Abstract
Background and purpose
Many countries worldwide, including Germany, reported that the first wave of the coronavirus disease 2019 (COVID‐19) pandemic in early 2020 influenced the care of acute ischemic stroke (AIS) patients, but data are lacking for further pandemic wave periods.
Methods
We conducted a nationwide, retrospective, cross‐sectional study of all hospitalized patients with the main diagnosis of AIS in 2019 and 2020. Primary outcomes were the number of hospitalizations for AIS, the application of stroke unit care, intravenous thrombolysis (IVT), and mechanical thrombectomy (MT), as well as the in‐hospital mortality during the different pandemic periods in 2020 compared to the corresponding periods in 2019. Secondarily, we analyzed differences in outcomes between patients with and without concurrent COVID‐19.
Results
We included 429,841 cases with AIS, of which 1268 had concurrent COVID‐19. Hospitalizations for AIS declined during both pandemic wave periods in 2020 (first wave: −10.9%, second wave: −4.6%). MT rates were consistently higher throughout 2020 compared to 2019, whereas the IVT rate dropped during the second wave period (16.0% vs. 17.0%, p < 0.001). AIS patients with concurrent COVID‐19 frequently received recanalization treatments, with an overall MT rate of 8.4% and IVT rate of 15.9%. The in‐hospital mortality was high (22.8% vs. 7.5% in noninfected AIS patients, p < 0.001).
Conclusions
These findings demonstrate a smaller decline in hospitalizations for AIS in the more severe second wave of the COVID‐19 pandemic. AIS patients with and without concurrent COVID‐19 who did seek acute care continued to receive recanalization treatments in Germany.
Keywords: COVID‐19, Germany, stroke, thrombectomy, thrombolysis
There was a substantial decline in hospitalizations for acute ischemic stroke during the two COVID‐19 pandemic waves in Germany, with a smaller reduction during the second wave of the pandemic. Acute ischemic stroke patients still frequently received acute stroke care, including recanalization treatments during the entire year of 2020, irrespective of SARS‐CoV‐2 status.

INTRODUCTION
The year 2020 was dominated by the coronavirus disease 2019 (COVID‐19) pandemic, caused by severe acute respiratory coronavirus 2 (SARS‐CoV‐2). Several neurological manifestations and complications have been reported, including acute ischemic stroke (AIS), that might be mainly caused by an inflammation‐induced prothrombotic state, but also by angiotensin‐converting enzyme‐2 receptor dysregulation or COVID‐19‐associated cardiac injury [1]. COVID‐19 in AIS patients is associated with substantially higher mortality [2, 3 and a frequent appearance of large vessel occlusions (LVOs) [4].
In addition to direct disease‐related complications, the first wave of the COVID‐19 pandemic influenced AIS care on a global level, with a strong decline in the number of AIS patient hospitalizations [5]. A similar decrease was observed for Germany during the first wave of the pandemic in spring 2020 [6]. The decline was attributed to lockdown measures and fear of attending hospitals. However, during the first pandemic wave period, the acute recanalization therapy rates remained at high levels in Germany. As the COVID‐19 pandemic is still ongoing, most countries have gone through the second wave of this pandemic, including Germany, where the second wave started in October 2020. This second wave was even worse, with a massive increase in the numbers of new infections with SARS‐CoV‐2 and a substantial rise in COVID‐19‐related deaths [7, 8. This development also unsettled the stroke community. To date, it is unknown to which extend this more severe second pandemic wave might have influenced the acute stroke care and the in‐hospital mortality of AIS patients in Germany.
Therefore, we sought to investigate and compare the number of patients hospitalized for AIS, treatment rates with intravenous thrombolysis (IVT) and mechanical thrombectomy (MT), and the in‐hospital mortality rate among AIS patients during the COVID‐19 pandemic in 2020, including both infection waves, using the full‐year nationwide data of Germany. Secondarily, we aimed to analyze differences in acute care and in‐hospital mortality of AIS patients with and without concurrent COVID‐19.
METHODS
This study followed the reporting STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guideline.
