Abstract
Aim
To ascertain a delay in attendances to the emergency department (ED) during 2020 lockdown.
Methods
Area‐based cohort study on paediatric (0‐15 years) attendances resulting in hospital admission in Tuscany, Italy, in February‐May 2020, and the corresponding periods in 2018‐19. We analysed times from symptom onset to arrival, the odds of arriving late (>90th centile of time) and paediatricians’ judgements of a late presentation by logistic models.
Results
As expected, ED attendance fell sharply (−62%) in 2020 vs 2018‐19. As for cases studied (455 in 2020 and 1161 in 2018–19), we documented a delay in arrival to the ED in 2020 versus 2018–19 for several groups of diagnoses, namely gastroenteritis, sepsis, wounds, burns and infections overall. Time to presentation over 90th centile was also higher in 2020 (odds ratio, OR: 1.44; 95% confidence interval: 1.00, 2.06), as were paediatricians’ judgements of a late arrival (18.9% of cases in 2020 vs. 13.4% in 2018‐19; OR: 1.58; 1.14, 2.19)
Conclusion
In a population‐based cohort, delayed attendances to ED ascertained both subjectively and objectively convey the message to families and to paediatricians to seek hospital care in case of severe or unremitting symptoms and not to wait longer than they normally would.
Keywords: COVID‐19, delayed attendance, emergency medicine, epidemiology, public health
Abbreviations
- CI
Confidence Interval
- COVID‐19
Corona Virus Disease 19
- ED
emergency department
- ICD‐9
International Classification of Diseases, 9th revision coding systems
- OR
odds ratio
KEYNOTES.
This population‐based study reported a simultaneous reduction of emergency department attendance and a delayed presentation during the first wave of the pandemic.
The delay was demonstrated both based on paediatricians’ judgements and on time elapsed from symptoms to presentation, in comparison with the previous 2 years.
We found a delay for sepsis, gastroenteritis, wounds and burns and, when considered together, additional infections including mastoiditis, cellulitis, urinary tract infections and bronchiolitis.
1. INTRODUCTION
Children are protected both in terms of susceptibility to SARS‐CoV‐2 infections and of serious illnesses. 1, 2 However, the negative effect of the pandemic on children health has been widely described, from an increase of mental health problems3 to a decreased attendance to health services.4 A decrease in emergency department (ED) attendance has been reported in children in several countries since the early phases of the pandemic, together with a case series of delayed presentations to hospital care and subsequent critical illnesses, because of reluctance to visit the hospital for fear of contracting SARS‐CoV‐2. 5, 6, 7 The issue of possible delayed presentations to the ED has been addressed also more systematically. In a survey performed at the end of April 2020 in United Kingdom and Ireland,8 paediatricians witnessed delayed presentation (from 14% to 47% of all presentations in different regions) during the two previous weeks. On the contrary, a two‐week prospective survey in seven hospitals in United Kingdom and Ireland9 found that parents reported a delay in ED attendance, that is waiting longer than they normally would, or were concerned about going to the ED only in 3.8% of cases. Both surveys8, 9 were based on the opinion of individual paediatricians and/or parents, and there were no baseline data for comparison.
With regard to surgical diseases, data on appendiceal complications as a proxy of delay in attendance to hospital for abdominal pain have been analysed in several countries during the pandemic in comparison with previous years 10, 11, 12, 13, 14, 15.
Delayed presentation to ED as a ‘secondary’ effect of the pandemic could notably be different in different countries due to a combination of public health organisation and family environment, and also needs to be confirmed in more structured surveys.
We therefore aimed to ascertain in a systematic way whether the reduction of the number of attendances to all ED settings that care for children in Tuscany, a region of Central Italy, during the first phase of the pandemic was accompanied by a delay in presentation for selected diseases. The possible delay was studied assessing physicians’ judgement but also evaluating time elapsed from the first symptoms to the presentation to the ED during a 3 and half month's period of 2020—during national lockdown—compared to the same period in the years 2018–19.
