Abstract
Aim
The COVID‐19 pandemic prompted the rapid development of remote medical services. During lockdown periods, children's growth data were obtained from parents’ home assessments. This study aimed to assess the accuracy of home height and weight measurements and analyse their utility in clinical decision‐making.
Methods
A retrospective, single‐centre observational study. Children aged 3–18 years were measured for weight and height at home using guidance provided to parents on proper measurements techniques before subsequent professional re‐evaluation at our endocrine institution clinic. The two sets of measurements were compared and analysed according to various clinical parameters.
Results
Height measurements at home and in the clinic were comparable (diff = 0.1 ± 1.3cm, p = 0.42) amongst the 107 children (mean age 10.2 ± 3.7, 56.1% males) participating in the study, except in overweight and obese children where they were significantly higher in the clinic (diff = 0.86 ± 1.48cm, p = 0.018). Weight and BMI were significantly higher in the clinic (diff = 0.45 ± 0.8kg and diff = 0.3 ± 0.6kg/m2, p<0.001 and p<0.001, respectively).
Conclusions
Height measurements of children by their parents were accurate except in obese and overweight children, whereas weight measurements tended to be lower than in the clinic. With proper guidance, parents’ home measurements of height and weight are accurate and suitable for clinical decision‐making.
Keywords: COVID‐19, growth assessment, home measurements, parents reported measurements
Abbreviations
- BMI
Body mass index
- CDC
Centers for Disease Control and Prevention
- GH
Growth hormone
- IQR
Interquartile range
- LOA
limits of agreement
- SCMCI
Schneider Children's Medical Center of Israel
- SD
Standard deviation
Key Notes.
The study evaluates the accuracy of parents‐reported height and weight measurements of their children during COVID‐19 lockdowns following guidance on proper measures techniques.
Height measurements of children by their parents were accurate except in obese and overweight children, weight measurements tended to be lower than in the clinic.
With proper guidance, parents’ home measurements of height and weight are accurate and suitable for clinical decision‐making.
1. INTRODUCTION
The COVID‐19 pandemic changed the face of medicine worldwide in every medical field and aspect, resulting in the rapid development of many remote medical services. 1 During lockdown times, growth assessment (ie, measurement of height and weight of children with various medical conditions) relied solely on parents’ reported measurements. The accuracy of these measurements is fundamental for proper clinical decision‐making in all fields of paediatrics, especially in treating conditions such as failure to thrive, short stature, childhood obesity and children treated with growth hormone (GH). Previous studies analysing the validity of parent‐reported weights and heights in children have reached conflicting conclusions. Some studies have shown low accuracy, whilst others published encouraging results claiming these measurements were sufficient for accurate BMI categorisation. 2 , 3 , 4 , 5 , 6 In some studies, parents were instructed how to correctly measure their children's weight and height at home, and in others, not. 6 , 7
At the beginning of the COVID‐19 pandemic, we provided all the parents of children treated in our endocrine clinic with written and illustrated instructions and directed them to a video available on our medical centre website, describing the accurate way to measure their child's height and weight. 8 We used the reported measurements for clinical decision‐making during our remote visits. At times of ease of the pandemic in Israel, we reintroduced some in‐hospital services. To service our patients safely and efficiently, we asked parents to continue measuring height and weight at home and to report the results at their subsequent clinic visit. The patients were then re‐measured in our clinic, allowing us to compare the reported measurements to objective measurements done by medical personnel.
The study's objectives were to assess parents‐reported child height and weight accuracy compared to in‐clinic measurements.
2. PATIENTS AND METHODS
A retrospective study analysing the accuracy of home measurements of height and weight in children attending the endocrine clinic at Schneider Children's Medical Center of Israel (SCMCI) for various endocrine conditions. The Ethics Committee of our institution approved the study according to the World Medical Association's Declaration of Helsinki.
