Abstract
We here studied some potential factors underlying variation in compliance with preventive behaviors against COVID‐19 by studying mask wearing during outdoor recreational activities in a midsize city of Argentina in 2020. The originality of present research relies on the complementation of observational (N = 15,507) and survey (N = 578) data and in assessing the determinants of and disposition to the same preventive behavior across activities. In Study 1, we did 8 weeks of unobtrusive systematic observation of mask wearing in outdoor recreational sites as a function of activity (walking, running, and cycling). In Study 2, we ran an online survey (concomitant with the last weeks of the observational study) to measure self‐reported mask use and relevant beliefs, including self‐ and other‐regarding motives. Behavioral observations showed that mask wearing declined over time for the three activities as predicted from a social dilemma perspective; nonetheless, compliance significantly differed across activities. Self‐reported mask use was predicted by the perceived risk of contagion for the self and for others, perceived comfort costs of wearing masks, and social norms, but not by perceived illness severity or mask effectiveness. We discuss some implications and limitations of present findings for the development of preventive strategies to reduce COVID‐19 transmission.
Keywords: COVID‐19, face masks, Health Belief Model, norm compliance, protective behaviors
INTRODUCTION
Wearing face masks has become a crucial preventive behavior in the current COVID‐19 pandemic. However, research shows that people's compliance with preventive recommendations to reduce the risk of contagion of COVID‐19, such as social distancing and mask wearing, varies a lot both within and among countries (e.g. Anaki & Sergay, 2021; Bogg & Milad, 2020; Breakwell et al., 2021; Chen et al., 2020; de Bruin & Bennet, 2020; Franzen & Wöhner, 2021). There is consensus among researchers and experts that an effort to understand this variability is a crucial element for an effective response to this pandemic (Betsch, 2020; Van Babel et al., 2020; West et al., 2020). The present research is a contribution in this direction.
The Health Belief Model (HBM) is a very popular theoretical model for predicting differences in health behavior according to which people's beliefs about whether they are at risk for a disease, and their perceptions of the consequences of taking action to avoid it, affect their disposition to do something about it (Rosenstock, 1974). The model involves several core concepts such as perceived susceptibility to and perceived severity of the disease, and perceived benefits, barriers, and costs associated to the relevant behaviors, and has been applied most often (Champion & Skinner, 2008) and most successfully (Brewer & Rimer, 2008) for health concerns that are prevention related and asymptomatic. Indeed, there are already a number of reports on the use of the HBM to comprehend the factors that may affect people's readiness to perform recommended preventive behaviors to reduce the risk of contagion of COVID‐19 (e.g. Barakat & Kasemy, 2020; Tong et al., 2020; Zareipour et al., 2020). Furthermore, other research, even if not in strict adherence to the HBM, has tested some of its core concepts for predicting COVID‐19 preventive behaviors as well (e.g. Anaki & Sergay, 2021; Hornik et al., 2021; Liu & Mesch, 2020; Prasetyo et al., 2020). All in all, there seems to be a general tendency of empirical support of the HBM variables as reliable predictors of COVID‐19 preventive behaviors.
A limitation of the HBM, nonetheless, involves its reliance on beliefs mostly focused on the individual, and not so much on others. In focusing on individuals' health‐related perceptions, the HBM does not explicitly address important social and interpersonal issues (Brewer & Rimer, 2008), such as the perceived consequences of preventive behaviors on others and the interdependency of social behavior. Many authors believe that other‐regarding preferences as well as the perception of social norms could be relevant factors underlying the display of preventive behaviors in this pandemic (Betsch, 2020; Hume et al., 2021; Patel, 2021). Therefore, we here propose to study the determinants of COVID‐19 preventive behaviors complementing some core concepts of the HBM with a social dilemma perspective that highlights relevant social aspects of preventive behaviors (Ling & Chyong Ho, 2020; Moussaoui et al., 2020).
Social dilemmas involve situations in which individual incentives and social goals may not be fully aligned (Dawes, 1980). In such situations, despite all‐encompassing cooperation maximizes social welfare, cooperation is personally costly, and therefore, individuals have incentives to restrain it and free ride on others' efforts (Nowak, 2011). Preventive behaviors in the current pandemic may present the inherent conflict of a social dilemma in which individual costs associated with these behaviors may represent stronger incentives than the perceived benefits of prevention (Ling & Chyong Ho, 2020), at least for some (e.g. the young; Franzen & Wöhner, 2021). Considering and stimulating other‐regarding motives have been proposed as potential solutions to unlocking social dilemmas and achieving socially desirable outcomes in the current pandemic (Betsch, 2020; Ling & Chyong Ho, 2020). For instance, some nudges tested to improve compliance with preventive behaviors have been targeted at focusing people's attention on the benefits conferred to others (Hume et al., 2021). In the same vein, Bicchieri (2006) proposed that social norms (beliefs about common behaviors as well as about behavioral prescriptions and sanctions for noncompliance) may serve to better align individual and social incentives in social dilemmas. Indeed, people may choose to perform socially beneficial individually costly behaviors if they believe others are behaving that way (Fischbacher et al., 2001). Patel (2021) has recommended this descriptive norm nudge to increase people's willingness towards COVID‐19 vaccination. However, normative messages may not be a silver bullet to instigate preventive behaviors (Bilancini et al., 2020), and much still needs to be learned about the extent to which and how people's preventive behaviors could be motivated out of social concerns.
In the present studies, we focused on studying demographic as well as belief‐related factors associated with COVID‐19 preventive behaviors, in particular mask wearing, while people did outdoor recreational activities such as walking, running, and cycling. There has been concern about outdoor activities involving contagion risks that can be reduced with appropriate behaviors (Arias, 2020; Blocken et al., 2020; Setti et al., 2020). Moreover, to our best knowledge, most research on COVID‐19 preventive behaviors have not assessed the frequency and determinants of the same behavior across different activities (see relevant references above), implicitly disregarding relevant variation that may arise as people perceived different risks, costs, and benefits in different situations.
In more detail, in Study 1, we went to public recreational sites in Bahía Blanca (Argentina) to unobtrusively measure people's use of face masks while they were walking, running, or cycling. This study provided hard behavioral data on compliance with mask wearing across weeks. It is relevant to highlight here that the present observational study contrasts against most research on preventive behaviors during the current pandemic, which has relied mainly on self‐reports (see Freeland et al., 2020). The potential issue of social desirability biases should incline researchers to consider self‐reports on health behaviors with caution. We are not the first to highlight the issue of social desirability in COVID‐19 survey research (de Bruin & Bennet, 2020; Haliwa et al., 2020). The main issue with self‐reports on health behavior is that survey respondents might feel inclined to overreport prohealth‐related behaviors as a self‐serving conscious or unconscious strategy (Contzen et al., 2015; Kristiansen & Harding, 1984; van de Mortel, 2008). Hence, an important strength of Study 1 was the collection of observational data on the level of preventive behaviors over time, allowing us to assess its relationship with demographic variables and epidemiological data and to validate survey self‐reports of preventive behaviors.
