Abstract
Objective
Glare caused by the headlights of on‐coming vehicles risk safe driving at night. The study aimed to determine the relationship between glare exposure and nighttime driving performance among commercial drivers in Ghana.
Methods
This cross‐sectional study involved commercial drivers with complaints of nighttime driving difficulties (N = 80; mean age = 41.5 ± 11.1 years). A questionnaire was used to investigate nighttime driving performance following glare exposure. We measured contrast sensitivity and visual acuity under photopic conditions. With an experimental setup in a mesopic setting, we measured visual acuity with and without glare exposure. The difference between the two mesopic visual acuities was quantified as disability glare index. With the same setup, photostress recovery time was also measured. Regression analyses were used to determine the relationship between nighttime driving performance score and the measures taken in both photopic and mesopic settings.
Results
The average nighttime driving performance score was 47.8 ± 17.5. Driving performance was negatively correlated with all variables (R = –0.87 to –0.30, all p < .01), except contrast sensitivity (R = 0.74, p < .01). A multiple linear regression showed that the model with all variables explained 83.8% of the variance, but only disability glare index was a significant predictor of nighttime driving performance following glare exposure (standardized B = –0.61, p < .01).
Conclusion
Our results show that the change in mesopic visual acuities following glare can predict nighttime driving performance. This measure can be incorporated into the assessment of driving fitness by licensing departments to evaluate whether a person can drive safely at night amidst glare exposure.
Keywords: disability glare index, glare, night time driving performance, photostress
1. INTRODUCTION
Driving is indisputably a vision‐dependent task.1, 2 Driving performance, the ability to effectively maneuver a set of driving skills such as braking, staying in lane, perception of pedestrians and traffic, etc., requires the driver to have good vision. The issuance of drivers’ licenses is therefore contingent upon meeting visual standards established to ensure public safety and effective vehicle control.1 However, most licensing departments only assess visual acuity (VA) to determine visual fitness for driving even though there are different components of visual function. Other seldomly assessed components of visual function such as contrast sensitivity,3 glare sensitivity,4, 5 color vision,6, 7 and visual field8 reportedly impact driving performance significantly.
Driving performance can be severely impaired at night due to low (mesopic) illumination.9, 10 Visual challenges associated with nighttime driving is further worsened by the headlights of on‐coming vehicles.11, 12, 13, 14 Straylight from headlights can reduce retinal image contrast which manifests as either dazzling glare or scotomatic glare.13, 14, 15 Dazzling glare occurs when high illumination sweeps across the retina and induces light avoidance behavior such as squinting and looking away from the source of glare.11, 13, 16 Scotomatic glare, also known as photostress, involves reduced visual sensitivity following exposure to high illumination which rapidly bleaches and delays the restoration of retinal photopigments.13, 16 Previous studies assessed glare sensitivity with the disability glare index estimated as the difference between mesopic visual acuity measured with and without glare exposure.11, 17 The photostress recovery test,13, 16, 18 the time to regain visual sensitivity following glare exposure, can also be used to assess glare sensitivity. Considering that exposure to glare worsens nighttime driving performance and risks driving safety, it is important to assess glare sensitivity prior to issuing driver's licenses.
Even though a quarter of driving happen at night, a significant proportion of all road traffic accidents (RTA) occur during the dark hours.19, 20, 21, 22 The statistics for RTA, in general, is disproportionally worrisome for developing nations,23, 24 accounting for approximately 90% of cases worldwide. In Ghana, one of the RTA prone countries in Sub‐Saharan Africa, the prevalence of RTAs has been increasing over the last decade, with an estimate of over 900 cases per 100 000 population..21, 24, 25 An analysis of crashes between 2013 and 2017 in Ghana found that 67% of cases happened at night.26 In addition to severe injury outcomes, the risk of death was 1.3 times greater for nighttime RTAs compared to daytime RTAs. Apart from pedestrian casualties, commercially operated vehicles (COVs), which serve as a major means of transportation in Ghana, account for a substantial proportion of RTA occurrences in the country. In view of this, good vision is indispensable for COV drivers to drive safely during the day and at night. However, Driver and Vehicle Licensing Authority (DVLA) offices in Ghana currently do not perform glare assessment to determine visual fitness for driving at night. The purpose of this study was to examine the relationship of nighttime driving performance with disability glare index and photostress recovery time among COV drivers in the Cape Coast Metropolis of Ghana.