2. METHODS
2.1. Data collection
We did a population‐based analysis on all paediatric (0‐15 years old) ED presentations in the Tuscany region in the period 1 January–31 December 2020, and in 2018‐2019. We then examined paediatric attendances in the period of the first wave of SARS‐CoV‐2 pandemic (17 February–31 May 2020) in ED with >5000 paediatric attendances/year, open 24/7 and with full‐time coverage by a paediatrician. As we aimed at studying a possible late attendance of more severe cases only, we restricted the study to ED presentations with the highest priority codes at triage (scores 1 to 3 of a 5‐level modified Emergency Severity Index),16 who were subsequently admitted to the paediatric ward or to a short‐term observation ward for at least 24 hours. Among the discharge diagnoses classified according to the International Classification of Diseases, 9th revision coding systems (ICD‐9), we excluded diagnoses with a very low prevalence (<4 inthe studied period), those with symptoms not additionally classified as diseases (e. g. fever, vomiting), fractures (very unlikely to arrive late at the hospital) and diseases possibly related to SARS‐CoV‐2 (e.g. pneumonia and bronchitis), though we included bronchiolitis and acute respiratory failure.
We studied ED attendances with the same characteristics in the corresponding period of years 2018 and 2019: two cases belonging to the same group of ICD‐9 discharge codes selected for 2020.
ED admissions data are derived from administrative data of the Regional Health Service (RFC106).
For each ED attendance, the data were made available on a web form to a paediatrician of the hospital that had the patient in charge, who accessed the forms by means of personal ID and password. Physicians checked the data of each patient provided on the web form, which included the patient’s age and sex, date and time of visit, ICD‐9 diagnosis. In addition, the paediatrician reported on the web form the following data taken from the hospital case reporting system: time elapsed from symptom onset to presentation to the hospital (expressed in hours up to the first 24, expressed in days up to 15 days and censored at > 15 days) and judgement on the presence of a delayed presentation to the ED (yes, no, not sure).
Two meetings were held with the participating paediatricians to explain the study. Before analyses, the data were reviewed by two paediatricians (LG, FR) and the paediatricians of each hospital and discordances on time to arrival were resolved by consensus.
After collecting the data, we grouped the diagnoses in 18 mutually exclusive, clinically meaningful groups that also differed for expected times to arrival to the ED (Table S1).
2.2. Statistical analysis
To quantify a possible delay in presentation to the hospital, we used 3 variables:
Time to presentation to ED, in hours/days as recorded in the hospital reporting system and described above. Given the highly positive skewed distribution of times to presentation, we compared them between years by using Wilcoxon or log‐rank tests.
For each diagnostic group, time to presentation was recoded to create a variable identifying cases whose time was above the 90th centile for each diagnostic group, taking the value of yes (>90th centile) or no. We performed a multivariable analysis using logistic models, estimating odds of outcome adjusted for the following covariates: hospitals and diagnostic groups. The choice of covariates was done based on the observation that median time of arrival was substantially different in different diagnostic groups and on the knowledge of the distribution of hospitals in the Tuscany Region, with a few hospitals covering larger areas than others. Thus, a later arrival is presented as a higher odds, and the corresponding contrast between years—2020 vs 2018‐2019—yields a higher odds ratio (OR) in case of later arrival in 2020.
The paediatricians’ judgement of late arrival: a binary variable where answers ‘no’ and ‘not sure’ were grouped together and analysed with a logistic model to estimate OR.
As data were collected within hospitals, observations are not independent. To take into account this structure of data in multivariable analysis, we carried out conditional logistic models (for time >90th centile and paediatriciansa judgements of late arrivals). To estimate the degree of clustering on hospitals, we used random‐effects logistic models. Owing to correlated errors, robust standard errors estimation was always used.17
Finally, we looked at possible deleterious delays in appendicitis arrivals by analysing the rate of appendiceal perforation over all appendicitis who underwent a surgical procedure, based only on hospital discharge records of the same hospitals from 17 February to 31 May 2020 and corresponding periods of 2018‐2019.
All statistical analysis was carried out with Stata version 15 (Stata Corp, College Station, USA).
All the data, including those on the web forms, were provided by the Regional Health Agency of Tuscany, which is a branch of the Regional Health Service, and were de‐identified. No ethical permission was therefore required according to Regional law.
3. RESULTS
We found substantial decreases in paediatric ED patient volume in 2020 vs 2018‐2019 (Figure 1). In particular, paediatric ED attendance fell briskly in February. In June, there was a slow increase in ED volume, although attendances were still substantially below those of the corresponding weeks of the two previous years until 31 December. From March to December 2020, attendance was 76,815, a drop of 62% from 202,112 (yearly average of the same period in 2018‐2019).
