Abstract
Patient-provider communication plays a major role in healthcare with its main goal being to improve the patient’s health and build a trustworthy relationship between the patient and the doctor. Provider’s efficiency and effectiveness in communication can be improved through training in order to meet the essential elements of communication that are relevant during medical encounters. We surmised that speech-enabled conversational agents could be used as a training tool. In this study, we propose designing an ontology-based interaction model that can direct software agents to train dental and medical students. We transformed sample scenario scripts into a formalized ontology training model that links utterances of the user and the machine that expresses patient-provider communication. We created two instance-based models from the ontology to test the operational execution of the model using a prototype software engine. The assessment revealed that the dialogue engine was able to handle about 62% of the dialogue links. Future direction of this work will focus on further enhancing and capturing the features of patient-provider communication, and eventual deployment for pilot testing.
Keywords: Ontology, Training, Dental education, Patient-provider communication, Conversational agent, Dialogue management
1. Introduction
Good patient-provider communication is an essential aspect of high-quality healthcare. It is a characteristic of clinical expertise that proves to be beneficial to both the provider and the patient. There is evidence that providers and patients do not communicate well and there is always a chance for possible misunderstandings [1]. Several misunderstandings that arise between providers and patients may be solved through a good rapport and communication. Inadequate provider-patient communication has been attributed to one of the root causes of increased violence in workplaces [2]. A rise in the lawsuits against doctors has been seen over the years and evidence has shown that poor communication between the provider and patient is an attributing factor [3, 4].
A good physician/dentist-patient communication greatly improves a patient’s susceptibility to understand and follow the provider’s instructions. This results in a reduction in patient anxiety, and an increase in patient satisfaction and adherence to healthy behaviors [5, 6], eventually leading to the desired treatment outcome. In a study done by Hall et al, they analyzed various outcomes of provider communication and found “adherence” to be a predictable outcome from good physician information delivery and more positive discussion [7]. Patient adherence is seen to be significantly related to provider-patient communication and that adherence, can be enhanced when a provider has undergone a training to be a better communicator [6]. The result of the analysis done by Zolnierek et al, showed that, “patients of physicians who communicate well have 19% higher adherence, and training physicians in communication skills improves patient adherence by 12%” [6]. Therefore, communication proves to be an essential component of healthcare as shall be seen for both the dental and medical field.
1.1. Training in Patient-Provider Communication
Effective communication is an essential element of medical care and should be a priority of medical education. According to Hausberg and colleagues, “[c]ommunication can be seen as the main ingredient in medical care” [8]. Professionalism being a fundamental aspect of good medical practice also demands not only knowledge and competence but also effective communication skill [9, 10]. As physicians progress from students to experts, their competence level has to expand as well from conducting generic communication task to successfully handling complex and demanding situations [11, 12] such as interacting with angry patients or families [13].
Medical students focus more on hands-on experiences to ameliorate their clinical skills and pay less attention to their communication skills. There is evidence that students’ communication skills depreciate over time especially during their clinical years [14] and teaching these skill is neglected during those years [15]. Communication training is critical and may even be more important in residency training [16]. Medical students communication skills are indispensable when looking into their clinical competence [17], and “[c]ompetence in interpersonal skills should be demonstrated through sustained therapeutic patient relationships and in balancing the biotechnical and inter- personal aspects of care” [13]. Training medical students builds good communication skills during their formative years, and serves as an investment towards making good future practitioners [18]. These skills can be learned during training and perfected over the years.
1.2. Effect of Patient-Provider Communication
Patients need to have a good understanding of their disease, the associated risk and the benefit of consistent treatment in order to have improved healthcare outcomes. It is important to understand the “preferences”, “beliefs” and “perspectives” [19] of patient during health evaluations so as to have a positive discussion and good information exchange. According to Epstein et al, physician-patient communication provides a means to manage the patient’s uncertainty, address emotions, decision making [20] all contributing to a better understanding of the prognosis given [21]. Effective communication during patient consultation including history-taking and care planning has been positively correlated with emotional health, symptom management and pain control [22].