2. MATERIALS AND METHODS
2.1. Study design
This was a cross‐sectional study involving a survey of driving performance upon exposure to glare and an experimental setup for visual function and glare sensitivity assessment. The study followed the tenets of the Declaration of Helsinki and was approved by the Ethics Review Board of the University of Cape Coast (ID: UCCIRB/CHAS/2018/43). Similarly, approval was obtained from the leadership of the Ghana Private Road Transport Union (GPRTU) at the Tantri commercial lorry park/station in Cape Coast, Ghana. This was an ideal setting for the study because it is the largest COV park in the Cape Coast Metropolis and provided access to drivers plying all major roads in Ghana.
2.2. Participants
The list of all licensed COV drivers was obtained from the Tantri GPRTU. To be included in this study, we required drivers to have at least 6 months of nighttime driving experience as documented in the drivers’ log books maintained by the Drivers’ Union. We also required eligible participants to have complaints of visual challenges at night but no clinically significant visual impairment or presence of ocular disease. Drivers who had difficulties sleeping or used sleep medications were excluded from the study. Eighty drivers met our eligibility criterion and were included in the study. Written informed consent was obtained from all participants.
2.3. Assessment of driving performance under glare exposure
We developed a five‐item questionnaire to explore participants’ driving performance upon encountering glare from the headlight of on‐coming traffic with guidance from authorities (based on realistic local context easily understood by drivers) at the DVLA in Cape Coast. The questionnaire was administered by a research assistant and required participants to affirm whether they could recognize pedestrians, crossing animals, road signs, on‐coming vehicle, and road borders when exposed to glare while driving at night. An affirmative response to each item received a score of 20, otherwise, participants received a score of zero. The sum of the scores was computed as the driving performance under glare exposure (possible maximum score = 100). These five items are commonly used to evaluate driving performance.11, 27 We piloted the questionnaire on 15 drivers (not included the final study) and obtained a reliability coefficient of 0.82. The following additional information were obtained from participants: age, level of education, driving history, road safety literacy, and eyecare seeking habits.
2.4. Visual function and glare assessment
Comprehensive ocular health and vision examinations were to ensure that all participants had no eye abnormalities including early lens changes and met the minimum visual requirement for driving in Ghana (VA of 20/30 or 0.18 logMAR). A battery of tests was then performed under photopic and mesopic illuminations. Photopic tests were performed first and the order of testing under each lighting condition was randomized to minimize fatigue and memorization. These tests were performed binocularly and with participants’ habitual visual correction.
2.5. Measurements in photopic illumination
Photopic distance VA was measured using a LogMAR VA chart. The Pelli‐Robson chart (Clement Clarke International Ltd.) was used to assess the contrast sensitivity. Participants were encouraged to guess letters until a set of three letters on the same line were misidentified. Each correctly identified letter was assigned a unit score of 0.05 log (O and C letter were considered interchangeable). The illuminance level for photopic tests was 120 ± 10 cd/m2 (digital light meter yf‐170).
2.6. Glare assessment in mesopic illumination
Mesopic testing was done at illuminance level of 0.30 ± 0.10 cd/m2 (average of three repeated measures) which was consistent with previous studies (0.1–1.0 cd/m2).11, 28 Participants were allowed 10 min to adapt to the mesopic conditions.28, 29 To induce dazzling glare and photostress, we constructed an experimental setup that mimicked the Aston halometer. The Aston halometer employs a point source illumination which closely represents headlight glare from on‐coming traffic.11 The setup involved the headlight of a motorcycle (12V/35/35W) measuring 18 cm by 14.5 cm. The luminous intensity (E) of the motorcycle headlight source was 3000 cd/m2 and was comparable to the average luminous intensity of headlights of common vehicles that ply Ghanaian roads. The headlight was positioned at an angle (θ) of 9.8° from participants’ line of sight, 150 cm away from participants’ eye. With these parameters, the amount of glare (Lv) introduced into participants’ eye was 31.87 lux (computed using the Stile Holladay disability glare formula30: Lv = 10E/θ2). The setup has been illustrated in Figure 1.
FIGURE 1.
