Abstract
The COVID-19 pandemic has impacted health systems and health programs across the world. For tuberculosis (TB), it is predicted to set back progress by at least twelve years. Public private mix (PPM)has made a vital contribution to reach End TB targets with a ten-fold rise in TB notifications from private providers between 2012 and 2019. This is due in large part to the efforts of intermediary agencies, which aggregate demand from private providers. The COVID-19 pandemic has put these gains at risk over the past year. In this rapid assessment, representatives of 15 intermediary agencies from seven countries that are considered the highest priority for PPM in TB care (the Big Seven) share their views on the impact of COVID-19 on their programs, the private providers operating under their PPM schemes, and their private TB clients.
All intermediaries reported a drop in TB testing and notifications, and the closure of some private practices. While travel restrictions and the fear of contracting COVID-19 were the main contributing factors, there were also unanticipated expenses for private providers, which were transferred to patients via increased prices. Intermediaries also had their routine activities disrupted and had to shift tasks and budgets to meet the new needs. However, the intermediaries and their partners rapidly adapted, including an increased use of digital tools, patient-centric services, and ancillary support for private providers.
Despite many setbacks, the COVID-19 pandemic has underlined the importance of effective private sector engagement. The robust approach to fight COVID-19 has shown the possibilities for ending TB with a similar approach, augmented by the digital revolution around treatment and diagnostics and the push to decentralize health services.
Keywords: Tuberculosis, COVID-19, Public-private mix, PPM, Health system, Private sector
1. Introduction
It has been over a year since COVID-19 was declared a pandemic. In addition to the over 3.29 million deaths attributed to COVID-19 to date [1], the pandemic threatens to reverse previous gains in public health outcomes, especially those in the fight against tuberculosis (TB). In a global survey by civil society organizations released in September 2020, 63% of healthcare workers from countries with grants from the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund) reported reductions in the number of people with TB coming to healthcare facilities for treatment [2]. Data from World Health Organization (WHO) in March 2021 shows that COVID-19 related disruptions have severely impacted over 84 countries with 1.4 million fewer people estimated to have received TB care in 2020 than in 2019 - a reduction of 21% from 2019 [3]. These COVID-19 related disruptions are estimated to cause an additional half a million TB deaths [3] and a setback of nearly 12 years [4].
Seven of the highest TB-burden countries (Bangladesh, India, Indonesia, Myanmar, Nigeria, Pakistan, and the Philippines), also known as the “Big Seven” priority countries for Public Private Mix (PPM), account for 60% of the global missing cases [5]. In these countries, 32% to 74% of the population seeks care in the private sector [6]. The proportion of total notifications contributed by the for-profit sector in these Big Seven countries has risen from 5% in 2012 to nearly 28% in 2019 [7], thereby helping countries to close the gaps in TB notification and underlining the importance of multisectoral framework to End TB [8]. This response has been enabled substantially by the emergence of Non-Governmental Organizations (NGOs) that can act as intermediaries and bridge the gaps between private providers and the government [9]. A number of these intermediary NGOs, plus the burden of TB and COVID=19 in these countries, is outlined in Table 1.
Table 1.
Context of TB, COVID-19 and PPM in countries that were analyzed.
