Abstract
Background and Aims:
Unpredictable difficult laryngoscopy remains a challenge for anaesthesiologists, especially in morbidly obese patients. The present study aimed to determine the efficacy of different sonographic measures as predictors of difficult laryngoscopy in morbidly obese patients undergoing elective surgery.
Methods:
This observational study evaluated 70 morbidly obese adult patients (body mass index >35 kg/m2) undergoing elective surgery under general anaesthesia with tracheal intubation. Pre-operative clinical and ultrasonographic variables (anterior condylar translation, tongue thickness, hyomental distance and oral cavity height) associated with difficult direct laryngoscopy ([Cormack Lehane (CL) grade>2]) were analysed. The primary outcome was to determine the efficacy of the above-mentioned sonographic measures as predictors of difficult laryngoscopy (CL grade >2). The secondary outcome compared ultrasonographic predictors with clinical predictors in morbidly obese patients for determining difficult direct laryngoscopy.
Results:
Amongst the primary outcome measures, limited condylar mobility (anterior condylar translation <9.25 mm) [odds ratio (OR) 0.3, confidence interval (CI):1.04-1.22;P<0.001;area under curve (AUC):0.8] and increased tongue thickness >5.85 cm [OR: 3.2, CI: 1.05–10; P < 0.04; AUC: 0.73] were two independent sonographic predictors for difficult direct laryngoscopy by multivariate logistic regression and receiver operating characteristic curve analyses in morbidly obese patients. The secondary outcome suggested that as compared to clinical predictors such as Mallampati grade and thyromental distance, ultrasonographic variables such as tongue thickness and limited condylar mobility (sensitivity: 56.4%, 70.9%, 66.7% and 93.3%, respectively) better predicted difficult direct laryngoscopy in morbidly obese patients.
Conclusion:
Limited condylar mobility and increased tongue thickness are independent sonographic predictors of difficult direct laryngoscopy in morbidly obese patients.
Keywords: Laryngoscopy; obesity, morbid; ultrasonography
INTRODUCTION
Morbid obesity is defined as body mass index (BMI) of >35 kg/m2 with associated comorbidity or >40 kg/m2 without significant comorbidity.[1] Obesity is associated with ischaemic heart disease, hypertension, diabetes and obstructive sleep apnoea, each adding to the risk of perioperative morbidity and mortality. Additionally, obesity is linked to 40%– 47% of airway mishaps causing difficulties in mask ventilation, laryngoscopy and intubation, both in operation theatres and intensive care units, respectively.[2] The incidence of difficult laryngoscopy in morbidly obese patients is 8.1%–31%.[3] This unpredictable difficult laryngoscopy remains a challenge in obese patients, especially if associated with difficult mask ventilation. Routine clinical screening tests such as the Mallampati score, inter-incisor distance, mento–hyoid distance and BMI have shown low sensitivity and specificity for prediction of difficult laryngoscopy with a limited predictive value.[4]
Airway assessment using ultrasound has been proposed recently as a simple bedside, easy-to-learn and non-invasive adjunct to clinical methods. Utility of airway ultrasound to predict difficult laryngoscopy using anterior neck soft tissue thickness, hyomental distance-related parameters and tongue parameters in submandibular view have been proven in general population[5,6] but have never been studied in morbidly obese patients.
The aim of the present study was to determine the efficacy of sonographic measures such as hyomental distance in neutral and extended positions, their ratio, tongue thickness (TT), width, TT to oral cavity height ratio, anterior neck soft tissue thickness at predefined levels and condylar mobility as predictors of difficult laryngoscopy (Cormack and Lehane grade >2) and their comparison with routine clinical screening tests in morbidly obese patients undergoing elective surgery under general anaesthesia.