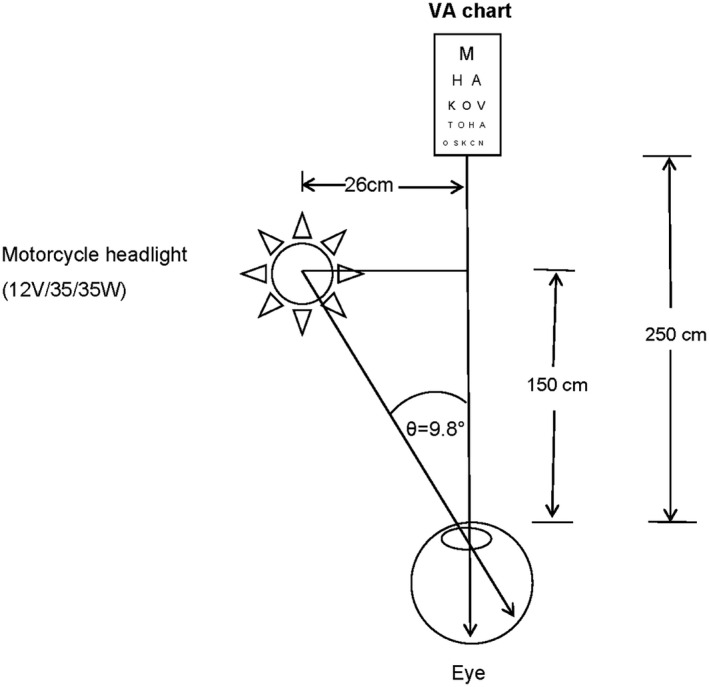
Illustration of experimental setup for glare assessment. The headlight was positioned on the left to represent the direction of glare source on Ghanaian roads
Under the mesopic illumination and with the glare source turned off, VA was measured using a decimal notation VA chart. This served as the baseline mesopic VA. We used the decimal notation chart to eliminate memorization of letters. The glare source positioned on the left side of the participant was turned on and VA was measured again. This was repeated after a five‐minute break to allow for restoration of baseline mesopic VA. The difference between VA taken without and with the glare source turned on was computed as the disability glare index.
With this setup, photostress recovery time was measured. Participants stared directly at the glare source for 10 seconds and then immediately switched to look at the decimal acuity chart. The time taken to read a line above the baseline mesopic VA was recorded as the photostress recovery time.16, 18 Estimation of the photostress recovery time was repeated after a five‐minute break. The mean of the two recovery times was used for the analysis.
2.7. Statistical analysis
Categorical variables were reported as frequencies, whereas mean and standard deviation (SD) were reported for continuous measures. The chi‐square test was used to assess the association between road targets and visual function parameter such as photopic VA, contrast sensitivity, DGI and mean PSRT. Linear regression models were used to investigate the relationship between driving performance and age, photopic VA, contrast sensitivity, disability glare index, and mean photostress recovery time. Significance level was set at 0.05. Data were analyzed using SPSS (version 26.0; IBM).
3. RESULTS
All study participants were males with median (interquartile range) of 39 (34–48) years. The highest level of education for all participants was Middle or Junior High School. Nine participants (11%) attended a driving school, the majority (51%), however, learnt driving through apprenticeship. All participants were compliant to the biennial renewal of driver's license regulation by the DVLA. The majority of participants (70%) reported they had eye examinations every two years, which usually coincided with the license renewal process. Participant's demographics and driving history have been summarized in Table 1. The mean (SD) value for contrast sensitivity was 1.88 (0.18) log units, 0.05 (0.10) logMAR for photopic VA, 0.14 (0.09) for baseline mesopic VA (decimal notation), 0.34 (0.09) for disability glare index (decimal notation) and 33.89 (9.90) seconds for photostress recovery time.
TABLE 1.