When there is a lack or poor communication between a provider and a patient, there is a higher chance of errors. Symptoms affecting patients may be missed or underestimated during consultations [23], which could potentially be attributed to lack of efficient communication between the physician and the patient. Experts estimate that approximately 98,000 people die in any given year from medical errors occurring in hospitals [24]. Before completing their education, physicians should demonstrate an ability to apply the essential skills of communication in a wide range of clinical situations. They should also be able to recognize and repair communication errors quickly [25].
Dental patient’s satisfaction relies greatly on the relationship developed with their providers. A large portion of this relationship entails efficient communication and the quality of this communication is closely related to the overall patient satisfaction [26]. According to Bansal et al, quality of care depends on two major concepts which includes patient perspective and satisfaction [27]. Patients do not asses the medical competence of a provider; however, the experience they have during the process of care highlights their perception regarding the quality of the care they receive [28]. For a patient, what counts most in a provider-patient communication process is having a sense of partaking in the treatment process and a feeling of having their needs fully understood by the provider [29]. A good patient–provider communication should be able to give a patient that control they want over their illness [30] and treatment, while receiving comfort and support from the provider [31].
Dental providers differ from each other and patients are faced with a variety of providers to choose from. Every patient has preferences they take into consideration when selecting their ideal dental provider and these preferences are drawn by the dentist ability to “express empathy, manage pain and have good communication skill” [32]. Communication is mandatory in attaining patient satisfaction and has equal importance to a patient as the technical skill of the provider [33].
1.3. Ontology and Intelligent Agent Research
The canonical definition of ontologies is attributed to Gruber’s, “an explicit specification of a conceptualization” through the use of binding concepts with expressive relationships for use by agents [34]. According to Feilmayr and Wöß, “[a]n ontology is a formal, explicit specification of a shared conceptualization that is characterized by high semantic expressiveness required for increased complexity” [35]. Ontologies are artifacts that represents domain knowledge using semantic web syntax languages expressed through OWL [36] and RDF [37, 38]. Using the syntax, we can encode high level concepts and logic, and then publish the artifact which can be shared and reused. Devices (i.e., agents) can read these artifacts and be able to conceptualize domain knowledge, thereby being able to perform reasoning capabilities and act upon that domain knowledge.
Some of the capabilities that are yielded through ontologies include facilitating exchange, sharing and standardization of data; providing support for natural language processing tools; represent complex information; and elicit machine reasoning using the “built-in” semantics of the artifacts.
The field of artificial intelligence (AI) research branches out to several categories – knowledge representation, natural language understanding, learning, search, inference, planning and problem solving, and vision [39]. Ontologies have wide-ranging impact on a few of the branches, most notability on knowledge representation, inference, and, within the context of the paper, planning and problem solving. Knowledge representation involves modeling physical and logical entities (e.g., using semantics and first order logic) and using these models to furnish meaning and understanding for agents. Inference involves producing missing or new information from available sources through logical reasoning. The machine reasoning from ontologies is capable of identifying categories of data, and analyzing logical consistency of the knowledge base. Agents that use the machine reasoning from ontologies are able to understand the meaning of concepts from the domain.
Planning and problem solving is another major topic in AI research. This topic involves a computational agent’s use of deliberation to devise a plan for the agent to act on and then devising steps to perform the chosen act. This is accomplished through developing formal computational models for planning and reacting, and then developing technologies that support and implement the models. Overall goals of this area are to equip the computational agent with autonomous or automated behavior to preform intended tasks, and contribute to the ability to interact with a highly variable environment to account for scenarios unanticipated by the designers of the agent.
There exists some potential in utilizing ontologies for automated planning research [40–52]. Within a planning domain there exist objects (agents, non-agent things, etc.), plans and its goals, and the actions to enact those plans. As an artifact that represents the concepts in a domain, it can model and reason objects, actions, plans, and goals of a planning domain [40]. With the representational and inferencing ability, ontologies could potentially automate a specific interaction domain space between user and machine.