In Study 2, we surveyed people about the frequency of mask wearing during outdoor activities while also asking about relevant beliefs to test them as potential predictors of the target preventive behaviors. We asked about some core concepts from the HBM (Champion & Skinner, 2008; Rosenstock, 1974) such as perceived illness susceptibility and severity, as well as perceived costs and benefits of mask wearing. In addition, to complement these concepts from the HBM, which only focuses on the perception of consequences directly relevant for the individual (Brewer & Rimer, 2008), we included a social dilemma perspective in which social norms and other‐regarding motives were surveyed as potentially relevant predictors of preventive behaviors (Ling & Chyong Ho, 2020; Moussaoui et al., 2020).
STUDY 1
In this study, we collected systematic observational data on people's compliance with the norm of wearing a face mask during outdoor activities across weeks. The goal was to estimate the variation in mask wearing across activities and time and assess its relationship with demographic (age and sex) and epidemiological data (local and nationwide numbers on COVID‐19 cases and deaths).
In Study 1, we took measures of mask wearing for 8 weeks, beginning in the first week local authorities allowed citizens to go out for outdoor recreational activities after the initial months of strict lockdown for the COVID pandemic in Argentina. In order to do outdoor recreational activities, local authorities had set up a web page in which people had to register before leaving their homes. Importantly, through this web page as well as other means (e.g. radio and TV spots), authorities made clear that mask wearing was mandatory for outdoor recreational activities. Considering mask wearing as a preventive behavior with the features of a social dilemma (personal costs and benefits to third parties), we expected the proportion of people wearing masks to decline with time, in particular if this norm was not enforced by authorities. The fact that we collected data from the first week outdoor recreational activities were allowed after the initial lockdown was an important feature of the present study because it allowed uncertainty about actual enforcement. Enforcement uncertainty should incline citizens to comply with mask wearing to some degree in the beginning, whereas the accumulation of experience of nonenforcement predicted lower compliance over time.
Methods
The protocol of present studies (both Studies 1 and 2) was reviewed and approved by the Bioethics Committee of the Municipal Hospital of Bahía Blanca (Hospital Municipal de Agudos “Dr. Leónidas Lucero”).
The local government in Bahía Blanca allowed outdoor recreational activities from May 25, 2020, after more than 2 months of strict lockdown (Figure 1 shows a timeline of local events in the pandemic and the number of new daily cases of COVID‐19 in Bahía Blanca). Since the first week this permission was in place, each of the five co‐authors went to one of five recreational sites selected for their known use for outdoor recreational activities at different times and days of the week to register whether people adhered to the required wearing of face masks during outdoor activities (Figure S2 shows a map of the city with the sampling sites marked in color). The selection of days and times was made considering observers' convenience, also trying to cover busy hours in order to capture mask use when it was most consequential (i.e. when it was most crowded). Systematic observations began on Thursday, May 28, and ended on Wednesday, July 8, covering 6 weeks for the first round of observations. The second round went from October 22 to November 4, covering another 2 weeks (see Figure 1).
FIGURE 1.
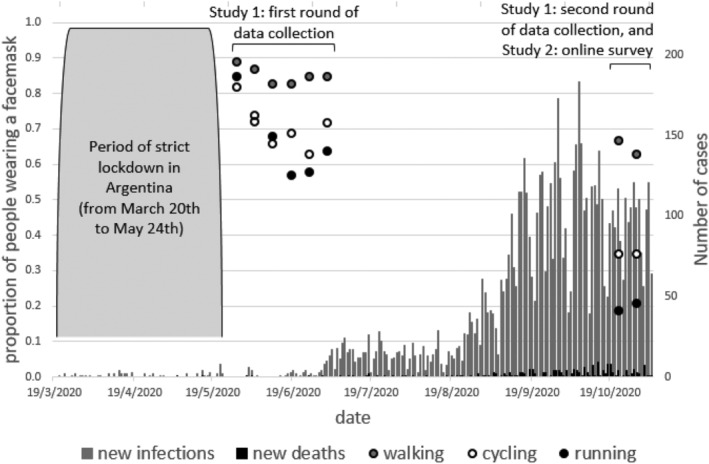
The Y axis on the left shows the proportion of people wearing a face mask as a function of week and activity (circles in the figure), whereas the right Y axis shows the number of new COVID‐19 cases and deaths on those weeks in Bahía Blanca (bars in the figure). The figure also shows the dates in which Studies 1 and 2 were run
Observation sessions lasted from 30 to 60 min. During sessions, observers used a paper notebook with a grid in which they wrote down the place, date, and start and end times of the session. Once in site, observers selected a path, if there was more than one, and began walking and registering the people they passed by (i.e. only those who were going in the opposite direction). For each registered person, records involved the size of the group (1: if they were alone), the activity they were doing (walking, running, or cycling), an estimated age (baby—if does not walk and looks younger than 12 months, child—up to 12 years old, adolescent—up to 18 years old, young adult—up to 30 years old, adult—up to 60 years old, and elderly), an estimated gender (female/male), and of most importance, whether they were wearing a face mask and, if they were wearing it, how they were using the mask (covering mouth and nose, covering only the mouth, or covering neither the nose nor the mouth). To minimize sampling biases in case the flow of people was excessive to register everyone, there was a rule by which observers would register the person who was approximately 10 m away at the moment of raising the head to score. Also, as far as possible, we avoided registering the same person more than once in the same session. Last, we took note whether at any point in the route we saw police presence nearby the recreational area (within 50 m of the place where an observation was recorded), though we almost never saw the police or any other formal authority around.
Statistical analyses
Analyses were done with STATA 13. We did Probit regressions with face mask wearing (1: yes; 0: no) as outcome variable, and several predictors: time (week number, from 1—first week of sampling by the end of May—to 23—eighth week of sampling in November), activity (we created a dummy variable for each activity, walking, running, and cycling), group size, estimated age, and estimated gender (1: female; 0: male). Similar analyses for the appropriate use of face mask as outcome variable can be found in the supporting information. Data, STATA codes for the analyses, and the supporting information can be found at the following Open Science Forum (OSF) link: https://osf.io/3qsu7/?view_only=b326ecf234e7418e96d173d1e5102dac.
Results and discussion
From the 15,507 observations throughout the 8 weeks of the study, 71 per cent of the records involved people walking, 15 per cent people running, and 12 per cent people cycling. Around half of the sample was attributed female gender (53%), and we recorded 0.005 per cent babies, 5 per cent children, 7.2 per cent teenagers, 26 per cent young adults, 54 per cent adults, and 7.6 per cent older adults (with a few missing cases).
Figure 1 shows the proportion of people wearing a face mask while walking, running, and cycling across weeks. A Probit regression with walking and running as dummy variables (using the cycling dummy as reference category) showed that mask wearing was significantly more likely for those walking (B = .65, p < .001) and marginally less likely for those running (B = −.07, p = .08) relative to those cycling (walking vs. running, χ 2 = 592, p < .001). This result highlights the fact that the same preventive behavior varies a lot across different activities and thus stresses the need to be cautious when generalizing results from a particular behavior in a given context and circumstance.