Data source and study sample
This is a German nationwide retrospective cross‐sectional study using the administrative diagnosis‐related group database (data transmission according to §21 KHEntgG and §24 para. 2 KHG; official data on file, source: Institut für das Entgeltsystem im Krankenhaus, www.g‐drg.de). In Germany, all inpatient stroke cases are encoded according to the German version of the 10th International Classification of Diseases (ICD‐10‐GM) and operating and procedure (OPS) keys issued by the Federal Institute for Drugs and Medical Devices. We included all hospitalized patients in Germany with the ICD‐10 main diagnosis I63 (ischemic stroke, n = 429,841) from 1 January 2019 to 31 December 2020. AIS patients being transferred once or multiple times from one hospital to another for acute stroke therapy and/or early rehabilitation were censored to avoid double and multiple counting cases with main diagnosis I63 (excluding "discharge key 06"). Case numbers with the main diagnosis of I63 were aggregated at the level of the 3‐digit ICD code.
Outcome
Primary outcomes were the number of AIS hospital admissions, application of acute recanalization procedures (IVT, MT), stroke unit care (SUC), and in‐hospital mortality among AIS patients during the following predefined periods of interest: 1 January to 29 February 2020 (pre‐first wave), 1 March to 31 May 2020 (first wave), 1 June to 30 September 2020 (pre‐second wave), 1 October to 31 December 2020 (second wave; Figure S1 in the online supplement). The number of AIS recanalization therapies was assessed using the corresponding OPS key for IVT (OPS code 8–020.8) and MT (OPS 8–836.80) in combination with the main diagnosis ICD I63. The following OPS codes combined with the I63 main diagnosis were analyzed to assess SUC: 8–981.x (complex treatment of acute stroke) and 8‐98b.*0/*1 (other complex treatment of acute stroke without/with teleconsultation). In‐hospital mortality was assessed using discharge key 07 (death during hospital stay).
Secondary outcomes were the acute care and in‐hospital mortality of AIS patients depending on the copresence of COVID‐19. Comorbid COVID‐19 was assessed by the concurrent coding of ICD U07.1 (laboratory‐confirmed COVID‐19).
Statistical analysis
Rates are given for categorical variables, and means and SDs for continuous variables. Absolute and relative changes in hospitalizations, treatment rates, and in‐hospital mortality rates in AIS patients between the different periods of interest are given in numbers and percent. We used the chi‐squared test for categorical variables and t‐test for continuous variables to compare each period of interest's data with the corresponding previous year period.
Additionally, differences between the periods of interest of 2020 versus 2019 were investigated using odds ratio (OR) estimates. ORs and 95% confidence intervals were calculated for the predefined outcomes under the random effects model (DerSimonian–Laird). Within and in‐between differences were analyzed with the Cochran test for heterogeneity and I 2 statistics.
The same approach was used to investigate statistical differences in outcome measures in AIS patients with concurrent COVID‐19 (AISpos) compared to noninfected AIS patients. Two‐sided p < 0.05 was set as the level of statistical significance.
RESULTS
Number of AIS patients
Before the first wave, the number of hospitalized AIS patients slightly increased by 1.0% as compared to the corresponding period in 2019. During the first and second waves of the COVID‐19 pandemic, there was a marked decline in patients hospitalized for AIS, with −10.9% during the first and −4.6% during the second pandemic wave period. In between, case numbers increased again, with only a mild decline (−1.5%) in hospitalized AIS patients compared to the previous year period (Figure 1).
FIGURE 1.
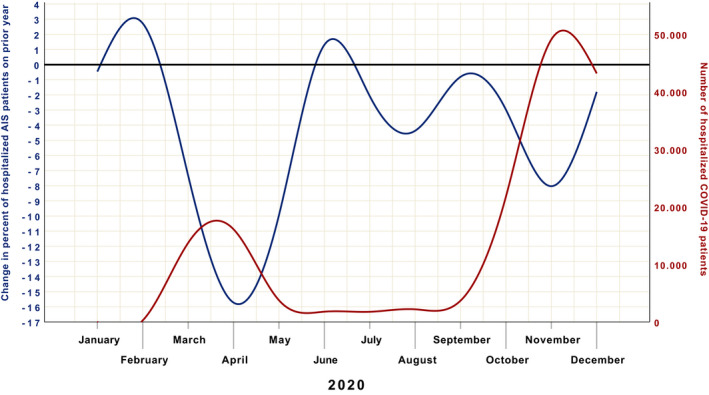
Relative change in acute ischemic stroke (AIS) patient hospitalizations during 2020. The relative change in AIS patient hospitalizations versus the prior year at a specific time point is displayed by the blue line. The cumulative number of hospitalized COVID‐19 patients at a particular time point is given by the red line
Demographics of AIS patients
The age of hospitalized AIS patients in 2020 did not differ from the previous year (Table 1). During both the first and second pandemic wave, we observed a greater decline in hospital admissions of female as compared to male AIS patients (first wave: −11.8% vs. −10.1%, second wave: −6.1% vs. −3.1%). This difference was statistically significant for the second pandemic wave (Table 1).