| Country | Population (millions) | COVID-19 burden [1] |
TB profile in 2019 [5] |
Context of Intermediary agencies who were interviewed |
|||||
|---|---|---|---|---|---|---|---|---|---|
| Total cases to date | Total death to date | Total TB Incidence (thousands) | Missing cases (thousands) | No. of Private TB notifications in 2019[6] | PPM Intermediary agency interviewed | Scope of the interviewed Intermediary Agency in Country’s PPM initiatives for TB | Drop in TB notification/diagnostics/private practice in comparison to 2019a | ||
| Bangladesh | 163 | 0.77 million | 11, 934 | 361 | 69 | 79 990 | BRAC | Covers 297 sub-districts from 42 districts in Bangladesh (out of 64 total country districts) | 75% drop in notifications during initial lockdown |
| icddr,b | PPM implementation in Dhaka and Chittagong | Nearly 90% private clinics shutdown during initial lockdown | |||||||
| IRD | PPM implementation in Dhaka and Mymensingh Division | NA | |||||||
| India | 1,370 | 22.66 million | 246, 116 | 2,640 | 478 | 680 948 | CHAI | Partner with Project JEET working in 182 districts out of 718 total country districts in India | 8.63% drop in notification in 2020 compared to 2019. 93% drop in testing in April 2020 compared to January 2020 but 23X increase by end of 2020 (due to COVID-19 mitigation plan and outsourcing GeneXpert to private labs) |
| CHRI - PATH | Partner with Project JEET working in 195 districts out of 718 total country districts in India | 21% drop in notification from private sector. 23% drop in presumptive TB cases enrollment in Nikshay. 3% increase in sputum sample transported (due to COVID-19 mitigation plan and outsourcing GeneXpert to private labs) | |||||||
| FIND | Partner with Project JEET working in 101 districts out of 718 total country districts in India | 16% drop in notification from private sector | |||||||
| REACH | PPM Implementation in 5 districts in Tamil Nadu (out of 38 districts in Tamil Nadu) | 62% drop in notification from private sector and 73% drop in testing. | |||||||
| WHP | PPM Implementation in 8 districts in Bihar (out of 38 districts in Bihar) | 36% drop in notification and 20% drop in testing in Patna district | |||||||
| Indonesia | 271 | 1.71 million | 47, 012 | 845 | 283 | 107 640 | FHI 360 | PPM project initiated in 9 districts (out of 7024 districts in Indonesia) | NA |
| Myanmar | 54 | 142, 947 | 3, 210 | 174 | 39 | 18 432 | PSI | Addressed 14.3% of Myanmar’s national TB burden | 30% drop in notification and referrals from private networks |
| Nigeria | 201 | 165, 419 | 2, 065 | 440 | 323 | 17 250 | SHOPS Plus | PPM implementation in 16 states in Nigeria (out of 36 + 1 states) | 51% drop in notification in Lagos and 18% drop in notification in Kano in April 2020, compared to January 2020. But once services resumed after lockdown, total notification increased by 57% in 2020 compared to 2019 |
| IHVN | PPM implementation in 21 states in Nigeria (out of 36 + 1 states) | 60% drop in GeneX pert utilization in first quarter of 2020. But once services resumed after lockdown, notification from PPM partners more than doubled (131%) in 2020 overall | |||||||
| Pakistan | 217 | 858, 026 | 18, 915 | 570 | 242 | 94 819 | Mercy Corps | PPM implementation expanding to 111 districts in 2021 (out of 136 total) | 39% drop in notification in initial months of lockdown in MC program districts. |
| Greenstar | PPM implementation in 20 districts | 5 – 6% drop in case detection during initial lockdown. Shutdown of nearly 50% of private practice | |||||||
| IRD | Technical partner to Indus Health and Hospital Network in TB implementation | NA | |||||||
| Philippines | 108 | 1.10 million | 18, 472 | 599 | 190 | 131 096 | FHI360 - Philippines | PPM implementation in the top 4 (out of 17) highest TB burden regions. | 20 – 25% decline in all TB care services. Nearly 60–80% private clinics shutdown during the initial lockdown |
| IRD | Implementation partners for nationwide Private Sector Diagnostics Consortium for TB | NA | |||||||
Source: a. These values were reported during the qualitative interview by the respective intermediary agencies. These are approximate values, based on their routine notification data for 2020 in their areas of operation. No further references were available at that point of time.
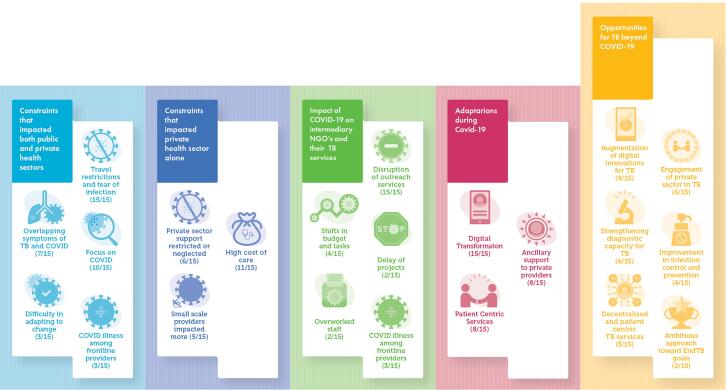
In response to the COVID-19 pandemic, the World Health Organization (WHO) has called on member states to adopt a whole-of-government and whole-of-society approach [10], and a wide variety of impacts and mitigation approaches have been seen for TB [11], [12]. While public–private partnerships can help support strained health systems, countries are unsure of how to optimally engage the private sector in their national response efforts to COVID-19 [13]. This applies to TB too. To inform this area, this rapid assessment is co-authored by fifteen representatives of intermediary agencies from the Big Seven countries – Bangladesh [3], India [5], Myanmar [1], Nigeria [2], Pakistan [2], Philippines [1] and Indonesia [1]. In the following sections, we summarize the impact of the COVID-19 pandemic on private sector providers of TB care, on TB patients, and on TB PPM intermediary agencies, plus the different adaptations to the pandemic, and opportunities seen to improve TB care (the findings are summarized in Fig. 1).