Separate regressions for each activity showed that wearing a mask significantly decreased across weeks for the three activities (while walking, B = −.04, p < .001; while running, B = −.07, p < .001; and while cycling, B = −.05, p < .001). As shown in Figure 1, as mask wearing declined over time, COVID cases and the associated death toll increased both locally and nationwide.
Wearing a mask while walking was positively predicted by being a female (B = .26, p < .001) and being older (B = .19, p < .001) and negatively predicted by group size (B = −.04, p = .016). Wearing a mask while running was positively predicted by being female (B = .25, p < .001) and negatively predicted by group size (B = −.17, p < .001), whereas age was not a significant predictor (B = −.03, p = .40). Last, wearing a mask while cycling was (negatively) predicted by group size only (B = −.06, p = .04; gender, B = .10, p = .10; and age, B = −.01, p = .62).
In sum, there were two general findings across activities. First, wearing masks decreased across weeks. And second, going outdoor for recreational activities in groups usually predicted fewer cases of mask wearing than going alone. Women wore masks more frequently than men both for walking and running, and whereas an older age predicted wearing a face mask while walking, that pattern did not occur in the other two activities.
STUDY 2
The goal of this second study was to aid the understanding of the factors leading to compliance with the norm of mask wearing during outdoor activities. More specifically, we tested variables from the HBM (Champion & Skinner, 2008), such as perceived COVID‐19 contagion risk, disease severity, the effectiveness of masks as a prevention measure, and costs of wearing masks, as predictors of mask wearing while walking, running, and cycling. To encompass other‐regarding motives as potential predictors of the target preventive behaviors, we also asked for perceptions of illness susceptibility and severity for third parties as well as of mask effectiveness to protect others. Last, we also tested whether social norms (personal, descriptive, and prescriptive) were significant predictors of mask use.
Methods
Participants
We relied on a nonprobabilistic convenience sample. The recruitment of participants to the online survey was done through emails and social media. We sent an invitation email to a database of 5000 email addresses including students, former students, teaching assistants, and professors from the Universidad Nacional del Sur and other tertiary‐level education institutions in Bahía Blanca. At the same time, each of the authors shared the survey link in her or his social media. Respondents were told about the anonymous and voluntary nature of the survey and the absence of risks and explicitly consented on responding it. The survey was filled in by 578 respondents in a period of 14 days (last week of October and first week of November 2020), time that coincided with the last 2 weeks of behavioral field observations from Study 1.
Instrument
The responses analyzed here are only a part of the survey questions, which also included topics, such as vaccination intent and political preferences, not reported here. The original survey was in Spanish, and an English translation of the survey questions relevant for present goals can be read in the supporting information.
The main outcome variables in the survey were respondents' frequency of mask use during outdoor recreational walking, running, and cycling. Respondents answered about the frequency of mask use during the mentioned activities in a 10‐point scale from “never” to “always,” both in general during the pandemic and in the last week in particular.
We also asked for different types of beliefs as potential predictors of mask wearing. Belief questions were asked separately for each activity unless indicated.
Perceptions of risk of contagion and mask effectiveness
Participants were asked to rate in a 10‐point scale from “no risk” to “very risky” their perceived risk of COVID‐19 contagion if they did the activity without face mask. We also asked respondents to estimate the risk of contagion if they did wear a mask, and the difference between the reported risk with and without mask was taken as an index of a perceived benefit of wearing a mask, hereafter called “effectiveness.” We also asked respondents to estimate the risk of contagion for third parties who passed by a person unknowingly ill of COVID‐19 doing an outdoor activity with or without a mask. The risk and effectiveness for the self are referred to as “risk_1” and “effectiveness_1,” respectively, whereas the risk and effectiveness for others are referred to as “risk_2” and “effectiveness_2,” respectively.
Perceived illness severity
In 10‐point scales from “no risk” to “very risky,” we asked for the expected severity of several potential negative consequences of getting COVID‐19, which included consequences for their own health and life risk, for their home economy, for their loved ones' health, and for others' health. Severity questions did not differentiate among activities.
Perceived costs of wearing a mask
In terms of the barriers for wearing a mask, we asked respondents to express their beliefs about the comfort and health adverse consequences of mask wearing. Questions asked to report in 10‐point scales from “not uncomfortable at all” to “very uncomfortable” to estimate mask comfort during a given activity and from “not at all dangerous” to “very dangerous” to estimate the perceived health risk of wearing a mask.
Social norms
We measured beliefs about the likelihood of informal and formal sanctions for not wearing masks during outdoor activities, common behaviors, and normative expectations, and we also elicited personal norms. Respondents expressed in a 10‐point scale from “very unlikely” to “very likely” the perceived likelihood of their attention being called by a formal authority or by a common citizen for not wearing a mask while doing outdoor activities (the estimation of formal and informal sanctions did not differentiate among activities). Empirical and normative expectations were elicited by asking respondents to estimate how many people wore a mask out of every 10 people walking, running, and cycling and how many believed not wearing a mask while doing the activity was morally reproachable, respectively. Personal norms involved replying in a 10‐point scale from “not at all” to “very much,” the extent to which respondents thought not wearing a mask while doing the activity was morally reproachable.
To control for the order of questions, we presented the survey in four different orderings across participants (see further details in the supporting information).
Analysis plan
First, we presented the descriptive statistics of the raw variables from the survey as a function of activity. Second, we grouped (averaged) many raw variables into fewer theoretical relevant groups (mask wearing, contagion risk for the self, contagion risk for others, severity for the self, severity for other, self‐protective effectiveness, other‐protective effectiveness, costs, and norms) and report their descriptive statistics as well as their Cronbach's alpha to assess internal consistency. Table S1 shows the indicators associated with each latent or composite variable. Third, to validate the main outcome variables from the survey, we were interested in assessing whether respondents' report of the frequency of mask use as a function of activity presented a similar pattern to that obtained from unobtrusive field observations in Study 1. Because some people reported going out just for one of the target activities, whereas others reported doing two or even the three activities, different nonparametric tests on mask wearing were done for each of these cases (Wilcoxon matched paired tests for repeated measures and Mann–Whitney U tests for between‐subject comparisons). Fourth and last, to search for the main predictors of mask wearing, we did hierarchically organised regressions. The entering order of factors in the regressions was as follows: sociodemographic controls, contagion risk, illness severity, benefits (mask effectiveness), costs, and norms. For each hierarchical regression, we reported whether the addition of each subsequent level of variables significantly improved the variance explained by the previous level. The alpha value was set at .05. Relying on the software G*Power (Faul et al., 2007), we determined that with the sample size collected (N = 578) and an alpha value set at .05, we achieved a power of .80 to detect an R 2 change of at least .0265 in the models with all the composite variables as predictors (risk_1, risk_2, severity_1, severity_2, effectiveness_1, effectiveness_2, costs, and norms). Data, STATA codes for the reported analyses, and the supporting information can be found at the following OSF link: https://osf.io/3qsu7/?view_only=b326ecf234e7418e96d173d1e5102dac.
