Abstract
Type‐I interferons (IFNs) mediate antiviral activity and have emerged as important immune mediators during coronavirus disease 19 (COVID‐19). Several lines of evidence suggest that impaired type‐I IFN signaling may predispose to severe COVID‐19. However, the pathophysiologic mechanisms that contribute to illness severity remain unclear. In this study, our goal was to gain insight into how type‐I IFNs influence outcomes in patients with COVID‐19. To achieve this goal, we compared clinical outcomes between 26 patients with neutralizing type‐I IFN autoantibodies (AAbs) and 192 patients without AAbs who were hospitalized for COVID‐19 at three Italian hospitals. The presence of circulating AAbs to type‐I IFNs was associated with an increased risk of admission to the intensive care unit and a delayed time to viral clearance. However, survival was not adversely affected by the presence of type‐I IFN AAbs. Our findings provide further support for the role of type‐I IFN AAbs in impairing host antiviral defense and promoting the development of critical COVID‐19 pneumonia in severe acute respiratory syndrome coronavirus 2‐infected individuals.
Keywords: Immunological deficiency syndromes, infectious diseases, innate immunity, translational immunology, viral infection
Neutralizing autoantibodies to type‐I interferons predispose people to severe coronavirus disease 19 (COVID‐19). These autoantibodies are associated with admission to the intensive care unit and delayed viral clearance. However, in our study, they were not associated with increased mortality.
INTRODUCTION
Type‐I interferons (IFNs) mediate antiviral immunity and exert other pleiotropic immune effects. Impaired type‐I IFN responses have been identified in patients with severe coronavirus disease 19 (COVID‐19), suggesting that type‐I IFNs play a critical role against severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2). 1 , 2
We recently reported 3 that neutralizing autoantibodies (AAbs) against IFNα and/or IFNω were identified in at least 10% of critically ill COVID‐19 patients but not in mildly symptomatic patients. These AAbs abolish type‐I IFN signaling, circulate prior to SARS‐CoV‐2 infection, as evidenced in patients with incontinentia pigmenti 4 and autoimmune polyendocrinopathy‐candidiasis‐ectodermal dystrophy/autoimmune polyglandular syndrome type‐1, 5 and persist throughout the course of illness. 3 The presence of neutralizing AAbs against type‐I IFNs in a subset of patients with life‐threatening COVID‐19 pneumonia has been replicated by several groups. 2 , 6 , 7
Our original report did not examine the detailed clinical course of COVID‐19 in patients harboring neutralizing AAbs against type‐I IFNs beyond severity of SARS‐CoV‐2 infection. 3 Furthermore, that study focused on patients with life‐threatening infection, excluding less severe cases of COVID‐19 who nonetheless required hospitalization. In the present study, we sought to determine the influence of AAbs to type‐I IFNs on clinical outcomes in patients hospitalized for COVID‐19.
RESULTS
We included 218 patients with COVID‐19 in this study. Severity of illness was classified as critical in 135 patients (61.9%), severe in 44 (17.9%) and mild/moderate in 39 (20.2%). Of note, the 135 patients with critical COVID‐19 were included in our previous report. 3 Neutralizing AAbs to type‐I IFNs were detected in 26 patients (11.9%), most of whom (17 patients) harbored AAbs to both IFNα and IFNω (Supplementary figure 1). AAbs to IFNβ were detected in a single patient who also had AAbs to both IFNα and IFNω. Clinical characteristics were compared between AAb‐positive (AAb+) and AAb‐negative (AAb–) patients (Supplementary table 1). The presence of AAbs was associated with male sex and severity of illness, whereas age and medical comorbidities did not significantly differ between the two groups in this cohort. The incidence of thrombotic complications was comparable between AAb+ and AAb− patients (Supplementary table 1). The proportion of patients who received anticoagulation or immunomodulatory medications such as corticosteroids and tocilizumab was not significantly different between AAb+ and AAb− patients (Supplementary table 1). AAb+ patients were significantly more likely to require invasive mechanical ventilation compared with AAb− patients (65.4% versus 29.9%, respectively; P = 0.001). Similarly, the proportion of patients who developed bacterial infections during the course of hospitalization was significantly greater in AAb+ (30.8%) versus AAb− (5.5%) patients (P < 0.001; Supplementary table 1).