1.4. Utilizing Technology for Training Medical and Dental Students
In the last decades, there has been an unprecedented increase in the role of technology in healthcare at different levels. There are different aspects of technology that can train a medical student into becoming a well-rounded physician. These new teachings/ training technologies cover the vast spectrum of healthcare. For example; “virtual patient (VP) simulation training to support certain aspects of clinical education” [53], “devices for initial training of combat medics and first responders, devices for training surgical procedures, virtual reality systems for diagnosis and therapy, and team training systems for crisis or incident management” [54] which have being increasingly adopted.
In teaching communication skills in specific to prospective providers, virtual humans are frequently used during training, as they can provide a standardized experience for all students [55]. In the study done by Wiehagen, he proposed and focused on four categories of medical simulation devices for improving provider training. They included “PC-Based Interactive Systems, Digitally Enhanced Mannequins, Virtual Workbenches, and Total Immersion Virtual Reality” [54]. He further discussed on the limitations of these devices with some of them being the expensive and complex nature of the simulators. The findings in the study done by Yedidia suggest that medical schools that commit to incorporating communications training can expect improved student performance in regards to patient care [56]. Regardless of the prevalent acknowledgment of the importance of improved patient-provider communication, training in communications skills has not been thoroughly incorporated into most medical school curricula [57, 58] nor has it been subjected to evaluation across different schools [59].
Future providers should be able to communicate information, risk involved, and any uncertainty in ways that patients can understand and engage the patients when necessary in decisions taking [1]. Communication is a skill that can be taught in many different ways to future healthcare providers. For example, Stevens et al. developed a virtual standardized patient to teach students on developing their communication skills [60]. Also, actors are presently used to train University of Texas dental students at a cost greater than $100 per actor [61].
One takeaway based on our scoping review is the cost to deploy technology-based training. Another is the minimal initiative and research for standardizing the technology-based training for medical and dental students. Lastly, using technology to train these students (while not expansively used) has shown some promise in preparing the students for the challenges of patient-provider communication. To address some of these gaps we introduce the use of speech-based conversational agents (computational software that can automate discourse with consumers) that can be utilized to train dental and medical students to experience some aspects of patient-provider communication, and work towards ameliorating the communication skill of healthcare providers thereby building trust and overall satisfaction to both the patient and the provider; and provide a reusable and economical tool for medical training.
Noted earlier, the objectives of automated planning research are to develop computational models to implement self-directed deliberation and develop software and hardware to support the models. This project embarks on creating computational models through the use of ontologies to formalize patient-provider training and execute the models through a software agent engine using the ontology models. The impact of this work could lead us toward the deployment of our model-driven implementation that can improve communication efforts between patient and provider, reduce cost in training, and possibly standardize training to where the models can be shared and reused.
2. Methods and Tools
2.1. Ontology Framework for Health Communication
In our earlier work, we developed an ontology called Patient Health Information Dialogue Ontology (PHIDO) [62] that was conceived from data and dialogue flows from a Wizard of OZ study for patient-provider communication of vaccine counseling [63, 64]. The ontology provided a foundation to construct chains of utterances (Speech Tasks) and linking those chains to other chains to form network graph conversations. Figure 1 shows an explanation of the structure of the ontology model.
Fig. 1.
Structure of Patient Health Information Dialogue Ontology. Dotted ellipses are example sub-classes.
PHIDO’s basic structure include a Communication Goal, which is a general goal for the machine to communicate. This class concept can be subclassed to specific communication goals for the agent to implement. For example, the Communication Goal can be subclassed to Communicate Benefits of Yearly Check-ups to encompass various speech tasks to fulfill the goal of communicating advantages of seeing one’s dentist on a year basis.