Fig. 1.
Constraints and adaptations in private health sector during COVID19 and the opportunities to reinforce private sector engagement and reimagine TB care. The numbers within parentheses denotes the number of respondents who agreed on the theme.
In this assessment, any reference to private providers refers to private health sector involved in service delivery including private hospitals, private laboratories and private pharmacies [14]. The authors acknowledge upfront that the data captured in this document reflects the experience between March 2020 to December 2020. Given the rapidly evolving nature of the pandemic and the roll out of vaccines starting towards the end of 2020, later experiences would necessitate a separate assessment.
2. Impact of COVID 19 on TB service delivery in the private healthcare sector
The private providers involved in TB service delivery faced several challenges during the pandemic in 2020 that impacted the entire cascade of TB care. In the initial months of the pandemic, when countries went into lockdowns and travel restrictions were imposed, there were disruptions in active case finding and contact tracing efforts, decreases in the demand for and use of TB diagnostics, drops in TB notifications and shutting of private practices (See Table 1). Although movement restrictions were slowly lifted in many regions by the end of 2020, at the time of the assessment the TB notification were nowhere near the same as in 2019 nor in line with the country targets. “We are getting around 70% of the TB notifications we saw in January/February 2020, but overall, we are at only 30–40% of our Global Fund target” (PATH, India).
The several constraints that impacted TB service delivery are summarized in Table 2. Some of these constraints were common for both the public and private health sectors, but private providers faced added challenges, as seen in Table 2.
Table 2.
Constraints in TB service delivery for private providers and the number of respondents identifying the constraint.
| Constraint | Examples | Descriptions from key informants |
|---|---|---|
| ||
| Travel restrictions and fear of infection (15/15) | • In Bangladesh, some providers with icddr,b, stopped chest X-rays because staff were not allowed to leave their neighbourhood • In Nigeria, drug stock-outs were reported due to the impact of movement restriction on supply logistics. |
“The patient could not come to the health facility and the community health care worker could not go to the patient.” (IHVN, Nigeria). “People are so worried about going to hospitals and catching the infection that the whole agenda of early diagnosis and seeking care has been very badly affected”. (FHI 360, Indonesia). |
| Focus on COVID (10/15) | • Some private hospitals in the Philippines were instructed to earmark between 20 and 60% of their beds and services for Covid-19 patients • IRD supported General Physicians in Karachi, Pakistan including Sehatmand Zindagi (Healthy Life) Centers to become COVID-19 care centers. • Drops in TB testing as Gene Xpert machines and lab technicians were repurposed for COVID-19 diagnostics reported in all the Big Seven countries. |
“When COVID-19 came, we suddenly realized that the demand for TB wasn’t there. Even the providers we were engaging with, they started asking questions about COVID-19not TB.” (CHAI India) “We experienced a massive drop in the capacity to test for TB… The number of days available to do TB tests reduced drastically, and so did the healthcare workers who performed the test for TB … their focus shifted away from TB testing” (IHVN, Nigeria). |
| Overlapping symptoms of TB and COVID (7/15) | • Patients reluctant to admit chest symptoms for fear of COVID-19 stigma • Providers refused to see chest symptomatics for fear of contracting COVID • Lab technicians refused to collect sputum samples for fear of COVID exposure |
“Even though the patients had cough they were reluctant to visit a clinic because of stigma associated with both TB and COVID-19.” (Mercy Corps, Pakistan) |
| COVID illness among frontline providers (3/15) | • 15 private physicians with PSI in Myanmar tested positive for COVID-19 and 1 physician died of COVID-19. | “In some instances, lab personnel who tested COVID-19 samples ended up contracting the disease. This resulted in shutting down of the entire lab and as a consequence, TB testing was restricted too.” (PSI, Myanmar). |
| Difficulty in adapting to change (3/15) | • Resistance among providers to use face mask • Teleconsultations were an added pressure especially for senior clinicians. |
“Government partners had little or no experience with virtual working.” (FHI 360, Philippines) |
| ||
