Abstract
The SARS‐CoV‐2 is a new coronavirus responsible for the COVID‐19 disease and has caused the pandemic worldwide. A large number of cases have overwhelmed the healthcare system worldwide. The COVID‐19 infection has been associated with a heightened risk of thromboembolic complications. Various mechanisms are leading to the high thrombotic risk in COVID‐19 patients such as inflammation, endotheliitis, hyperviscosity, and hypercoagulability. We searched PubMed, EMBASE, and CINAHL from January 2020 to December 2020. We used the following search terms: COVID‐19, coagulopathy, and thrombosis. We reviewed the epidemiology, clinical features, mechanisms, and treatment of COVID‐19‐associated coagulopathy.
Keywords: COVID‐19, endotheliitis, heparin, microthrombosis, thrombosis
1. INTRODUCTION
The coronavirus disease 2019 (COVID‐19) pandemic is caused by the severe acute respiratory syndrome corona virus‐2 or SARS‐CoV‐2, which is a single‐strand positive‐sense RNA virus that belongs to the genera of betacoronaviridae. The virus is named corona because of the presence of a crown‐like halo on electron microscopy. The SARS‐CoV‐2 showed ∼96% sequence homology with the bat coronavirus RaTG13. 1 , 2 The high sequence homology may point towards bats origin of the virus and the possibility of species jumping. The sequence homology to SARS‐CoV and MERS‐CoV are 79.6% and 33.84%, respectively. 1 The virus entry inside the cell depends on the interaction between the viral spike protein or “s” protein and the human angiotensin‐converting enzyme 2 (ACE2). 3 The ACE2 protein is a membrane‐bound receptor expressed on the surface of lung alveolar epithelial cells (Type II pneumocyte) and enterocytes of the small intestine that explains the route of entry in COVID‐19 infection. 4 The serine protease TMPRSS2 primes the S protein for binding with the ACE2 receptor. Li et al. 5 reported the highest level of ACE2 expression in the small intestine, testis, kidneys, heart, thyroid, and adipose tissue, indicating that SARS‐CoV‐2 may infect various extrapulmonary organs. In December 2019, local health authorities in China reported a cluster of patients with mysterious pneumonia cases of unknown cause, which was initially linked to a seafood wholesale market in Wuhan, China. Zhu et al. 6 identified the causative agent as a novel coronavirus (2019‐nCoV) from samples of airway epithelial cells. From Wuhan, the disease spreads globally. Person‐to‐person transmission via droplets and contact is the main means of transmission. COVID‐19‐associated coagulopathy (CAC) is an important feature of COVID‐19 infection and may cause respiratory complications and death.
1.1. Pathophysiology of COVID‐19‐associated coagulopathy
COVID‐19 coagulopathy involves both the venous and arterial system, and it develops due to coagulation activation by several factors that affect Virchow's triad: endotheliitis, hypercoagulopathy, and stasis. The hyperinflammation of COVID‐19 infection itself may lead to a hypercoagulable state by activating the coagulation pathway and inactivating the anticoagulation and fibrinolysis pathway. Hypoxia due to COVID‐19 lung pathology may lead to vasoconstriction and hyperviscosity of the blood. 7 Moreover, hypoxia can shift the anti‐inflammatory and anti‐thrombotic properties of basal endothelium towards a proinflammatory and prothrombotic phenotype by altering the expression of transcription factors such as hypoxia‐inducible factor‐1 (HIF‐1). 8 Figure 1 shows the various pathogenesis mechanisms of COVID‐19‐associated coagulopathy.
FIGURE 1.
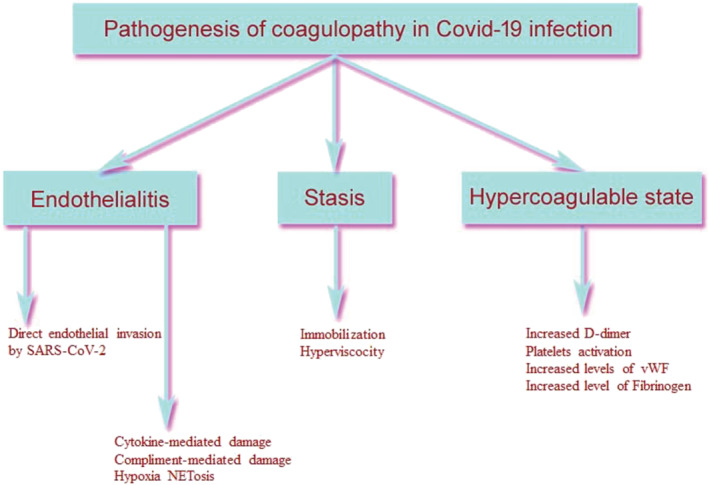
Various pathogenesis mechanisms of COVID‐19‐associated coagulopathy
1.2. Endothelium and SARS‐CoV‐2
The endothelium has an important role in mediating neutrophilic inflammation and microvascular thrombosis. Endothelial cells inhibit coagulation through several mechanisms. They display several anticoagulants substances such as proteoglycans, heparan sulfate, and thrombomodulin. Moreover, they sequester von Willebrand factor (vWF) within their storage granules as Weibel–Palade bodies (WPB). They also synthesize and release nitric oxide (NO), which inhibits platelet activation. 9 Endothelial dysfunction shifts the vascular endothelium from an anticoagulant to a procoagulant state. SARS‐CoV‐2 can directly infect endothelial cells of various organs via ACE2 receptors and can cause endotheliitis and its dysfunction. Varga et al. 10 noted the presence of viral inclusions in endothelial cells of various organs associated with diffuse endothelial inflammation and apoptosis. Autopsy study has also confirmed severe endothelial injury and the presence of intracellular viral particles. 11 Goshua et al. 12 reported significantly high levels of marker of endothelial and platelet activation in hospitalized patients with COVID‐19, which increased further with disease severity. The plasma mean vWF was 565% [SD 199] in 48 patients admitted to the ICU versus 278% [133] in 20 non‐ICU patients, p < 0.0001. Similarly, the soluble P‐selectin level was 15·9 ng/ml [4.8] versus 11·2 ng/ml [3.1], p = 0.0014, in ICU and non‐ICU patients, respectively. They also reported a significant correlation between endotheliopathy and mortality. Escher et al. 13 similarly reported markedly high vWF levels (vWF: antigen 555%, vWF: activity 520%) and Factor VIII levels (clotting activity of 369%) along with a continued rise in D‐dimer levels in a patient with severe COVID‐19 infection. All these indicate widespread activation of endothelial cells in COVID‐19 infection. Endothelial cell activation is triggered by various pathways such as proinflammatory cytokines, hypoxia, complement, and neutrophil extracellular traps (NETosis), resulting in the release of vWF and P‐selectin. The vWF promotes thrombosis by binding to platelet receptors and thus activate platelet adhesion and aggregation. 14 They may also cause thrombotic microangiopathy. 15 Moreover, along with angiopoitein‐2, vWF regulate angiogenesis also, characteristically seen in COVID‐19 infection. 16 Sugiyama et al. 17 had shown that experimental influenza infection of human endothelial cells promotes platelet‐endothelial adhesion and also induces shedding of cell surface anticoagulants. In the future, we need to study the role of antiplatelet agents on the outcome of respiratory viral infections.
1.3. Platelets and COVID‐19
Thrombocytopenia in COVID‐19 is usually mild. Huang et al. 18 reported a platelet count below 100 × 109/L only in 5% of hospitalized patients and 8% of those in ICU. The mechanisms of preserved platelet counts include an increased thrombopoietin production by liver activation and excessive platelet production by megakaryocytes in the lungs. 19 Significant thrombocytopenia, if occurs, is due to the consumption of platelets by the formation of pulmonary thrombi. 19 Lippi et al. 20 in a meta‐analysis of nine studies involving 1779 COVID‐19 patients (399 with severe disease) reported a significantly lower platelet count in patients with severe disease (weighted mean difference −31 × 109/L; 95% CI: −35 to −29 × 109/L). Subsequently, a subgroup analysis comparing patients by survival reported lower platelet count correlated with mortality. Manne et al. 21 have reported an increased gene expression and activation of platelets in COVID‐19 infection, which also supports its role in thrombosis. Because platelets lack SARS‐CoV‐2 ACE2 receptors, the activation of platelets may be mediated by an increased mitogen‐activated protein kinases (MAPK) pathway activation and thromboxane generation.