Participant's demographic and driving information
| Variable | |
|---|---|
| Median age (interquartile range), years | 39 (34–48) |
| N (%) | |
| Gender (male) | 80 (100) |
| Middle/Junior High School education | 80 (100) |
| Medium of training | |
| Driving school | 9 (11) |
| Apprenticeship | 41 (51) |
| Other | 30 (38) |
| Biennial renewal of license | 80 (100) |
| Frequency of road safety education | |
| Annually | 51 (64) |
| Biennially or more | 29 (36) |
| Frequency of eye examinations | |
| Annually | 4 (5) |
| Biennially | 56 (70) |
| Triennially or more | 20 (25) |
| HISTORY of RTA | |
| Yes | 5 (6) |
| No | 75 (94) |
| Mean (SD) | |
| Habitual VA (LogMAR) | 0.0 (0.1) |
| Years of driving | 14.8 (9.8) |
| Daily duration of nighttime driving | 3.5 (1.1) |
RTA, road traffic accident; SD, standard deviation
Table 2 presents the association between the detection of road targets and components of visual function including photopic VA, contrast sensitivity, DGI and mean PSRT. While mean PSRT was not significantly associated with detection of any target, DGI was significantly associated with road signs, road borders, and pedestrians. Figure 2 presents the proportion of participants who reported they could identify on‐coming vehicles, road signs, road borders, pedestrians, and crossing animals under glare exposure from on‐coming traffic during nighttime driving. Of these, the most frequently identified targets were approaching vehicles, followed by road signs, and crossing animals were the least frequently identified. The overall mean (SD) driving performance score under glare exposure was 47.8 (17.5). The mean driving performance score for the 5 participants who had a history of RTA was significantly lower than the remaining participants who had never been involved in an accident (22 vs. 47, p < .01). Whereas mean PSRT was not distinguishable between the two, the mean DGI value for participants with a history of RTA was greater than those who had no history of RTA (0.5 vs. 0.3, p < .01).
TABLE 2.
Association between the detection of targets and visual function assessed with chi‐square test
| Visual function parameters | ||||
|---|---|---|---|---|
| Targets | Photopic VA | Contrast sensitivity | DGI | Mean PSRT |
| On‐coming vehicles | 23.8 (p < .01) | 5.3 (p = .91) | 28.1 (p = .08) | 26.1 (p = .80) |
| Road signs | 25.1 (p < .01) | 41.8 (p < .01) | 67.1 (p < .01) | 33.7 (p = .43) |
| Road borders | 17.6 (p = .04) | 26.4 (p < .01) | 43.8 (p < .01) | 52.9 (p = .02) |
| Pedestrians | 29.2 (p < .01) | 19.0 (p = .06) | 40.0 (p = .02) | 37.9 (p = .25) |
| Crossing animals | 5.2 (p = .82) | 15.2 (p = .17) | 26.0 (p = .13) | 39.5 (p = .20) |
FIGURE 2.
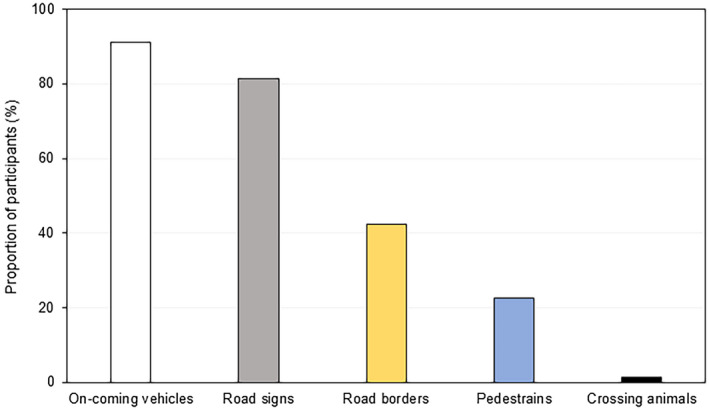
Bar graph showing the proportion of participants that could identify specific targets under glare exposure while driving at night
Figure 3 presents the relationship of nighttime driving performance with participants’ age (3A), contrast sensitivity (3B), photopic VA (3C), baseline mesopic VA (3D), disability glare index(3E), and photostress recovery time (3F). Driving performance was negatively correlated with all variables (R = –0.87 to –0.30, all p < .01), except contrast sensitivity (R = 0.74, p < .01). Multiple linear regression with all six variables yielded a significant model for predicting nighttime driving performance, F(6, 73) = 165.4, p < .01, and explained 92.6% of the variance. Table 3 shows a summary of the multiple regression analysis. With age and DGI as the only significant predictors, the predictive model for driving performance is estimated as (−0.33 * age) + (−0.60 * DGI) + 103.28.
FIGURE 3.