TABLE 1.
Characteristics of acute ischemic stroke patients
| Characteristic | Jan–Feb [pre‐first wave] | Mar–May [first wave] | Jun–Sep [pre‐second wave] | Oct–Dec [second wave] |
|---|---|---|---|---|
| 2020, n (2019) | 38,155 (37,764) | 51,554 (57,889) | 73,472 (74,616) | 47,073 (49,318) |
| Relative change, 2020 vs. 2019 | +1.0% | −10.9% | −1.5% | −4.6% |
| Age, years (2019) | 74.4 ± 9.2 (74.4 ± 9.1) | 74.3 ± 9.1 (74.4 ± 9.1) | 74.0 ± 9.1 (74.0 ± 8.9) | 74.2 ± 9.2 (74.2 ± 9.1) |
| Gender, male (2019) | 52.4% (52.4%) | 53.2% (52.8%) | 53.1% (53.2%) | 52.9% (52.1%) |
| Change in male patients, n (%) | +224 (+1.1%) | −3,096 (−10.1%) | −656 (−1.7%) | −809 (−3.1%) |
| Change in female patients, n (%) | +167 (+0.9%) | −3,239 (−11.8%) | −488 (−1.4%) | −1,436 (−6.1%) |
| IVT rate | 16.2% (16.3%) | 16.7% (16.4%) | 16.1% (16.0%) | 16.0%a (17.0%) |
| MT rate | 7.5%a (7.1%) | 8.1%a (6.8%) | 7.8%a (7.0%) | 7.9%a (7.3%) |
| SUC rate | 73.9%a (72.1%) | 76.7%a (74.2%) | 75.9%a (75.1%) | 74.1%a (76.4) |
| In‐hospital mortality rate | 7.4% (7.4%) | 8.0%a (7.5%) | 7.1% (7.0%) | 8.0% (7.8%) |
Age is given as mean ± standard deviation, and rates are given in percent. Pandemic periods in 2020 are defined as pre‐first wave: January to February, first wave: March to May, pre‐second wave: June to September, and second wave: October to December 2020. The corresponding control periods in 2019 are given in parentheses.
Abbreviations: IVT, intravenous thrombolysis; MT, mechanical thrombectomy; SUC, stroke unit care.
a p < 0.05 comparing pandemic periods to the corresponding previous year periods.
Treatment rates of AIS patients
The proportion of AIS patients who received stroke unit care was higher before the first wave (73.9% vs. 72.1%, p < 0.001), during the first wave (76.7% vs. 74.2%, p < 0.001), and after the first wave (75.9% vs. 75.1%, p < 0.001) of the pandemic as compared to the 2019 periods. During the second wave, the proportion of SUC decreased to 74.1%, which was significantly lower as compared to the corresponding period in 2019 (76.4%, p < 0.001; Table 1).
The use of IVT in AIS patients was significantly lower during the second wave (16.0% vs. 17.0%, p < 0.001) but did not differ in any other period as compared to 2019. The MT rate was consistently higher in 2020 as compared to 2019, with the most remarkable difference during the first wave of the pandemic (8.1% vs. 6.8%, p < 0.001; Table 1).
The proportion of AIS patients who died during the hospital stay was significantly higher during the first wave period in 2020 as compared to the corresponding period in 2019 (8.0% vs. 7.5%, p = 0.021), whereas there was no statistical difference in any other time period (Table 1). Log OR estimates for all outcomes are displayed in Figure 2.
FIGURE 2.

Log odds ratio of primary outcomes stratified by the different pandemic periods. Log odds ratio > 0 indicates a higher likelihood for patients during 2020. CI, confidence interval; IVT, intravenous thrombolysis; MT, mechanical thrombectomy; SUC, stroke unit care
AIS patients with concurrent COVID‐19
Throughout the year 2020, a total of 1268 hospitalized AIS patients were coded with a concurrent COVID‐19 diagnosis in Germany. The number of these AISpos patients peaked during the first and second wave of the COVID‐19 pandemic, with the highest number during the second wave period (n = 909, 1.9% of all AIS patients in this period; Table 2). The mean age of the AISpos patients was 76.6 years, and 50.1% were male. The overall SUC, IVT, and MT rates were 48.3%, 15.9%, and 8.4% compared to 75.5% (p < 0.001), 16.3% (p = 0.696), and 7.9% (p = 0.461) in AIS patients without COVID‐19. Log OR estimates are given in Figure 3.