1.4. Inflammothrombiosis
Profound inflammation seen in COVID‐19 infection is the most likely cause of thrombus formation and the process is called immunothrombosis or thromboinflammation. The central component of thromboinflammation is the loss of normal anti‐inflammatory and antithrombotic functions of endothelium. Endothelial cells prevent thrombus formation in healthy individuals by exerting their antiplatelet, anticoagulant, and anti‐inflammatory actions. Inflammatory damage to endothelial cells due to SARS‐CoV‐2 leads to the following consequences: loss of anticoagulant surface, fibrin formation, release of endothelial granules and deposition of vWF, leukocyte recruitment, and complement activation. Apart from its effects on endothelium, the inflammatory pathway may also activate coagulation via other mechanisms: complement activation, NETosis, activation of monocytes. 22
1.5. Role of complement in thrombosis
The complement pathway is an important component of the innate defence system and helps in viral clearance. However, complement activations have several downstream deleterious effects such as inflammation, apoptosis, and thrombosis. Magro et al. 23 reported autopsy findings from five decedents with severe COVID‐19 infections and ARDS and observed evidence of complement‐mediated microvascular injury. They noted marked deposition of C5b‐9, C4d, and Mannan‐binding lectin serine protease (MASP)‐2 supporting a generalized activation of alternate and lectin‐based pathways. There was also evidence of co‐localization of SARS‐CoV‐2 and activated complement components. There are several mechanisms proposed about how the complement pathways are activated in COVID‐19 infection. Zhou et al. 24 had shown that Mannose‐binding lectin (MBL) binds to a site on SARS‐CoV “S” glycoprotein, which does not interfere with the viral binding with ACE2 receptors. This binding activated the lectin pathway. Complement activation may occur without interaction with the viral S protein. One important pathway is the Renin–Angiotensin–Aldosterone pathway. The ACE2 receptors undergo down‐regulation after SARS‐CoV‐2 binding, resulting in an accumulation of angiotensin II and Angiotensin‐(1–7). 25 The high angiotensin II and Angiotensin‐(1–7) lead to the generation of reactive oxygen species (ROS) formation and complement activation. It also interferes with the antioxidant mechanism. Activated complement and its products may promote thrombus formation by various mechanisms. It causes activation of platelets, endothelial cells, induction of tissue factors, secretion of VW factor, and enhanced expression of P‐selectin. The lectin pathway activates thrombin and fibrinolysis inhibitor. 26 Therefore, the SARS‐CoV‐2 infection has the potential to drive complement‐mediated inflammation, endothelial injury, and thrombosis. Diurno et al. 27 in a case series from Italy have reported efficacy of eculizumab in COVID‐19‐associated ARDS with a fall in inflammatory parameters.
1.6. Neutrophils extracellular traps
Neutrophils extracellular traps (NETs) are extracellular tangles of DNA released by Neutrophils and are enriched with granules‐derived antimicrobial peptides and enzymes. 28 The purpose is to contain the infection, but NETs also play a role in microthrombi formation by proving a scaffold and by promoting the propagation of thrombus. They do so by causing platelet and RBC adhesion and by concentrating effector proteins and coagulation factors. 29 , 30 Neutrophils bound to NETs in an active stage digests major coagulation inhibitors antithrombin III and tissue factor pathway. 31 Zuo et al. 32 reported significantly elevated levels of NETs in 50 hospitalized patients with COVID‐19 compared with healthy controls. Heparin destabilizes NETs by removing histone moiety, suggesting an additional antithrombotic effect of heparin. 28
1.7. Hyperviscosity
Maier et al. 33 reported hyperviscosity in 15 COVID‐19 patients and four patients with a viscosity above 3.5 cP had a documented thrombus. Hyperviscosity develops due to an increase in fibrinogen levels and can promote thrombosis as one of the components of Virchow's triad, and it can also damage the endothelium. 34 Fibrinolysis resistance is another potential mechanism of COVID‐19‐associated coagulopathy. 35 Children may be less prone to COVID‐19‐associated coagulopathy. 36 It is due to a higher α2‐Macroglobulin (α2‐M) level, which is a protease inhibitor and is having antithrombin activity. 37 Being localized on the luminal surface of the endothelium, α2‐M may protect the development of SARS‐CoV‐2‐induced thrombophlebitis.
1.8. Macrophage activation syndrome in COVID‐19 pneumonia
Macrophage activation syndrome (MAS) or secondary haemophagocytic lymphohistocytosis may develop in COVID‐19 patients and is characterized by highly elevated CRP and hyperferritinaemia, coagulopathy, and abnormal liver function. 38 , 39
1.9. Thrombotic microangiopathy
This is characterized by microvascular thrombosis, microangiopathic haemolytic anaemia (MAHA), and thrombocytopenia. On autopsy, microvascular thrombus has been detected in COVID‐19 infection. COVID‐19 patients may show decreased haemoglobin, increase in LDH, and bilirubin, and a decrease in haptoglobin along with schistocytes. 40 Features suggestive of thrombotic thrombocytopenia purpura (TTP) and haemolytic uraemic syndrome (HUS) have also been reported in the literature. 41
1.10. Antiphospholipids syndrome
Antiphospholipids syndrome is characterized by thrombotic complications, particularly in young patients. The COVID‐19 patients had shown the presence of antiphospholipids antibodies such as lupus anticoagulant and anticardiolipin, and anti‐β2‐glycoprotein antibodies have been detected in COVID‐19 patients. The characteristics laboratory parameter includes prolonged aPTT. However, the lupus anticoagulant data should be analysed with care in patients with COVID‐19 infection with underlying inflammation as markedly high CRP may cause false‐positive result if CRP sensitive reagents are used. 42 , 43
2. CLINICAL MANIFESTATIONS OF COVID‐19‐ASSOCIATED COAGULOPATHY
COVID‐19 infection is a state of hyperinflammation and systemic hypercoagulability characterized by a tendency of venous, arterial, and microvascular thrombosis. Another characteristic of CAC is the frequent occurrence of catheter‐associated thrombosis and clotting of vascular access catheter and dialysis circuits. The risk of thrombosis is high in hospitalized COVID‐19 patients and in particular patients admitted in the intensive care unit (ICU). Patients may develop myocardial infarction, and the culprit lesion is not identified by coronary angiography in approximately 40% of patients with COVID‐19 with an acute ST‐elevation myocardial infarction (STEMI). 44
Thrombotic phenomenon seen in COVID‐19 infection:
Microthrombosis of various organs, often leading to organ dysfunction (lung, kidney, and liver, etc.);
Venous thromboembolism (VTE): pulmonary embolism (PE) and deep vein thrombosis (DVT);
Stroke: large vessels and often young patients 45 ;
Myocardial infarction, often in absence of culprit lesions;
Thrombosis occurs despite routine thromboprophylaxis. 46
The evidences for COVID‐19‐associated coagulopathy are the following evidences: high D‐dimer, increase VTE prevalence, cerebrovascular accident (CVA) (case reports) and microthrombosis (autopsy studies). D‐dimer is the degradation product of cross‐linked fibrin and is measured by two different assays based on molecular weight: fibrinogen equivalent unit (FEU) and D‐dimer unit (DDU). The normal reference range is <500 ng/ml FEU. The source of elevated D‐dimer in COVID‐19 infection is excessive fibrinolysis. Fibrinolysis of the fibrin deposited in the intra‐alveolar space in acute lung injury patients may also raise the D‐dimer levels. 47 The fibrinolysis process is being mediated by the urokinase‐type plasminogen activator (uPA) secreted by the alveolar epithelial cells. 48 The endothelial cells damaged by inflammation may also elevate the D‐dimer levels in COVID‐19 infection. 10 The CD169+ macrophages are also important in SARS‐CoV‐2 viral spread within the body 49 and are responsible for D‐dimer generation.
Elevated D‐dimer on admission is a poor prognostic marker and is associated with severe disease and in‐hospital mortality. In a retrospective study from China, which included 1099 COVID‐19 patients, a D‐dimer ≥0.5 μg/ml was observed among 60% of patients with severe disease compared with 43.2% patients with mild disease (p = 0.002). Patients who attained the primary composite endpoint (admission to an intensive care unit, the use of mechanical ventilation, or death) had a higher D‐dimer level compared with those who did not (69.4% vs.44.2%). However, thrombocytopenia defined as a platelet count of less than 150 × 109/L was seen in only 36.2% of patients of COVID‐19 disease. 50 Huang et al. 18 in a prospective study of 41 COVID‐19 positive cases reported a significantly high D‐dimer level and PT on admission in ICU patients compared with those in the wards (D‐dimer level: 2.4 and 0.5 mg/L, respectively, p = 0.0042). The corresponding PT values were 12.2 and 10.7 s, respectively (p value = 0.012). Zhou et al. 51 in a multivariable regression analysis of 191 COVID‐19 patients reported an odds ratio of 18.42 (2.64–128.55, p = 0.0033) of in‐hospital mortality for patients with a D‐dimer of >1 μg/ml. Other factors included older age (OR: 1.10, 95% CI: 1.03–1.17, p value = 0.0043) and higher sequential organ failure score (SOFA) score (OR: 5.65, 95% CI: 2.61–12.33, p = <0.0001). A low platelet count (<100 × 109/L) and a high prothrombin time (PT) (≥16 s) levels were observed in 20% and 13% of nonsurviving patients, respectively.
Tang et al. 52 in a retrospective‐designed study from Wuhan, China, reported a difference in coagulation profiles in patients with COVID‐19 infection between survivors and nonsurvivors. They reported an overall mortality of 11.5%. The coagulation profiles of the nonsurvivors on admission were as follows: a significantly higher D‐dimer (2.12 mg/L vs. 0.61 mg/L, p value < 0.001) and fibrin degradation product (FDP) levels, a significantly longer PT and aPTT levels compared with survivors. However, the fibrinogen level was elevated in both the group. They also reported the progression of coagulopathy to overt DIC as indicated by the International Society on Thrombosis and Haemostasis (ISTH) DIC score of ≥5 in 71.4% of nonsurvivors compared with 0.6% of survivors only. Petrilli et al. 53 in a single‐centre prospective cohort study conducted on 5279 COVID‐19 patients admitted to a hospital in New York City reported that a D‐dimer level of >2500 ng/ml was more strongly associated with critical illness than age or comorbidities (odds ratio: 3.9, range 2.6 to 6.0).