The CommunicationGoal has speech tasks (SpeechTasks) connected through an object property of hasSpeechTasks. These SpeechTasks comprise of several sub-goals to fulfill their communication goal. Some of these tasks could be essential (answering patient questions, pleasantry interaction) or trivial tasks (repeating an utterance, requesting a repeat). Additionally, the SpeechTasks are comprised of linked utterances (Utterance) that are connected to hasUtterance. Each Utterance are linked with utteranceLink object property, which has sub-object properties of follow and precedes that are inverses of each other. The important utterances within the dialogue flow of this model are ParticipantUtterance (the utterance of the human user) and SystemUtterance (the utterance of the agent). Every Utterance is associated with hasUtteranceString (string text of what is to be evoked), hasUtteranceExample (sample utterances of that type of Utterance), and hasFocus (Boolean flag to indicate the position of the dialogue conversation). These links of Utterances models the network representation of the dialogue flow that we will discuss in the later sections. Overall, the PHIDO ontology model serves as a domain knowledge base fora specific type of health conversation with a consumer.
2.2. Ontology-Driven Software Engine for Conversational Agents
In a later study, we developed a software engine that uses the PHIDO model to reason and manage the health dialogue strategies [65]. This software engine is named Conversational Ontology Operator (COO). The engine is a software wrapper that is composed of various software libraries – Stanford Core NLP [66], OWL-API [67], rdf4j [68], Hermit reasoner library [69], and some utility libraries. This engine aims to automate the dialogue interaction between a consumer and the agent. The automation of the dialogue is directed by the PHIDO model that maps out the potential sequences of utterances.
Figure 2 shows a brief description of the software engine’s process of utilizing the Utterance classes and updating the position of the dialogue. The COO, the software engine, in tandem with the PHIDO model begins at an Utterance that has hasFocus flagged to true. The software engine determines what the next Utterance type is. If the Utterance type is a SystemUtterance, the next Utterance sends the hasUtterance data string to the natural language interface, and then updates the SystemUtterance as the current Utterance by setting the hasFocus to true. If it is not, it captures input from the natural language interface and matches the input with two or more possible ParticipantUtterances. Once the engine finds the probable ParticipantUtterance, it flags the probable Participant Utterance’s hasFocus to true. This basic process loops through continuously. More detailed treatment of the process is provided in our previous work [65].
Fig. 2.
Activity diagram showing the software engine loop’s process of deciding the next steps in the dialogue interaction.
Compared to our previous efforts, the software engine initiates and directs the conversation mainly due to the ontology model representing a dialogue interaction as an expert in a health topic and the user as the passive consumer. In this effort, the software engine will be the passive actor in the interaction with the consumer, who is the domain expert (dental student). The system will be reliant on the dental student consumer to initiate and propel the conversation. To do this, we will create our PHIDO model to reflect this interaction, and the software engine will utilize the model to preform interaction decisions for dialogue.
2.3. Modeling Training Dialogue Interaction
In collaboration with the University of Texas Health Science Center’s School of Dentistry, we were provided with sample training dialogue scenario scripts based on fictious personas representing a fictional archetype, essentially eight individual fictious patients. These eight training dialogue scripts were previously used in an experimental undergraduate project [61]. We drafted flow charts for each individual dialogue script using draw.io [70]. We qualitatively analyzed each of the drafted flow charts and attempted to find some common patterns that were shared in the charts. From our analysis, we derived and drafted a meta-level flow chart that captures the core interaction from the scripts. We also developed a list of Utterance types from our review of the script and assigned basic Utterance types to the meta-level flow chart. Table 1 shows the complete list of the Utterances classes specific to this domain, along with their association to the ParticipantUtterance and the SystemUtterance classes of PHIDO. Each specific ParticipantUtterance inquiries were paired with corresponding SystemUtterances. For example, an utterance that was Oral_cancer_history_inquiry (e.g., “Do you have a history of oral cancer in your family?”) corresponds to an Oral_cancer_history_information response (e.g., “My father had oral cancer some years ago before he passed away..”).
Table 1.
