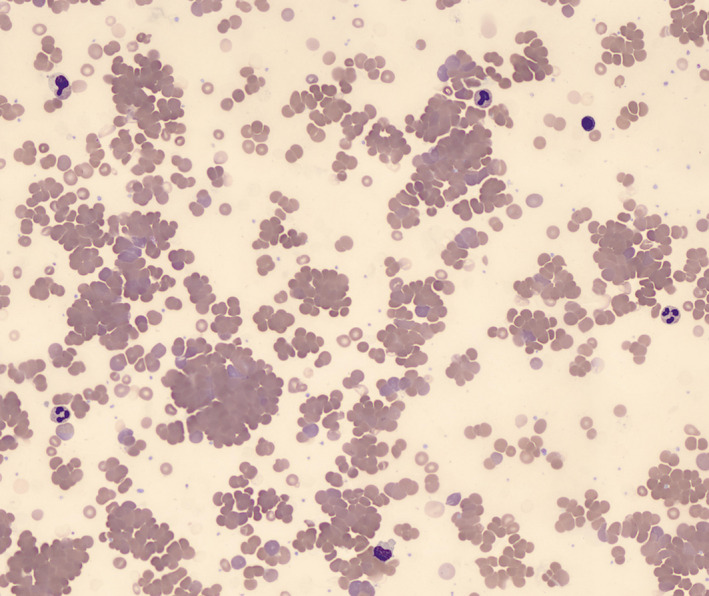
A 45‐year‐old female presented to the emergency department with a 1‐week history of shortness of breath, palpitations, fatigue and dark urine. The symptoms had developed 3 days after she received the first dose of COVID‐19 vaccine (Pfizer). There was no history of fever, cough, joint pain or recent medication use. Physical examination showed tachycardia, jaundice and pallor. Laboratory studies showed hemoglobin of 57 g/l, 10% reticulocytes, lactate dehydrogenase (LDH) 671 iu/l (normal range 125–220), total bilirubin 46.4 μmol/l (3–20) and direct bilirubin 12.5 μmol/l (0.5–8.6). A peripheral blood film showed marked agglutination (image). A direct antiglobulin test was positive for C3. Investigations for an underlying cause of cold agglutinin disease, including antinuclear antibody, cytomegalovirus, Epstein–Barr virus, human immunodeficiency virus, parvovirus, mycoplasma, flow cytometric immunophenotyping and protein electrophoresis, were all negative. Computed tomography of neck, chest and abdomen was normal.
The patient was treated with supportive blood transfusion and weekly rituximab for four cycles. She achieved complete remission 8 weeks after rituximab therapy.
Aggravation of cold agglutinin disease by vaccination for SARS‐CoV‐2 has been reported. Our patient indicates that de novo disease may also be precipitated.