2.1. Patients
The study included healthy children aged 3–18 years, measured for weight and height at home the day before visiting the endocrine clinic, and re‐measured in the clinic by experienced medical personnel. Excluded were children whose height was not measured at home, children with skeletal deformities, those who could not stand by themselves, and those where technical difficulties prevented proper measurements in the clinic. Data collected on each patient included gender, age, height and weight at home and in the clinic. To compare the accuracy of home measurements in subgroups of the cohort, the participants were subdivided according to the following clinical parameters: (1) overweight and obese children as compared to normal‐weight children [overweight defined according to the Centers for Disease Control and Prevention (CDC) as BMI at or above the 85th and below the 95th percentile, and obesity as BMI above the 95th percentile] 9 ; (2) short‐statured children as compared to children with normal height (short stature defined as more than two standard deviations below the mean height for their age according to the CDC growth charts) 10 ; and growth hormone‐treated as compared to non‐growth hormone‐treated children.
2.2. Height and weight measurements
Parents were guided on how to measure their children at home according to CDC guidelines. 8 Instructions were given orally by phone and sent via email, including a Figure S1 as shown in the supplementary material and a link to a short tutorial video on the SCMCI website. These instructions emphasised proper clothing and body position of the measured child, as well as the correct measurement technique to be used. In‐clinic heights were measured with a Harpenden stadiometer (Holtain Ltd., Crosswell, United Kingdom) and weight with a calibrated scale. Body mass index (BMI) was calculated as weight (kg)/height2 (m2).
2.3. Statistical analysis
Continuous normally distributed data are expressed as mean (±SD), non‐normally distributed continuous data as median [interquartile range (IQR) and range], and categorical data as number and percentage. The differences between clinic and home measurements were calculated (diff = clinic measurement — home measurement). A one‐sample t test was used to evaluate the null hypothesis that the mean of the difference equals zero. Linear multivariate regression analysis was used to assess the effects of age and gender on the differences between clinic and home measurements.
Bland‐Altman plots were used to display the degree of agreement between measured and parents‐reported weight, height and BMI. In short, Bland‐Altman plots are used to evaluate the agreement among two different instruments or two measurement techniques, allowing identifying any systematic difference between the measurements (ie, proportional bias) or possible outliers. The mean difference is the estimated bias, where the SD of the different measurements is the random fluctuation around this mean. If the mean value of the difference differs significantly from 0, the presence of a fixed bias is indicated. It is common to compute 95% limits of agreement (LOA) for each comparison (average difference ± 1.96 standard deviations of the difference). If the differences between means ± 1.96 SD are not clinically significant, the two methods may be used interchangeably. The difference between the methods is regressed based on the average of the two methods, searching for a proportional bias. 11
3. RESULTS
Table 1 describes the study cohort of 107 children who participated in the study. The mean height difference between home and clinic measurements was not statistically significant (diff = 0.1 ± 1.3 cm, p = 0.42), and no proportional bias was found. In a multivariate analysis, age and gender did not affect differences in height measurements. Figure 1 shows the Bland‐Altman plot of agreement between the height measurements. Weight and BMI were significantly higher when measured in the clinic compared to parents‐ reported measurements [diff = 0.45 ± 0.8 kg (p < 0.001), and diff = 0.3 ± 0.6 kg/m2 (p < 0.001), respectively]. No proportional bias was found for both weight and BMI analyses. The difference between clinic and home weight measurements was not affected by gender but had an inverse correlation with the child's age, with reported weights tending to be lower than those measured in the clinic (r = 0.25, p = 0.045). BMI differences were not significantly affected by age or gender. Figure 2 shows the Bland‐Altman plot of agreement between the weight and BMI measurements at home and in the clinic. Table 2 depicts a subgroup analysis. Heights measured at home in overweight and obese children were significantly lower than in the clinic (diff = 0.86 ± 1.48cm, p = 0.018). This group is significantly different from normal‐weight children, in which such a difference was not observed (between‐group difference, p = 0.003). No other subgroup differences in weight or height measurements were found (Table 2).
TABLE 1.