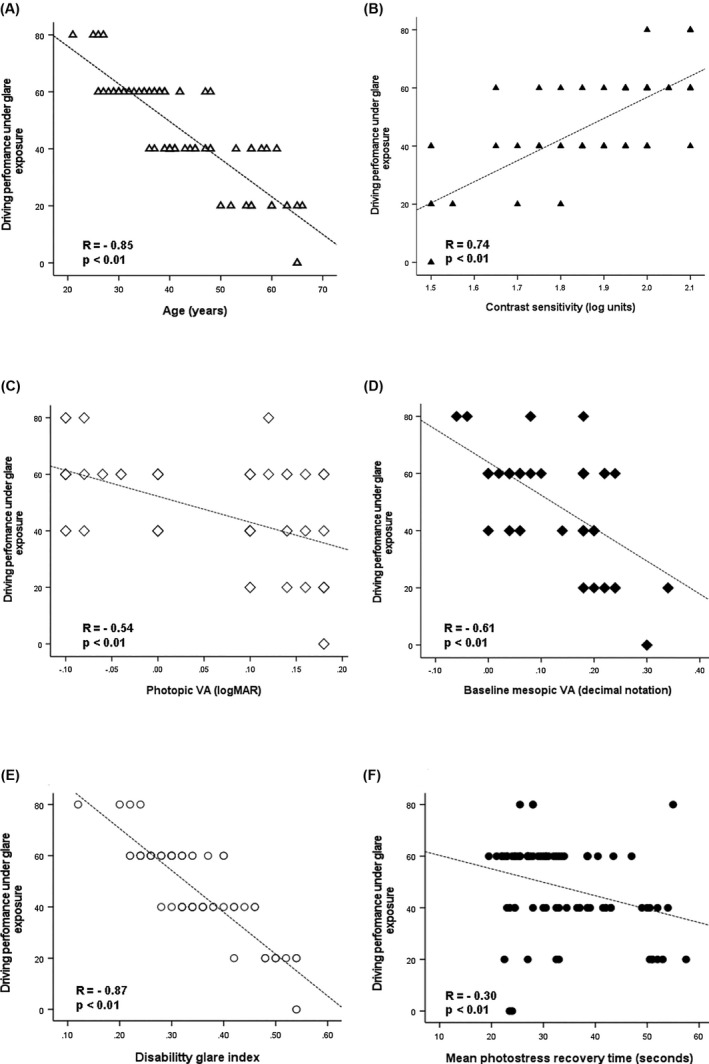
Scatter plots showing the relationship of nighttime driving performance under glare exposure with age (panel A), contrast sensitivity (panel B), photopic VA (panel C), baseline mesopic VA (panel D), disability glare index (panel E) and photostress recovery time (panel F)
TABLE 3.
Multiple regression analysis summary for predicting nighttime driving performance
| Parameter | Standardized slope (p‐value) |
|---|---|
| Age | −0.33 (<.01) |
| Contrast sensitivity | −0.02 (.82) |
| Photopic VA | −0.05 (.39) |
| Baseline mesopic VA | −0.11 (.06) |
| Disability glare index | −0.60 (<.01) |
| Photostress recovery time | −0.01 (.67) |
4. DISCUSSION
Nighttime driving can be very challenging for many drivers. In addition to reduced visibility at night, exposure to glare caused by the headlight of approaching vehicles significantly impacts driving performance and also increases the risk for RTA occurrences.14, 31 This study showed that the difference between mesopic visual acuities measured with and without a glare source (disability glare index) was a significant predictor of nighttime driver performance following exposure to glare. This finding suggests that the measurement of disability glare index in addition to photopic visual acuity provides an additional indicator for determining one's fitness to drive safely at night.
Currently, photopic VA is the only standardized test performed at DVLA offices in Ghana to determine whether one meets the visual requirement for driving.32 This assessment, however, does not provide a comprehensive evaluation of driving fitness, particularly for nighttime driving.33, 34 Separate regression analyses revealed that whereas 29.2% and 37.1% of the variance in nighttime driving performance were explained by photopic VA and baseline mesopic VA, respectively, disability glare accounted for 75.2% of the variance (Figure 3). Consequently, disability glare index or the change in mesopic VA following glare exposure remained the only significant determinant of driving performance upon encountering glare from an on‐coming vehicle. Our results are consistent with previous studies11, 33, 34 which showed that visual function assessments in low illumination were better predictors of nighttime driving performance than photopic assessments. This observation indicates that the incorporation of disability glare index estimation into driving fitness assessment may help identify licensed and potential drivers who may be at greater risk of getting involved in RTAs following exposure to glare from on‐coming traffic.