Classification of the utterance pairs with sample descriptions. The colon(s) indicates depth of the class within the hierarchy.
| ParticipantUtterance | SystemUtterance | Explanation/Example from script |
|---|---|---|
| Persona_health_inquiry | Persona_health_information | Patient’s General care “Please tell me your height and weight”, “patient’s vital signs” |
| :Confirmation_of_persona_health_information | Affirmative response to any inquiry. Applicable to any inquiry “Yes”, “Ok” |
|
| :Disconfirmation_of_persona_health_information | Dissenting response to any inquiry. Applicable to any inquiry. “No”, “Sorry I don’t …” |
|
| :Persona_Dental_Health_inquiry | :Persona_Dental_Health_information | Questions specific to dental health “Tell me more about your toothache.” |
| ::Aesthetic_inquiry | ::Aesthetic_information | Questions about appearance of teeth “Are you unhappy with the way your smile or how your teeth look or feel?”, “Have you had your teeth Whitened before?” |
| ::Anesthetic_inquiry | ::Anesthetic_information | Questions about Anesthesia “Problems in past with local anesthetic?” |
| ::Dental_Habit_inquiry | ::Dental_Habit_information | Questions about Patient’s involuntary dental habits. “Do you habitually clench or grind teeth during the day or night?” |
| ::Oral_cancer_history_inquiry | ::Oral_cancer_history_information | Patient’s and family history of oral cancer “Do you have a history of oral cancer in your family?” |
| ::Oral_Dental_Appliance_inquiry | ::Oral_Dental_Appliance_information | Questions about present or past usage of oral appliance. “Yes, presently I am wearing my orthodontic retainers well…when I remember to wear them.” |
| ::Prior_Dental_Visit_inquiry | ::Prior_Dental_Visit_information | Questions about past dental visits. “And do you remember what you had done the last time you saw a dentist?” |
| Persona_General_Health_inquiry | :Persona_General_Health_informtion | Questions about patient’s current status on health “Are you currently under the care of a physician?” |
| ::Allergy_inquiry | ::Allergy_information | Questions about patient’s allergies. “Do you have any allergies (i.e., medications, foods, latex, cosmetics, and metals)?” |
| ::Cancer_history_inquiry | ::Cancer_history_information | Questions about previous or current cancer diagnosis. “What cancer were you diagnosed with?” |
| ::Cardiovascular_inquiry | ::Cardiovascular_information | Question relating to the heart “What treatment have you had for CAD (Coronary Artery Disease)?”, “Do you have a pace maker?” |
| ::Dermatological_inquiry | ::Dermatological_information | Questions about skin conditions “Have you been diagnosed with any skin conditions?” |
| ::Diabetic_History_inquiry | ::Diabetic_History_information | Questions about diabetes “Do you have a first-degree relative with diabetes?” |
| ::Endocrine_question | ::Endocrine_information | Questions regarding the Endocrine system (glands) “Have you been diagnosed with any of the following conditions; Frequent thirst, Frequent urination?” |
| ::Family_history_inquiry | ::Family_history_information | Questions about diseases that run in patient’s family “Do you have any diseases or medical problems that run in your family (i.e., arthritis, diabetes, cancer, cardiovascular disease)?” |
| ::HEENT_inquiry | ::HEENT_information | Questions about Head, eyes, ears, nose, throat. “Have you been diagnosed with any of the following conditions? Head injury, Vision problems, Hearing, impairment, Allergic rhinitis, Chronic sinusitis” |
| ::Hematological_Inquiry | ::Hematological_information | Questions relating to blood disorders “Have you been diagnosed with any of the following conditions like Bleeding Disorders:” |
| ::Immunological_inquiry | ::Immunological_information | Questions regarding immune system. “Have you been diagnosed with an autoimmune disease?” |
| ::Medication_inquiry | ::Medication_information | Regarding patient’s current medication status. “Are you currently taking any prescription medications?” |
| :::Medication_dosage_inquiry | :::Medication_dosage_information | Questions about dosage of medication patient is currently taking. “Can you tell me the doses for each medication you’re taking?” |
| ::Musculoskeletal_inquiry | ::Musculoskeletal_information | Question relating to the skeletal system “Have you been diagnosed with any of the following conditions? Arthritis, Osteoporosis, Gout, Other musculoskeletal disorders…” |