| Private sector support restricted or neglected by public sector (6/15) | • In Nigeria, the Gene Xpert cartridges and microscopy reagents were procured by national program mainly for the public sector. • In Bangladesh, the government announced some incentives only for healthcare workers in the public sector. |
“Since the providers were not part of any government source, they were not provided with any training regarding how to manage the pandemic nor provided any PPE.” (Greenstar, Pakistan) “There was no clear guideline on what private providers need to do when they encountered a positive COVID-19 patient or where they need to send for testing.” (PSI, Myanmar). |
| Some private providers (particularly small scale) forced to close (5/15) | • Smaller or rural practices including private pharmacists were unable to meet the infection control measures needed to stay open during the lock-down • The cash crunch faced by private hospitals was widespread across other health areas too [15]. |
“The most affected were the private sector in the community – the private vendors, the community pharmacies – with small to medium scale enterprises. Some have lost their capital and had to completely shut down” (IHVN, Nigeria). |
Though these constraints impacted screening for patients with TB symptoms, the intermediaries also noted more walk ins in some private clinics as patients presented directly to health facilities once their symptoms worsened, and many of these patients were diagnosed with having TB. “Only the very sick patients admitted to having cough and gave sputum to be tested for TB and a high proportion of them tested positive for TB.” (SHOPS Plus, Nigeria). However, during the period of lockdown, in most countries this rise in patients confirmed with TB was not high enough to match the reduced total patient flow, resulting in an overall drop in notifications. In addition, the intermediaries observed that many private providers had additional costs – and that those costs were passed on to patients seeking care (see next section).
3. Unanticipated expenses for private providers resulted in increased prices charged to patients
During the pandemic, TB treatment and diagnostics in the public sector and by government or donor-funded PPM providers continued to be free of charge or highly subsidized in all of these high burden countries. “A significant (amount of) funding is from the Global Fund to provide free TB care in the private sector [Under PPM scheme].” (PSI, Myanmar)
Despite the free TB services, patients incurred high costs for general health visits due to six main reasons.
-
3.1.
A major cost for patients went into covering the expenses for personal protective equipment (PPE) and other infection prevention measures. “Whatever services were available became more costly because of personal protective equipment being charged to the patient.” (FHI 360, Indonesia).
-
3.2.
Some private practitioners also insisted that patients take additional tests and/or a receive a negative COVID-19 test result before they could be seen for other ailments, raising the cost for TB testing. In the Philippines, private providers were required to perform a COVID-19 test for every patient who required more than 30 min of interaction with the provider.
-
3.3.
Even when patients had insurance coverage they still had to pay out of pocket in some instances, as their insurance schemes did not cover either COVID-19 expenses or COVID-19 specific health facilities. “Patients holding HMO (Health Maintenance Organization) cards also had to pay out of pocket.” (FHI 360, Philippines)
-
3.4.
Though there was a fall in the number of patients presenting at private clinics, the cost to run the clinic (rent, electricity, etc.) either remained the same or was increased due to the additional costs incurred to ensure infection prevention “The clinics that used to see 20 patients an hour can now see only about 4 patients an hour, so they charge more per patient” (FHI 360, Philippines).
-
3.5.
Additionally, to meet the shortage of supplies, in-person consultations were charged more than virtual consultations.
-
3.6.
Patients also incurred indirect costs due to travelling long distance and purchasing products such as soap, hand sanitizer, and masks.
4. Impact of Covid-19 on intermediary ngos and their TB services
The most common impact of COVID-19 for the intermediary organizations was the disruption of field work and outreach activities. “Reinforcing relationships between field office staff and providers has been critically affected because of movement restrictions and lack of in-person contact.” (PATH, India). The travel restrictions made it difficult for the field staff to continue active case finding, treatment monitoring, and medical camps and to monitor the progress in their projects. The field staff were also stigmatized as their neighbours and landlords were afraid of contracting COVID-19 and restricted them from going out of (or returning to) their homes.