Results and discussion
Descriptive statistics
The online survey was responded by 578 individuals. Respondents' mean (±1 SD) age was 33 ± 11 years old, ranging from 18 to 76; 64 per cent self‐identified as women and 34 per cent as men (very few preferred not to respond the gender question); and relative to respondents' highest level of achieved education, 59 per cent reported complete tertiary studies (which included university degrees), 35 per cent reported incomplete tertiary studies, and 6 per cent reported complete secondary education or below.
In Table 1, we presented the descriptive statistics for the raw variables in which self‐reports discriminated among activities. Mask wearing in general highly correlated with mask wearing during the last week for the three activities (for walking, r = .87, n = 382, p < .001; for running, r = .94, n = 84, p < .001; and for cycling, r = .91, n = 149, p < .001). Therefore, we only reported mask wearing for each activity in general (see Table 1). Self‐reported mask wearing across activities showed a similar pattern to that observed in the field (Figure 1, Study 1): people walking showed the highest frequency of mask use, followed by bike riders, and then by runners. Between‐subject comparison showed that wearing a mask while walking was reported to be more frequent than in the other two activities (vs. running, χ 2 = 15.36, n = 379, p < .001; vs. cycling, χ 2 = 13.31, n = 313, p < .001); however, there were no significant differences in the frequency of mask wearing between those reporting to have gone running and those gone cycling (χ 2 = 1.76, n = 214, p = .18). For the within‐subject comparison, all differences in mask wearing between activities resulted significant (see Table 1). Similar results were found when the same analyses were done only with respondents who reported going for outdoor activities in sites sampled in Study 1 (see the supporting information).
TABLE 1.
Mean (±1 SD) of self‐reports that discriminated among walking, running, and cycling
| Walking | Running | Cycling | Walk vs. run | Walk vs. ride | Run vs. ride | |
|---|---|---|---|---|---|---|
| Mask wearing | 8.48 (2.63) | 5.16 (3.88) | 5.89 (3.70) | <.001 | <.001 | .003 |
| Risk_1 (for the self) | 6.26 (2.90) | 5.73 (3.00) | 4.62 (3.00) | <.001 | <.001 | <.001 |
| Risk_2 (for others) | 7.22 (2.80) | 7.18 (2.88) | 6.04 (3.04) | .605 | <.001 | <.001 |
| Effectiveness_1 (for the self) | 3.35 (3.08) | 2.69 (3.19) | 2.08 (3.02) | <.001 | <.001 | <.001 |
| Effectiveness_2 (for others) | 3.31 (2.30) | 3.13 (2.37) | 2.67 (2.48) | .012 | <.001 | <.001 |
| Comfort cost | 5.98 (2.93) | 8.56 (2.17) | 7.43 (2.70) | <.001 | <.001 | <.001 |
| Health costs | 3.55 (2.94) | 5.63 (3.34) | 5.02 (3.29) | <.001 | <.001 | <.001 |
| Prescriptive norm | 5.44 (2.16) | 3.95 (2.40) | 3.55 (2.35) | <.001 | <.001 | <.001 |
| Descriptive norm | 6.07 (1.99) | 2.89 (2.29) | 3.04 (2.19) | <.001 | <.001 | .553 |
| Personal norm | 7.01 (3.26) | 5.26 (3.43) | 4.78 (3.39) | <.001 | <.001 | <.001 |
Note: The three right‐hand side columns show p‐values corresponding to Wilcoxon matched paired tests.
All in all, people reported wearing masks more frequently when walking than when cycling, and when cycling than when running in Study 2 in agreement with observational data collected in the same weeks (Study 1). In addition, self‐report and behavioral data both showed that the quantitative difference in mask wearing between people walking and people doing the other two activities was larger than between those running and those cycling (see the last 2 weeks in Figure 1 and mask use in Table 1). In sum, the mentioned similarities in the frequency of mask use between self‐reports and observational data provided some confidence that self‐reports tracked objective behavioral data from the field in some meaningful way.
In turn, the difference in mask wearing across activities was evident to respondents as indicated by their estimation of how common each behavior was (descriptive norm; see Table 1). Relative to the perceived risk of contagion for a person doing the activity without mask (risk_1), respondents perceived more risk for walking than running and cycling (further discussion of these findings can be found in the Determinants of risk perceptions section in the supporting information at the OSF link). In terms of the risk of contagion for someone passing by an unknowingly sick person doing the activity without mask (risk_2), respondents perceived greater risk for passing by a person walking or running than a person cycling. Mask effectiveness for self and others' protection was estimated to be higher for walking than for running and cycling, following the same ordering across activities as risk perception. In terms of the perceived comfort and health costs of wearing a mask, respondents' perceived them to be higher for running than for cycling and walking. Prescriptive and personal norms showed that respondents believed that others and themselves, respectively, found walking without mask to be more reproachable than running or cycling without mask (we further explored and discussed the determinants of respondents' personal norms in the supporting information).
In terms of pairwise correlations, the main finding was that the frequency of mask wearing significantly correlated with all the composite scores of the main potential predictors considered (see Table 2). To better understand the predictive relationship of these factors with mask wearing as outcome variable, we reported hierarchical regressions below.
TABLE 2.
Descriptive statistics (including Pearson's correlation coefficients) of the main composite variables of Study 2
| Mean (±1 SD) | Cronbach's α | N | (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) Mask use | 7.61 (3.05) | .97 | 531 | ||||||||
| (2) Risk_1 | 5.54 (2.72) | .90 | 578 | .55*** | |||||||
| (3) Risk_2 | 6.81 (2.73) | .93 | 578 | .50*** | .80*** | ||||||
| (4) Severity _1 | 4.88 (1.81) | .63 | 577 | .19*** | .34*** | .31*** | |||||
| (5) Severity _2 | 5.10 (2.91) | Single item | 572 | .10* | .22*** | .19*** | .39*** | ||||
| (6) Effective_1 | 2.71 (2.81) | .89 | 573 | .43*** | .74*** | .57*** | .21*** | .16*** | |||
| (7) Effective_2 | 3.04 (2.13) | .87 | 578 | .33*** | .46*** | .58*** | .10* | .08* | .55*** | ||
| (8) Costs | 5.96 (2.32) | .88 | 577 | −.36*** | −.38*** | −.33*** | −.07 | .02 | −.36*** | −.19*** | |
| (9) Norms | 4.25 (1.45) | .79 | 578 | .50*** | .48*** | .48*** | .21*** | .18*** | .31*** | .26*** | −.30*** |
p < .05.
p < .01.
p < .001.
Predictors of mask wearing
The hierarchical regression in Table 3 involved composite variables and showed that, in its first step that included sociodemographic controls, the only significant predictor was age, meaning that older people reported more frequent use of masks during outdoor activities. As expected considering the available information on risk groups for COVID‐19 (e.g., see Franzen & Wöhner, 2021), age significantly predicted the estimated severity of the illness for the self (standardised B = .184, p < .001; but not the estimated severity for others' health, standardised B = −.01, p = .81). Age also predicted social norms (standardised B = .11, p = .012), but not perceptions of risk of contagion (standardised B = .05, p = .20) or mask effectiveness (standardised B = .03, p = .49). The following steps of the regression showed that the addition of perceived contagion risk, estimated costs of wearing a mask, and social norms made a significant contribution in the explanation of mask wearing variance, whereas the estimated severity of getting ill and the perceived effectiveness of wearing a mask did not add significant explanatory value.