VTE risk is high in patients with COVID‐19, and ICU patients with severe COVID‐19 infections have a higher incidence of VTE than patients admitted in the general wards and historic ICU rates, despite standard VTE prophylaxis. The prevalence is heterogeneous in various studies. The majority of studies were retrospective in nature and including inpatients in ICU. Moreover, there was inconsistent use of thromboprophylaxis also. Llitjos et al. 54 screened 26 severe COVID‐19 patients in two French intensive care units (ICU) by complex duplex ultrasound (CDU). All patients were on anticoagulation: prophylactic anticoagulation in eight (31%) patients and therapeutic anticoagulation in 18 (69%) patients. The cumulative incidence of peripheral VTE was 69%, which included six patients with PE (23%). The VTE incidence in the prophylactic and therapeutic anticoagulation group was 100% and 56%, respectively (p = 0.03). Klok et al. 46 evaluated the cumulative incidence of venous and arterial thrombotic events, including DVT, PE, ischaemic strokes, and myocardial infarction in 184 patients admitted to the ICU. All patients received nandroparin (2850 to 5700 IU per day based on body weight) prophylaxis. The composite incidence of thrombotic events was 31% (95% CI: 20–41) and arterial thrombosis was 3.7% (95% CI: 0–8.2). Computed tomography‐diagnosed pulmonary embolism was the most frequent thrombotic complication (n = 25, 81%). Age and coagulopathy defined as prolongation of PT > 3 s and aPTT > 5 were the independent predictors of thrombotic events. DIC was not detected in any patient. Helms et al. 55 in a French prospective study involving 150 critically ill COVID‐19 patients reported thrombotic complications developed in 64 patients and majority of them had a pulmonary embolism (16.7%) despite thromboprophylaxis. Patients with COVID‐ARDS develop significantly higher thrombotic complications than non‐COVID‐ARDS (11.7% versus 2.1%, p value <0.008). Among 29 patients undergoing renal replacement therapy, 28 (96.6%) developed circuit clotting, and three out of 12 patients requiring extracorporeal membrane oxygenator (ECMO) developed circuit thrombotic occlusions. The authors reported the presence of Lupus anticoagulant in 50 of 57 patients tested (87.7%). None of the COVID‐19‐associated ARDS developed DIC. Al‐Samkari et al. 56 retrospectively analysed the incidence of thrombotic and haemostatic complications of 400 hospitalized COVID‐19 patients from the United States. Radiographically confirmed VTE was 4.8% (95% CI: 2.9–7.3), 3.1% in noncritically ill patients and 7.6% in critically ill patients. Overall incidence of VTE was 9.5%. All patients were receiving standard‐dose thromboprophylaxis. Arterial thrombosis was detected in 2.8%. They also reported an overall bleeding rate of 4.8%, and it was 7.6% among critically ill patients. Elevated D‐dimer (D‐dimer > 2500 ng/ml) had an odds ratio of 6.79 for thrombosis. Thrombosis was also associated with inflammatory markers.
Another striking complication of COVID‐19 infection is the occurrence of acute large vessel occlusion in patients less than 50 years of age presenting with ischaemic strokes. Among the five patients reported in the case series by Oxley et al., 45 the youngest one was 33 years of age and the mean National Institute of Health stroke scale (NIHSS) score was 17, suggestive of severe large vessel stroke. In the Klok et al. 46 series, out of 184 patients, 65 patients were diagnosed with PE, five developed ischaemic strokes, and two patients had arterial thrombosis. Beyrouti et al. 57 published a case series of six COVID‐19 patients with ischaemic stroke with the youngest patient of age 53 years. Most patients had severe disease and various underlying comorbidities. They reported the following distinct characteristics:
Large vessel occlusion in all patients and in three, it involves multiple territories;
Ischaemic stroke developed in two patients despite on thromboprophylaxis;
Majority of patients had a very high D‐dimer level (>7000 μg/L);
Concurrent VTE developed in two patients;
Majority developed ischaemic stroke 8–24 days after symptoms onset, indicating a delayed onset of COVID‐19‐associated stroke;
Concurrent venous thromboembolism may occur;
Positive lupus anticoagulant without a history of antiphospholipid syndrome.
Annie et al. 58 in database‐based research from the United States found a low incidence of stroke of 0.7% among young patients ≤50 years of age; however, patients who developed stroke had a grim prognosis. In a systematic review, Wijeratne et al. 59 observed that patients with higher neutrophil–lymphocytes ratios on admission had a shorter interval between infective symptoms of COVID‐19 and clinical manifestations of ischaemic stroke. The prognosis was also poor as 75% of patients with acute ischaemic stroke died or were severely disabled. An ischaemic stroke usually occurs 8–24 days after symptom onset but may also occur in the early phase of the disease. The mechanisms of ischaemic stroke in COVID‐19 infection are the hypercoagulable state, vasculitis, and cardiomyopathy. 60
Zhang et al. 61 documented antiphospholipid antibodies in three ICU patients with multiple hemispheric infarcts. Antiphospholipid antibodies consist of lupus anticoagulant (LA), anticardiolipin antibody, and anti‐ß2 glycoprotein 1 antibody. They also reported concomitant elevation of PT, aPTT, fibrinogen, D‐dimer, and CRP. Bowles et al. 62 found LA in 31 of 34 (91%) COVID‐19 patients who had an elevated aPTT; however, the frequency of VTE was 6%. The significance of LA and APLA in COVID needs further exploration.
2.1. Microvascular thrombi
Two types of microthrombi have been reported in the literature: hyaline platelet‐fibrin thrombi located in capillaries and arterioles and laminated fibrin clots seen in preacinar and large intra‐acinar arteries. 63 , 64 Fox et al. 65 performed autopsies on four decedents from New Orleans, LA, and reported small vessel occlusion due to fibrin‐platelets accumulation and microangiopathy along with haemorrhage. They also noted the absence of thromboembolism in the pulmonary arteries at the hilum. Microscopic examination also revealed CD61 + megakaryocytes within alveolar capillaries, actively producing platelets. In another autopsy series, Ackermann et al. 11 observed distinctive vascular changes in COVID‐19 pneumonia. They compared autopsy findings of COVID‐19 patients with lungs obtained on autopsy from patients with ARDS secondary to influenza A (H1N1) infection and age‐matched, uninfected control lungs. They reported a ninefold higher prevalence of microthrombi and a twofold increase in angiogenesis in COVOID‐19 infection compared with influenza infection (p value <0.001). There was also evidence of endotheliitis. Similarly, Menter et al. 66 published the autopsy findings of COVID‐19 patients from Switzerland and noticed microthrombi of alveolar capillaries in 45% of patients. Microvascular thrombi are not a unique feature in patients with COVID‐19 infection and have been observed in ARDS due to various causes. 64 Microvascular thrombosis in patients with COVID‐19 infection may cause hypoxemic respiratory failure with preserved compliance.
2.2. COVID‐19 coagulopathy versus sepsis‐induced disseminated intravascular coagulation (DIC)
COVID‐19‐associated coagulopathy differs from the classical sepsis‐induced DIC. Delabranche et al. proposed a three‐step model in the natural history of sepsis‐induced coagulopathy (SIC): adaptive haemostasis, thrombotic DIC, and fibrinolytic DIC. 67 Phase of adaptive haemostasis is characterized by an increase in platelet count, and fibrinogen production, shortening of PT and activated partial thromboplastin time (aPTT). The inhibition of fibrinolysis by plasminogen activator inhibitor‐1 (PAI‐1) results in a low D‐dimer level. The thrombotic DIC phase is characterized by a prolonged clotting time (PT and aPTT) with a high platelet and fibrinogen consumption leading to a decrease in their levels. D‐dimer is also moderately increased. The stage of fibrinolytic DIC shows very low levels of fibrinogen, platelets, a prolonged PT and aPTT, and very high D‐dimers. Microangiopathic haemolytic anaemia may also be seen. Therefore, the classical laboratory findings include reduced platelet counts and fibrinogen levels, an increase in PT, aPTT, and D‐dimer levels. The COVID‐19‐associated coagulopathy, in contrast, shows a more profound rise in the D‐dimer level. The PT and aPTT time remains either normal or mildly elevated. The fibrinogen level is elevated in COVID‐19 infection unlike in sepsis‐induced DIC where the level is decreased. This is the reason why thrombosis is more common in COVID‐19 infection rather than bleeding. The platelet count is usually normal or there is mild thrombocytopenia. Huang et al. 18 reported a platelet count of less than 100 × 109/L in only 5% of 41 hospitalized COVID‐19 patients from China. The absence of thrombocytopenia indicates that CAC is not a consumptive coagulopathy unlike DIC. Another reason for a lack of thrombocytopenia is proinflammatory cytokines secreted in COVID‐19 patients which increase platelet counts. 68 Table 1 shows the distinguishing features of disseminated intravascular coagulation and COVID‐19‐ associated coagulopathy.
TABLE 1.