The impact of two clinical manifestations of glare were investigated in this study: dazzling glare and photostress. Although there was significant negative correlation (Figure 3F), the multivariate regression analysis (Table 3) showed that photostress recovery time was not a significant predictor of nighttime driving performance following glare exposure. This may be partly due to the fact that the participants included in the current study, of whom 50% were below 40 years, had no clinically significant pathologies. Studies have shown the presence of age‐related ocular diseases delays photostress recovery time beyond 60 seconds,18, 35, 36 however, the range of recovery time observed in this study was 19 to 57 seconds. Nonetheless, this finding is not sufficient to discount the relevance of photostress recovery time in determining visual capacity for nighttime driving because older drivers and those at greater risk of developing age‐related ocular problems may experience delayed restoration of visual sensitivity following exposure to high illumination.36, 37 Clinicians can therefore perform photostress recovery test in addition to the estimation of disability glare index to obtain a better appreciation of the risks faced by drivers with complaints of visual challenges at night. Clinicians may be guided by the predictive factor [(−0.33 * age) + (−0.60 * DGI) + 103.28] found in this study. This can help identify the appropriate interventions which will minimize the risks of getting involved in RTAs.
Road borders, pedestrians and crossing animals were reported as the most missed targets following glare exposure at night (Figure 2). In Kimlin et al, participants performed poorly at detecting pedestrians and road markings.11 Using simulated roadside targets, Theeuwes et al reported a significant reduction in the ability of drivers to detect pedestrians following exposure to glare.38 These observations translate into veering off driving lanes, crashing into road borders and knocking down of animals and humans. Whereas there are no effective measures to deal with glare from headlights, some approaches have proven to be useful. These include wearing of antireflective spectacles,36 use of polarized headlight systems,16 and wearing of reflective clothing by cyclists and pedestrians.37
A limitation of the current study is that driving performance was estimated using a structured questionnaire instead of driving simulator as has been described in previous studies.11, 35 We did not have access to a driving simulator due to technological constraints, therefore, we had to resort to using a survey. Some studies have used questionnaires successfully to assess driving performance and driving habits.10, 39 The results of the current study are, however, comparable to findings of previous studies11, 35 which employed driving simulators. While future studies may utilize an objective measure of nighttime driving performance upon glare exposure, an improved version of the current questionnaire can be adopted. The revised instrument should be limited to the items such as road signs, road borders, etc., which were strongly associated with visual function (Table 2). Additionally, item‐specific questions could be included to obtain a more accurate assessment of the impact of glare on driving performance. Similarly, several factors including poor visibility, fatigue and impaired driving due to sleep deprivation have been linked to RTAs at night. Our study concentrated on the relationship between visual parameters and RTAs. Future studies may have to consider the contribution of these other parameters to the occurrence of RTAs at night.
5. CONCLUSION
Glare caused by the headlight of on‐coming vehicles risks safe driving at night. Our results showed that among the different components visual function associated with driving performance, the change in mesopic visual acuity following glare exposure was the most significant determinant of whether drivers can identity other road users and targets at night. While an objective assessment of nighttime driving performance is needed, the findings of this study provide useful information that can be adopted by DVLA offices and clinicians to ascertain whether new drivers and those seeking license renewal are capable of driving safely at night. The evaluation of glare sensitivity could help curb the frequency of RTAs on Ghanaian roads.
DISCLOSURE
Approval of the research protocol: The study followed the tenets of the Declaration of Helsinki and all the methods were approved by the Institutional Review Board (IRB) of the University of Cape Coast, Ghana (ID: UCCIRB/CHAS/2018/43). Similarly, approval was obtained from the leadership of the Ghana Private Road Transport Union (GPRTU) at the Tantri commercial lorry park/station in Cape Coast, Ghana. Informed consent: Written informed consent was obtained from participants before the study. Registry and the registration no. of the study/trial: N/A. Animal Studies: N/A. Conflict of Interest: The authors declare no conflict of interest.
AUTHORS CONTRIBUTION
SBBK conceived the project. SBBK and EA drafted the project protocols; SBBK, EA, SH, and EKAM were involved in the data collection. SBBK, EA, and SLA were involved in analysis, interpretation, and drafted the original manuscript. All authors critically reviewed and approved the manuscript.
ACKNOWLEDGMENTS
The authors are grateful to the drivers who availed themselves for this study. We also appreciate the co‐operation of the leadership of the driver Unions who provided us with information in this study.
Boadi‐Kusi SB, Austin E, Abu SL, Holdbrook S, Morny EKA. Disability glare and nighttime driving performance among commercial drivers in Ghana. J Occup Health. 2021;63:e12279. 10.1002/1348-9585.12279
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author.