METHODS
With the approval of the Institutional Ethics Committee (NK/5042/MD/527) and written informed consent, this prospective observational study included morbidly obese adults (>18 years) posted for elective surgery under general anaesthesia with tracheal intubation at a tertiary care academic institute from 17/3/2019 to 30/6/2020. Patients with previous history of major airway surgery/airway pathology, previous history of difficult laryngoscopy or intubation, pregnant, uncooperative patients, patients with cervical spine injury, limited neck mobility, neck swelling, buck teeth, dental braces, rheumatic disease and asymmetric mobility of the temporomandibular joint as in maxillofacial injuries/malignancies were excluded from the study. This study adheres to the applicable Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
Pre-operative evaluation was performed by an anaesthesiologist responsible for the case (A1) one day before surgery. Demographic variables were collected and clinical screening tests to predict difficult airway, such as upper lip bite test (ULBT), Mallampati grading, inter-incisor distance, neck circumference and thyromental distance, were noted. Fujifilm SonoSite M-turbo (Inc. Bothell, WA 98021 USA) system was used by an anaesthesiologist (A2) having expertise in airway ultrasound (performed >100 airway ultrasound scans) not involved in performing laryngoscopy. Ultrasound was performed at the submandibular level using 2–5-MHz curvilinear ultrasound probe, with the patient in supine position with head and neck elevated in ramp position with the help of pillows; with the examiner on the right side of the patient. Hyomental distance (HMD) in neutral (HMD-N) and extended (HMD-E) neck positions,[7] TT and oral cavity height (OCH) were measured by placing the probe in the mid-sagittal plane and the tongue width was measured by placing the probe in the transverse plane. Anterior neck soft tissue thickness was measured using 6–13-MHz linear ultrasound probe in transverse plane at the level of hyoid bone, cricoid and vocal cords. Anterior condylar translation was measured on the right side, at the level of zygomatic arch with ultrasound probe placed anterior to tragus and parallel to the zygomatic arch, and images were obtained with mouth open and closed. The position of the ultrasound probe was marked on the skin with a marker to prevent probe displacement. Two different ultrasound images were compared to see for anterior condylar translation, defined as the horizontal distance traversed by the condylar vertex from its baseline position in mouth closed vs final position in mouth open ultrasound image after the images were placed one below the other, with the help of image measurement tools. The average of three readings for anterior condylar translation was taken to reduce measurement bias, if any. Limited condylar mobility was defined as the value of anterior condylar translation that was lower than the prediction cut-off value for difficult laryngoscopy.
Standard monitoring, including 5-lead electrocardiogram (ECG), oxygen saturation (SpO2) end-tidal carbon dioxide (EtCO2), temperature and non-invasive blood pressure, was attached once the patient was inside the operation theatre. Patients were placed in the 'ramp' position achieved with pillows placed under their chest, head and neck until horizontal alignment between the sternal notch space and the external auditory meatus was achieved. Pre-oxygenation with 100% oxygen was done using a face mask for 3 minutes. General anaesthesia was induced using intravenous fentanyl based on lean body weight and intravenous propofol in titrated doses till the patient became unresponsive to verbal stimuli. Difficult mask ventilation was recorded if there was inadequate mask seal, use of assistance and desaturation (Spo2 <90%). Depolarising/non-depolarising muscle relaxant was used depending upon clinical assessment of the airway. Laryngoscopy with appropriate sized Macintosh blade was performed by an anaesthesiologist (A1) having >6 years of experience in airway management who was blinded to the airway ultrasound findings assessed by a separate anaesthesiologist (A2). External laryngeal manipulation allowed an optimal laryngeal view, and visualised Cormack and Lehane (CL) grade on laryngoscopy was noted. Patients were divided into two groups. CL grades 1 and 2 were included in the 'easy laryngoscopy' group whereas 3 and 4 were included in the 'difficult laryngoscopy' group. Trachea was intubated with an appropriate-sized endotracheal tube. Incidence of difficult mask ventilation/laryngoscopy, first attempt and overall successful intubation rate, rescue intubation by video-laryngoscope followed by fibreoptic bronchoscope and airway-related trauma were recorded.
The sample size of 70 was calculated using an incidence rate of difficult laryngoscopy (CL grade >2) of 22% (8.1%–31%) at 5% level of significance, 80% power and precision of 10%.[3,4] In total, 85 patients were enroled to account for possible dropouts. For the purpose of analysis, patients were grouped into easy and difficult laryngoscopy groups and predictors were expressed between these groups. Parametric data were analysed using the Student-t test and non-parametric data was analysed using the Mann–Whitney U test. The comparison of categorical variables between the groups was assessed by the Chi-square test, or in cases of a minimum expected count of less than 5, the Fisher exact test, and these values were reported as absolute numbers and percentages. Univariate and forward stepwise multivariate logistic regression analysis were performed to identify independent clinical and sonographic determinants of difficult laryngoscopy. P < 0.05 was considered as significant. Area under curve for receiver operating characteristics was calculated. Data were analysed using the computer statistical software system, Statistical package for the social science (SPSS) version 22.0 (SPSS, Chicago, IL).