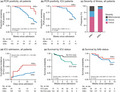
Sufficient information to calculate the time to viral clearance was available in 119 patients, including 17 AAb+ patients and 102 AAb− patients. The median number of samples per patient did not differ between AAb+ and AAb− patients [median (interquartile range) 4 (3–5) versus 3 (2–4), respectively, P = 0.09]. The presence of neutralizing AAbs to type‐I IFNs was associated with a markedly delayed time to viral clearance of SARS‐CoV‐2, as modeled by Cox proportional hazards [hazard ratio, 0.24; 95% confidence interval, 0.07–0.77; log‐rank P = 0.003; Figure 1a]. The mean time to viral clearance in the overall cohort was 15 days. By contrast, the mean time to viral clearance was 24 days in AAb+ patients. This finding was particularly striking in patients admitted to the intensive care unit (ICU) (Figure 1b), with 100% of AAb‐positive ICU patients remaining PCR positive 4 weeks after hospital admission. In addition, AAb positivity was associated with more severe infection (Figure 1c) and an increased risk for ICU admission during the first 15 days of hospitalization (Figure 1d; hazard ratio, 2.59; 95% confidence interval, 1.43–4.69; P = 0.004). Notably, although ICU admission was associated with greater mortality in the entire cohort of 218 patients (Figure 1e; hazard ratio, 2.35; 95% confidence interval, 1.14–4.85; P = 0.02), the presence of AAbs was not associated with patient survival (Figure 1f; hazard ratio, 0.64; 95% confidence interval, 0.22–1.81; P = 0.37), a finding that was consistent regardless of patient sex or ICU status (Supplementary figure 2).
Figure 1.

Severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) clearance, admission to the intensive care unit (ICU) and survival in coronavirus disease 19 (COVID‐19) patients with versus without autoantibodies (AAbs) to type‐I interferons (IFNs). (a) Proportion of all patients testing positive for SARS‐CoV‐2 by PCR nasal swab test during the course of illness in patients with (n = 17) versus without (n = 102) AAbs to type‐I IFNs. (b) Proportion of patients testing positive for SARS‐CoV‐2 by PCR nasal swab test during the course of illness in a subset of patients who required ICU care with (n = 11) versus without (n = 50) AAbs to type‐I IFNs. (c) Severity of illness in patients with (n = 26) versus without (n = 192) AAbs to type‐I IFNs. P = 0.012 by a Chi‐squared test. (d) Cumulative incidence of ICU admission during the first 2 weeks of hospitalization in patients with (n = 25, including 3 admitted to ICU within 24 h of hospitalization) versus without (n = 190, including 16 admitted to ICU within 24 h of hospitalization) AAbs to type‐I IFNs. Data on the timing of ICU admission relative to hospital admission were not available for three patients. (e) Kaplan–Meier plot displaying survival during the 10‐week period following hospital admission in patients admitted to the ICU (n = 75) versus those not admitted to the ICU (n = 143). (f) Kaplan–Meier plot displaying survival during the 10‐week period following hospital admission in patients with (n = 26) versus without (n = 192) AAbs to type‐I IFNs. “No. at risk” in panels a–c refers to the number of patients in each group [AAb positive (AAb+) or AAb negative (AAb−)] who were alive at the specified time point. CI, confidence interval.
DISCUSSION
Previous studies have shown that patients with AAbs against type‐I IFNs have a predilection for developing life‐threatening COVID‐19. 3 , 6 , 7 In addition, most patients with autoimmune polyendocrinopathy‐candidiasis‐ectodermal dystrophy/autoimmune polyglandular syndrome type‐1, 8 who carry neutralizing AAbs against type‐I IFNs, are at risk for severe hypoxemic COVID‐19 pneumonia. 5 , 9 Initial reports of exogenous administration of IFNβ or plasma exchange in these patients, or IFNα2 in those with inborn errors of type‐I IFN immunity, during the early nonhypoxemic phase of COVID‐19 have provided promising results. 4 , 5 , 10 , 11 The identification of type‐I IFN AAbs in a sizable proportion of patients with severe COVID‐19 in conjunction with the observation that the overwhelming majority of AAbs to type‐I IFNs in patients with COVID‐19 are directed against IFNα and/or IFNω but not IFNβ provide a compelling rationale for the preferential investigation of IFNβ over IFNα in future clinical studies. 2 , 3 , 4 , 5 , 6 , 7
While prior studies have established that patients with defects in the type‐I IFN signaling pathway are predisposed to severe COVID‐19, 1 , 3 the pathophysiologic mechanisms that contribute to this enhanced illness severity remain unclear. We now show that patients with type‐I IFN AAbs have delayed viral clearance contributing to the greater likelihood of developing critical COVID‐19 pneumonia requiring ICU admission and mechanical ventilation. However, despite their increased morbidity, these patients surprisingly did not have an increased risk of death in our cohort. Several factors may account for the lack of association between survival and the presence of neutralizing anti‐type‐I IFN antibodies. In particular, coordination between humoral and cellular adaptive immune responses has been shown to play a critical role in determining COVID‐19 severity and outcome. 12 Moreover, while a lack of type‐I IFN signaling during early infection is clearly detrimental for SARS‐CoV‐2 containment, type‐I IFNs may contribute to secondary inflammation during the late hyperinflammatory stage of COVID‐19. Furthermore, in addition to immunologic factors, a variety of clinical and demographic characteristics, most notably patient age and the presence of comorbid conditions, play a critical role in influencing clinical outcomes. However, we did not detect differences in age or the prevalence of comorbid conditions in patients with versus without AAbs. Importantly, this does not rule out the possibility that one or more unmeasured confounding factors may explain the comparable mortality between groups. More studies will be needed to verify these results and to examine whether neutralizing AAbs against type‐I IFNs are associated with a greater frequency of bacterial infections in hospitalized COVID‐19 patients as observed in our cohort.