TABLE 3.
Standardised coefficients from a hierarchical regression with mask wearing as outcome variable
| (1) | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|
| Age | .12* | .08* | .08 † | .08 † | .08 † | .05 |
| Gender (F = 1; M = 0) | .04 | −.01 | −.01 | −.01 | .03 | .03 |
| Secondary education (c) | −.06 | −.00 | −.00 | −.02 | −.02 | .00 |
| Tertiary education (i) | −.28 | −.11 | −.12 | −.14 | −.19 | −.11 |
| Tertiary education (c) | −.35 | −.13 | −.12 | −.15 | −.19 | −.11 |
| Risk_1 | .40*** | .39*** | .34*** | .31*** | .26** | |
| Risk_2 | .19** | .19** | .18* | .14* | .07 | |
| Severity_1 | .02 | .03 | .03 | .02 | ||
| Severity_2 | −.01 | −.02 | .00 | −.02 | ||
| Effectiveness_1 | .05 | .02 | .02 | |||
| Effectiveness_2 | .03 | .05 | .06 | |||
| Costs | −.17*** | −.13** | ||||
| Norms | .26*** | |||||
| R 2 | .02 † | .33*** | .33*** | .33*** | .35*** | .39*** |
| ΔR 2 | .31*** | .002 | .001 | .022*** | .046*** | |
| N | 511 | 511 | 506 | 501 | 500 | 500 |
Abbreviations: c, complete; i, incomplete.
p < .05.
p < .01.
p < .001.
p < .1.
In agreement with the hierarchical regression with composite scores (Table 3), independent regressions for each of the three activities with the raw measures from the survey (Table 4) showed that the addition of variables measuring perceived risk of contagion, costs of wearing a mask, and social norms significantly contributed to the explanation of variance in mask wearing. In turn, the addition of variables measuring estimated severity of getting COVID‐19 and the effectiveness of wearing a mask in reducing the contagion likelihood did not add significant explanatory value. In more detail, risk of contagion for the self if not wearing a mask was a significant predictor of mask wearing in all three activities, and the perceived risk of contagion for others passing by a sick person without mask predicted wearing a mask for walking and cycling, but not for running. In turn, the estimated comfort cost of wearing a mask negatively predicted wearing a mask for the three activities, whereas estimated health costs only negatively predicted mask wearing for walking. Last, we can see that most variability in mask use explained by social norms came from respondent's personal norms and empirical (descriptive) expectations about others' use of masks, whereas the estimated likelihood of formal and informal sanctions and prescriptive norms were rarely significant.
TABLE 4.
Standardised coefficients from hierarchical regressions with mask wearing as outcome variable as a function of outdoor activity
| Walking | Running | Cycling | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (1) | (2) | (3) | (4) | (5) | (6) | (1) | (2) | (3) | (4) | (5) | (6) | |
| Demographic controls | ||||||||||||||||||
| Age | .05 | .02 | .03 | .04 | .04 | .006 | −.03 | −.008 | −.015 | −.01 | −.006 | −.01 | .15 † | .11 † | .10 | .10 | .09 | .07 |
| Gender (F = 1; M = 0) | .04 | −.01 | −.01 | −.006 | .06 | .04 | −.15 † | −.17* | −.18* | −.20** | −.14 † | −.09 | −.06 | −.04 | −.05 | −.06 | −.01 | −.04 |
| Secondary education | −.09 | −.07 | −.09 | −.09 | −.09 | −.12 | −.1 | .07 | .08 | .09 | −.067 | .2 | −.05 | .05 | .02 | .04 | .03 | .04 |
| Tertiary education (i) | −.26 | −.17 | −.21 | −.22 | −.27 | −.28 | −.57 | −.27 | −.27 | −.19 | −.14 | −.19 | −.29 | −.07 | −.14 | −.12 | −.16 | .14 |
| Tertiary education (c) | −.28 | −.14 | −.18 | −.20 | −.24 | −.27 | −.57 | −.21 | −.22 | −.11 | −.08 | −.13 | −.37 | −.08 | −.18 | −.16 | −.17 | −.15 |
| Risk | ||||||||||||||||||
| For the self | .37 *** | .38 *** | .34 *** | .31 *** | .21 ** | .515 *** | .52 *** | .53 ** | .43 ** | .11 | .37 *** | .38 *** | .26* | .17 | .06 | |||
| For others | .19** | .18** | .20** | .16* | .066 | .03 | .01 | .13 | .15 | .11 | .16* | .13 | .12 | .11 | .01 | |||
| Severity | ||||||||||||||||||
| Own health | .03 | .03 | .04 | .004 | .01 | −.02 | −.00 | .04 | .16 † | .17 † | .12 | .05 | ||||||
| Own life risk | −.03 | −.03 | −.02 | .02 | .04 | .05 | .06 | .04 | −.08 | −.08 | −.02 | .03 | ||||||
| Own economy | −.11* | −.10* | −.09* | −.07 † | −.03 | −.06 | −.08 | .004 | −.04 | −.02 | −.01 | .01 | ||||||
| Loved ones' health | .06 | .06 | .05 | .015 | .02 | .03 | −.05 | −.07 | .05 | .04 | −.00 | .02 | ||||||
| Others' health | −.002 | −.002 | .01 | .02 | −.002 | .005 | .08 | −.01 | −.07 | −.07 | −.01 | −.05 | ||||||
| Effectiveness | ||||||||||||||||||
| For protecting the self | .04 | .01 | −.014 | −.03 | −.09 | −.08 | .16 | .07 | .03 | |||||||||
| For protecting others | −.02 | −.01 | −.01 | −.145 | −.13 | −.055 | .02 | .01 | .06 | |||||||||
| Costs | ||||||||||||||||||
| Comfort | −.11* | −.05 | −.28 ** | −.13 | −.35 *** | −.26 *** | ||||||||||||
| Health | −.14** | −.08 † | −.00 | .006 | −.09 | −.03 | ||||||||||||
| Norms | ||||||||||||||||||
| Informal sanction | .06 | −.08 | .005 | |||||||||||||||
| Formal sanction | −.08* | −.004 | −.06 | |||||||||||||||
| Prescriptive | −.08 † | −.03 | −.14* | |||||||||||||||
| Descriptive | .27 *** | .33 *** | .15* | |||||||||||||||
| Personal | .32 *** | .37** | .38 *** | |||||||||||||||
| R 2 | .01 | .29 *** | .295 *** | .295 *** | .337 *** | .45 *** | .08* | .364 *** | .368*** | .38 *** | .44 *** | .575 *** | .03 | .27 *** | .282 *** | .293 *** | .422 *** | .522 *** |
| ΔR 2 | .28 *** | .009 | .001 | .042 *** | .117 *** | .28 *** | .004 | .013 | .057 ** | .137 *** | .237 *** | .011 | .011 | .13 *** | .1 *** | |||
| N | 470 | 470 | 456 | 456 | 455 | 455 | 155 | 155 | 150 | 150 | 150 | 150 | 214 | 214 | 210 | 210 | 210 | 210 |
Abbreviations: c, complete; i, incomplete.
p < .05.
p < .01.
p < .001.
p < .1.