RESULTS
A total of 85 patients were assessed for eligibility for enrolment in this prospective observational study. Data were analysed for 70 patients [Figure 1], out of which 79% (55) patients had easy laryngoscopy. The incidence of difficult laryngoscopy was 21% (15). Here, 80% of the patients with difficult laryngoscopy had difficult mask ventilation. Only 33% of the patients in the difficult laryngoscopy group could be intubated in the first attempt. Demographic parameters and clinical predictors are summarised in Table 1. The mean age of morbidly obese patients with easy laryngoscopy was lower [42.23 ± 12.05 vs 52.46 ± 12.11 (P = 0.005*)]. The easy laryngoscopy group had lower Mallampati (MMP) class values (P = 0.004*). Amongst the ultrasound parameters, a statistically significant difference in hyomental distance in neutral position [4.94 ± 0.69 vs 4.31 ± 0.73 cm; P = 0.003)*], hyomental distance in extension [5.52 ± 0.83 vs 4.75 ± 0.58 cm; P = 0.001*)], TT [5.12 ± 0.82 vs 5.69 ± 0.75 cm; P = 0.007*)] and condylar mobility [10.76 ± 2.04 vs 8.19 ± 1.79 mm; P = 0.001*)] was observed [Table 2]. Age, MMP grade, HMD-E, HMD-N, anterior condylar translation, OCH, anterior soft tissue neck at various levels and TT were analysed by multivariate logistic regression [Table 3] to determine the predictors of difficult laryngoscopy. Age, anterior condylar translation [Odds Ratio: 0.39 (1.04–1.22)] and TT [Odds Ratio: 3.2 (1.04–10.05)] were significant predictors of difficult laryngoscopy by multivariate logistic regression analysis. Receiver operating characteristic (ROC) curve analysis [Figure 2] was performed. Amongst the three parameters, the highest sensitivity of 93.3% and AUC of 0.80 was observed with anterior condylar translation, and TT had the highest specificity of 69.1% and AUC of 0.72 [Table 4]. At a cut-off value of 9.25 mm, anterior condylar translation was 93.3% sensitive and 67.3% specific for diagnosis of difficult laryngoscopy in morbidly obese patients. There were no episodes of desaturation and airway-related trauma in both groups.
Figure 1.
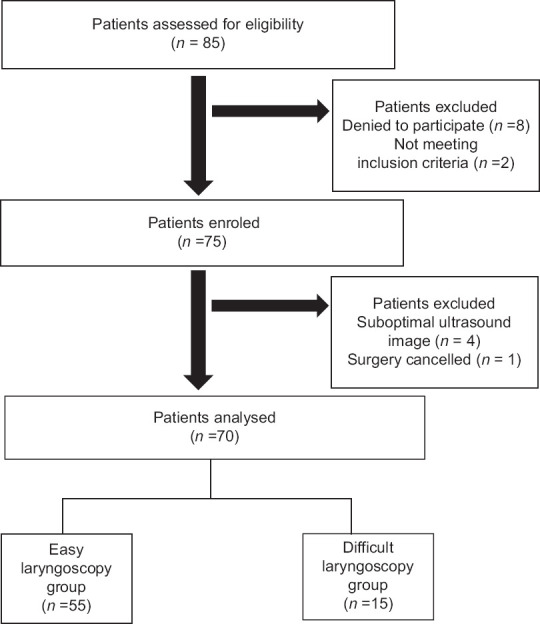
Study flow chart
Table 1.