| ::Neurological_and_Psychiatric_Inquiry | ::Neurological_and_Psychiatric_information | Questions regarding to patient’s mental state. “What form of depression have you been diagnosed with?” |
| ::Obstetric_and_Gynecological_inquiry | ::Obstetric_and_Gynecological_information | Questions regarding child bearing “Are you pregnant or think you might be pregnant?” |
| ::Physical_activity_and_Diet_inquiry | ::Physical_activity_and_Diet_information | Question regarding patients physical activity and diet “What’s your diet and physical activity like?” |
| ::Previous_surgery_inquiry | ::Previous_surgery_information | Past surgeries done. “I’ve had 3 surgeries for my melanoma, the first in January 1997…” |
| ::Renal_and_Gastrointestinal_inquiry | ::Renal_and_Gastrointestinal_information | Questions about kidneys/ relating to stomach and intestines “Have you been diagnosed with any of the following conditions? Renal failure or Insufficiency, Kidney stones/Stomach or duodenal ulcer, Crohn’s disease”, |
| ::Respiratory_Inquiry | ::Respiratory_information | Questions relating to respiratory system. “Do you presently suffer from any of the following? Chest pain exacerbated by deep breathing, Cough, Difficulty breathing, Sleep apnea/snoring, Wheezing” |
| ::Sexually_transmitted_disease_inquiry | ::Sexually_transmitted_disease_information | Questions about infectious diseases (STD) “Have you been diagnosed with any sexually transmitted disease such as Syphilis, HIV, or Herpes?” |
| ::Social_Behavioral_inquiry | ::Social_Behavioral_information | Questions regarding patient’s leisure activities. “Do you smoke or consume tobacco?” |
In Fig. 3, we show the meta-level abstraction that models the basic dialogue interaction from our review of the dialogue scripts and charts. The dialogue interaction initiates with the Participant Introduction Utterance (“Hello, we will be completing your dental history today”). If the software engine does not capture the participant input, or if the input does not match any of the next Utterances, the PHIDO model will default to Request Repeat Utterance to ask for a repeat. Otherwise, the software engine will direct the conversation to the next Utterance of Reciprocal System Introduction (“Hi Doctor, okay! I am ready”) and the Chief Compliant inquiry. Depending on the encoded utterance, the dialogue will segue to either the Persona Appointment Agenda where there is an utterance that expresses what the purpose of the patient visit is or go directly Persona health information that expresses a specific aspect of the patient issue. Afterwards, Fig. 3 outlines the dialogue interaction where there is a “drill down” inquiry by the student user probing for more information about the patient, and the patient responding with pieces of their personal health information ranging from cancer history, dental aesthetic information, prior appointments, etc.
Fig. 3.
Meta-level abstraction that represents the dialogue interaction for patient-provider training. Blue nodes are the ParticipantUtterances and the red nodes are the SystemUtterances.
Using Protégé 5.50 [71], we authored and represented the aforementioned dialogue interaction using the foundations provided through the PHIDO model as a new ontology artifact. Certain Utterances, like the Participant Introduction Utterance, were provided, but we added the ParticipantUtterances and SystemUtterances listed from Table 1 which are unique for this project. This ontology serves as a knowledge base to represent the training conversation in the scenarios that could be imported to COO, the aforementioned software engine that automate the dialogue interaction that specifically uses the PHIDO- based models. The ontology models created for the dialogue flow charts resulted in 142 Classes, 27 Object properties, and 6 Data properties.
2.4. Evaluation
To test the operationalization of the model, we developed two test data models based off of the two dialogue scenario scripts, representing two different patients, that had complex discourse. These test data models were published as two separate PHIDO-based ontologies with instance level data as linked utterances. Figure 4 shows the instances for one of the test ontologies.
Fig. 4.
Close-up screenshot of instances (utterance data) for one of the test ontology models viewed through Protégé.