TABLE 2.
Characteristics of AIS patients with concurrent COVID‐19 (laboratory confirmed)
| Characteristic | Jan–Feb [pre‐first wave] | Mar–May [first wave] | Jun–Sep [pre‐second wave] | Oct– Dec [second wave] |
|---|---|---|---|---|
| N | 18 | 253 | 88 | 909 |
| % of all AIS | 0.05%a | 0.5%b | 0.1%a | 1.9%b |
| Age, years | 72.1 ± 7.9 (74.4 ± 9.2) | 76.6 ± 10.8c (74.3 ± 9.1) | 75.6 ± 9.6 (74.0 ± 9.1) | 76.7 ± 10.9c (74.1 ± 9.1) |
| Sex, male | 66.7% (52.4%) | 52.6% (53.2%) | 52.3% (53.1%) | 48.8%c (52.9%) |
| IVT rate | 0a,c (16.2%) | 18.6% (16.7%) | 13.6%a (16.1%) | 15.6% (16.0%) |
| MT rate | 0a,c (7.5%) | 6.7% (8.1%) | 14.8%a (7.8%) | 8.5% (7.9%) |
| SUC rate | 0a,c (73.9%) | 52.6%c (76.8%) | 45.5%a,c (75.9%) | 48.4%c (74.6%) |
| In‐hospital mortality rate | 22.2% (7.4%) | 20.6%c (7.9%) | 10.2% (7.1%) | 24.6%c (7.7%) |
Age is given as mean ± standard deviation, and rates are shown in percent. Pandemic periods in 2020 are defined as pre‐first wave: January to February, first wave: March to May, pre‐second wave: June to September, and second wave: October to December 2020. The corresponding data of patients without concurrent COVID‐19 is given in parentheses.
Abbreviations: AIS, acute ischemic stroke; IVT, intravenous thrombolysis; MT, mechanical thrombectomy; SUC, stroke unit care.
a p <0.05 for comparing pre‐first and pre‐second wave periods.
b p <0.05 for comparing first and second wave periods.
c p <0.05 for comparing AISpos patients and AIS patients without COVID‐19 in the corresponding period.
FIGURE 3.
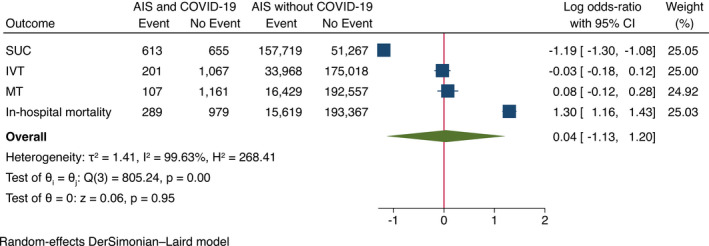
Log odds ratio of outcomes according to the presence of concurrent COVID‐19. Log odds ratio > 0 indicates a higher likelihood for AIS patients with concurrent COVID‐19. AIS, acute ischemic stroke; CI, confidence interval; IVT, intravenous thrombolysis; MT, mechanical thrombectomy; SUC, stroke unit care
We observed marked fluctuations of specialized acute stroke treatments in AISpos patients during the different pandemic periods in 2020. The first and second pandemic waves were characterized by a frequent IVT application in AISpos patients (first wave: 18.6%, second wave 15.6%, p = 0.278) without a statistically significant difference compared to AIS patients without concurrent COVID‐19 (first wave: 16.7%, second wave: 16.0%, p > 0.05 for both comparisons; Table 2). The proportion of AISpos patients receiving MT increased from the first wave (6.7%) to the second wave period (8.5%, p = 0.337). There was no significant difference in the use of MT in AISpos patients compared to AIS patients without COVID‐19 (first wave: 8.1%, second wave: 7.9%, p > 0.05 for both comparisons). The highest MT rate in AISpos patients was found during the pre‐second wave period (14.8% vs. 7.8% in noninfected AIS patients, p = 0.066).