Comparison of demographic profile and clinical predictors between easy and difficult laryngoscopy group
| Parameter | Easy laryngoscopy (n=55) | Difficult laryngoscopy (n=15) | P |
|---|---|---|---|
| Age (years)† | 42.23±12.05 | 52.46±12.11 | 0.005* |
| BMI (kg/m2)† | 41.33±5.27 | 43.06±6.70 | 0.286 |
| Gender (Male/female)‡ | 19/36 | 7/8 | 0.389 |
| Macroglossia‡ | 4/55 (7%) | 1/15 (6.6%) | 1.000 |
| MMP grade‡ | |||
| I | 8 (14.5%) | 0 (0%) | 0.004* |
| II | 23 (41.8%) | 4 (26.7%) | |
| III | 24 (43.6%) | 8 (53.3%) | |
| IV | 0 (0%) | 3 (20%) | |
| ULBT‡ | |||
| I | 54 (98.1%) | 13 (86.6%) | 0.114 |
| II | 1 (1.8%) | 2 (13.3%) | |
| Neck circumference† | 45.87±3.30 | 46.46±3.75 | 0.388 |
| IID† (cm) | 6.73±1.20 | 6.06±1.49 | 0.124 |
| TMD† (cm) | 8.39±1.16 | 7.87±0.99 | 0.071 |
BMI: Body Mass Index, ASA: American society of Anesthesiologists grading, MMP: Mallampati grade, ULBT: Upper lip bite test, IID: Interincisor distance, TMD: Thyromental distance. †Data expressed in mean±SD. Compared using Student’s t-test. ‡Data expressed in number. Compared using χ2 test and Fisher’s exact test as appropriate.*P≤0.05 is considered significant
Table 2.
Comparison of ultrasonographic parameters
| Ultrasonographic Parameters | Easy laryngoscopy (n=55) | Difficult laryngoscopy (n=15) | P |
|---|---|---|---|
| HMD-E (cm) | 5.52±0.83 | 4.75±0.58 | 0.001* |
| HMD-N (cm) | 4.94±0.69 | 4.31±0.73 | 0.003* |
| HMD-E/N | 1.10±0.10 | 1.13±0.14 | 0.496 |
| TT (cm) | 5.12±0.82 | 5.69±0.75 | 0.007* |
| TT/OCH | 0.86±0.08 | 0.90±0.05 | 0.026* |
| ANTERIOR CONDYLAR TRANSLATION (mm) | 10.76±2.04 | 8.19±1.79 | <0.001* |
| ASTN hyoid (cm) | 1.08±0.21 | 1.13±0.19 | 0.302 |
| ASTN cricoid (cm) | 1.12±0.25 | 1.04±0.25 | 0.226 |
| ASTN vocal cords (cm) | 1.09±0.25 | 1.17±0.31 | 0.337 |
HMD-E: Hyomental distance in extension, HMD-N: Hyomental distance in neutral neck position, HMD-E/N: HMD-E/HMD-N, TT: Tongue thickness, OCH: Oral cavity height, ASTN: Anterior soft tissue neck. The results are expressed as mean±SD and Student’s t test is applied.*P≤0.05 is considered significant
Table 3.
Unadjusted odds ratio using univariate logistic regression and Adjusted odds ratio using multivariate logistic regression
| Parameter | Univariate regression unadjusted odds ratio | Multivariate regression adjusted odds ratio | ||
|---|---|---|---|---|
|
|
|
|||
| OR (95% CI) | P | OR (95% CI) | P | |
| AGE | 1.104 (1.003-1.215) | 0.044* | 1.131 (0.222-0.686) | 0.004* |
| MMP | 4.501 (0.644-31.482) | 0.130 | - | - |
| HMD-E | 0.022 (0.000-1.320) | 0.068 | - | - |
| HMD-N | 23.504 (0.455-1215.174) | 0.117 | - | - |
| TT | 3.392 (1.062-10.832) | 0.039* | 3.247 (1.048-10.053) | 0.041* |
| Anterior condylar translation | 0.294 (0.120-0.722) | 0.008* | 0.390 (1.041-1.229) | 0.001* |
HMD-E: Hyomental distance in extension, HMD-N: Hyomental distance in neutral neck position, MMP: Mallampati grading, TT: Tongue thickness. *P≤0.05 is considered significant, OR-Odds ratio; CI-Confidence interval
Figure 2.