Descriptive statistics of the study cohort
| Participants (n = 107) | Mean ± SD a |
|---|---|
| Age (years) | 10.2 ± 3.7 |
| Gender—Male (%) | 60 (56.1%) |
| Height at home (cm) | 132.4 ± 21.0 |
| Height at the clinic (cm) | 132.3 ± 20.9 |
| Weight at home (kg) | 34.6 ± 15.1 |
| Weight at the clinic (kg) | 35.0 ± 15.3 |
| BMI at home (kg/m2) | 18.2 ± 4.0 |
| BMI at the clinic (kg/m2) | 18.5 ± 4.0 |
Data presented as Mean ± SD unless otherwise specified.
FIGURE 1.
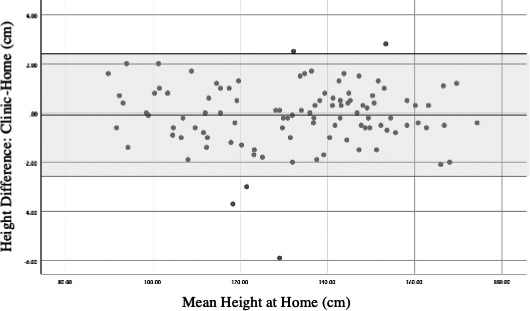
Bland‐Altman plot comparing height at home and in the clinic
FIGURE 2.
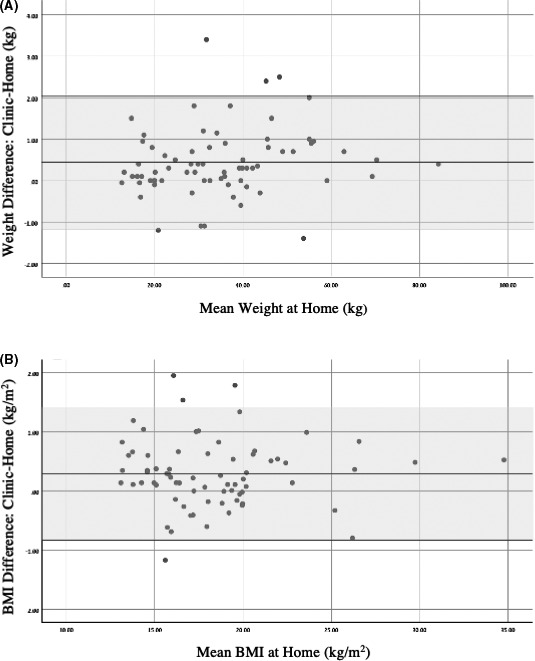
Bland‐Altman plots comparing (A) weight and (B) BMI at home and in the clinic
TABLE 2.
Height and weight differences stratified according to the height, weight, and GH treatment status of the children
| Number (%) | Diff. Height ± SD | p value | Diff. Weight ± SD | p value | |
|---|---|---|---|---|---|
| Short Stature | 56 (52.3) | −0.15 ± 1.22 | 0.662 | 0.40 ± 0.84 | 0.748 |
| Normal Stature | 51 (47.7) | −0.04 ± 1.34 | 0.47 ± 0.81 | ||
| GH Treatment | 26 (24.3) | −0.19 ± 1.15 | 0.686 | 0.64 ± 0.92 | 0.236 |
| Non—GH Treatment | 81 (75.7) | −0.10 ± 1.31 | 0.37 ± 0.78 | ||
| Normal Weight | 87 (81.3) | 0.10 ± 1.16 | 0.003 | 0.44 ± 0.85 | 0.907 |
| Overweight/Obese | 20 (18.7) | −0.86 ± 1.48 | 0.41 ± 0.68 |
Bold value indicates statistically significant.
4. DISCUSSION
The study aimed to assess the reliability of parents‐reported measurements of height and weight of children during the COVID‐19 pandemic. Measurements of height taken by the children's parents were comparable to those taken in the clinic, except in overweight or obese children in which weight and BMI measured at home were significantly lower than when taken in the clinic.