In summary, we show that type‐I IFN AAbs are associated with delayed SARS‐CoV‐2 clearance, ICU admission, mechanical ventilation and critical COVID‐19 pneumonia but do not appear to independently affect survival. Early administration of IFNβ in patients harboring type‐I IFN AAbs may help hasten SARS‐CoV‐2 clearance and avert the development of critical COVID‐19 pneumonia.
METHODS
All patients included in this study were adults (age ≥18 years) who were admitted with laboratory‐confirmed COVID‐19 to one of three Italian hospitals (ASST Spedali Civili, Brescia; Ospedale San Gerardo, Monza and Ospedale S. Matteo, Pavia) between February and May 2020. 13 The maximum severity of COVID‐19 during hospitalization was determined for each patient using a previously described scoring system. 13 Neutralizing AAb characterization was performed as previously described. 3 Patients were classified as AAb+ if neutralizing AAbs to one or more type‐I IFNs (IFNα, IFNβ and IFNω) were detected in peripheral blood, whereas individuals who lacked such antibodies were considered AAb−. Time to viral clearance was defined as the interval from hospitalization to the first date on which nasopharyngeal PCR testing was negative without a subsequent positive test. Patients whose most recent test was positive were censored on that date. All PCR tests were performed in the context of clinical care without prespecified requirements for testing frequency or the number of tests per patient. All analyses involving viral clearance were limited to patients whose medical records included the date of sample collection and results for all PCR tests. Mortality was defined as death within 10 weeks of hospital admission. Patients with unknown status at this time point were censored on the date the patient was last known to be alive. To focus on COVID‐19‐related indications for ICU admission rather than nosocomial factors, time to ICU admission was modeled during the first 15 days of hospitalization. Continuous variables were summarized by median and interquartile ranges and groups were compared using a Mann–Whitney U‐test. Categorical variables were compared by the Fisher exact test (when the number of individuals in any group was < 5) or a Chi‐squared test. Patient survival, time to viral clearance and time to ICU admission since hospital admission were modeled using univariate Cox proportional hazards regression; groups were compared using the log‐rank test. For all analyses, statistical significance was defined as P < 0.05. Data were analyzed using R version 4.0.4 (R Foundation, Vienna, Austria).
CONFLICT OF INTEREST
The authors have no conflicts of interest to disclose.
AUTHOR CONTRIBUTIONS
Michael S Abers: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Software; Visualization; Writing‐original draft; Writing‐review & editing. Lindsey B Rosen: Data curation; Investigation. Ottavia M Delmonte: Data curation; Resources. Elana Shaw: Data curation; Investigation. Paul Bastard: Data curation; Investigation. Luisa Imberti: Data curation; Funding acquisition. Virginia Quaresima: Data curation; Funding acquisition. Andrea Biondi: Data curation; Funding acquisition. Paolo Bonfanti: Data curation; Funding acquisition. Riccardo Castagnoli: Data curation; Funding acquisition; Writing‐review & editing. Jean‐Laurent Casanova: Funding acquisition; Resources; Writing‐review & editing. Helen C Su: Resources; Writing‐review & editing. Luigi D Notarangelo: Funding acquisition; Project administration; Resources. Steven M Holland: Conceptualization; Funding acquisition; Project administration; Resources. Michail S Lionakis: Conceptualization; Funding acquisition; Investigation; Supervision; Writing‐original draft; Writing‐review & editing.
DATA AVAILABILITY STATEMENT
Data are available upon request.