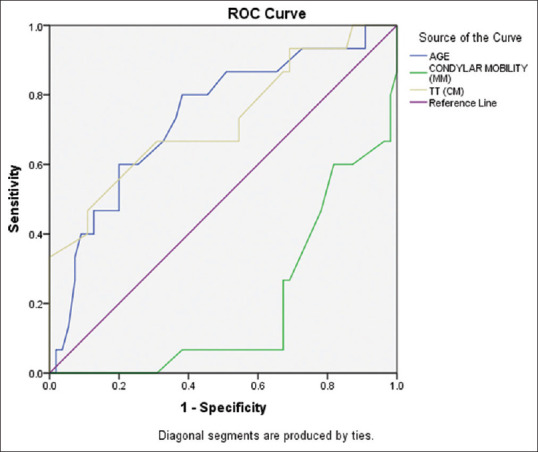
Receiver operating characteristic curve, shows the area under curve for condylar mobility (green), age (blue), TT (yellow line) and reference line (violet). Difficult laryngoscopy was taken as Cormack-Lehane grade >2. Higher values of age and tongue thickness are represented on the left side of the curve, and lower values of condylar mobility are represented on the right side of the curve predicting difficult laryngoscopy
Table 4.
Diagnostic validity of tests for predicting difficult laryngoscopy
| PARAMETER | CUT-OFF VALUE | SENSITIVITY | SPECIFICITY | AUC |
|---|---|---|---|---|
| Age (in years) | 45.5 | 80% | 61.8% | 0.736 |
| TT (cm) | 5.85 | 66.7% | 69.1% | 0.726 |
| Anterior condylar translation (mm) | 9.25 | 93.3% | 67.3% | 0.803 |
| TMD (cm) | 8.05 | 70.9% | 73.3% | _ |
| MMP grade | >2 | 56.4% | 73.3% | _ |
TT: Tongue thickness, TMD: Thyromental Distance, MMP: Mallampati grade, AUC: Area Under Curve
DISCUSSION
Our study showed that limited condylar mobility (defined by anterior condylar translation <9.25 mm) and increased TT were two independent ultrasonographic predictors for difficult direct laryngoscopy by multivariate logistic regression analyses in morbidly obese subjects. The study also suggested that as compared to clinical predictors such as MMP grade and thyromental distance, ultrasonographic variables such as TT and limited condylar mobility (sensitivity: 56.4%, 70.9%, 66.7% and 93.3%, respectively) predicted difficult direct laryngoscopy in morbidly obese subjects better. The current study is the first to suggest that limited condylar mobility had a 93% sensitivity and 67% specificity in predicting difficult direct laryngoscopy in morbidly obese subjects with odds ratio of 0.39 (1.04–1.22) and P < 0.001.
Condylar mobility measured ultrasonographically in our study measured only the anterior condylar translation of the temporomandibular joint. The temporomandibular joint has five different movements, namely sliding in anterior, inferior, lateral and medial planes as well as rotation at the condylar level.[8] Various clinical tests of difficult airway explored in the current study also assess mandibular mobility such as the inter-incisor distance test as well as the ULBT. While the inter-incisor distance test measured mouth opening with anteroinferior mandibular sliding movements and mandibular condylar rotation, the ULBT measured the anteroinferior sliding mandibular movements only.[8,9] An inter-incisor distance of <4 cm had a sensitivity of 20%; while a ULBT of >1 had a sensitivity of 13.33% for prediction of difficult laryngoscopy in the study population as compared to limited condylar mobility, which had a sensitivity of 93.3%. Limited condylar mobility also gave a more objective, accurate and reproducible measurement, which may be replicated in future studies than inter-incisor distance and ULBT at bedside, which may be more prone to subjective measurement errors. The ultrasound probe was kept at the level of zygomatic arch in our study for better measurement of the anterior horizontal distance traversed by mandibular condyles similar to the studies by Chen et al.[9] and Landes et al.[10]
Increased TT of >5.8 cm as measured by ultrasound in multivariate logistic regression analysis is also a good predictor of difficult direct laryngoscopy in morbidly obese subjects with an odds ratio of 3.2 {(1.05–10); P = 0.04}. Clinical tests used in the current study such as the modified MMP test also indirectly and subjectively grades tongue volume to oral cavity opening to an extent but are limited by mandatory tongue protrusion and limited predictive capability.[11] The sensitivity of predicting difficult direct laryngoscopy in morbidly obese patients is 66.7% with TT >5.8 cm as compared to 56% with MMP grade >2, thereby conferring superiority to objective measurement of TT by bedside ultrasound. Our results are similar to the studies by Yao and Wang[12] and Yadav et al.[13], where TT >6.1 cm was associated with difficult laryngoscopy and intubation in non-obese subjects. Contrasting to our study, tongue volume was not associated with difficult laryngoscopy in 12 obese subjects on submandibular sonography in a study by Wojtczak et al.,[14] due to bias created by small sample size. Authors also opined that tongue volume if expressed as a ratio to mandibular volume may be a predictor of difficult laryngoscopy in obese patients. Also, as laryngoscopy compresses the tongue, the compressed TT may be a better tool than TT alone to predict difficult laryngoscopy.