Remote growth assessment of children became of crucial significance in endocrine clinics during the COVID‐19 pandemic. Our findings suggest that height measurements taken by the children's parents were comparable to those done in the clinic. These results contradict most previous studies looking at the accuracy of parentally reported height measurements. 2 , 3 , 4 , 5 , 6 However, those studies relied on surveys of relatively large populations that replied to questioners, where in most cases, parents were not asked to measure their children. Moreover, in the few studies where parents were asked to measure their child's height, they were not instructed how to do it correctly. 6 , 7 Our study differs in that it constitutes a cohort of children who regularly attend an endocrine clinic mainly for growth assessment, and some of whom are treated with GH. Their parents have been exposed to growth measurements in the clinic, understand the importance of accurate measurements and were instructed how to take growth measurements at home. It is, therefore, possible that under these conditions, height measurements taken at home may be accurate and suitable for clinical decision‐making in an endocrine clinic setting. Interestingly, in overweight and obese children, parental height measurements were significantly lower compared to the clinic measurements. The reason for this difference is not clear. It has been suggested that excessive body weight increases the risk of developing lumbar hype‐lordosis and causes posterior axial tilt, which lowers the measured height. 12 Therefore, it is plausible that these children's overall body shape interfered with parental measurements more than in the clinic, where experienced personnel overcame these effects by employing appropriate measurement techniques.
In our study, as previously reported by others, parents tended to report a lower weight than the clinic's measured weight, with underreporting of weight increasing with age. 5 , 13 It is suggested that underreporting of weight, especially of older and heavier children, is because of parental misperceptions and social desirability. 4 , 13 , 14 , 15 In our study, children were weighed at home before visiting the clinic, thereby minimising the effects of perceptions and desirability. Therefore, the disparities in weight may be due to additional factors, such as the precision of household scales. Previous studies demonstrated that many scales used to measure body weight at home, clinic or fitness centres are imprecise. Furthermore, these studies suggested decreased precision of the scales as weight increased. 16 , 17 Another factor possibly explaining the difference between home and clinic weights may be the variability of weight during the day. 18 Bodyweight is a bit lower in the morning because less food and fluids are consumed overnight, and water is lost through sweat and breathing. 18 , 19 While children were weighed in our clinic between 8–12 am, at‐home measurements were done at various times, including early in the morning when weight was at its lowest during the day. Nevertheless, in the current study, the differences in weight and BMI between home and clinic measurements were relatively minor compared to previous studies. 5 , 7 , 20 These differences of less than 0.5 kg and 0.3 kg/m2 for weight and BMI, respectively, are, in our opinion, acceptable for clinical decision‐making.
Our study is limited by its relatively small cohort. However, it is unique insofar as the parents were instructed on how to measure their children correctly. The validity of our results is strengthened by the fact that all confirmatory measurements were done in a single endocrine clinic by experienced personnel. Nevertheless, more extensive studies are needed to confirm our findings.
In conclusion, height measurements of children by their parents were accurate except in obese and overweight children, whereas at‐home weight measurements tend to be lower than in the clinic. Our results suggest that with the proper guidance of parents, home measurements of height and weight may be sufficient for everyday clinical decision‐making. In this era, where remote medicine is ubiquitous, we believe that home measurements can be clinically used.
CONFLICT OF INTEREST
All authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Supporting information
Supplementary Material
ACKNOWLEDGEMENTS
We thank Mrs. Rotem Diamant for significantly contributing to the manuscript.