The intermediaries had to shift their budgets and tasks to accommodate the needs of the changed situation. Overall, budgets and plans for face-to-face follow-up, training, monitoring, meetings and outreach programs decreased in the periods of lockdown. By contrast, there was an increased focus on online meetings and communication, as well as increased responsibilities for field staff. Post-lockdown, the regular programs resumed and were trying to catch up. Increased costs and attention were given to purchasing of PPE for private providers, training additional staff to screen patients for TB and COVID-19 and additional allowances for transport and communication for field staff. These additional tasks in turn burdened the staff who felt overworked and had to work extra hours to follow up with patients and partners. “Sometimes, I am in calls all day” exclaimed one of the stakeholders. Many field staff and laboratory staff from these intermediary agencies were also challenged by COVID-19-related morbidity and mortality, further straining the staffing. “Out of 150 field staff, 15–18 had COVID-19, but all recovered” (Greenstar, Pakistan). All these restrictions delayed several initiatives that were planned for the year 2020 by the intermediaries. “We had wanted to expand to new geographies, but recruitment and trainings were severely delayed” (CHAI, India).
In the face of these challenges, many stakeholders from the intermediary agencies were consistently appreciative of the Global Fund and other donors, mainly for non-delayed funding accompanied by flexibility within the grant to meet the additional costs such as procuring PPE. The proactive measures taken by the Global Fund and other donors to support the mitigation plans helped the intermediaries to advance funding to the service providers. In the Philippines, despite the budget cuts for the National TB Program, private hospitals were able to access Xpert cartridges because of the continued support from the Global Fund. “Funders have shown a high degree of resilience, support, and empathy to us, and they allowed adaptations to operations and timeline which was greatly appreciated” (PATH, India).
5. Innovative adaptations in TB care that emerged during Covid19
In spite of the constraints that accompanied the COVID-19 pandemic, the private providers and intermediary agencies found ways to adapt to the new reality. The adaptations outlined below on the digital transformation and increase in patient-centric services were also noted in the public sector. More specifically related to private provider engagement, intermediaries provided various ancillary supports for private providers under their PPM programs.
5.1. Digital transformation
Digital tools have offered massive opportunities to connect with others from home, including doctor-patient relations, work meetings, trainings, and data-collection processes. A variety of these tools were mentioned by the respondents and are summarized in Table 3.
Table 3.
Digital transformation during COVID-19 and the commonly used platforms.
| Digital adaptation | Examples | Descriptions from key informants |
|---|---|---|
| Teleconsultations and Telemedicine | • Telemedicine platforms e.g. WHP and Govt. of Bihar (India) partnered to initiate a new telemedicine platform in the state • Telephone consultation • Whatsapp video calls |
“Telemedicine companies have mushroomed around this pandemic.” (icddr,b, Bangladesh) |
| Modified observation of therapy | • Regular phone calls • SMS reminders • Refill reminders through call centers e.g. CHAI’s partnership with Indian e-pharma, 1 mg • Digital Adherence tools e.g. 99 DOTS, Video DOT |
“We ensured to track the medicine refill dates of the patients so that we could communicate with them over the phone or using WhatsApp.” (CHAI, India). |
| Remote monitoring and evaluation | • Facebook messenger • Viber • Google forms • Phone calls • Whatsapp video calls • Zoom video calls |
“Before the pandemic, routine data on TB notification and TB treatment were collected in person and reviewed every quarter. This was replaced with online forms, telephone calls and messaging facilities like whatsapp and sms.” (Mercy Corps, Pakistan) |
| Remote training and coordination | • Zoom webinars • TeleECHO |
“During the pandemic we (SHOPS Plus) used the TeleECHO platform to spread awareness on TB and COVID-19, how to differentiate between these two and how to triage.” (SHOPS Plus, Nigeria) |
| Digital tools in Diagnostics | • AI based Chest X ray • Digital X rays • Online reports |
“BRAC’s online X ray reading system that was introduced in 2018 was scaled up during COVID-19” (BRAC, Bangladesh) |
| Updated systems | • Integration of whatsapp calling in Nikshay [16] • Mobile notification app in Philippines • Web based procurement of diagnostic supplies through the Philippines Private Sector Diagnostics Consortium • Scale up of TB Screening and Tracking for Accelerated Referral and Reporting (TB STARR) app in Kanos |
“Many community health workers have become empowered to use technology well, including TB survivors who are being trained to be TB champions.” (REACH, India) |
5.2. Patient centric services
Many existing systems and practices were modified to better suit the patients’ needs. “They (Field Staff) changed their model of TB management and prevention” (BRAC, Bangladesh). Programs and providers have been pushed out of their comfort zone to implement the vision of patient-centered TB care as outlined in Table 4.
Table 4.