GENERAL DISCUSSION
The main findings of present studies were the following. In terms of the behavioral data, first, we observed that the frequency of mask wearing declined across weeks for the three activities measured. This behavioral pattern went in contrast to the increase in COVID‐19 cases and associated death toll both locally and nationwide. The declining compliance with mask wearing was predicted from a social dilemma perspective according to which personally costly prosociality may be difficult to sustain without norm enforcement or other mechanism to nudge compliance. Indeed, downward snowballing of cooperation in the context of social dilemmas is a common cross‐cultural phenomenon (e.g. Henrich et al., 2006). Second, we found that people walking were the ones with the highest proportion of mask use followed by people cycling, whereas runners were the ones showing the least compliance.
In terms of the survey results, first, reported mask use followed the same pattern across activities as that observed in the field, which provided confidence on the validity of self‐reports. Second, self‐reported mask wearing was significantly predicted by perceptions of risk of contagion for the self and for others. The association of preventive behaviors with perceived risk of contagion for the individual has been shown before both in the current pandemic (Anaki & Sergay, 2021; Prasetyo et al., 2020; Rad et al., 2021) and in the context of the H1N1 pandemic more than a decade ago (Bish & Michie, 2010). In turn, the relevance of other‐regarding risk beliefs in predicting mask wearing agreed with cross‐country research showing that prosociality is positively associated with increased risk perception (Dryhurst et al., 2020). This suggests that other‐regarding concerns may be a reasonable target to stimulate compliance, which could be a strategy particularly suited to tackle people who may not be personally worried about getting the disease, such as the young (Franzen & Wöhner, 2021).
Third, neither did perceived illness severity nor perceived mask effectiveness add significant value to predicting mask wearing in the survey data. These findings contrast with other research on COVID‐19 preventive behavior (Anaki & Sergay, 2021; Hornik et al., 2021; Tong et al., 2020). Unfortunately, we can only speculate about the sources of divergence between present results and those from others, which can go from the time the surveys were taken to the many differences associated with considering samples from different countries (e.g. different implemented policies; Frey et al., 2020). For instance, differences in the consistency of information about effective protection may lead to very different rates of preventive behavior (Witte & Allen, 2000), and such consistency may change with time as we observed, for example, with changes in the recommendations of the World Health Organization (WHO) on the use of masks for the general public in the current pandemic. Indeed, Prasetyo et al. (2020) found that the level of understanding of COVID‐19, which could be related to the available information, had an impact on the perceived effectiveness of preventive behaviors.
Fourth, personal costs of mask wearing, in particular comfort costs, resulted a significant negative predictor of mask wearing, which seems as a likely explanation of why runners were the group least disposed to wearing masks. Interestingly, comfort costs were even taken into account while considering whether not wearing a mask was morally reproachable. This is surprising under the view that moral considerations, in principle, should focus attention towards the avoidance of harm to third parties (Gray et al., 2012) more than towards personal comfort issues. This result might suggest that the people sampled in the present survey weakly weighted others' costs and benefits when deciding whether to wear a face mask. Indeed, the standardised coefficient of the perception of risk of contagion for others tended to be merely around half the size of the coefficient for the perception of risk of contagion for the self in predicting mask wearing across activities and was even nonsignificant for predicting runners' use of masks (see Table 4).
Last, we found that both personal and descriptive norms were the most important predictors of mask wearing. Indeed, conditional cooperation (the propensity to incur prosocial costs as long as I perceive others doing so) may underlie the observed decrease in compliance across weeks found in Study 1. Economic experiments have repeatedly illustrated cross‐culturally that cooperation may be difficult to sustain without mechanisms to enforce it because free riders disincentivize conditional cooperators' efforts (Henrich et al., 2006). Different strategies beyond enforcement have been suggested to address this issue in the current pandemic, which could go from using in situ normative nudges in the form of signs or posters to the involvement of group leaders (Van Babel et al., 2020), which, for instance, in the case of runners could be the person in charge of the training group.
Before closing this article, we want to mention some limitations of the research described here. First of all, it is important to have in mind that present findings cannot be directly generalized to the population from which present samples were obtained because we did not rely on representative samples. The corroboration of present findings in other samples will serve to test the robustness of present conclusions.
Second, we need to have in mind that the estimated effect of beliefs on preventive behaviors depended on self‐reports. Self‐reported mask wearing could be validated with observational data, which is a methodological strength of the present research. However, beliefs cannot be validated in a similar manner. Though this is a problem with most research relying on self‐reports, it is relevant to have in mind that this could introduce bias for different reasons. For instance, respondents could have adjusted their belief reports based on their reported behavior to reduce cognitive dissonance (Festinger, 1962). In short, results from self‐reports need to be taken with caution.
Last, we only considered some of the core concepts of the HBM for reasons of brevity and presumed relevance. However, there are a number of other concepts both from the HBM and from other health behavior models (see Glanz & Bishop, 2010, for a review) that could be worth exploring in future research. For example, due to our field work (Study 1), we became aware of a lack of cues to action (e.g. reminders of relevant preventive behaviors) in the sampling sites, which relevance in inciting compliance should be explored.
ETHICS STATEMENT
Present research was reviewed and approved by the Bioethics Comittee of the Hospital Municipal, Bahía Blanca, Argentina.
Supporting information
Figure S1. Timeline of the pandemic in Bahía Blanca, Argentina.
Figure S2. Recreational sites in Bahía Blanca, Argentina, where we obtained systematic records of facemask wearing during outdoor recreational activities (image taken from Google Maps; the colored lines were added by the authors to mark the sampling sites).
Figure S3. Proportion of people (averaged across weeks) who did not wear a mask, wear a mask only covering the mouth, or wear a mask covering both mouth and nose, as a function of activity (walking, cycling, or running).
Figure S4. Percentage of people walking who did not wear a mask, wear a mask only covering the mouth, or wear a mask covering both mouth and nose, as a function of week of observation (week 1 began on May 28th 2020; week 23 finished on November 4th 2020).
Figure S5. Percentage of people cycling who did not wear a mask, wear a mask only covering the mouth, or wear a mask covering both mouth and nose, as a function of week of observation (week 1 began on May 28th 2020; week 23 finished on November 4th 2020).
Figure S6. Percentage of people running who did not wear a mask, wear a mask only covering the mouth, or wear a mask covering both mouth and nose, as a function of week of observation (week 1 began on May 28th 2020; week 23 finished on November 4th 2020).
Table S1 shows the indicators (raw questions) associated with each composite (latent) variable.