The distinguishing features of disseminated intravascular coagulation and COVID‐19‐associated coagulopathy
| Parameters | DIC | COVID‐19 coagulopathy |
|---|---|---|
| D‐dimer | Increased | Profoundly increased |
| PT | Frequently Increased | Normal or increase |
| aPTT | Frequently Increased | Normal or increase |
| Platelet count | Frequently low | Normal, thrombocytopenia rare |
| Fibrinogen | Decrease | Increase initially, may decrease in later stage |
| Fibrin degradation products (FDPs) | Increased | Increased |
| Consumptive coagulopathy | Seen | Rare |
| vWF | Increased | increased |
| Antithrombin (AT) | Decreased | Increased |
| Outcome | Bleeding | Thrombosis |
3. LABORATORY INVESTIGATIONS
The ISTH recommends measurement of the following parameters in decreasing order of importance: D‐dimer, PT, and platelet count in all patients presenting with COVID‐19 infection. 69 Other parameters are aPTT, INR, fibrin degradation products, and fibrinogen. The D‐dimer and fibrinogen if showing a rising trend should be monitored on daily basis. Worsening of D‐dimer indicates severe disease and poor prognosis.
3.1. Rotational thromboelastometry
There are various point‐of‐care (POC) coagulation monitoring devices that assess the viscoelastic properties of whole blood, for example, thrombelastography (TEG®), rotation thrombelastometry (ROTEM®), and Sonoclot® analysis. 70 This technique has the advantage of measuring the clotting process, starting with fibrin formation and continue through to clot retraction and fibrinolysis at the bedside of the patients. 71 Pavoni et al. 72 in a retrospectively‐designed study analysed 40 critically ill Italian patients by rotation thrombelastometry (ROTEM®) on the day of admission, days 5 and 10. The VTE was detected in 20% of patients. The whole blood thromboelastometry showed evidence of hypercoagulability such as a shortened clotting time (CT), shortened clot formation time (CFT), and increase in maximum clot firmness (MCF). No evidence of secondary hyperfibrinolysis was seen. The hypercoagulable state persists initially for the first 5 days. It starts decreasing 10 days later and does not return to the normal values. Panigada et al. 73 evaluated 24 severe COVID‐19 patients by thromboelastography and observed a hypercoagulable state rather than DIC. There was a decrease in R (time to fibrin formation) and K (time to 20‐min clot) values and increased K (speed to clot) angle and MA (clot strength). The fibrinogen level and D‐dimer levels are increased.
3.2. Prevention and management of COVID‐19‐associated coagulopathy
Anticoagulant therapy was associated with decreased mortality in COVID‐19 patients. In a retrospective study, Tang et al. 74 evaluated the effect of prophylactic anticoagulation on 28‐day mortality in a cohort of 449 patients with severe COVID‐19 infection, 99 patients received prophylactic VTE anticoagulation for at least 7 days. Ninety‐seven (22%) patients had an ISTH SIC score of >4. Overall, they could not detect any difference in 28‐day mortality between heparin users and nonheparin‐treated patients. However, when stratified by D‐dimer level and SIC score, they observed 28‐day mortality benefit with heparin use only in patients with an elevated D‐dimer sixfold higher than ULN (32.8% vs. 52.4%, p value 0.017) and SIC ≥ 4 (40.0% vs. 64.2%, p value 0.029). Patients with a high D‐dimer or meeting SIC criteria (Table 2) have a better prognosis with anticoagulation therapy. However, the authors did not mention the incidence of VTE. Yin et al. 75 in a retrospective study had shown a significant decrease in 28‐day mortality in heparin users compared with nonusers when the D‐dimer level was more than six times the upper limit of normal (>3.0 μg/ml) (32.8% vs. 52.4%, p = 0.017). Paranjpe et al. 76 evaluated the effect of in‐hospital treatment dose anticoagulation and survival in 2773 COVID‐19 patients in New York and found benefit in a subset of patients requiring intubation (n = 395). The in‐hospital mortality and median survival in the anticoagulant group were 29.1% and 21 days as compared with 62.7% and 9 days, respectively, in those who did not receive treatment dose anticoagulation. Major bleeding has been reported in 3% of cases. This study also found that the anticoagulated group required invasive mechanical ventilation to a significantly high number. However, the authors did not mention the rationale of anticoagulation therapy, so this is difficult to interpret. Table 2 shows the ISTH‐proposed SIC scoring. 78 Heparin has several other potential benefits that seem attractive in the setting of COVID‐19 infection. It has antivirals: anti‐inflammatory, endothelial protection activity. 79 SARS‐CoV‐2 viral entry inside cells is mediated by binding of the viral spike protein to ACE2 receptors. Cell surface heparan sulfate is one co‐factor for viral entry. 80 Heparin being a glycosaminoglycan similar to heparin may bind with the spike protein and impair viral entry.
TABLE 2.
The International Society of Thrombosis and Haemostasis (ISTH) proposed “sepsis‐induced coagulopathy” (SIC) scoring 77
| Item | Score | Range |
|---|---|---|
| Platelet count (×109/L) | 1 | 100–150 |
| 2 | <100 | |
| PT‐INR | 1 | 1.2–1.4 |
| 2 | >1.4 | |
| SOFA score | 1 | 1 |
| 2 | ≥2 | |
| Total score for SIC | ≥4 |
3.3. Venous thromboembolism prophylaxis
In patients with COVID‐19‐related acute illness who do not have suspected or confirmed VTE, the American Society of Hematology (ASH) 2021 recommends prophylactic dose thromboprophylaxis over intermediate‐intensity or therapeutic‐intensity thromboprophylaxis. 81 ISTH interim guidance on recognition and management of coagulopathy in COVID‐19 also recommended thromboprophylaxis with low molecular weight heparin (LMWH) in all hospitalized COVID‐19 patients except in the presence of active bleeding, platelet counts less than 25 × 109/L, or fibrinogen less than 0.5 g/L. 69 The bleeding risk should always be assessed routinely. In a retrospective analysis, Nadkarni et al. 82 reported the following major bleeding rates: 3.0% in patients on therapeutic anticoagulation, 1.7% in patients on prophylactic anticoagulation compared with 1.9% in patients who were not receiving any anticoagulation. Patients with a contraindication to pharmacological prophylaxis should receive mechanical thromboprophylaxis, for example, intermittent pneumatic compression devices. However, they should be regularly reassessed for switching over to pharmacological prophylaxis. LMWH is preferred over UFH as the latter requires frequent monitoring and increasing healthcare staff contact with patients. Alhazzani et al. 83 in a systematic review and meta‐analysis that included seven trials with 7226 medical‐surgical ICU patients in 2013 observed that compared with UFH, LMWH reduced the rates of pulmonary embolism (risk ratio, 0.62 [95% CI: 0.39, 1.00]; p = 0.05; I = 53%) and symptomatic pulmonary embolism (risk ratio, 0.58 [95% CI: 0.34, 0.97]; p = 0.04). However, there was no significant differences in major bleeding and DVT. Factors that may help in deciding the choice of anticoagulants include availability, resources required, familiarity, minimization of personal protective equipment (PPE) use, renal function, a history of heparin‐induced thrombocytopenia, concerns about gastrointestinal tract absorption, and drug–drug interactions. 81 Fondaparinux may be considered in patients with a history of heparin‐induced thrombocytopenia. Pharmacological thromboprophylaxis with heparin reduces mortality in patients with SIC score >4 or D‐dimer >6 times the ULN. 74 Pharmacological thromboprophylaxis for outpatients with COVOID‐19 infection is not routinely recommended; however, thromboprophylaxis may be considered in patients with immobility, particularly when other risks factors for VTE such as the history of prior VTE or malignancy are present. 84
3.4. Hospitalized patients with severe COVID‐19
The incidence of VTE is particularly high in severe COVID‐19 patients, and the threshold for ordering investigation for VTE should be low, particularly in patients with sudden, rapid deterioration in oxygen saturation (unexplained), tachypnoea, unilateral leg symptoms, and hypotension. Screening for DVT can be done by point of care ultrasounds (POCUS) in the ICU. 85 Patients with COVID‐19‐related critical illness who do not have suspected or confirmed VTE, the ASH 2021 guideline recommends prophylactic dose thromboprophylaxis over intermediate‐intensity or therapeutic‐intensity thromboprophylaxis. 81 The randomized, multicentric INSPIRATION trial randomly assigned 600 people with critical COVID‐19 admitted in the ICU to receive intermediate‐dose (enoxaparin, 1 mg/kg daily) or standard‐dose prophylactic (enoxaparin, 40 mg daily). The intermediate‐dose prophylactic did not improve a composite outcome of thrombosis, use of ECMO, or mortality within 30 days (hazard ratio [HR] 1.06; 95% CI: 0.83 to 1.36). 86 The intermediate‐dose cohort also had an increased, although statistically nonsignificant trend towards bleeding. Therefore, the routine use of intermediate‐dose prophylactic is not recommended. The preprint version of the three randomized trials (REMAP‐CAP, ACTIV‐4a, ATTACC) that included 1074 hospitalized patients with severe COVID‐19 reported that the therapeutic‐dose anticoagulation did not improve the hospital survival compared with the standard prophylactic dosing (64.3 vs. 65.3%, adjusted odds ratio [OR] 0.88; 95% CI: 0.67 to 1.16). The median organ support‐free days were 3 days (interquartile range −1, 16) and 5 days (interquartile range −1, 16), respectively, in patients assigned to therapeutic anticoagulation versus usual care pharmacological thromboprophylaxis (adjusted odds ratio 0.87, 95% credible interval [CrI]: 0.70–1.08, posterior probability of futility [odds ratio < 1.2] 99.8%). The major bleeding was reported in 3.1% of patients on therapeutic dosing and 2.4% of those assigned to standard prophylaxis. The difference was not statistically significance. 87 Thromboprophylaxis should be given for the entire duration of the hospital stay. Figure 2 shows the thromboprophylaxis at various sites of care.
