoo JP, King CH, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Lalloo R, Laslett LL, Lathlean T, Leasher JL, Lee YY, Leigh J, Lim SS, Limb E, Lin JK, Lipnick M, Lipshultz SE, Liu W, Loane M, Ohno SL, Lyons R, Ma J, Mabweijano J, MacIntyre MF, Malekzadeh R, Mallinger L, Manivannan S, Marcenes W, March L, Margolis DJ, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGill N, McGrath J, Medina-Mora ME, Meltzer M, Mensah GA, Merriman TR, Meyer AC, Miglioli V, Miller M, Miller TR, Mitchell PB, Mocumbi AO, Moffitt TE, Mokdad AA, Monasta L, Montico M, Moradi-Lakeh M, Moran A, Morawska L, Mori R, Murdoch ME, Mwaniki MK, Naidoo K, Nair MN, Naldi L, Narayan KM, Nelson PK, Nelson RG, Nevitt MC, Newton CR, Nolte S, Norman P, Norman R, O’Donnell M, O’Hanlon S, Olives C, Omer SB, Ortblad K, Osborne R, Ozgediz D, Page A, Pahari B, Pandian JD, Rivero AP, Patten SB, Pearce N, Padilla RP, Perez-Ruiz F, Perico N, Pesudovs K, Phillips D, Phillips MR, Pierce K, Pion S, Polanczyk GV, Polinder S, Pope CA 3rd, Popova S, Porrini E, Pourmalek F, Prince M, Pullan RL, Ramaiah KD, Ranganathan D, Razavi H, Regan M, Rehm JT, Rein DB, Remuzzi G, Richardson K, Rivara FP, Roberts T, Robinson C, De Leòn FR, Ronfani L, Room R, Rosenfeld LC, Rushton L, Sacco RL, Saha S, Sampson U, Sanchez-Riera L, Sanman E, Schwebel DC, Scott JG, Segui-Gomez M, Shahraz S, Shepard DS, Shin H, Shivakoti R, Singh D, Singh GM, Singh JA, Singleton J, Sleet DA, Sliwa K, Smith E, Smith JL, Stapelberg NJ, Steer A, Steiner T, Stolk WA, Stovner LJ, Sudfeld C, Syed S, Tamburlini G, Tavakkoli M, Taylor HR, Taylor JA, Taylor WJ, Thomas B, Thomson WM, Thurston GD, Tleyjeh IM, Tonelli M, Towbin JA, Truelsen T, Tsilimbaris MK, Ubeda C, Undurraga EA, van der Werf MJ, van Os J, Vavilala MS, Venketasubramanian N, Wang M, Wang W, Watt K, Weatherall DJ, Weinstock MA, Weintraub R, Weisskopf MG, Weissman MM, White RA, Whiteford H, Wiersma ST, Wilkinson JD, Williams HC, Williams SR, Witt E, Wolfe F, Woolf AD, Wulf S, Yeh PH, Zaidi AKM, Zheng ZJ, Zonies D, Lopez AD, Murray CJL, AlMazroa MA, Memish ZA. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012December15;380(9859):2163–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gosselin RA, Spiegel DA, Coughlin R, Zirkle LG. Injuries: the neglected burden in developing countries. Bull World Health Organ. 2009April;87(4):246–246a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Global Status Report on Road Safety 2013: Supporting a decade of action. Geneva: World Health Organization; 2013. [Google Scholar]
- 7.Mock C, Cherian MN. The global burden of musculoskeletal injuries: challenges and solutions. Clin Orthop Relat Res. 2008October;466(10):2306–16. Epub 2008 Aug 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alkire BC, Raykar NP, Shrime MG, Weiser TG, Bickler SW, Rose JA, Nutt CT, Greenberg SL, Kotagal M, Riesel JN, Esquivel M, Uribe-Leitz T, Molina G, Roy N, Meara JG, Farmer PE. Global access to surgical care: a modelling study. Lancet Glob Health. 2015June;3(6):e316–23. Epub 2015 Apr 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spiegel DA, Nduaguba A, Cherian MN, Monono M, Kelley ET. Deficiencies in the availability of essential musculoskeletal surgical services at 883 health facilities in 24 low- and lower-middle-income countries. World J Surg. 2015June;39(6):1421–32. [DOI] [PubMed] [Google Scholar]
- 10.The World Bank. Health nutrition and population statistics. 2017. Accessed 2019 Mar 20. https://datacatalog.worldbank.org/dataset/health-nutrition-and-population-statistics
- 11.The World Bank. Poverty and equity database. 2016. Accessed 2019 Jan 15. https://datacatalog.worldbank.org/dataset/poverty-and-equity-database
- 12.Varela C, Young S, Groen R, Banza L, Mkandawire NC, Viste A. Untreated surgical conditions in Malawi: a randomised cross-sectional nationwide household survey. Malawi Med J. 2017September;29(3):231–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agarwal-Harding KJ, Chokotho LC, Mkandawire NC, Martin C Jr, Losina E, Katz JN. Risk factors for delayed presentation among patients with musculoskeletal injuries in Malawi. J Bone Joint Surg Am. 2019May15;101(10):920–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yablon IG, Heller FG, Shouse L. The key role of the lateral malleolus in displaced fractures of the ankle. J Bone Joint Surg Am. 1977March;59(2):169–73. [PubMed] [Google Scholar]