We imported the test model ontologies into software engine which was executed through Eclipse IDE’s command console. We interacted with the console in the role of dental student using the utterances from the test script and we recorded each successful and unsuccessful transition from one utterance to another on a spreadsheet. Later, we tallied the transition links accounting the number of successful and unsuccessful utterance links, and reviewed the test script models to assess the operational errors.
3. Results
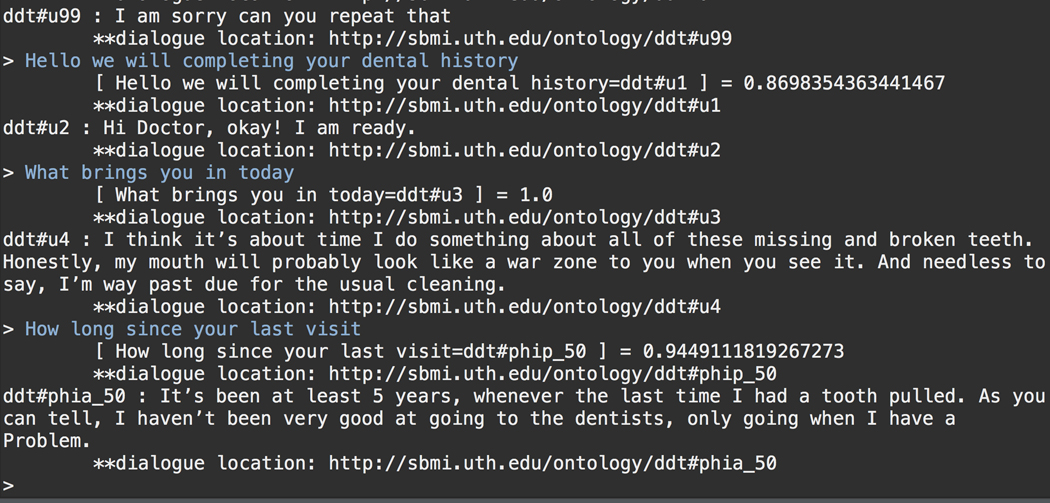
We created two test models from sample dialogues and performed an assessment with the test scripts through the dialogue software engine (that imported the knowledge base) to verify each dialogue chain in the script (235 dialogue chains in total). Figure 5 shows a sample demonstration from the command console prompt.
Fig. 5.
Sample execution of the dialogue model through the experimental software engine (COO) in debugging mode.
The total assessment from the two test models revealed that the dialogue engine was able to handle about 62% of the dialogue links (i.e., transition from one utterance to another). Most of the errors encountered were due to the link from Persona health information to Persona health inquiry (see Fig. 3), originating from the software engine’s algorithm conflicting with a gap in ontology model. We deduced that a possible solution would be to add an utterance between Persona health information and Persona health inquiry to accommodate the error.
4. Discussion and Future Direction
This work adds to existing research on the utility of ontologies for automated planning and deliberation, specifically in the domain of dialogue management of patient- provider communication training. In addition, we exhibited possible extensions of our work with the PHIDO model and the COO engine for conversational agents beyond the vaccine education domain, and onto the domain of training dental students on patient-provider communication. Specifically, we demonstrated the flexibility of our previous works’ approach by adapting the interaction to where the machine simulates the passive agent, taking on a non-expert role in the dialogue exchange with a human expert user.
In this study, we investigated the development of patient-provider training models to support training of prospective dental students to gain experience communicating with diverse patients. These training models were manifested as ontology artifacts that can be utilized by software and smart devices to automate the interaction of an individual patient from dialogue scripts that represented individual patient visits. We leveraged some of our previous work in an ontology-driven software engine for conversational agents for vaccine counseling but reorienting it to passive dental patient proxies. This arrangement places the conversational responsibility on the prospective dental student to initiate and engage the patient verbally.
While we were able to translate the dialogue scenario scripts to a formal model of dialogue interaction and execute it using our ontology-based method, we intend to refine the model to address the alluded the gap which we believe is easily rectifiable through the addition of an Utterance concept. However, it may also highlight the rigidity of the dialogue model, and we may encounter unanticipated challenges.