FIGURE 2.
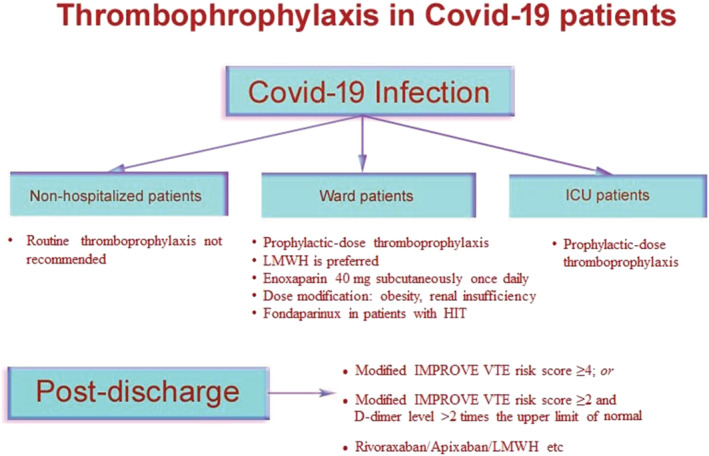
Thromboprophylaxis in COVID‐19 patients at various sites of care
3.5. Indications for therapeutic‐dose anticoagulation (e.g., enoxaparin 1 mg/kg every 12 h) 88 , 89 , 90
Therapeutic dose anticoagulation should only be used in patients with proven VTE unless there is a contraindication to anticoagulation. Patients with strongly suspected VTE in whom a standard computed tomography with pulmonary angiography (CTPA) or ventilation/perfusion (V/Q) scan is not feasible, the following may be sufficient to initiate treatment:
Evidence of DVT (confirmed by POCUS);
Consider PE in the case of:
-
a
Sudden unexplained deterioration in respiratory status (acute worsening of oxygenation, blood pressure, tachycardia with chest imaging findings are not consistent with worsening COVID‐19 pneumonia or fluid overload);
-
b
Marked increase/rising D‐dimer from priors;
-
c
Point of care transthoracic echocardiography showing presence of clot in transit in the main pulmonary artery or intra‐cardiac, evidence of acute, otherwise unexplained right heart strain and high clinical suspicious for PE;
-
d
Recurrent clotting of intravascular access devices (arterial lines, central venous catheters) or extracorporeal circuits (continuous renal replacement therapy, extracorporeal membrane oxygenation [ECMO]) despite prophylactic‐intensity anticoagulation. The intensity of anticoagulation may be increased after assessment of individual patient's bleeding risk;
-
e
Hospitalized COVID‐19 patients who are already receiving therapeutic anticoagulation with direct‐acting oral anticoagulant or warfarin (for atrial fibrillation, prosthetic heart valves and history of previous VTE), therapeutic‐dose enoxaparin should be used.
3.6. Standard prophylactic dose
Enoxaparin 40 mg subcutaneously once daily is given. Patients with BMI > 40 should receive enoxaparin 40 mg subcutaneously every 12 h. 91 Patients with renal insufficiency should have their enoxaparin dose modified or should receive UFH. Fondaparinux should be used 2.5 mg daily if creatinine clearance >50 ml/min and 1.5 mg daily if creatinine clearance is between 20 and 50 ml/min. 92
3.7. Intermediate‐intensity anticoagulation
Enoxaparin 40 mg subcutaneously every 12 h is given if BMI < 40 or 0.5 mg/kg subcutaneously every 12 h should be given especially if the patient is obese.
3.8. High‐intensity anticoagulation
Enoxaparin 1 mg/kg subcutaneously every 12 h is administered when creatinine clearance above 30 ml/min. if creatinine clearance is less than 30 ml/min, Enoxaparin 1 mg/kg subcutaneously once daily or IV UFH should be given. Monitoring of UFH should be based on anti‐Xa assay as APTT level is often raised in COVID‐19. 93
3.9. Patients on chronic anticoagulation therapy
Patients who are on chronic anticoagulation therapy are at risk of contracting SARS‐CoV‐2 infection due to frequent hospital visits. Their hospital visit due to periodic INR testing should be minimized. The American College of Chest Physicians' guideline suggested that a 12‐week INR testing interval may be appropriate. 91 Other options would be to use portable coagulometers, which the patient can use at home. Warfarin may also be switched to a direct oral acting anticoagulant (DOAC) except in patient with an antiphospholipid syndrome or those who are on mechanical valve prostheses, valvular atrial fibrillation, and breastfeeding patients. 92 Stable COVID‐19 patients who are on a DOAC may continue it but should switch if any sign of progression of COVID‐19 infection occurs. Stable COVID‐19 patients on warfarin should be considered switching over to LMWH/UFH. Similarly, unstable COVID‐19 patients should be switched over to LMWH/UFH for the better ability to monitor.
4. DIAGNOSIS OF PE
Diagnosis of PE is difficult in COVID‐19 patients due to the issues of getting the radiological investigations as shifting the patients outside the ICU for imaging is often difficult and may contaminate the surroundings. 93 As the incidence of VTE is high in COVID‐19, the clinical threshold for ordering investigation should be low. A presumptive diagnosis of PE should be considered in patients with sudden, unexplained hypoxemia, hypotension, tachycardia, tachypnoea, increasing A‐a gradient, increasing oxygen requirements disproportionate to the radiological severity of pneumonia, and new right ventricular strain on bedside echocardiography. The European Society of Radiology and the European Society of Thoracic Imaging 94 suggested that if supplemental oxygen is needed in patients with limited disease extension, contrast‐enhanced CT should be performed to rule out PE. Therapeutic anticoagulation may be initiated even with a presumptive diagnosis. The duration of anticoagulation in suspected or confirmed VTE cases should be 3–6 months. Treatment of VTE should consider the following factors: renal function and bleeding risk (e.g., thrombocytopenia), drug–drug interactions, and the issues with monitoring.
5. OUTPATIENT THROMBOPROPHYLAXIS
Gervaise et al. 95 evaluated retrospectively evaluated 72 nonhospitalized COVID‐19 patients who were referred to the emergency department for CTPA and observed acute PE in 18% of COVID‐19 patients. Routine outpatient prophylaxis is not recommended. However, there is a possibility of potential benefits in patients with underlying comorbidities or past/family history of VTE or thrombophilia. However, future clinical trials will answer this question.
5.1. Extended thromboprophylaxis
Bajaj et al. 96 in a systematic review and meta‐analysis of five trials including 40 247 patients hospitalized for acute medical illness reported the beneficial effects of extended postdischarge thromboprophylaxis by 4 to 6 weeks period in reducing symptomatic or fatal VTE events. However, there was an increased risk of major or fatal bleeding. In another systematic review and meta‐analysis, Chiasakul et al. 97 reported that extended prophylaxis significantly decreased the risk of symptomatic VTE (RR = 0.52; 95% CI: 0.36–0.76, I 2 = 38%) but not VTE‐related death (RR = 0.80; 95% CI: 0.60–1.09, I 2 = 0%). However, it significantly increased the risk of major bleeding (RR = 2.04; 95% CI, 1.42–2.91, I 2 = 23%). An exploratory analysis of Mariner study regarding the role of extended duration rivaroxaban therapy of 10 mg once a day for 45 days among hospitalized medically ill patients showed a 28% reduction in fatal and major thromboembolic events without a significant increase in major bleeding risk. 98 Roberts et al. 99 reported a postdischarge VTE rate of 4.8 per 1000 discharges after 1877 discharges compared with 3.1 per 1000 discharges in 2019 among non‐COVID patients (after 18 159 discharges) within 42 days after discharge. The odds ratio for postdischarge VTE associated with COVID‐19 compared with control was 1.6 (95% CI: 0.77–3.1). Therefore, routine postdischarge prophylaxis is not recommended in all patients with COVID‐19. However, all hospitalized COVID‐19 patients should be routinely screened for extended thromboprophylaxis.
The following criteria may be used to select a patient for extended thromboprophylaxis
Modified International Medical Prevention Registry on Venous Thromboembolism (IMPROVE) VTE risk score ≥4; or
Modified IMPROVE VTE risk score ≥2 and D‐dimer level >2 times the upper limit of normal. 100 , 101
Any decision to use postdischarge VTE prophylaxis for patients with COVID‐19 should include consideration of the individual patient's risk factors for VTE, including reduced mobility, bleeding risks, and feasibility. Participation in clinical trials is also encouraged. Table 3 shows the modified IMPROVE‐VTE risk score. 102
TABLE 3.
Modified IMPROVE‐VTE risk score 102
| VTE risk factor | VTE risk score |
|---|---|
| Previous VTE | 3 |
| Known thrombophilia | 2 |
| Current lower limb paralysis or paresis | 2 |
| History of cancer excluding non‐melanoma skin cancer present at any time in the past 5 years (cancer must be in remission to meet eligibility criteria) | 2 |
| ICU/CCU stay | 1 |
| Complete immobilization ≥1 day | 1 |
| Age ≥60 years | 1 |
The following drugs may be used for extended postdischarge prophylaxis. 103 , 104
Rivaroxaban: 10 mg orally once daily for 31 to 39 days. Dose modification: It should not be used with a creatinine clearance (CrCl) of <30 ml/min;
Betrixaban: 160 mg orally loading dose, followed by 80 mg once daily thereafter for 35 to 42 days. Dose modification: if CrCl 15–29 ml/min, 80 mg orally loading dose, followed by 40 mg once daily;
Enoxaparin 40 mg subcutaneously once a day. Dose modification: if CrCl 15–29 ml/min, Enoxaparin 30 mg subcutaneously once a day, if CrCl <15 ml/min, consider other options.