Patient centric services.
| Patient services | Examples | Descriptions from key informants |
|---|---|---|
| Emphasis on infection prevention providing safer environment for staff and patients | • Smaller medical camps • Infrastructure updates such as better ventilation, distant seating arrangement and frequent sanitization. • Installation of infection prevention shields in consultation rooms • Rotation of staff schedule • Limit counselling and handover brochures instead |
“Instead of larger medical camps with 60 to 70 patients at a time, smaller medical camps with 5 to 10 patients at a time were organized.” (Mercy Corps, Pakistan) |
| Relaxation of DOT guidelines | • Prescription of drugs for a longer duration at one time • Skipped sputum microscopy and conducted Gene Xpert for rapid results |
“Everyone was more comfortable with giving 1–2 months of medicine refills to patients, instead of daily DOTS” (WHP, India). |
| Combined screening for TB and COVID | • Integration of COVID -19 screening along with TB screening systems. e.g. TBSTARR app by SHOPS Plus • Bi-directional screening for TB and COVID-19 in India, Bangladesh, and Indonesia • Mobile X-ray vans to screen for TB and COVID-19 e.g. Indus Hospital and Health Network and IRD Pakistan |
“We pivoted our electronic data systems [in Pakistan] very quickly to capture Covid-19 screening data in addition to TB screening” (IRD Global). |
| TB care at doorstep | • Delivery of medications to client’s residence • Sputum collection at client’s residence |
“As soon as the lockdown was declared, we had to ensure that the patients were adequately stocked with treatments.” (CHAI, India) |
5.3. Ancillary support to private providers
Many intermediaries have taken this opportunity to further systematize the engagement of private providers and find new support mechanisms. The initial response of many intermediary agencies was to conduct a rapid survey to assess the ground reality and identify needs of the private providers. “We conducted a rapid assessment to understand what challenges the private providers faced and how they can be best supported to provide TB services without any interruption.” (Mercy Corps, Pakistan). Based on these assessments, the intermediaries were able to support their private providers as outlined in Table 5.
Table 5.
Ancillary support to private providers.
| Ancillary support | Examples | Descriptions from key informants |
|---|---|---|
| Supply of PPE, drugs, diagnostics and other health equipment | • Procurement of face masks, hand sanitizers and PPE kits for providers and patients. • Distribution of GeneXpert cartridges, oxygen cylinders, pulse oximeters, etc. • Arranged ‘movement pass’ for transport for vendors and others involved in transport logistics |
“One of the first things we did was ensure uninterrupted drug supply, as we cater to about 75% of the private sector patients in the city of Chennai.” (REACH, India) “With the movement pass, they would not be stopped on the way to move the samples to the diagnostic labs, the reference labs or the GeneXpert sites” (IHVN, Nigeria) |
| New guidelines to continue TB services | • Guidelines and information notes from WHO to continue TB services. • Updated guidelines from National TB programs • Infection prevention guidelines from intermediaries |
“We (Mercy Corps) provided infection prevention guidelines so that the private providers can follow them and take necessary precaution for the well being of both the patient and the provider.” (Mercy Corps, Pakistan) |
| Create public awareness about the situation | • Updated communication strategies • Created education materials • Organized awareness campaigns |
“We worked with a media company to build social media campaigns around destigmatizing TB and COVID-19 together” (FHI 360, Philippines) |
Some of the initiatives under all three adaptations existed before the pandemic. Though there are no quantifiable data, the intermediaries observed a mixed response to all these adaptations. While there was either an accelerated uptake or immediate scale-up of some of these initiatives, a few initiatives were limited to certain regions within the country with limited implementation and outcome. “A policy [for bidirectional screening] was there [in India], but [looking at the latest reports on TB notification] we do not know how it has transpired” (CHAI, India). “In a few cases it [bidirectional screening] happened, but routinely it was a real a challenge…if we consider the scale to offer similar screening for everybody, the country is not yet ready.” (BRAC, Bangladesh)
6. Opportunities for TB care beyond Covid-19
The assessment has shown that the impact of COVID-19 has created many constraints to TB care programs and challenges for people affected by TB. However, the intermediaries also identified several opportunities that can pave the way for improving TB care; these are outlined in Box 1. The prioritization and scale of these of these efforts will depend on national context and plans.
Box 1. Opportunities for TB care beyond COVID-19.