Tenenbaum A, Shefer‐Averbuch N, Lazar L, Yakobovitch‐Gavan M, Phillip M, Oron T. Growth assessment of children during the COVID‐19 pandemic—Can we rely on parental measurements? Acta Paediatr. 2021;110:3040–3045. 10.1111/apa.16034
Funding information
This research did not receive any specific grant from any funding agency in the public, commercial, or not‐for‐profit sector
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- 1. Hollander JE, Carr BG. Virtually Perfect? Telemedicine for Covid—19. N Engl J Med. 2020;382(18):1679‐1681. [DOI] [PubMed] [Google Scholar]
- 2. Huybrechts I, De Bacquer D, Van Trimpont I, De Backer G, De Henauw S. Validity of parentally reported weight and height for preschool‐aged children in Belgium and its impact on classification into body mass index categories. Pediatrics. 2006;118(5):2109‐2118. [DOI] [PubMed] [Google Scholar]
- 3. Scholtens S, Brunekreef B, Visscher TL, et al. Reported versus measured body weight and height of 4—year—old children and the prevalence of overweight. Eur J Public Health. 2007;17(4):369‐374. [DOI] [PubMed] [Google Scholar]
- 4. Akerman A, Williams ME, Meunier J. Perception versus reality an exploration of children's measured body mass in relation to caregivers estimates. J Health Psychol. 2007;12(6):871‐882. [DOI] [PubMed] [Google Scholar]
- 5. O'Connor DP, Gugenheim JJ. Comparison of measured and parents’ reported height and weight in children and adolescents. Obesity (Silver Spring). 2011;19(5):1040‐1046. [DOI] [PubMed] [Google Scholar]
- 6. Huybrechts I, Beirlaen C, De Vriendt T, et al. Validity of instruction leaflets for parents to measure their child's weight and height at home: results obtained from a randomised controlled trial. BMJ Open. 2014;4(2):e003768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chai LK, Collins CE, May C, Holder C, Burrows TL. Accuracy of Parent—Reported Child Height and Weight and Calculated Body Mass Index Compared with Objectively Measured Anthropometrics: Secondary Analysis of a Randomized Controlled Trial. J Med Internet Res. 2019;21(9):e12532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Measuring Children's Height and Weight Accurately at Home, Healthy Weight, Nutrition, and Physical Activity, Centers for Disease Control and Prevention (CDC), https://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/measuring_children.html/#Height. Accessed April 11, 2021.
- 9. Overweight & Obesity, CDC. https://www.cdc.gov/obesity/index.html. Accessed April 11, 2021.
- 10. CDC Growth Charts, national Center for Health Statistics, CDC, https://www.cdc.gov/growthcharts/cdc_charts.htm. Accessed April 11, 2021.
- 11. Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8(2):135‐160. [DOI] [PubMed] [Google Scholar]
- 12. Jankowicz‐Szymańska A, Bibro M, Wodka K, Smola E. Does excessive body weight change the shape of the spine in children? Child Obes. 2019;15(5):346‐352. [DOI] [PubMed] [Google Scholar]
- 13. Weden MM, Brownell PB, Rendall MS, Lau C, Fernandes M, Nazarov Z. Parent‐reported height and weight as sources of bias in survey estimates of childhood obesity. Am J Epidemiol. 2013;178(3):461‐473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Larson MR. Social desirability and self—reported weight and height. Int J Obes Relat Metab Disord. 2000;24(5):663‐665. [DOI] [PubMed] [Google Scholar]
- 15. Seghers J, Claessens AL. Bias in self—reported height and weight in preadolescents. J Pediatr. 2010;157(6):911‐916. [DOI] [PubMed] [Google Scholar]
- 16. Yorkin M, Spaccarotella K, Martin‐Biggers J, Quick V, Byrd‐Bredbenner C. Accuracy and consistency of weights provided by home bathroom scales. BMC Public Health. 2013;13(1):1194. 10.1186/1471-2458-13-1194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Stein RJ, Haddock CK, Poston WS, Catanese D, Spertus JA. Precision in weighing: a comparison of scales found in physician offices, fitness centers, and weight loss centers. Public Health Rep. 2005;120(3):266‐270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bhutani S, Kahn E, Tasali E, Schoeller DA. Composition of two—week change in body weight under unrestricted free‐living conditions. Physiol Rep. 2017;5(13):e13336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Weissenberg S. Insensible water loss during sleep: a theoretical exercise. Adv Physiol Educ. 2005;29(4):213‐215. [DOI] [PubMed] [Google Scholar]
- 20. Wright DR, Glanz K, Colburn T, Robson SM, Saelens BE. The accuracy of parent‐reported height and weight for 6–12—year—old US children. BMC Pediatr. 2018;18(1):52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