The American College of Cardiology (ACC) suggested extended thromboprophylaxis with LMWH or DOACs for a maximum period of 45 days in case of high risk for VTE such as D‐dimer level of more than two times the upper limit of normal or presence of active cancer and a low risk of bleeding.
5.2. Drug–drug interactions
LMWH, UFH, and Fondaparinux can be given safely with other COVID‐19 drugs as there are no proven interactions. Moreover, the anti‐inflammatory effects of Heparin could have a potential benefit. 105 Lopinavir–ritonavir inhibits CYP3A4 and P‐gp and increases the blood level of direct Xa inhibitors such as apixaban and rivaroxaban. 106 Similarly, chloroquine/hydroxychloroquine increases the blood level of direct Xa inhibitors.
5.3. Role of thrombolysis in patients with COVID‐19
Wang et al. 107 in a small case series of three patients with COVID‐19‐associated ARDS studied the role of tPA. The tPA dose used was 25 mg given intravenously over 2 h followed by a 25‐mg tPA infusion over the subsequent 22 h. Anticoagulation therapy was withheld during tPA infusion. All three patients showed an initial improvement in PaO2/FiO2 ratio; however, the improvement was durable in only one patient. There were no bleeding events. Thrombolytic therapy has also been associated with bleeding complications. There is currently no high‐quality evidence for thrombolysis in COVID‐19 patients. Therefore, thrombolytic should be used only in the following clinical conditions such as ST‐elevation myocardial infarction, acute ischaemic stroke, or high‐risk (massive) PE with haemodynamic compromise. 93
5.4. COVID‐19 and heparin resistance
Heparin resistance is defined as the need for 35 000 units of heparin (UFH)/day. 77 Causes include antithrombin deficiency, presence of heparin‐binding proteins (platelet factor4, histidine‐rich glycoprotein, vitronectin, fibronectin), and elevated factor VIII and fibrinogen, which affect aPTT. White et al. 108 reported heparin resistance in 80% of ICU admitted COVID‐19 patients and a suboptimal peak anti‐Xa following therapeutic anticoagulation in 100% patients where it was measured. Patients with heparin resistance should be monitored with anti‐Xa rather than aPTT. Dutt et al. 109 evaluated anti‐FXa activity in hospitalized COVID‐19 patients who were receiving enoxaparin 40 mg once a day with normal creatinine clearance and platelet counts. They compared the 4‐h postdose anti‐FXa between the ward and ICU patients. About 95% of ITU patients failed to achieve the target anti‐FXa activity (0.2–0.4 IU/ml) compared with 27% of ward patients. This study suggests two things: first ITU patients with COVID‐19 required augmented pharmacological thromboprophylaxis. Second, anti‐FXa‐guided LMWH dosing is important even in the ward patients as approximately 30% showed suboptimal anti‐FXa levels with standard dosing. Monitoring inaccuracies regarding measurement of anti‐FXa and aPTT may occur in patients with COVID‐19 and severe illness. Elevated fibrinogen and elevated factor FVIII falsely lower the aPTT levels whereas hypertriglyceridemia increases anti‐FXa level and antiphospholipid antibodies increases levels of both anti‐FXa and aPTT. 110
5.5. Choice of agents
There is no study comparing various anticoagulant agents in COVID‐19 infection. However, data extrapolated from the study done in patients with acute medical illness had shown no benefit of direct oral anticoagulant (DOACs) drugs over LMWH. Neumann et al. 111 in a systematic review reported that the use of DOACs was not associated with a reduction in the risk of PE or symptomatic DVT in comparison with LMWH. Moreover, there was an increased risk of major bleeding (RR 1.70; 95% CI: 1.02–2.82). The Chest guideline recommends LMWH, Fondaparinux, or UFH over the use of DOACs in acutely ill hospitalized patients with COVID‐19. In acutely ill hospitalized patients with COVID‐19, LMWH and Fondaparinux should be preferred over UFH as it will prevent exposure of HCWs. 112 , 113
5.6. Conclusions
COVID‐19 infection is associated with a higher incidence of the thromboembolic phenomenon and the incidence is particularly high in ICU patients. COVID‐19‐associated coagulopathy is a predictor of poor outcome. All hospitalized COVID‐19 patients should be advised pharmacological thromboprophylaxis unless there is contraindication. The role of intermediate to high dose thromboprophylaxis needs further well‐designed study.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
AUTHOR CONTRIBUTION
MS conceived and designed the article, made critical revisions, and approved the final version. MS, IM, PNQ, and MBG collected data and wrote the first draft of the manuscript. MS, IM, PNQ, and MBG contributed to the writing of the manuscript. IM, MS, and MBG drew the images. All authors reviewed and approved the final manuscript.
ETHICS STATEMENT
Not required.
ACKNOWLEDGMENTS
We thank all medical staff fighting against COVID‐19 and all the colleagues involved in this review.
Sarkar M, Madabhavi IV, Quy PN, Govindagoudar MB. COVID‐19 and coagulopathy. Clin Respir J. 2021;15(12):1259-1274. doi: 10.1111/crj.13438
DATA AVAILABILITY STATEMENT
All data are included in the manuscript.
REFERENCES
- 1. Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270‐273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565‐574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hoffmann M, Kleine‐Weber H, Schroeder S, et al. SARS‐CoV‐2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181(2):271‐280.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hamming I, Timens W, Bulthuis ML, Lely AT, Navis GJ, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203(2):631‐637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Li MY, Li L, Zhang Y, Wang XS. Expression of the SARS‐CoV‐2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis Poverty. 2020;9(1):1‐7, 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727‐733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gupta N, Zhao YY, Evans CE. The stimulation of thrombosis by hypoxia. Thromb Res. 2019;181:77‐83. [DOI] [PubMed] [Google Scholar]
- 8. Joly BS, Siguret V, Veyradier A. Understanding pathophysiology of hemostasis disorders in critically ill patients with COVID‐19. Intensive Care Med. 2020. Aug;46(8):1603‐1606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pober JS, Sessa WC. Evolving functions of endothelial cells in inflammation. Nat Rev Immunol. 2007. Oct;7(10):803‐815. [DOI] [PubMed] [Google Scholar]
- 10. Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID‐19. Lancet. 2020. May 2;395(10234):1417‐1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ackermann M, Verleden SE, Kuehnel M, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in COVID‐19. N Engl J Med. 2020;383(2):120‐128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Goshua G, Pine AB, Meizlish ML, et al. Endotheliopathy in COVID‐19‐associated coagulopathy: evidence from a single‐centre, cross‐sectional study. Lancet Haematol. 2020. Aug;7(8):e575‐e582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Escher R, Breakey N, Lämmle B. Severe COVID‐19 infection associated with endothelial activation. Thromb Res. 2020;190:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lenting PJ, Christophe OD, Denis CV. von Willebrand factor biosynthesis, secretion, and clearance: connecting the far ends. Blood. 2015;125(13):2019‐2028. [DOI] [PubMed] [Google Scholar]
- 15. O'Sullivan JM, Gonagle DM, Ward SE, Preston RJS, O'Donnell JS. Endothelial cells orchestrate COVID‐19 coagulopathy. Lancet Haematol. 2020;7(8):e553‐e555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Starke RD, Ferraro F, Paschalaki KE, et al. Endothelial von Willebrand factor regulates angiogenesis. Blood. 2011;117(3):1071‐1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sugiyama MG, Gamage A, Zyla R, et al. Influenza virus infection induces platelet‐endothelial adhesion which contributes to lung injury. J Virol. 2015. Dec 4;90(4):1812‐1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China Lancet. 2020;395(10223):497‐506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Thachil J. What do monitoring platelet counts in COVID‐19 teach us? J Thromb Haemost. 2020. Aug;18(8):2071‐2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lippi G, Plebani M, Michael HB. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID‐19) infections: a meta‐analysis. Clin Chim Acta. 2020. Mar 13;506:145‐148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Manne BK, Denorme F, Middleton EA, et al. Platelet gene expression and function in patients with COVID‐19. Blood. 2020;136(11):1317‐1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gris JC, Perez‐Martin A, Quéré I, Sotto A. COVID‐19 associated coagulopathy: the crowning glory of thrombo‐inflammation concept. Anaesth Crit Care Pain Med. 2020. Jun;39(3):381‐382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Magro C, Mulvey JJ, Berlin D, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID‐19 infection: a report of five cases. Transl Res. 2020;220:1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zhou Y, Lu K, Pfefferle S, et al. A single asparagine‐linked glycosylation site of the severe acute respiratory syndrome coronavirus spike glycoprotein facilitates inhibition by mannose binding lectin through multiple mechanisms. J Virol. 2010;84(17):8753‐8764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Vaduganathan M, Vardeny O, Michel T, McMurray JJV, Pfeffer MA, Solomon SD. Renin‐angiotensin‐aldosterone system inhibitors in patients with COVID‐19. N Engl J Med. 2020;382(17):1653‐1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Keragala CB, Draxler DF, McQuilten ZK, Medcalf RL. Haemostasis and innate immunity—a complementary relationship: a review of the intricate relationship between coagulation and complement pathways. Br J Haematol. 2018;180(6):782‐798. [DOI] [PubMed] [Google Scholar]