- Augmentation of the digital innovations for TB
-
•“Digital advancements like utilization of internet tools to conduct virtual trainings and payment through mobile transfers are some opportunities that can be harnessed for the future” (PSI, Myanmar)
-
•“The government’s appetite and acceptance for all kinds of technology is now higher than ever before. So, we’re hoping they will invest more in digital tools.” (FHI 360, Philippines)
-
•
- Partnership between government and private sector in TB
-
•“The true spirit of public and private mix was seen especially during the COVID19 pandemic” (Mercy Corps, Pakistan)
-
•“The potential of the private health sector must be mobilized to provide TB services to patients in the community” (Greenstar, Pakistan)
-
•“The informal private sector could also be enhanced and leveraged as an alternative for patients when they cannot access the formal private sector.” (SHOPS Plus, Nigeria)
-
•
- Strengthening diagnostic capacity for TB
-
•“The availability of these multiplex platforms like Truenat and CBNAAT will further help strengthen the TB services” (FIND, India)
-
•“For the COVID pandemic we're seeing that results can be ready much faster. We need to have a point of care test for TB that generates results during the visit.” (IHVN, Nigeria)
-
•
- Improvement in infection-control and prevention
-
•“I think the good thing which has happened after COVID is that providers keep their premises very clean and ensure that patients wear a mask or cover their mouth and nose with a piece of cloth.” (CHAI, India)
-
•“Private providers need to be strengthened on infection prevention and emergency preparedness for any such sudden demands in the health system.” (Mercy Corps, Pakistan)
-
•
- Decentralized and patient centric TB services
-
•“[We need to] go towards patients and the community with mobile x-ray and to ensure that testing is done” (Greenstar, Pakistan)
-
•“TB patients’ care and follow up should become easier and patient-centric” (IRD, Global)
-
•
- Ambitious approach towards EndTB goals
-
•“Contact screening for COVID has brought into focus that it is possible… I don’t think there will be any more excuses saying contact screening for TB cannot be done, be it public sector or private sector.” (REACH, India).
-
•“We were doing nearly ∼80,000 COVID tests per day in Delhi alone with about half of them being RT-PCRs. If we are able to do this, why can’t we do it for TB as well?” (FIND, India)
-
•
7. Conclusion
This rapid assessment of the TB intermediary agencies in seven high TB burden countries gives a good indication of the wide variety of disruptions that COVID-19 has caused in the overall health system and particularly to private TB healthcare services during 2020. Similar impacts on TB [12], [17], [18] and PPM [19] have also been reported in countries other than the Big Seven, even as performance on some quality of care indicators has been successfully maintained [20].
The work of the private health sector and the intermediaries was disrupted and caused changes in work processes and increased stress on staff. Despite the challenges, they have shown resilience and flexibility to adapt to continue to support TB services. In some instances, the contributions from the private sector increased drastically at the end of 2020, once services resumed.
However, as the pandemic is still evolving and some of these countries are in the next wave of the COVID-19 pandemic, the constraints seem to continue, and the identified adaptations have not yet been scaled up and the opportunities have not yet been fully leveraged.
The progress in the fight against TB that has been lost during the COVID-19 pandemic cannot be recovered overnight and will require arduous efforts from all stakeholders. PPM is essential in rebuilding the healthcare services system to end TB. The call to take engagement of private providers to scale is not something new. The PPM Roadmap for Tuberculosis that was released in 2018 captured ten key actions that are required to scale up private sector engagement [21]. The COVID-19 pandemic has only accelerated the need to prioritize those ten action items. Partnerships with private sector and intermediary agencies are crucial to build more resilient systems that can be leveraged in times of crisis and must be included in all measures recommended for countries to ensure continuity of TB services [22]. TB programs should also take advantage of the changes brought about by COVID-19 to reimagine patient-centered TB care.
Ethical statement
This was a rapid assessment conducted as key informant interviews.
CRediT authorship contribution statement
Conceptualization by MP, HMYD, WAW, GS, PH and JK. Formal analysis and visualization by JK and PH. Data curation, investigation, methodology and project administration by JK, PH, CO and MK. JK and PH wrote the original manuscript with input from AR, BO, HWH, HH, IS, KF, LM, ML, NJ, RA, RM, SC, SB, SM, SV, SA, TA, CO, MK, US, WAW, GS, HMYD and MP.