Freidin, E. , Acera Martini, L. , Senci, C. M. , Duarte, C. , & Carballo, F. (2022). Field observations and survey evidence to assess predictors of mask wearing across different outdoor activities in an Argentine city during the COVID‐19 pandemic. Applied Psychology: Health and Well‐Being, 14(1), 81–100. 10.1111/aphw.12292
DATA AVAILABILITY STATEMENT
Data, STATA codes for the reported analyses, and the supporting information can be found at the following OSF link: https://osf.io/3qsu7/?view_only=b326ecf234e7418e96d173d1e5102dac.
REFERENCES
- Anaki, D. , & Sergay, J. (2021). Predicting health behavior in response to the coronavirus disease (COVID‐19): Worldwide survey results from early March 2020. PLoS ONE, 16(1), e0244534. 10.1371/journal.pone.0244534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arias, F. J. (2020). Are runners more prone to become infected with COVID‐19? An approach from the raindrop collisional model. Journal of Science in Sport and Exercise, 3(2), 167–170. 10.1007/s42978-020-00071-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barakat, A. M. , & Kasemy, Z. A. (2020). Preventive health behaviours during coronavirus disease 2019 pandemic based on health belief model among Egyptians. Middle East Current Psychiatry, 27, 43. 10.1186/s43045-020-00051-y [DOI] [Google Scholar]
- Betsch, C. (2020). Monitoring behavioural insights related to COVID‐19. The Lancet, 395, 1255–1256. 10.1016/S0140-6736(20)30729-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bicchieri, C. (2006). The grammar of society: The nature and dynamics of social norms. Cambridge University Press. [Google Scholar]
- Bilancini, E. , Boncinelli, L. , Capraro, V. , Celadin, T. , & di Paolo, R. (2020). The effect of norm‐based messages on reading and understanding COVID‐19 pandemic response governmental rules. Journal of Behavioral Economics for Policy, 4(COVID‐19 Special Issue), 45–55. 10.31234/osf.io/7863g [DOI] [Google Scholar]
- Bish, A. , & Michie, S. (2010). Demographic and attitudinal determinants of protective behaviours during a pandemic: A review. British Journal of Health Psychology, 15, 797–824. 10.1348/135910710X485826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blocken, B. , Malizia, F. , van Druenen, T. , & Marchal, T. (2020). Towards aerodynamically equivalent COVID19 1.5 m social distancing for walking and running. Retrieved April 15, 2021, from http://www.urbanphysics.net/Social%20Distancing%20v20_White_Paper.pdf
- Bogg, T. , & Milad, E. (2020). Demographic, personality, and social cognition correlates of coronavirus guideline adherence in a U.S. sample. Health Psychology, 39(12), 1026–1036. 10.1037/hea0000891 [DOI] [PubMed] [Google Scholar]
- Breakwell, G. M. , Fino, E. , & Jaspal, R. (2021). The COVID‐19 preventive behaviors index: Development and validation in two samples from the United Kingdom. Evaluation & the Health Professions, 44(1), 77–86. 10.1177/0163278720983416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer, N. T. , & Rimer, B. K. (2008). Perspectives on health behavior theories that focus on individuals. In Glanz K., Rimer B. K., & Viswanath K. (Eds.), Health behavior and health education: Theory, research, and practice, fourth edition (chapter 7, pp. 149–165). John Wiley & Sons. [Google Scholar]
- Champion, V. L. , & Skinner, C. S. (2008). The Health Belief Model. In Glanz K., Rimer B. K., & Viswanath K. (Eds.), Health behavior and health education: Theory, research, and practice, fourth edition (chapter 3, pp. 45–65). John Wiley & Sons. [Google Scholar]
- Chen, Y. , Zhou, R. , Chen, B. , Chen, H. , Li, Y. , Chen, Z. , Zhu, H. , & Wang, H. (2020). Knowledge, perceived beliefs, and preventive behaviors related to COVID‐19 among Chinese older adults: Cross‐sectional web‐based survey. Journal of Medical Internet Research, 22(12), e23729. 10.2196/23729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contzen, N. , de Pasquale, S. , & Mosler, H. (2015). Over‐reporting in handwashing self‐reports: Potential explanatory factors and alternative measurements. PLoS ONE, 10(8), e0136445. 10.1371/journal.pone.0136445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawes, R. M. (1980). Social dilemmas. Annual Review of Psychology, 980(31), 69–93. [Google Scholar]
- de Bruin, W. B. , & Bennet, D. (2020). Relationships between initial COVID‐19 risk perceptions and protective health behaviors: A national survey. American Journal of Preventive Medicine, 59(2), 157–167. 10.1016/j.amepre.2020.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dryhurst, S. , Schneider, C. R. , Kerr, J. , Freeman, A. L. J. , Recchia, G. , van der Bles, A. M. , Spiegelhalter, D. , & van der Linden, S. (2020). Risk perceptions of COVID‐19 around the world. Journal of Risk Research, 23(7–8), 994–1006. 10.1080/13669877.2020.1758193 [DOI] [Google Scholar]
- Faul, F. , Erdfelder, E. , Lang, A.‐G. , & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39, 175–191. [DOI] [PubMed] [Google Scholar]
- Festinger, L. (1962). A theory of cognitive dissonance. Stanford Univer. Press. [Google Scholar]
- Fischbacher, U. , Gächter, S. , & Fehr, E. (2001). Are people conditionally cooperative? Evidence from a public goods experiment. Economics Letters, 71, 397–404. 10.1016/S0165-1765(01)00394-9 [DOI] [Google Scholar]
- Franzen, A. , & Wöhner, F. (2021). Coronavirus risk perception and compliance with social distancing measures in a sample of young adults: Evidence from Switzerland. PLoS ONE, 16(2), e0247447. 10.1371/journal.pone.0247447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeland, K. , Dew, E. M. A. , Sarwer, D. B. , Burg, M. M. , Hart, T. A. , Ewing, S. W. F. , Fang, C. Y. , Blozis, S. A. , Puterman, E. , Marquez, B. , & Kaufmann, P. G. (2020). Health psychology in the time of COVID‐19. Health Psychology, 39(12), 1021–1025. 10.1037/hea0001049 [DOI] [PubMed] [Google Scholar]
- Frey, C. B. , Chen, C. , & Presidente, G. (2020). Democracy, culture, and contagion: Political regimes and countries' responsiveness to Covid‐19. Covid Econ, 18, 222–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz, K. , & Bishop, D. B. (2010). The role of behavioral science theory in development and implementation of public health interventions. Annual Review of Public Health, 31, 399–418. 10.1146/annurev.publhealth.012809.103604 [DOI] [PubMed] [Google Scholar]
- Gray, K. , Young, L. , & Waytz, A. (2012). Mind perception is the essence of morality. Psychological Inquiry, 23, 101–124. 10.1080/1047840X.2012.651387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haliwa, I. , Lee, J. , Wilson, J. , & Shook, N. J. (2020). Mindfulness and engagement in COVID‐19 preventive behavior. Preventive Medicine Reports, 20, 101246. 10.1016/j.pmedr.2020.101246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henrich, J. , McElreath, R. , Barr, A. , Ensminger, J. , Barrett, C. , Bolyanatz, A. , Cardenas, J. C. , Gurven, M. , Gwako, E. , Henrich, N. , Lesorogol, C. , Marlowe, F. , Tracer, D. , & Ziker, J. (2006). Costly punishment across human societies. Science, 312, 1767–1770. 10.1126/science.1127333 [DOI] [PubMed] [Google Scholar]