REFERENCES
- 1.Owsley C, McGwin G Jr. Vision and driving. Vision Res. 2010;50(23):2348‐2361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wood JM. 2015 Glenn A. Fry Award Lecture: driving toward a new vision: understanding the role of vision in driving. Optom Vis Sci. 2019;96(9):626‐636. [DOI] [PubMed] [Google Scholar]
- 3.Owsley C, Stalvey BT, Wells J, Sloane ME, McGwin G Jr. Visual risk factors for crash involvement in older drivers with cataract. Arch Ophthalmol. 2001;119(6):881‐887. [DOI] [PubMed] [Google Scholar]
- 4.Wood JM, Tyrrell RA, Chaparro A, Marszalek RP, Carberry TP, Chu BS. Even moderate visual impairments degrade drivers’ ability to see pedestrians at night. Invest Ophthalmol Vis Sci. 2012;53(6):2586‐2592. [DOI] [PubMed] [Google Scholar]
- 5.van den Berg TJTP, van Rijn LJ, Kaper‐Bongers R, et al. Disability glare in the aging eye. Assessment and impact on driving. J Optom. 2009;2(3):112‐118. [Google Scholar]
- 6.Boadi‐Kusi SB, Kyei S, Asare FA, Owusu‐Ansah A, Awuah A, Darko‐Takyi C. Visual function among commercial vehicle drivers in the central region of Ghana. J Optom. 2016;9(1):54‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Atchison DA, Pedersen CA, Dain SJ, Wood JM. Traffic signal color recognition is a problem for both protan and deutan color‐vision deficients. Hum Factors. 2003;45(3):495‐503. [DOI] [PubMed] [Google Scholar]
- 8.McGwin G Jr, Xie A, Mays A, et al. Visual field defects and the risk of motor vehicle collisions among patients with glaucoma. Invest Ophthalmol Vis Sci. 2005;46(12):4437‐4441. [DOI] [PubMed] [Google Scholar]
- 9.Wood JM. Nighttime driving: visual, lighting and visibility challenges. Ophthalmic Physiol Opt. 2020;40(2):187‐201. [DOI] [PubMed] [Google Scholar]
- 10.Puell MC, Palomo C, Sánchez‐Ramos C, Villena C. Mesopic contrast sensitivity in the presence or absence of glare in a large driver population. Graefes Arch Clin Exp Ophthalmol. 2004;242(9):755‐761. [DOI] [PubMed] [Google Scholar]
- 11.Kimlin JA, Black AA, Wood JM. Nighttime driving in older adults: effects of glare and association with mesopic visual function. Invest Ophthalmol Vis Sci. 2017;58(5):2796‐2803. [DOI] [PubMed] [Google Scholar]
- 12.Stafford Sewall AA, Whetsel Borzendowski SA, Tyrrell RA. The accuracy of drivers’ judgments of the effects of headlight glare on their own visual acuity. Perception. 2014;43(11):1203‐1213. [DOI] [PubMed] [Google Scholar]
- 13.Putnam C. Overview of glare types and their relationship with macular pigment optical density. Int J Approx Reason. 2017;5:1131‐1140. [Google Scholar]
- 14.Mainster MA, Timberlake GT. Why HID headlights bother older drivers. Br J Ophthalmol. 2003;87(1):113‐117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aslam TM, Haider D, Murray IJ. Principles of disability glare measurement: an ophthalmological perspective. Acta Ophthalmol Scand. 2007;85(4):354‐360. [DOI] [PubMed] [Google Scholar]
- 16.Mainster MA, Turner PL. Glare's causes, consequences, and clinical challenges after a century of ophthalmic study. Am J Ophthalmol. 2012;153(4):587‐593. [DOI] [PubMed] [Google Scholar]
- 17.Bailey IL, Bullimore MA. A new test for the evaluation of disability glare. Optom Vis Sci. 1991;68(12):911‐917. [DOI] [PubMed] [Google Scholar]
- 18.Glaser JS, Savino PJ, Sumers KD, McDonald SA, Knighton RW. The photostress recovery test in the clinical assessment of visual function. Am J Ophthalmol. 1977;83(2):255‐260. [DOI] [PubMed] [Google Scholar]
- 19.Sullivan JM, Flannagan MJ. The role of ambient light level in fatal crashes: inferences from daylight saving time transitions. Accid Anal Prev. 2002;34(4):487‐498. [DOI] [PubMed] [Google Scholar]