Declaration of Competing Interest
WAW is employed by the United States Agency for International Development (USAID), Washington DC, USA. The views and opinions expressed in this article are those of the authors and do not necessarily reflect the view of the U.S. Agency for International Development or the U.S. Government.The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Max Roser, Hannah Ritchie, Esteban Ortiz-Ospina and Joe Hasell. Coronavirus Pandemic (COVID-19). Published online at OurWorldInData.org. 2020. Retrieved from: 'https://ourworldindata.org/coronavirus' accessed on 10 May 2021.
- 2.The Impact of COVID-19 on the TB Epidemic: A Community Perspective. 2020. Available at http://www.stoptb.org/assets/documents/resources/publications/acsm/Civil%20Society%20Report%20on%20TB%20and%20COVID.pdf accessed on 14 April 2021.
- 3.World Health Organization. Impact of the COVID-19 pandemic on TB detection and mortality in 2020. 22 March 2021.
- 4.Stop TB Partnership. One year on. New data show global impact of COVID-19 on TB epidemic is worse than expected. Stop TB Partnership Media Brief. 18 March 2021.
- 5.World Health Organization. Global Tuberculosis Report 2020. 2020.
- 6.Montagu, D and Chakraborty, N. Private Sector Utilization: Insights from Standard Survey Data. Geneva: World Health Organization.2019.
- 7.World Health Organization. Engaging private health care providers in TB care and prevention: a landscape analysis – 2020 update. In press.
- 8.World Health Organization. Multisectoral accountability framework to accelerate progress to End Tuberculosis by 2030. 23 May 2020.
- 9.United States Agency for International Development. Public Private Mix (PPM) Models for the Sustainability of Successful TB Control Initiatives. 2014.
- 10.World Health Organization. The best time to prevent the next pandemic is now: countries join voices for better emergency preparedness. 2020.
- 11.U.S. Agency for International Development. 2021. The intersection of TB and COVID-19. Available at https://docs.google.com/presentation/d/1oR8P7QwGtcI4Cg8wuvVCnfH3MxV7 kmZHrYFUANlSaA8 . Accessed May 5 2021.
- 12.Migliori G.B. Worldwide Effects of Coronavirus Disease Pandemic on Tuberculosis Services, January-April 2020. Emerg Infect Dis. 2020;26(11):2709–2712. doi: 10.3201/eid2611.203163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O’Hanlon B., Hellowell M. Six Current Policy Challenges. Geneva. 2020. Enabling the private health sector in the national response to COVID-19. [Google Scholar]
- 14.Klinton JS. The Private Health Sector: An Operational Definition. World Health Organization. Geneva. 2020. https://www.who.int/publications/i/item/the-private-health-sector-an-operational-definition accessed on 14 April 2021.
- 15.Yamunan S. Fear of Covid-19 spread makes private hospitals turn away patients – or charge them higher bills. Scroll.in. 23 April 2020. Available at https://scroll.in/article/959727/fear-of-covid-19-spread-makes-private-hospitals-turn-away-patients-or-charge-them-higher-bills Accessed on 06 May 2021.
- 16.Nikshay knowledge base. What’s new. Available at. https://nikshay.zendesk.com/hc/en-us/articles/360016723931-What-s-New accessed on 24 February 2021.
- 17.McQuaid CF, Vassall A, Cohen T, Fiekert K, White RG. The impact of COVID-19 on TB: a review of the data. Int J Tuberc Lung Dis. 2021 Jun 1. [DOI] [PMC free article] [PubMed]
- 18.Teo A.K.J., Ong C.W.M., Hsu L.Y. COVID-19 and TB: a progression-regression conundrum. Int J Tuberc Lung Dis. 2021;25(6):421–423. doi: 10.5588/ijtld.21.0219. [DOI] [PubMed] [Google Scholar]
- 19.Min J., Kang J.Y., Kim J., Yang J., Kwon Y., Shim E. Impact of COVID-19 on TB services in Korea. Int J Tuberc Lung Dis. 2021;25(5):400–402. doi: 10.5588/ijtld.20.0942. [DOI] [PubMed] [Google Scholar]
- 20.Min J., Kim H.W., Koo H.-K., Ko Y., Oh J.Y., Kim J. Impact of COVID-19 Pandemic on the National PPM Tuberculosis Control Project in Korea: the Korean PPM Monitoring Database between July 2019 and June 2020. J Korean Med Sci. 2020;35(43) doi: 10.3346/jkms.2020.35.e388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Public–private mix for TB prevention and care: a roadmap. Geneva: World Health Organization; 2018.
- 22.World Health Organization. Tuberculosis and COVID - WHO Information Note. World Health Organization; 2020.