- Hornik, R. , Kikut, A. , Jesch, E. , Woko, C. , Siegel, L. , & Kim, K. (2021). Association of COVID‐19 misinformation with face mask wearing and social distancing in a nationally representative US sample. Health Communication, 36(1), 6–14. 10.1080/10410236.2020.1847437 [DOI] [PubMed] [Google Scholar]
- Hume, S. , John, P. , Sanders, M. , & Stockdale, E. (2021). Nudge in the time of coronavirus: The compliance to behavioural messages during crisis. Retrieved from SSRN, April, 15, 2021. 10.2139/ssrn.3644165 [DOI]
- Kristiansen, C. M. , & Harding, C. M. (1984). The social desirability of preventive health behavior. Public Health Reports, 99(4), 384–388. [PMC free article] [PubMed] [Google Scholar]
- Ling, G. H. T. , & Chyong Ho, C. M. (2020). Effects of the coronavirus (COVID‐19) pandemic on social behaviours: From a social dilemma perspective. Technium Social Sciences Journal, 7, 312–320. 10.31235/osf.io/8duvx [DOI] [Google Scholar]
- Liu, X. , & Mesch, G. S. (2020). The adoption of preventive behaviors during the COVID‐19 pandemic in China and Israel. International Journal of Environmental Research and Public Health, 17, 7170. 10.3390/ijerph17197170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moussaoui, L. S. , Ofosu, N. D. , & Desrichard, O. (2020). Social psychological correlates of protective behaviours in the COVID‐19 outbreak: Evidence and recommendations from a nationally representative sample. Applied Psychology. Health and Well‐Being, 12(4), 1183–1204. 10.1111/aphw.12235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nowak, M. A. (2011). Super‐cooperators: Altruism, evolution, and why we need each other to succeed. New York: Free Press. [Google Scholar]
- Patel, M. (2021). Test behavioural nudges to boost COVID immunization. Nature, 590, 185. 10.1038/d41586-021-00329-z [DOI] [PubMed] [Google Scholar]
- Prasetyo, Y. T. , Castillo, A. M. , Salonga, L. J. , Sia, J. A. , & Seneta, J. A. (2020). Factors affecting perceived effectiveness of COVID‐19 prevention measures among Filipinos during enhanced community quarantine in Luzon, Philippines: Integrating protection motivation theory and extended theory of planned behavior. International Journal of Infectious Diseases, 99, 312–323. 10.1016/j.ijid.2020.07.074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rad, R. E. , Mohseni, S. , Takhti, H. K. , Azad, M. H. , Shahabi, N. , Aghamolaei, T. , & Norozian, F. (2021). Application of the protection motivation theory for predicting COVID‐19 preventive behaviors in Hormozgan, Iran: A cross sectional study. BMC Public Health, 21, 466. 10.1186/s12889-021-10500-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenstock, I. (1974). Historical origins of the health belief model. Health Education Monographs, 2, 328–335. [DOI] [PubMed] [Google Scholar]
- Setti, L. , Passarini, F. , de Gennaro, G. , Barbieri, P. , Perrone, M. G. , Borelli, M. , Palmisani, J. , Di Gilio, A. , Piscitelli, P. , & Miani, A. (2020). Airborne transmission route of COVID‐19: Why 2 meters/6 feet of inter‐personal distance could not be enough. International Journal of Environmental Research and Public Health, 17, 2932. 10.3390/ijerph17082932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong, K. K. , Chen, J. H. , Yu, E. W. , & Wu, A. M. S. (2020). Adherence to COVID‐19 precautionary measures: Applying the health belief model and generalised social beliefs to a probability community sample. Applied Psychology. Health and Well‐Being, 12(4), 1205–1223. 10.1111/aphw.12230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Babel, J. J. , Baicker, K. , Boggio, P. S. , Capraro, V. , Cichocka, A. , Cikara, M. , Crockett, M. J. , Crum, A. J. , Douglas, K. M. , Druckman, J. N. , Drury, J. , Dube, O. , Ellemers, N. , Finkel, E. J. , Fowler, J. H. , Gelfand, M. , Han, S. , Haslam, S. A. , Jetten, J. , … Willer, R. (2020). Using social and behavioural science to support COVID‐19 pandemic response. Nature Human Behaviour, 4, 460–471. 10.1038/s41562-020-0884-z [DOI] [PubMed] [Google Scholar]
- van de Mortel, T. F. (2008). Faking it: Social desirability response bias in self‐report research. Journal of Advanced Nursing, 25(4), 40–48. [Google Scholar]
- West, R. , Michie, S. , Rubin, G. J. , & Amlôt, R. (2020). Applying principles of behaviour change to reduce SARS‐CoV‐2 transmission. Nature Human Behaviour, 4, 451–459. 10.1038/s41562-020-0887-9 [DOI] [PubMed] [Google Scholar]
- Witte, K. , & Allen, M. (2000). A meta‐analysis of fear appeals: Implications for effective public health campaigns. Health Education & Behavior, 27, 591–615. 10.1177/109019810002700506 [DOI] [PubMed] [Google Scholar]
- Zareipour, M. , Ardakani, M. F. , Moradali, M. R. , Jadgal, M. S. , & Movahed, E. (2020). Determinants of COVID‐19 prevention behavior in the elderly in Urmia: Application of health belief model. Open Access Macedonian Journal of Medical Sciences, 8(T1), 646–650. 10.3889/oamjms.2020.5653 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Timeline of the pandemic in Bahía Blanca, Argentina.
Figure S2. Recreational sites in Bahía Blanca, Argentina, where we obtained systematic records of facemask wearing during outdoor recreational activities (image taken from Google Maps; the colored lines were added by the authors to mark the sampling sites).
Figure S3. Proportion of people (averaged across weeks) who did not wear a mask, wear a mask only covering the mouth, or wear a mask covering both mouth and nose, as a function of activity (walking, cycling, or running).
Figure S4. Percentage of people walking who did not wear a mask, wear a mask only covering the mouth, or wear a mask covering both mouth and nose, as a function of week of observation (week 1 began on May 28th 2020; week 23 finished on November 4th 2020).
Figure S5. Percentage of people cycling who did not wear a mask, wear a mask only covering the mouth, or wear a mask covering both mouth and nose, as a function of week of observation (week 1 began on May 28th 2020; week 23 finished on November 4th 2020).
Figure S6. Percentage of people running who did not wear a mask, wear a mask only covering the mouth, or wear a mask covering both mouth and nose, as a function of week of observation (week 1 began on May 28th 2020; week 23 finished on November 4th 2020).
Table S1 shows the indicators (raw questions) associated with each composite (latent) variable.
Data Availability Statement
Data, STATA codes for the reported analyses, and the supporting information can be found at the following OSF link: https://osf.io/3qsu7/?view_only=b326ecf234e7418e96d173d1e5102dac.