Overall, 289 of 1268 AISpos patients (22.8%) died during hospital stay compared to 15,619 of 208,986 noninfected AIS patients (7.5%, p < 0.001). The in‐hospital mortality rate in AISpos patients was 20.6% during the first pandemic wave, 10.2% in the pre‐second wave period, and finally increased to 24.6% in the second pandemic wave period (Table 2).
DISCUSSION
There was a substantial decline in patients hospitalized for AIS in 2020, with the most pronounced decline during the first wave period of the COVID‐19 pandemic in Germany. Although the number of COVID‐19 patients was much higher during the second pandemic wave, the decrease in AIS patient hospitalizations was only approximately half of that compared to the first wave period. A significant decrease in stroke admissions has also been noted in other European countries, such as Greece. Data from three representative tertiary care hospitals showed that the decline in stroke admissions and acute coronary syndromes was almost similar between the first two pandemic wave periods, although the number of new infections with SARS‐CoV‐2 was also higher in Greece during the second wave period [9, 10. For Germany, we also found differences in German citizens’ mobility between the two wave periods. The national analysis of mobile communication data in Germany revealed an average mobility reduction of −20% during the first and only −9% during the second wave period as compared to the corresponding periods in 2019 [11]. The decline in German citizens' mobility during these periods was probably a consequence of the national lockdowns. The probable lower obedience to the second lockdown that the difference of the mobility reduction between the first and second wave period might reflect indicates a change in behavior of German citizens. During the first pandemic wave, there was a great fear of acquiring a SARS‐CoV‐2 infection during a hospital stay [12]. Although speculative, a reduction in fear of contracting a SARS‐CoV‐2 infection might attribute to the smaller decline in AIS hospitalizations during the second wave period. In this context, the routine implementation of hygiene concepts into hospital infrastructure [13] during and after the first wave of the pandemic might have reassured the German population. On the other hand, public notices like from the German Society of Neurology during the first wave of the pandemic encouraged the public to seek help in hospitals in case of medical emergencies like stroke [14]. A sensitization of the German population to such side effects may also be responsible for the lower decline in hospitalized AIS patients during the second pandemic wave.
Interestingly, there was a greater decline in female AIS patient hospitalizations, particularly during the second wave period. Preliminary data from the official German death statistic of 2020 did not demonstrate a sex difference in overall case fatalities, irrespective of age groups. Therefore, we do not assume that the observed difference is attributed to a sex difference in the population at risk for stroke due to an unequal increase of deaths among German women [15]. One possible explanation is that compared to men, much more women older than 70 years receive out‐ or inpatient nursing care in Germany (1,926,000 vs. 878,000 in 2019) [16]. Since March 2020, German nursing institutions were almost sealed off. They had to comply with strict quarantine rules due to COVID‐19‐related outbreaks in these institutions, with consequent high numbers of deaths in this vulnerable population of older people [8, 17, 18. Therefore, we speculate that acute medical care was severely compromised in German care facilities. Another explanation could be that a disparity in behavior between women and men in responding to the COVID‐19 pandemic‐related lockdown measures and sex differences in the perception regarding the seriousness of COVID‐19 contributed to the observed sex differences of AIS hospitalizations. Galasso et al. reported that women from eight countries, including Germany, more often considered COVID‐19 a severe health problem than men. Furthermore, the agreement and compliance with restraining measures and rules were also higher in women [19]. Although these results might not be directly transferable to our findings, a sex difference in behavior might also explain the more pronounced decline in female AIS patients during the two pandemic waves in Germany.
Whereas AIS patients were treated significantly more often in a stroke unit during the first 9 months in 2020 compared to 2019, SUC significantly decreased during the second pandemic wave from October to December 2020. This might be most likely attributed to the substantially heavier second pandemic wave, with a significant increase of new infections with SARS‐CoV‐2 and consecutively rising numbers of critically ill patients treated in intensive care units in Germany [7, 8. This development resulted in a reorganization of care with newly established separated COVID‐19 intermediate and intensive care units that consecutively decreased the number of stroke unit beds in some areas. Furthermore, the number of hospitalized AIS patients with concurrent COVID‐19 was 3.6 times higher during the second wave compared to the first pandemic wave period. AIS patients with concurrent COVID‐19 were usually not treated on the regular stroke units in Germany but again on specialized COVID‐19 intensive care units. The decline in the SUC rate paralleled the significantly lower use of IVT in AIS patients during the second pandemic wave period. It has been reported that IVT use has been affected by the pandemic on a global level during the height of the first pandemic period from March to June 2020 [5]. However, this was not true for Germany, where the first pandemic wave was much weaker than the second wave period with lower numbers of new infections with SARS‐CoV‐2 weekly [7].