FIGURE 1.
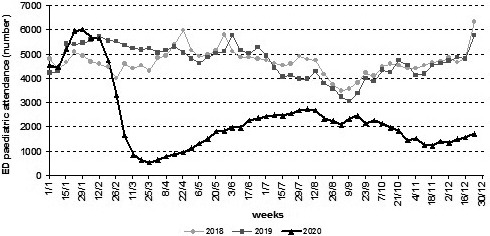
Emergency department paediatric attendance in 2020 and in 2018–2019 by week; data averaged over prior 7 days
ED attendance from 17 February to 31 May 2020 for more severe cases—as defined above—in the 15 hospitals with >5000 paediatric attendances/year, and with full‐time coverage by a paediatrician, was 1.166 cases. Of these, we evaluated for late presentation and according to designated diagnoses 455 cases in 2020 and 1161 for the corresponding periods of 2018 and 2019.
The distribution of time from symptom onset to ED presentation for all the diagnoses in which an evaluation of time was possible from hospital electronic charts (431 of 455 in 2020 and 1082 of 1161 for the previous two years) is shown in Table 1. Starting from the 50th centile, times were somewhat longer for cases seen in 2020 in comparison with those seen in the previous two years (12 h vs. 10, 48 h vs. 24 and 96 h vs. 72 for 50th, 75th and 90th centile, respectively).
TABLE 1.
Distribution of time from symptom onset to the emergency department presentation; 17 February to 31 May 2020 and corresponding periods of 2018‐2019
| Years | No of patients | Time in hours* | |||
|---|---|---|---|---|---|
| 25th centile | 50th centile | 75th centile | 90th centile | ||
| 2020 | 431 | 2 | 12 | 48 | 96 |
| 2018‐19 | 1082 | 2 | 10 | 24 | 72 |
p = 0.34, Two‐sample Wilcoxon rank‐sum test.
Time from symptom onset to presentation.
Table 2 shows the distribution of time when diagnostic categories were considered; for gastroenteritis, sepsis, wounds and burns and a residual group of conditions, time from symptom onset to ED presentation was substantially higher for 2020 in comparison with the previous two years. When all ‘infectious’ cases (gastroenteritis, sepsis, mastoiditis, cellulitis, abscess, urinary tract infections, orchitis, bronchiolitis) were considered together, their arrival was delayed in 2020 vs 2018‐2019 (Time of arrival: mean 49.1 vs 39.4; P<0.08, log‐rank test).
TABLE 2.
Time from symptom onset to presentation to the emergency department in different diagnosis groups; 17 February to 31 May 2020 and corresponding periods of 2018‐2019
| Diagnosis group | No of patients | Time in hours, median (IQR) | p * | ||
|---|---|---|---|---|---|
| 2020 | 2018‐2019 | 2020 | 2018‐2019 | ||
| Medical | |||||
| Gastroenteritis | 8 | 67 | 48 (36‐84) | 16 (7‐24) | <0.01 |
| Dehydration | 10 | 56 | 24 (12‐72) | 24 (12‐72) | 0.87 |
| Diabetes | 8 | 19 | 360 (288‐384) | 336 (168‐384) | 0.61 |
| Epilepsy | 60 | 117 | 1 (1‐2) | 1 (1‐2) | 0.11 |
| Mastoiditis/cellulitis/abscess | 16 | 58 | 24 (10‐120) | 24 (8‐48) | 0.38 |
| Urinary infections/orchitis | 43 | 61 | 24 (8‐72) | 24 (6‐72) | 0.87 |
| Sepsis / suspected sepsis | 9 | 18 | 72 (24‐120) | 18 (3‐48) | <0.01 |
| Bronchiolitis | 52 | 103 | 24 (8.5‐48) | 24 (8‐48) | 0.98 |
| Acute respiratory failure | 16 | 50 | 36 (12.5‐60) | 24 (5‐48) | 0.14 |
| Collapse and syncope | 11 | 37 | 1 (1‐3) | 1 (1‐2) | 0.60 |
| Head injury | 14 | 52 | 1 (1‐4) | 1 (1‐2) | 0.46 |
| Other injuries | 15 | 31 | 1 (1‐2) | 1 (1‐2) | 0.42 |
| Foreign body ingestion | 11 | 18 | 1 (1‐2) | 1 (1‐3) | 0.76 |
| Wounds/burns | 18 | 36 | 2 (1‐2) | 1 (1‐1.5) | 0.03 |
| Surgical | |||||
| Appendicitis | 69 | 159 | 14 (8‐24) | 20 (8‐24) | 0.26 |
| Testicular torsion | 15 | 45 | 10 (2‐72) | 5 (3‐24) | 0.44 |
| Abdominal or pelvic organ torsion | 14 | 23 | 12 (6‐48) | 10 (4‐24) | 0.28 |
| Other diagnoses | 42 | 133 | 24 (5‐96) | 12 (4‐48) | 0.09 |
Abbreviatons: IQR, interquartile range.