Other ultrasound predictors such as HMD-N, HMD-E and their ratio, anterior neck soft tissue thickness at various levels were not statistically significant predictors of difficult laryngoscopy on multivariate analysis in our study. Our results are in contrast to the results of Andruszkiewicz et al.[5] who reported HMD in extension to be a statistically significant ultrasound predictor of difficult laryngoscopy in the non-obese population. The difference is probably due to different study populations. It should also be noted here that HMD in extension, though significant in their study, had a low sensitivity of 38% even in the non-obese population, suggesting that if airway assessment is based on this predictor alone there is a high chance of missing patients with potentially difficult laryngoscopy. Our results are also in contrast with Yadav et al.[13] for anterior neck soft tissue thickness parameters, who studied normal patients as opposed to morbidly obese patients in our study. The neck circumference of our patients (45cm) was greater than that reported by Yadav et al (35cm) ; nevertheless Indian patients with morbid obesity may have a different distribution pattern for adipose tissue (back of neck) and only the front of neck regions were studied with ultrasound in our study.
In our study, the incidence of difficult laryngoscopy was 21% (n = 70). Moreover, 80% (12/15) of the patients with difficult laryngoscopy in the study population had difficult mask ventilation as well, underlining the importance of pre-operative prediction of difficult laryngoscopy by ultrasound predictors. This might indicate a need for preprocedural preparation of difficult airway cart by the cautious anaesthetist. Intubation with Macintosh blade failed in 5 out of 15 patients in difficult laryngoscopy group requiring rescue intubation with video-laryngoscope. Strengths of the current study include elimination of the observer bias as airway ultrasound and laryngoscopy were performed by two independent anaesthetists; use of 'ramp' position for morbidly obese patients, which led to lesser 'false high' CL grades in morbidly obese patients compared to standard laryngoscopy in 'sniff' position. TT was measured in the 'ramp' position, which correlated to the position assumed during laryngoscopic examination under anaesthesia in the study population. Laryngoscopy was done by an anaesthetist who was blinded to the airway ultrasound findings recorded by another experienced anaesthetist. Limitations of the current study include exclusion of patients with previous history of difficult laryngoscopy/intubation to avoid potential bias during clinical and ultrasonographic airway examinations. The current study does not identify the incidence of difficult intubation in morbidly obese patients. Difficult mask ventilation and difficult laryngoscopy may not always translate to difficult intubation. Condylar translation has anterior and inferior components. Only anterior condylar mobility was measured in the current study as condylar rotation can compensate for inferior condylar translation. Patients with pre-existing reduced temporomandibular mobility due to injury, ankylosis, arthritis and myofascial pain were not excluded. Small sample size and results narrowed to the Indian subcontinent are additional limitations of the study. Validation of the results of ultrasound findings with computed tomography or magnetic resonance imaging was not performed.