- 27. Diurno F, Numis FG, Porta G, et al. Eculizumab treatment in patients with COVID‐19: preliminary results from real life ASL Napoli 2 Nord experience. Eur Rev Med Pharmacol Sci. 2020;24(7):4040‐4047. [DOI] [PubMed] [Google Scholar]
- 28. Kaplan MJ, Radic M. Neutrophil extracellular traps: double‐edged swords of innate immunity. J Immunol. 2012;189(6):2689‐2695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Brill A, Fuchs TA, Savchenko A, et al. Neutrophil extracellular traps promote deep vein thrombosis in mice. J Thromb Haemost. 2011;10:136‐144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Fuchs TA, Brill A, Duerschmied D, et al. Extracellular DNA traps promote thrombosis. Proc Natl Acad Sci U S A. 2010;107(36):15880‐15885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Massberg S, Grahl L, von Bruehl ML, et al. Reciprocal coupling of coagulation and innate immunity via neutrophil serine proteases. Nat Med. 2010. Aug;16(8):887‐896. [DOI] [PubMed] [Google Scholar]
- 32. Zuo Y, Yalavarthi S, Shi H, et al. Neutrophil extracellular traps in COVID‐19. JCI Insight. 2020. Jun 4;5(11):e138999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Maier CL, Truong AD, Auld SC, Polly DM, Tanksley CL, Duncan A. COVID‐19‐associated hyperviscosity: a link between inflammation and thrombophilia? Lancet. 2020;395(10239):1758‐1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gertz M, Kyle R. Hyperviscosity syndrome. J Intensive Care Med. 1995;10(3):128‐141. [DOI] [PubMed] [Google Scholar]
- 35. Weiss E, Roux O, Moyer JD, et al. Fibrinolysis resistance: a potential mechanism underlying COVID‐19 coagulopathy. Thromb Haemost. 2020. Sep;120(9):1343‐1345. [DOI] [PubMed] [Google Scholar]
- 36. Schramm W, Seitz R, Gürtler L. COVID‐19‐associated coagulopathy—hypothesis: are children protected due to enhanced thrombin inhibition by higher α2‐macroglobulin (α2‐M)? J Thromb Haemost. 2020;18(9):2416‐2418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ganrot PO, Schersten B. Serum α2‐macroglobulin concentration and its variation with age and sex. Clin Chim Acta. 1967;15(1):113‐120. [Google Scholar]
- 38. McGonagle D, Sharif K, O'Regan A, Bridgewood C. The role of cytokines including interleukin‐6 in COVID‐19 induced pneumonia and macrophage activation syndrome‐like disease. Autoimmun Rev. 2020;19(6):102537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Vadasz Z, Brenner B, Toubi E. Immune‐mediated coagulopathy in COVID‐19 infection. Semin Thromb Hemost. 2020;46(7):838‐840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Campbell CM, Kahwash R. Will complement inhibition be the new target in treating COVID‐19 related systemic thrombosis? Circulation. 2020. Jun 2;141(22):1739‐1741. [DOI] [PubMed] [Google Scholar]
- 41. Iba T, Levy JH, Connors JM, Warkentin TE, Thachil J, Levi M. The unique characteristics of COVID‐19 coagulopathy. Crit Care. 2020. Jun 18;24(1):1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Schouwers SM, Delanghe JR, Devreese KM. Lupus anticoagulant (LAC) testing in patients with inflammatory status: does C‐reactive protein interfere with LAC test results? Thromb Res. 2010;125(1):102‐104. [DOI] [PubMed] [Google Scholar]
- 43. Connell NT, Battinelli EM, Connors JM. Coagulopathy of COVID‐19 and antiphospholipid antibodies. J Thromb Haemost. 2020:28;1‐2. 10.1111/jth.14893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Stefanini GG, Montorfano M, Trabattoni D, et al. ST‐elevation myocardial infarction in patients with COVID‐19: clinical and angiographic outcomes. Circulation. 2020;141(25):2113‐2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Oxley TJ, Mocco J, Majidi S, et al. Large‐vessel stroke as a presenting feature of COVID‐19 in the young. N Engl J Med. 2020;382(20):e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Klok F, Kruip M, van der Meer N, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID‐19. Thromb Res. 2020. Jul;191:145‐147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hunt BJ, Levi M. Re The source of elevated plasma D‐dimer levels in COVID‐19 infection. Br J Haematol. 2020;190:e133‐e134. 10.1111/bjh.16907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Béné MC, Castoldi G, Knapp W, et al. CD87 (urokinase‐type plasminogen activator receptor), function and pathology in hematological disorders: a review. Leukemia. 2004;18(3):394‐400. [DOI] [PubMed] [Google Scholar]
- 49. Park MD. Macrophages: a Trojan horse in COVID‐19? Nat Rev Immunol. 2020;20(6):351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708‐1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: a retrospective cohort study. The Lancet. 2020;395(10229):1054‐1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18(4):844‐847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Petrilli CM, Jones SA, Yang J, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. Bmj. 2020;369:m1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Llitjos JF, Leclerc M, Chochois C, et al. High incidence of venous thromboembolic events in anticoagulated severe COVID‐19 patients. J Thromb Haemost. 2020;18(7):1743‐1746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Helms J, Tacquard C, Severac F, et al. CRICS TRIGGERSEP Group (Clinical Research in Intensive Care and Sepsis Trial Group for Global Evaluation and Research in Sepsis). High risk of thrombosis in patients with severe SARS‐CoV‐2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020. Jun;46(6):1089‐1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Al‐Samkari H, Karp Leaf RS, Dzik WH, et al. COVID‐19 and coagulation: bleeding and thrombotic manifestations of SARS‐CoV‐2 infection. Blood. 2020;136(4):489‐500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Beyrouti R, Adams ME, Benjamin L, et al. Characteristics of ischaemic stroke associated with COVID‐19. J Neurol Neurosurg Psychiatry. 2020. Aug;91(8):889‐891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Annie F, Bates MC, Nanjundappa A, Bhatt DL, Alkhouli M. Prevalence and outcomes of acute ischemic stroke among patients ≤50 years of age with laboratory confirmed COVID‐19 infection. Am J Cardiol. 2020. Sep 1;130:169‐170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Wijeratne T, Sales C, Karimi L, Crewther SG. Acute ischemic stroke in COVID‐19: a case‐based systematic review. Front Neurol. 2020;11:1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Spence JD, de Freitas GR, Pettigrew LC, et al. Mechanisms of stroke in COVID‐19. Cerebrovasc Dis. 2020;49(4):451‐458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Zhang Y, Xiao M, Zhang S, et al. Coagulopathy and antiphospholipid antibodies in patients with COVID‐19. N Engl J Med. 2020;382(17):e38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Bowles L, Platton S, Yartey N, et al. Lupus anticoagulant and abnormal coagulation tests in patients with COVID‐19. N Engl J Med. 2020. Jul 16;383(3):288‐290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Eeles GH, Sevitt S. Microthrombosis in injured and burned patients. J Pathol Bacteriol. 1967;93(1):275‐293. [DOI] [PubMed] [Google Scholar]
- 64. Tomashefski JF Jr, Davies P, Boggis C, Greene R, Zapol WM, Reid LM. The pulmonary vascular lesions of the adult respiratory distress syndrome. Am J Pathol. 1983;112(1):112‐126. [PMC free article] [PubMed] [Google Scholar]
- 65. Fox SE, Akmatbekov A, Harbert JL, Li G, Quincy Brown J, Vander Heide RS. Pulmonary and cardiac pathology in African American patients with COVID‐19: an autopsy series from New Orleans. Lancet Respir Med. 2020;8(7):681‐686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Menter T, Haslbauer JD, Nienhold R, et al. Post‐mortem examination of COVID19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings of lungs and other organs suggesting vascular dysfunction. Histopathology. 2020. Aug;77(2):198‐209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Delabranche X, Helms J, Meziani F. Immunohaemostasis: a new view on haemostasis during sepsis. Ann Intensive Care. 2017;7(1):117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Conti P, Ronconi G, Caraffa A, et al. Induction of pro‐inflammatory cytokines (IL‐1 and IL‐6) and lung inflammation by coronavirus‐19 (COVI‐19 or SARS‐CoV‐2): anti‐inflammatory strategies. J Biol Regul Homeost Agents. 2020;34(2):327‐331. [DOI] [PubMed] [Google Scholar]
- 69. Thachil J, Tang N, Gando S, et al. ISTH interim guidance on recognition and management of coagulopathy in COVID‐19. J Thromb Haemost. 2020;18(5):1023‐1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Ganter MT, Hofer CK. Coagulation monitoring: current techniques and clinical use of viscoelastic point‐of‐care coagulation devices. Anesth Analg. 2008. May;106(5):1366‐1375. [DOI] [PubMed] [Google Scholar]
- 71. Andersen MG, Hvans CL, Tonnesen E, Hvas AM. Thromboelastometry as a supplementary tool for evaluation of haemostasis in severe sepsis and septic shock. Acta Anaesthesiol Scand. 2014;58(5):525‐533. [DOI] [PubMed] [Google Scholar]