- 15.Toth MJ, Yoon RS, Liporace FA, Koval KJ. What’s new in ankle fractures. Injury. 2017October;48(10):2035–41. Epub 2017 Aug 9. [DOI] [PubMed] [Google Scholar]
- 16.Robertson GA, Wood AM, Aitken SA, Court Brown C. Epidemiology, management, and outcome of sport-related ankle fractures in a standard UK population. Foot Ankle Int. 2014November;35(11):1143–52. Epub 2014 Aug 4. [DOI] [PubMed] [Google Scholar]
- 17.Grimes CE, Mkandawire NC, Billingsley ML, Ngulube C, Cobey JC. The cost-effectiveness of orthopaedic clinical officers in Malawi. Trop Doct. 2014July;44(3):128–34. Epub 2014 May 12. [DOI] [PubMed] [Google Scholar]
- 18.Mkandawire N, Ngulube C, Lavy C. Orthopaedic clinical officer program in Malawi: a model for providing orthopaedic care. Clin Orthop Relat Res. 2008October;466(10):2385–91. Epub 2008 Jul 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Agarwal-Harding KJ, Chokotho L, Young S, Mkandawire N, Chawinga M, Losina E, Katz JN. Assessing the capacity of Malawi’s district and central hospitals to manage traumatic diaphyseal femoral fractures in adults. PLoS One. 2019November20;14(11):e0225254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lau BC, Wu HH, Mustafa M, Ibrahim J, Conway D, Agarwal-Harding K, Shearer DW, Chokotho L. Developing research to change policy: design of a multicenter cost-effectiveness analysis comparing intramedullary nailing to skeletal traction in Malawi. J Orthop Trauma. 2018October;32(Suppl 7):S52–7. [DOI] [PubMed] [Google Scholar]
- 21.Davis D Continuing medical education. Global health, global learning. BMJ. 1998January31;316(7128):385–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Agarwal-Harding KJ, von Keudell A, Zirkle LG, Meara JG, Dyer GS. Understanding and addressing the global need for orthopaedic trauma care. J Bone Joint Surg Am. 2016November2;98(21):1844–53. [DOI] [PubMed] [Google Scholar]
- 23.Carey JN, Caldwell AM, Coughlin RR, Hansen S. Building orthopaedic trauma capacity: IGOT international SMART course. J Orthop Trauma. 2015October;29(Suppl 10):S17–9. [DOI] [PubMed] [Google Scholar]
- 24.Fils J, Bhashyam AR, Pierre JB, Meara JG, Dyer GS. Short-term performance improvement of a continuing medical education program in a low-income country. World J Surg. 2015October;39(10):2407–12. [DOI] [PubMed] [Google Scholar]
- 25.Karhade AV, Qudsi RA, Usoro AO, Dejean CB, Dyer GSM. Education improves musculoskeletal radiology interpretation by trainees in a low-resource setting. J Surg Educ. 2019Nov-Dec;76(6):1605–11. Epub 2019 Jun 17. [DOI] [PubMed] [Google Scholar]
- 26.Rozich JD, Howard RJ, Justeson JM, Macken PD, Lindsay ME, Resar RK. Standardization as a mechanism to improve safety in health care. Jt Comm J Qual Saf. 2004January;30(1):5–14. [DOI] [PubMed] [Google Scholar]
- 27.Agarwal-Harding KJ, Atadja L, Chokotho LC, Banza LN, Mkandawire N, Katz JN. The experiences of adult patients receiving treatment for femoral shaft fractures at Kamuzu Central Hospital, Malawi: a qualitative analysis. 2020. Unpublished data.
- 28.Coles CP, Tornetta P 3rd, Obremskey WT, Spitler CA, Ahn J, Mirick G, Krause P, Nana A, Rodriguez-Buitrago A; Orthopaedic Trauma Associationʼs Evidence-Based Quality Value and Safety Committee. Ankle fractures: an expert survey of Orthopaedic Trauma Association members and evidence-based treatment recommendations. J Orthop Trauma. 2019September;33(9):e318–24. [DOI] [PubMed] [Google Scholar]
- 29.Marmor M, Hansen E, Han HK, Buckley J, Matityahu A. Limitations of standard fluoroscopy in detecting rotational malreduction of the syndesmosis in an ankle fracture model. Foot Ankle Int. 2011June;32(6):616–22. [DOI] [PubMed] [Google Scholar]
- 30.International Labour Office. Report V (1). Transitioning from the informal to the formal economy. International Labour Conference, 103rd Session, 2014. 2014. Accessed 2020 Nov 17. https://www.ilo.org/wcmsp5/groups/public/---ed_norm/---relconf/documents/meetingdocument/wcms_218128.pdf