Supporting information
Supplementary figures 1 & 2 and Supplementary table 1
ACKNOWLEDGMENTS
This work was supported by the Division of Intramural Research of the NIAID, NIH. The Laboratory of Human Genetics of Infectious Diseases is supported by the Howard Hughes Medical Institute, the Rockefeller University, the St. Giles Foundation, the National Institutes of Health (NIH) (R01AI088364), the National Center for Advancing Translational Sciences (NCATS), NIH Clinical and Translational Science Award (CTSA) program (UL1 TR001866), a Fast Grant from Emergent Ventures, Mercatus Center at George Mason University, the Yale Center for Mendelian Genomics and the GSP Coordinating Center funded by the National Human Genome Research Institute (NHGRI) (UM1HG006504 and U24HG008956), the French National Research Agency (ANR) under the “Investments for the Future” program (ANR‐10‐IAHU‐01), the Integrative Biology of Emerging Infectious Diseases Laboratory of Excellence (ANR‐10‐LABX‐62‐IBEID), the French Foundation for Medical Research (FRM) (EQU201903007798), the FRM and ANR GENCOVID project, ANRS‐COV05, the Square Foundation, Grandir ‐ Fonds de solidarité pour l’enfance, the SCOR Corporate Foundation for Science, Institut National de la Santé et de la Recherche Médicale (INSERM) and the University of Paris. ASST Spedali Civili di Brescia and IRB of Fondazione IRCCS Policlinico San Matteo received a grant from Regione Lombardia, Italy (project “Risposta immune in pazienti con COVID‐19 e co‐morbidità”). PB is supported by the MD‐PhD program of the Imagine Institute (with the support of the Fondation Bettencourt‐Schueller).
REFERENCES
- 1. Zhang Q, Bastard P, Liu Z, et al. Inborn errors of type I IFN immunity in patients with life‐threatening COVID‐19. Science 2020; 370: eabd4585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. van der Wijst MVS, Hartoularos GC, Bastard P, et al. Longitudinal single‐cell epitope and RNA‐seq reveals the immunological impact of type 1 interferon autoantibodies in critical COVID‐19. Sci Transl Med 2021. 10.1101/2021.03.09.434529. in press. [DOI] [Google Scholar]
- 3. Bastard P, Rosen LB, Zhang Q, et al. Autoantibodies against type I IFNs in patients with life‐threatening COVID‐19. Science 2020; 370: eabd4585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bastard P, Levy R, Henriquez S, Bodemer C, Szwebel TA, Casanova JL. Interferon‐β therapy in a patient with incontinentia pigmenti and autoantibodies against type I IFNs infected with SARS‐CoV‐2. J Clin Immunol 2021; 41: 931–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bastard P, Orlova E, Sozaeva L, et al. Preexisting autoantibodies to type I IFNs underlie critical COVID‐19 pneumonia in patients with APS‐1. J Exp Med 2021; 218: e20210554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Koning R, Bastard P, Casanova JL, et al. Autoantibodies against type I interferons are associated with multi‐organ failure in COVID‐19 patients. Intensive Care Med 2021; 47: 704–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Troya J, Bastard P, Planas‐Serra L, et al. Neutralizing autoantibodies to type I IFNs in >10% of patients with severe COVID‐19 pneumonia hospitalized in Madrid, Spain. J Clin Immunol 2021; 41: 914–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Constantine GM, Lionakis MS. Lessons from primary immunodeficiencies: autoimmune regulator and autoimmune polyendocrinopathy‐candidiasis‐ectodermal dystrophy. Immunol Rev 2019; 287: 103–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Meisel C, Akbil B, Meyer T, et al. Mild COVID‐19 despite autoantibodies against type I IFNs in autoimmune polyendocrine syndrome type 1. J Clin Invest 2021; 131: e150867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Levy R, Bastard P, Lanternier F, Lecuit M, Zhang SY, Casanova JL. IFN‐α2a therapy in two patients with inborn errors of TLR3 and IRF3 infected with SARS‐CoV‐2. J Clin Immunol 2021; 41: 26–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. de Prost N, Bastard P, Arrestier R, et al. Plasma exchange to rescue patients with autoantibodies against type I interferons and life‐threatening COVID‐19 pneumonia. J Clin Immunol 2021; 41: 536–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rydyznski Moderbacher C, Ramirez SI, Dan JM, et al. Antigen‐specific adaptive immunity to SARS‐CoV‐2 in acute COVID‐19 and associations with age and disease severity. Cell 2020; 183: 996–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Abers MS, Delmonte OM, Ricotta EE, et al. An immune‐based biomarker signature is associated with mortality in COVID‐19 patients. JCI Insight 2021; 6: e144455. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary figures 1 & 2 and Supplementary table 1
Data Availability Statement
Data are available upon request.