In contrast, the use of MT was consistently higher throughout the year 2020 compared to 2019, with the highest relative difference during the first pandemic wave period (+1.3%). The higher use of MT in 2020 is probably part of Germany's steadily rising MT rate over the past years [20, 21, 22. However, together with the marked decline in AIS patients and the significantly higher in‐hospital mortality of AIS patients during the first pandemic wave period, we assume that hospitalized AIS patients during the first wave had more severe strokes, whereas primarily patients with minor stroke did not seek medical care in hospitals. Based on our findings, this hypothesis does not apply to the second pandemic wave, in which the decline in hospitalized AIS patients was lower and in‐hospital mortality was not different from the previous year period.
In Germany, SARS‐CoV‐2 infection was present in 0.6% of all patients hospitalized for AIS in 2020. As expected, the highest numbers of hospitalized AISpos patients were noted during the first and second wave periods. This German SARS‐CoV‐2 infection rate is lower than the recently published data of 457 selected stroke centers from more than 70 countries that report a SARS‐CoV‐2 infection rate of 3.3% among 52,026 stroke admissions. Two aspects might be responsible for the observed differences between the two studies. First of all, the study by Nogueira et al. [5] focused on the 4 months at the first pandemic wave height and included several countries that were more severely affected by the pandemic than Germany. Second, this study included all types of cerebrovascular events (transient ischemic attack, ischemic stroke, and intracerebral hemorrhage), whereas our study focused on ischemic stroke patients.
Although LVOs are probably more frequent in COVID‐19‐associated AIS [4, 23 the general use of MT in AISpos patients was similar to noninfected AIS patients. Nevertheless, treatments with MT and IVT showed a dynamic difference during the different pandemic periods in Germany. The IVT rates of AISpos patients were consistently high in 2020, whereas the MT rate in AISpos patients peaked during the pre‐second wave period and declined again during the second wave period. However, the MT rate in the second wave period was still higher as compared to the first wave period, with its much lower number of COVID‐19 patients. The increase of the MT rate since the first pandemic wave period might be attributed to a particular focus on LVOs in AISpos patients and the routine implementation of practical hygiene concepts, resulting in a fast and safe triage of patients with reduced risk of infection of health care workers. Furthermore, shortening the delay from onset to initiation of recanalization treatment could also be attributed to an earlier presentation of AIS patients to the hospital during the second wave, but this remains speculative, as this dataset does not provide such information. Although recanalization treatments were frequently applied in AISpos patients in Germany, the mortality rate remained high, supporting that AIS and concurrent COVID‐19 are associated with worse prognosis [24].
Limitations
Our nationwide study has limitations. The data refer to the overall number of hospitalized patients with a main diagnosis of AIS, irrespective of the clinical details, such as time of onset, symptom severity, premorbid functional status, and comorbidities. Thus, the data of treatment rates are at risk of confounding. Although in‐hospital mortality data are recorded, we do not have information on long‐term functional outcomes, such as the modified ranking scale after 90 days. However, our administrative data have high accuracy, because registration of all stroke cases and acute treatment procedures is a prerequisite to get financial compensation. To rule out that an incorrect coding leads to better remuneration for the respective hospitals, the medical health insurance services closely control the process, including the coding of operating and procedure keys for MT and IVT. Nevertheless, incorrect coding cannot be excluded in some cases, but systematic error is unlikely. To exclude double‐coding procedures, the system itself assures that one IVT or MT procedure refers to only one AIS patient, even if the patient has been transferred to a second hospital for MT.
Reliance on routine clinical coding might underestimate the incidence of minor strokes, which can be misdiagnosed as a transient ischemic attack or stroke mimics. However, we do not assume a systematic over‐ or underestimation of AIS in the respective periods, because that would have resulted in a noticeable change in the proportion of AIS patients treated with, for example, IVT or MT. Furthermore, there was no change in the German coding system nor a revision of the ICD version during the analyzed periods that could have affected the coding quality.
Despite these common limitations, administrative data have been considered appropriate for investigating such dynamics over the years [25].