Two‐sample Wilcoxon rank‐sum test.
A conditional logistic model adjusting for groups of diagnoses and hospital clustering showed that there was an increase of late arrival—defined as the 90th centile in each diagnostic group—in 2020, with an OR of 1.44 (95% CI: 1.00, 2.06; p = 0.05). Hospital clustering explained 3.4% of variance of outcome in a random‐effects model.
According to the judgement of participating paediatricians, delays in presentations were present in 18.9% of cases (86/455) in 2020 vs. 13.4% (155/1161) in 2018‐2019, while in 23/455 (5.1%) and in 53/1161 (4.6%), there was uncertainty as to whether there was a delay. (p = 0.015, Pearson's chi‐squared test). In a conditional logistic model adjusting for groups of diagnoses and hospital clustering, the OR of physician judgement of delay was 1.58 (95% CI: 1.14, 2.19; p = 0.006) in 2020 vs. 2018‐19. Hospital clustering explained 11% of the variance of outcome in a random‐effects model.
Among appendicitis that underwent surgery, the frequency of peritonitis was somewhat higher in 2020 (23/49 cases = 49%) than in 2018‐19 (44/118 = 37.3%) (OR= 1.61; 95% CI; 0.80; 3.25 at conditional logistic analysis adjusting for centre).
4. DISCUSSION
This area‐based cohort study in Tuscany confirmed that during the first wave of the pandemic, the number of ED presentations fell briskly. It also confirmed that children were brought to the hospital later than usual. Paediatricians judged that children were brought to the hospital too late in a greater proportion of cases in comparison with the corresponding periods of 2018–2019. This was confirmed by two objective measures, that is a longer time from symptom onset to presentation to the ED and a greater proportion of children with a diagnosis‐specific time >90th centile in 2020 incomparison with the two previous years.
The delay was chiefly due to late presentation of sepsis, gastroenteritis, wounds and burns, and a miscellany of conditions, though for a few diagnoses our sample possibly lacked sufficient statistical power. Taking together, all presumably infectious cases (gastroenteritis, sepsis, mastoiditis, cellulitis, abscess, urinary tract infections, orchitis and bronchiolitis) their presentation to ED was also significantly delayed in 2020 vs. 2018‐2019. A possible explanation for our findings on infections is that during the pandemic, as in‐person visits by general paediatric practitioners were reduced, common antibiotics for upper respiratory infections were used more freely, for example in case of fever. This might have resulted in infections not cured either because sustained by bacteria possibly not responsive to antibiotics commonly used for respiratory infections (i.e. amoxicillin in case of urinary tract infections or sepsis) or because of viral pathogenesis (i.e. gastroenteritis and bronchiolitis).
We did not observe a delayed presentation in cases of diabetes, which was instead reported in a paper on five large hospitals in Italy5 and in a survey done in the United Kingdom and Ireland.8 However, in both studies paediatricians had witnessed a delay in presentation to the ED, with no objective measurements and, above all, no comparison with previous years.
Surgical emergencies (appendicitis, testicular or other abdominal organ torsion) also did not arrive substantially later during the pandemic, though time from symptom onset to presentation to the emergency department was longer in 2020 versus previous years. An additional analysis restricted to cases of appendicitis who underwent surgery showed a tendency to a larger percentage of appendiceal perforation in 2020 incomparison with the two previous years. Our results confirmed previous ones obtained in most 10, 11, 12, 13, 14 but not all15 countries in Europe, Israel, USA and China of an increase, sometimes a borderline/not significant one, in complications rates for appendicitis during pandemic which has been attributed to late presentations.