CONCLUSION
Limited condylar mobility and increased TT are independent sonographic predictors of difficult direct laryngoscopy in morbidly obese patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Lukosiute A, Karmali A, Cousins JM. Anaesthetic preparation of obese patients: Current status on optimal work-up. Curr Obes Rep. 2017;6:229–37. doi: 10.1007/s13679-017-0268-5. [DOI] [PubMed] [Google Scholar]
- 2.De Jong A, Molinari N, Pouzeratte Y, Verzilli D, Chanques G, Jung B, et al. Difficult intubation in obese patients: Incidence, risk factors, and complications in the operating theatre and in intensive care units. Br J Anaesth. 2015;114:297–306. doi: 10.1093/bja/aeu373. [DOI] [PubMed] [Google Scholar]
- 3.Özdilek A, Beyoglu CA, Erbabacan Ş E, Ekici B, Altinda Ş F, Vehid S, et al. Correlation of neck circumference with difficult mask ventilation and difficult laryngoscopy in morbidly obese patients: An observational study. Obes Surg. 2018;28:2860–7. doi: 10.1007/s11695-018-3263-3. [DOI] [PubMed] [Google Scholar]
- 4.Falcetta S, Cavallo S, Gabbanelli V, Pelaia P, Sorbello M, Zdravkovic I, et al. Evaluation of two neck ultrasound measurements as predictors of difficult direct laryngoscopy.A prospective observational study. Eur J Anaesthesiol. 2018;35:605–12. doi: 10.1097/EJA.0000000000000832. [DOI] [PubMed] [Google Scholar]
- 5.Andruszkiewicz P, Wojtczak J, Sobczyk D, Stach O, Kowalik I. Effectiveness and validity of sonographic upper airway evaluation to predict difficult laryngoscopy. J Ultrasound Med. 2016;35:2243–52. doi: 10.7863/ultra.15.11098. [DOI] [PubMed] [Google Scholar]
- 6.Yao W, Zhou Y, Wang B, Yu T, Shen Z, Wu H, et al. Can mandibular condylar mobility sonography measurements predict difficult laryngoscopy? Anesth Analg. 2017;124:800–6. doi: 10.1213/ANE.0000000000001528. [DOI] [PubMed] [Google Scholar]
- 7.Koundal V, Rana S, Thakur R, Chauhan V, Ekke S, Kumar M. The usefulness of Point of Care Ultrasound (POCUS) in pre-anaesthetic airway assessment. Indian J Anaesth. 2019;63:1022–8. doi: 10.4103/ija.IJA_492_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Travers KH, Buschang PH, Hayasaki H, Throckmorton GS. Associations between incisor and mandibular condylar movements during maximum mouth opening in humans. Arch Oral Biol. 2000;45:267–75. doi: 10.1016/s0003-9969(99)00140-5. [DOI] [PubMed] [Google Scholar]
- 9.Chen HY, Wu SK, Lu CC, You JY, Lai CL. Assessing the mobility of the mandibular condyle by sonography. Patient Prefer Adherence. 2014;8:1419–25. doi: 10.2147/PPA.S72532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Landes CA, Sader R. Sonographic evaluation of the ranges of condylar translation and of temporomandibular joint space as well as first comparison with symptomatic joints. J Craniomaxillofac Surg. 2007;35:374–81. doi: 10.1016/j.jcms.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 11.Lundstrom LH, Vester-Andersen M, Møller AM, Charuluxananan S, L'Hermite J, Wetterslev J. Poor prognostic value of the modified Mallampati score: A meta-analysis involving 177 088 patients. Br J Anaesth. 2011;107:659–67. doi: 10.1093/bja/aer292. [DOI] [PubMed] [Google Scholar]
- 12.Yao W, Wang B. Can tongue thickness measured by ultrasonography predict difficult tracheal intubation? Br J Anaesth. 2017;118:601–9. doi: 10.1093/bja/aex051. [DOI] [PubMed] [Google Scholar]
- 13.Yadav NK, Rudingwa P, Mishra SK, Pannerselvam S. Ultrasound measurement of anterior neck soft tissue and tongue thickness to predict difficult laryngoscopy: An observational analytical study. Indian J Anaesth. 2019;63:629–34. doi: 10.4103/ija.IJA_270_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wojtczak JA. Submandibular sonography: Assessment of Hyomental distances and ratio, tongue size, and floor of the mouth musculature using portable sonography. J Ultrasound Med. 2012;31:523–8. doi: 10.7863/jum.2012.31.4.523. [DOI] [PubMed] [Google Scholar]