CONCLUSIONS
A substantial decline in AIS hospitalizations characterized the first pandemic wave in spring 2020. Although the number of patients with COVID‐19 was much higher during the second wave period in fall/winter 2020, the decline in AIS hospitalizations was substantially lower compared to the first wave period. This was most likely attributable to reduced fear of infection, routine implementation of hygiene concepts, and improvements in hospital infrastructure for effective clinical management of COVID‐19 patients.
Irrespective of comorbid COVID‐19, acute AIS therapies remained at high levels in Germany during the first and second pandemic wave period, including recanalization treatments and SUC. Nevertheless, AIS and concurrent COVID‐19 were associated with very high in‐hospital mortality.
ACKNOWLEDGMENT
Open access funding enabled and organized by Projekt DEAL. WOA Institution: Ruhr‐Universitat Bochum Blended DEAL: Projekt DEAL.
CONFLICT OF INTEREST
None.
AUTHOR CONTRIBUTIONS
Daniel Richter: Conceptualization (equal), data curation (supporting), formal analysis (lead), methodology (equal), project administration (equal), visualization (lead), writing–original draft (lead), writing–review & editing (equal). Jens Eyding: Conceptualization (equal), writing–review & editing (equal). Ralph Weber: Conceptualization (equal), writing–review & editing (equal). Dirk Bartig: Conceptualization (equal), data curation (lead), formal analysis (supporting), writing–review & editing (equal). Armin Grau: Conceptualization (equal), writing–review & editing (equal). Werner Hacke: Conceptualization (equal), writing–review & editing (equal). Christos Krogias: Conceptualization (equal), formal analysis (supporting), methodology (equal), project administration (equal), visualization (supporting), writing–original draft (supporting), writing–review & editing (equal).
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study represents a secondary data analysis of data from the German Federal Statistical Office, complying with the German data protection regulations. No informed consent or ethical approval was required.
Supporting information
Figure S1
Richter D, Eyding J, Weber R, et al. A full year of the COVID‐19 pandemic with two infection waves and its impact on ischemic stroke patient care in Germany. Eur J Neurol. 2022;29:105–113. 10.1111/ene.15057
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Tsivgoulis G, Palaiodimou L, Zand R, et al. COVID‐19 and cerebrovascular diseases: a comprehensive overview. Ther Adv Neurol Disord. 2020;8(13):1756286420978004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Richter D, Krogias C, Eyding J, Bartig D, Grau A, Weber R. Letter to the editor: Comparison of stroke care parameters in acute ischemic stroke patients with and without concurrent Covid‐19. A Nationwide analysis. Neurol Res Pract. 2020;2:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tan YK, Goh C, Leow AST, et al. COVID‐19 and ischemic stroke: a systematic review and meta‐summary of the literature. J Thromb Thrombolysis. 2020;50(3):587‐595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yaghi S, Ishida K, Torres J, et al. SARS‐CoV‐2 and stroke in a New York healthcare system. Stroke. 2020;51:2002‐2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nogueira RG, Qureshi MM, Abdalkader M, et al. Global impact of COVID‐19 on stroke care and intravenous thrombolysis. Neurology. 2021;96(23):e2824‐e2838. 10.1212/WNL.0000000000011885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Richter D, Eyding J, Weber R, et al. Analysis of nationwide stroke patient care in times of COVID‐19 pandemic in Germany. Stroke. 2021;52(2):716‐721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. COVID‐19‐Fälle nach Altersgruppe und Meldewoche. Accessed August 5, 2021. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Daten/Altersverteilung.html
- 8. Tage‐Inzidenzen nach Bundesländern und Kreisen (fixierte Werte) sowie Gesamtübersicht der pro Tag ans RKI übermittelten Fälle und Todesfälle. Accessed August 5, 2021 https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Daten/Fallzahlen_Kum_Tab.html