Our data, that point to a possible increased reluctance of parents in seeking hospital care during the COVID‐19 outbreak, are consistent with those reported in a few studies in adults. Admissions for acute myocardial infarction were substantially reduced in Italy in 2020 vs 2019, and for patients admitted, a delay was documented for time from symptom onset to coronary angiography and for time from first medical contact to coronary revascularisation.18 These findings have been confirmed in other countries.19
The strength of our study lies in the area‐based ascertainment of cases from a whole Italian Region (Tuscany), in the comparison with earlier years, and in the evaluation of a possible delay based not only on physicians' judgement but also on time elapsed from first symptoms to presentation. We focussed on ED attendances presenting with higher acuity (as evidenced by a triage code in the 3 most acute categories on a 5‐point scale) yielding a hospital admission of at least 24 h. We a priori selected a number of conditions that could have presented a delay in ED presentation, excluding rare conditions that could not be adequately compared across years, fractures (that we deemed improbable that were not taken to hospital on time) and presentations without a definite diagnosis (e.g. fever and vomiting).
As a limitation, we cannot demonstrate how much the reported delays were associated with harm to children, though delayed presentations for medical and surgical conditions which require fast assessment and treatment like sepsis or acute respiratory failure or testicular torsion were probably accompanied by a more severe and prolonged course of the disease. On the other hand, a retrospective national cohort study in Scotland suggested that a reduction in paediatric emergency care utilisation was not associated with evidence of severe harm.20
In conclusion, our study demonstrates a delayed hospital care seeking for several paediatric conditions during the COVID‐19 pandemic in a population‐based retrospective survey. Based on these findings, the message to both families and paediatricians is to seek hospital care in case of severe or unremitting symptoms and not to wait longer than they normally would.
CONFLICT OF INTEREST
The authors have no conflicts of interests to declare.
Supporting information
Table S1
Acknowledgements
We acknowledge the contribution of the Members of the Tuscany Pediatric Emergency Study Group: Antonella Amendolea (Division of Neonatology and Pediatrics, Cecina Hospital, Cecina, Italy); Nicoletta Battiglia (Pediatric Unit, San Giuseppe Hospital, Empoli, Italy); Francesca Bechi (Paediatric and Neonatologic Unit, Santo Stefano Hospital, Prato, Italy); Rosa Castaldo (Pediatric Unit, Misericordia Hospital, Grosseto, Italy); Mauro Ceccherini (Pediatric Unit, San Donato Hospital, Arezzo, Italy); Rosa Giuseppina Costa (Division of Neonatology and Pediatrics, Apuane Hospital, Massa Carrara, Italy); Claudia Maggi (Division of Neonatology and Pediatrics, Lotti Hospital, Pontedera, Italy); Silvia Navari and Nicolò Miggiano (Division of Neonatology and Pediatrics, Versilia Hospital, Viareggio, Italy); Paola Pelosi (Pediatric Unit, Santa Maria Annunziata Hospital, Bagno a Ripoli, Italy); Andrea Petracchi (Division of Neonatology and Pediatrics, Spedali Riuniti di Livorno, Livorno, Italy); Roberta Puxeddu (Pediatric Unit, San Jacopo Hospital, Pistoia, Italy); Annalisa Rossetti (Pediatric Clinic, Department of Molecular Medicine and Development, Le Scotte University Hospital, Siena, Italy); Luca Tafi (Paediatric and Neonatal Unit, Valdarno Hospital, Montevarchi, Italy); Francesco Vierucci (Division of Neonatology and Pediatrics, San Luca Hospital, Lucca, Italy).