- 20.Plainis S, Murray IJ, Pallikaris IG. Road traffic casualties: understanding the night‐time death toll. Inj Prev. 2006;12(2):125‐128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ackaah W, Adonteng DO. Analysis of fatal road traffic crashes in Ghana. Int J Inj Contr Saf Promot. 2011;18(1):21‐27. [DOI] [PubMed] [Google Scholar]
- 22.Varghese C, Shankar U. Passenger Vehicle Occupant Fatalities by Day and Night – A Contrast. NHTSA, Traffic Safety Facts. 2007. http://www‐nrd.nhtsa.dot.gov/Pubs/810637.PDF. Accessed August 12, 2020. [Google Scholar]
- 23.WHO . Global Status Report on Road Safety 2018. WHO. 2018. https://www.who.int/publications‐detail‐redirect/9789241565684. Accessed August 21, 2020. [Google Scholar]
- 24.Adeloye D, Thompson JY, Akanbi MA, et al. The burden of road traffic crashes, injuries and deaths in Africa: a systematic review and meta‐analysis. Bull World Health Organ. 2016;94(7):510‐521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Siaw NA, Duodu E, Sarkodie SK, editors. Trends in road traffic accidents in Ghana; implications for improving road user safety. 2013. [Google Scholar]
- 26.Ackaah W, Apuseyine BA, Afukaar FK. Road traffic crashes at night‐time: characteristics and risk factors. Int J Inj Contr Saf Promot. 2020;27(3):392‐399. [DOI] [PubMed] [Google Scholar]
- 27.Ranney TA, Simmons LA, Masalonis AJ. Prolonged exposure to glare and driving time: effects on performance in a driving simulator. Accid Anal Prev. 1999;31(6):601‐610. [DOI] [PubMed] [Google Scholar]
- 28.Koefoed VF, Baste V, Roumes C, Høvding G. Contrast sensitivity measured by two different test methods in healthy, young adults with normal visual acuity. Acta Ophthalmol. 2015;93(2):154‐161. [DOI] [PubMed] [Google Scholar]
- 29.Sturr JF, Kline GE, Taub HA. Performance of young and older drivers on a static acuity test under photopic and mesopic luminance conditions. Hum Factors. 1990;32(1):1‐8. [DOI] [PubMed] [Google Scholar]
- 30.Vos JJ. On the cause of disability glare and its dependence on glare angle, age and ocular pigmentation. Clin Exp Optom. 2003;86(6):363‐370. [DOI] [PubMed] [Google Scholar]
- 31.Lachenmayr B, Berger J, Buser A, Keller O. Reduced visual capacity increases the risk of accidents in street traffic. Der Ophthalmologe. 1998;95(1):44‐50. [DOI] [PubMed] [Google Scholar]
- 32.Ovenseri‐Ogomo G, Adofo M. Poor vision, refractive errors and barriers to treatment among commercial vehicle drivers in the Cape Coast municipality. Afr Health Sci. 2011;11(1):97‐102. [PMC free article] [PubMed] [Google Scholar]
- 33.Wood JM, Owens DA. Standard measures of visual acuity do not predict drivers’ recognition performance under day or night conditions. Optom Vis Sci. 2005;82(8):698‐705. [DOI] [PubMed] [Google Scholar]
- 34.Gruber N, Mosimann UP, Müri RM, Nef T. Vision and night driving abilities of elderly drivers. Traffic Inj Prev. 2013;14(5):477‐485. [DOI] [PubMed] [Google Scholar]
- 35.Sandberg MA, Gaudio AR. Slow photostress recovery and disease severity in age‐related macular degeneration. Retina. 1995;15(5):407‐412. [DOI] [PubMed] [Google Scholar]
- 36.Rodriguez JD, Wallstrom G, Narayanan D, Welch D, Abelson MB. An alternative psychophysical diagnostic indicator of the aging eye. J Ophthalmol. 2019;2019:2036192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Messenio D, Marano G, Gerosa S, Iannelli F, Biganzoli EM. The influence of age on the recovery of the ERG photostress test. Doc Ophthalmol. 2013;126(2):87‐97. [DOI] [PubMed] [Google Scholar]
- 38.Theeuwes J, Alferdinck JWAM, Perel M. Relation between glare and driving performance. Hum Factors. 2002;44(1):95‐107. [DOI] [PubMed] [Google Scholar]
- 39.Kimlin JA, Black AA, Djaja N, Wood JM. Development and validation of a vision and night driving questionnaire. Ophthalmic Physiol Opt. 2016;36(4):465‐476. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.