- 9. Katsouras C, Karapanayiotides T, Papafaklis M, et al. Greater decline of acute stroke admissions compared with acute coronary syndromes during COVID‐19 outbreak in Greece: Cerebro/cardiovascular implications amidst a second wave surge. Eur J Neurol. 2020;28(10):3452‐3455. 10.1111/ene.14666 [DOI] [PubMed] [Google Scholar]
- 10. Katsouras C, Tsivgoulis G, Papafaklis M, et al. Persistent decline of hospitalizations for acute stroke and acute coronary syndrome during the second wave of the COVID‐19 pandemic in Greece: collateral damage unaffected. Ther Adv Neurol Disord. 2021;14:175628642110295. 10.1177/17562864211029540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mobilitätsindikatoren auf Basis von Mobilfunkdaten. Accessed April 6, 2021. https://www.destatis.de/DE/Service/EXDAT/Datensaetze/mobilitaetsindikatoren‐mobilfunkdaten.html;jsessionid=30FE5B9E7D43A4999A0B49E9BAE541A6.live741
- 12. American College of Emergency Physicians COVID‐19 . Accessed May 6, 2021. https://www.emergencyphysicians.org/globalassets/emphysicians/all‐pdfs/acep‐mc‐Covid19‐april‐poll‐analysis.pdf
- 13. Empfehlungen des RKI zu Hygienemaßnahmen im Rahmen der Behandlung und Pflege von Patienten mit einer Infektion durch SARS‐CoV‐2. Accessed May 31, 2021. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Hygiene.html
- 14. Das Phaenomen der leeren Stroke‐units waehrend der Corona‐Krise. Accessed July16th, 2021. https://dgn.org/neuronews/journal_club/phaenomen‐der‐leeren‐stroke‐units‐waehrend‐der‐corona‐krise‐prof‐christian‐gerloff‐sprach‐dazu‐in‐ndr‐visite/
- 15. Sonderauswertung zu Sterbefallzahlen der Jahre 2020/2021. Accessed April 6, 2021. https://www.destatis.de/DE/Themen/Gesellschaft‐Umwelt/Bevoelkerung/Sterbefaelle‐Lebenserwartung/Tabellen/sonderauswertung‐sterbefaelle.html;jsessionid=1100067C6DD11BD21D5C14059951351F.live722?nn=209016
- 16. Pflegestatistik ‐ Pflege im Rahmen der Pflegeversicherung ‐ Deutschlandergebnisse ‐ 2019. Accessed July16, 2021. https://www.destatis.de/DE/Themen/Gesellschaft‐Umwelt/Gesundheit/Pflege/Publikationen/Downloads‐Pflege/pflege‐deutschlandergebnisse‐5224001199004.html;jsessionid=3948C26E0910246C47DB4B0C01300508.live742?nn=238640
- 17. Prävention und Management von COVID‐19 in Alten‐ und Pflegeeinrichtungen und Einrichtungen für Menschen mit Beeinträchtigungen und Behinderungen. Accessed July16th, 2021. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Alten_Pflegeeinrichtung_Empfehlung.pdf?__blob=publicationFile
- 18. Coronavirus Disease 2019 (COVID‐19) Daily Situation Report of the Robert Koch Institute ‐ 27/04/2020 ‐ UPDATED STATUS FOR GERMANY. Accessed July16, 2021. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/2020‐04‐27‐en.pdf?__blob=publicationFile
- 19. Galasso V, Pons V, Profeta P, Becher M, Brouard S, Foucault M. Gender differences in COVID‐19 attitudes and behavior: Panel evidence from eight countries. Proc Natl Acad Sci USA. 2020;117(44):27285‐27291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Schlachetzki F, Theek C, Hubert ND, et al. Low stroke incidence in the TEMPiS telestroke network during COVID‐19 pandemic effect of lockdown on thrombolysis and thrombectomy. J Telemed Telecare. 2020;1‐7. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Krogias C, Weber R, Richter D, Bartig D, Eyding J. Nationwide treatment reality of patients with acute ischemic stroke in Germany: Update of the regionalized analysis on use of recanalization treatment procedures and stroke complex treatment. Nervenarzt. 2020;91(10):908‐919. [DOI] [PubMed] [Google Scholar]
- 22. Richter D, Weber R, Eyding J, et al. Acute ischemic stroke care in Germany ‐ further progress from 2016 to 2019. Neurol Res Pract. 2021;3(1):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ladopoulos T, Zand R, Shahjouei S, et al. COVID‐19: Neuroimaging Features of a Pandemic. J Neuroimaging. 2021;31(2):228‐243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ntaios G, Michel P, Georgiopoulos G, et al. Characteristics and outcomes in patients with COVID‐19 and acute ischemic stroke: the global COVID‐19 stroke registry. Stroke. 2020;51(9):e254‐e258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sacco S, Pistoia F, Carolei A. Stroke tracked by administrative coding data: is it fair? Stroke. 2013;44(7):1766‐1768. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