- 72. Pavoni V, Gianesello L, Pazzi M, Stera C, Meconi T, Frigieri FC. Evaluation of coagulation function by rotation thromboelastometry in critically ill patients with severe COVID‐19 pneumonia. J Thromb Thrombolysis. 2020. Aug;50(2):281‐286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Panigada M, Bottino N, Tagliabue P, et al. Hypercoagulability of COVID‐19 patients in intensive care unit. A report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost. 2020. Jul;18(7):1738‐1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18(5):1094‐1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Yin S, Huang M, Li D, et al. Difference of coagulation features between severe pneumonia induced by SARS‐CoV2 and non‐SARS‐CoV2. J Thromb Thrombolysis. 2020. Apr;3:1‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Paranjpe I, Fuster V, Lala A, et al. Association of treatment dose anticoagulation with in‐hospital survival among hospitalized patients with COVID‐19. J am Coll Cardiol. 2020. Jul 7;76(1):122‐124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Levine MN, Hirsh J, Gent M, et al. A randomized trial comparing activated thromboplastin time with heparin assay in patients with acute venous thromboembolism requiring large daily doses of heparin. Arch Intern Med. 1994. Jan 10;154(1):49‐56. [PubMed] [Google Scholar]
- 78. Iba T, Nisio MD, Levy JH, Kitamura N, Thachil J. New criteria for sepsis‐induced coagulopathy (SIC) following the revised sepsis definition: a retrospective analysis of a nationwide survey. BMJ Open. 2017;7(9):e017046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Hippensteel JA, LaRiviere WB, Colbert JF, Langouët‐Astrié CJ, Schmidt EP. Heparin as a therapy for COVID‐19: current evidence and future possibilities. Am J Physiol Lung Cell Mol Physiol. 2020. Aug 1;319(2):L211‐L217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Milewska A, Nowak P, Owczarek K, et al. Entry of human coronavirus NL63 into the cell. J Virol. 2018;92:e01933‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Cuker A, Tseng EK, Nieuwlaat R, et al. American Society of Hematology 2021 guidelines on the use of anticoagulation for thromboprophylaxis in patients with COVID‐19. Blood Adv. 2021. Feb 9;5(3):872‐888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Nadkarni GN, Lala A, Bagiella E, et al. Anticoagulation, bleeding, mortality, and pathology in hospitalized patients with COVID‐19. J am Coll Cardiol. 2020;76(16):1815‐1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Alhazzani W, Lim W, Jaeschke RZ, Murad MH, Cade J, Cook DJ. Heparin thromboprophylaxis in medical‐surgical critically ill patients: a systematic review and meta‐analysis of randomized trials. Crit Care Med. 2013. Sep;41(9):2088‐2098. [DOI] [PubMed] [Google Scholar]
- 84. Bikdeli B, Madhavan MV, Jimenez D, et al. COVID‐19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow‐up: JACC state‐of‐the‐art review. J am Coll Cardiol. 2020. Jun 16;75(23):2950‐2973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Aryal MR, Gosain R, Donato A, et al. Venous thromboembolism in COVID‐19: towards an ideal approach to thromboprophylaxis, screening, and treatment. Curr Cardiol Rep. 2020;22(7):52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Sadeghipour P, Talasaz AH, Rashidi F, et al. Effect of intermediate‐dose vs standard‐dose prophylactic anticoagulation on thrombotic events, extracorporeal membrane oxygenation treatment, or mortality among patients with COVID‐19 admitted to the intensive care unit: the INSPIRATION randomized clinical trial. Jama. 2021. Apr 27;325(16):1620‐1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Therapeutic Anticoagulation in Critically Ill Patients with COVID‐19—Preliminary Report. The REMAP‐CAP, ACTIV‐4a, ATTACC Investigators. doi: https://www.medrxiv.org/content/10.1101/2021.03.10.21252749v1.full.pdf (pre‐print) (accessed on 20th June, 2021)
- 88. https://www.uptodate.com/contents/covid-19-hypercoagulability (accessed on 20th June, 2021)
- 89. https://www.hematology.org/covid-19/covid-19-and-vte-anticoagulation (accessed on 20th June, 2021)
- 90. https://www.massgeneral.org/assets/MGH/pdf/news/coronavirus/guidance-from-mass-general-hematology.pdf (accessed on 20th June, 2021)
- 91. Efird LE, Kockler DR. Fondaparinux for thromboembolic treatment and prophylaxis of heparin‐induced thrombocytopenia. Ann Pharmacother. 2006;40(7–8):1383‐1387. [DOI] [PubMed] [Google Scholar]
- 92. Coppola A, Lombardi M, Tassoni MI, et al. COVID‐19, thromboembolic risk and thromboprophylaxis: learning lessons from the bedside, awaiting evidence. Blood Transfus. 2020. May;18(3):226‐229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Barnes GD, Burnett A, Allen A, et al. Thromboembolism and anticoagulant therapy during the COVID‐19 pandemic: interim clinical guidance from the anticoagulation forum. J Thromb Thrombolysis. 2020. Jul;50(1):72‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Holbrook A, Schulman S, Witt DM, et al. Evidence‐based management of anticoagulant therapy: antithrombotic therapy and prevention of thrombosis, 9th edn: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e152S‐e184S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Gervaise A, Bouzad C, Peroux E, Helissey C. Acute pulmonary embolism in non‐hospitalized COVID‐19 patients referred to CTPA by emergency department. Eur Radiol. 2020;30(11):6170‐6177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Bajaj NS, Vaduganathan M, Qamar A, et al. Extended prophylaxis for venous thromboembolism after hospitalization for medical illness: a trial sequential and cumulative meta‐analysis. PLoS Med. 2019. Apr 29;16(4):e1002797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Chiasakul T, Evans CR, Spyropoulos AC, Raskob G, Crowther M, Cuker A. Extended vs. standard‐duration thromboprophylaxis in acutely ill medical patients: a systematic review and meta‐analysis. Thromb Res. 2019. Dec;184:58‐61. [DOI] [PubMed] [Google Scholar]
- 98. Spyropoulos AC, Ageno W, Albers GW, et al. Post‐discharge prophylaxis with rivaroxaban reduces fatal and major thromboembolic events in medically ill patients. J am Coll Cardiol. 2020;75(25):3140‐3147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Roberts LN, Whyte MB, Georgiou L, et al. Postdischarge venous thromboembolism following hospital admission with COVID‐19. Blood. 2020. Sep 10;136(11):1347‐1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Spyropoulos AC, Lipardi C, Xu J, et al. Modified IMPROVE VTE risk score and elevated D‐dimer identify a high venous thromboembolism risk in acutely ill medical population for extended thromboprophylaxis. TH Open. 2020;4(1):e59‐e65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Cohen AT, Harrington RA, Goldhaber SZ, et al. Extended thromboprophylaxis with betrixaban in acutely ill medical patients. N Engl J Med. 2016;375(6):534‐544. [DOI] [PubMed] [Google Scholar]
- 102. Raskob GE, Spyropoulos AC, Zrubek J, et al. The MARINER trial of rivaroxaban after hospital discharge for medical patients at high risk of VTE. Design, rationale, and clinical implications. Thromb‐Haemost. 2016;115(06):1240‐1248. [DOI] [PubMed] [Google Scholar]
- 103. Cohen AT, Spiro TE, Büller HR, et al. Rivaroxaban for thromboprophylaxis in acutely ill medical patients. N Engl J Med. 2013. Feb 7;368(6):513‐523. [DOI] [PubMed] [Google Scholar]
- 104. Cohen AT, Harrington RA, Goldhaber SZ, et al. Extended thromboprophylaxis with betrixaban in acutely Ill medical patients. N Engl J Med. 2016. Aug 11;375(6):534‐544. [DOI] [PubMed] [Google Scholar]
- 105. Canonico ME, Siciliano R, Scudiero F, Sanna GD, Parodi G. The tug‐of‐war between coagulopathy and anticoagulant agents in patients with COVID‐19. Eur Heart J Cardiovasc Pharmacother. 2020. Jul 1;6(4):262‐264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Liverpool Drug Interactions Group . University of Liverpool (Charts updated 9 April 2020). https://www.covid19-druginteractions.org
- 107. Wang J, Hajizadeh N, Moore EE, et al. Tissue plasminogen activator (tPA) treatment for COVID‐19 associated acute respiratory distress syndrome (ARDS): a case series. J Thromb Haemost. 2020;18(7):1752‐1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. White D, MacDonald S, Bull T, et al. Heparin resistance in COVID‐19 patients in the intensive care unit. J Thromb Thrombolysis. 2020;50(2):287‐291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Dutt T, Simcox D, Downey C, et al. Thromboprophylaxis in COVID‐19: anti‐FXa‐the missing factor? Am J Respir Crit Care Med. 2020;202(3):455‐457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Adie SK, Farina N. Impact of COVID‐19 on monitoring of therapeutic unfractionated heparin. J Thromb Thrombolysis. 2021. Apr;51(3):827‐829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Neumann I, Izcovich A, Zhang Y, et al. DOACs vs LMWHs in hospitalized medical patients: a systematic review and meta‐analysis that informed 2018 ASH guidelines. Blood Adv. 2020;4(7):1512‐1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Moores LK, Tritschler T, Brosnahan S, et al. Prevention, diagnosis, and treatment of VTE in patients with coronavirus disease 2019: CHEST guideline and expert panel report. Chest. 2020;158(3):1143‐1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Bikdeli B, Madhavan MV, Jimenez D, et al. COVID‐19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow‐up: JACC state‐of‐the‐art review. J am Coll Cardiol. 2020;75(23):2950‐2973. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are included in the manuscript.