Rusconi F, Di Fabrizio V, Puglia M, et al. Delayed presentation of children to the emergency department during the first wave of COVID‐19 pandemic in Italy: Area‐based cohort study. Acta Paediatr. 2021;110:2796–2801. 10.1111/apa.16019
REFERENCES
- 1.Ludvigsson JF. Systematic review of COVID‐19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020;109:1088–1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Viner RM, Mytton OT, Bonell C, et al. Susceptibility to SARS‐CoV‐2 infection among children and adolescents compared with adults: a systematic review and meta‐analysis. JAMA Pediatr. 2021;2021(175):212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guessoum SB, Lachal J, Radjack R, et al. Adolescent psychiatric disorders during the COVID‐19 pandemic and lockdown. Psychiatry Res. 2020;291:113264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McDonald HI, Tessier E, White JM, et al. Early impact of the coronavirus disease (COVID‐19) pandemic and physical distancing measures on routine childhood vaccinations in England, January to April 2020. Euro Surveill. 2020;25:2000848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID‐19. Lancet Child Adolesc Health. 2020;4:e10–e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McDonnell T, Nicholson E, Conlon C, et al. Assessing the impact of COVID‐19 public health stages on paediatric emergency attendance. Int J Environ Res Public Health. 2020;17:6719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schaffert M, Zimmermann F, Bauer L, et al. Austrian study shows that delays in accessing acute paediatric health care outweighed the risks of COVID‐19. Acta Paediatr. 2020;109:2309–2310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lynn RM, Avis JL, Lenton S, Amin‐Chowdhury Z, Ladhani SN. Delayed access to care and late presentations in children during the COVID‐19 pandemic: a snapshot survey of 4075 paediatricians in the UK and Ireland. Arch Dis Child. 2021;106:e8. [DOI] [PubMed] [Google Scholar]
- 9.Roland D, Harwood R, Bishop N, Hargreaves D, Patel S, Sinha I. Children's emergency presentations during the COVID‐19 pandemic. Lancet Child Adolesc Health. 2020;4:e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Place R, Lee J, Howell J. Rate of pediatric appendiceal perforation at a children's hospital during the COVID‐19 pandemic compared with the previous year. JAMA Netw Open. 2020;3:e2027948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gerall CD, DeFazio JR, Kahan AM, et al. Delayed presentation and sub‐optimal outcomes of pediatric patients with acute appendicitis during the COVID‐19 pandemic. J Pediatr Surg. 2021;56:905–910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Snapiri O, Rosenberg Danziger C, Krause I, et al. Delayed diagnosis of paediatric appendicitis during the COVID‐19 pandemic. Acta Paediatr. 2020;109:1672–1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Somers K, Elwahab SA, Raza MZ, et al. Impact of the COVID‐19 pandemic on management and outcomes in acute appendicitis: Should these new practices be the norm? The Surgeon. 2021. [Epub ahead of print]. 10.1016/j.surge.2021.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang Y, Li Y, Du X. Acute complex appendicitis during the COVID‐19 epidemic: a single‐institution retrospective analysis based on real‐world data. Am J Emerg Med. 2021;46:74–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tristán GJ, Romero SH, Pellitero ES, Espiñera CR, Martín DA, Góngora RE. Acute appendicitis in children during the COVID‐19 pandemic neither delayed diagnosis nor worse outcomes. Pediatric Emerg Care. 2021;37:185–190. [DOI] [PubMed] [Google Scholar]
- 16.Durani Y, Brecher D, Walmsley D, Attia MW, Loiselle JM. The Emergency Severity Index Version 4: reliability in pediatric patients. Pediatr Emerg Care. 2009;25:751–753. [PubMed] [Google Scholar]
- 17.Localio AR, Berlin JA, Ten Have TR, Kimmel SE. Adjustments for center in multicenter studies: an overview. Ann Intern Med. 2001;135:112–123. [DOI] [PubMed] [Google Scholar]
- 18.De Rosa S , Spaccarotella C, Basso C, Calabrò MP, Curcio A, Filardi PP. Reduction of hospitalizations for myocardial infarction in Italy in the COVID‐19 era. Eur Heart J. 2020;41:2083‐2088. Erratum in: Eur Heart J 2021; 42: 322. Erratum in: Eur Heart J 2021; 42: 683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kiss P, Carcel C, Hockham C, Peters SAE. The impact of the COVID‐19 pandemic on the care and management of patients with acute cardiovascular disease: a systematic review. Eur Heart J Qual Care Clin Outcomes. 2021;7:18–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Williams TC, MacRae C, Swann OV, Haseeb H, Cunningham S, Davies P. Indirect effects of the COVID‐19 pandemic on paediatric healthcare use and severe disease: a retrospective national cohort study.Arch Dis Child. 2021. [Epub ahead of print]. 10.1136/archdischild-2020-321008 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1