Bearing in mind we were given eight scripts/patients, the model we devised may be limited. In our previous work, we relied on using Wizard of Oz simulations as a way to gain authentic insight of how and what the dialogue interaction is executed. Through these simulations we were able to create the PHIDO-based model that mirror the authentic interactions of the simulation with live users. Our future direction may involve conducting simulations to gain an accurate insight, and also give us an avenue to pursue pilot testing with the automated deployment of the agent.
Another aspect for us to consider are some of the “trivial” social exchanges that sometimes occur between provider and patient. For example, small talk, or similar social emotional exchanges, is not uncommon to occur between the patient and the provider which has been cited to have some benefits in improving the relationship between them [72]. The dialogue scripts did contain minor small talk (e.g., parking issues by the patient), and our model did not include these types of interactions. However, a future research objective is to study social emotional exchanges in health care, and the underlying mechanism for us to represent it computationally.
There were also idiosyncrasies revealed in the different scripts that represented personality types through their utterances or choice words. One of our on-going, current focus involves the exploration of ontologies for personas that could link to the dialogue ontology model. These ontology-based personas could add a layer of interaction and possibly add more heterogeneous and individualized interaction of the agent.
5. Conclusion
Using scenarios provided by collaborators from UTHealth’s School of Dentistry, we developed a standard computational model for patient-provider training using ontology-driven tools from our previous endeavors. Using sample utterances from the scenarios, we were able to automate the dialogue that mimics the fictionalized, individual patients from those scenario scripts. Our operational tests revealed some gaps that can be rectified through modification of the dialogue model. Future goals aim to further enhance the realism of the interaction by deploying or simulating the work with potential dental students and adding diverse, individualized dialogue discourse into the model.
Acknowledgements.
Research was supported by the UTHealth Innovation for Cancer Prevention Research Training Program (Cancer Prevention and Research Institute of Texas grant # RP160015), the National Library of Medicine of the National Institutes of Health under Award Numbers R01LM011829 and R00LM012104, and the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under Award Number R01AI130460 and R01AI130460–03S1.
References
- 1.Towle A, Godolphin W: Framework for teaching and learning informed shared decision making. BMJ 319, 766–771 (1999) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khatri R: Client aggression towards health service providers in Nepal. Health Prospect. 14, 22 (2015). 10.3126/hprospect.v14i2.14264 [DOI] [Google Scholar]
- 3.Virshup BB, Oppenberg AA, Coleman MM: Strategic risk management: reducing malpractice claims through more effective patient-doctor communication. Am. J. Med. Qual 14, 153–159 (1999). 10.1177/106286069901400402 [DOI] [PubMed] [Google Scholar]
- 4.Ranjan P, Kumari A, Chakrawarty A: How can doctors improve their communication skills? J. Clin. Diagn. Res 9, JE01–04 (2015). 10.7860/JCDR/2015/12072.5712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anderson R: Patient expectations of emergency dental services: a qualitative interview study. Br. Dent. J 197, 331–334, discussion 323 (2004). 10.1038/sj.bdj.4811652 [DOI] [PubMed] [Google Scholar]
- 6.Haskard Zolnierek KB, DiMatteo MR: Physician communication and patient adherence to treatment: a meta-analysis. Med. Care 47, 826–834 (2009). 10.1097/MLR.0b013e31819a5acc [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hall JA, Roter DL, Katz NR: Meta-analysis of correlates of provider behavior in medical encounters. Med. Care 26, 657–675 (1988). 10.1097/00005650-198807000-00002 [DOI] [PubMed] [Google Scholar]
- 8.Ong LM, de Haes JC, Hoos AM, Lammes FB: Doctor-patient communication: a review of the literature. Soc. Sci. Med 40, 903–918 (1995). 10.1016/0277-9536(94)00155-m [DOI] [PubMed] [Google Scholar]
- 9.Hausberg MC, Hergert A, Kröger C, Bullinger M, Rose M, Andreas S: Enhancing medical students’ communication skills: development and evaluation of an undergraduate training program. BMC Med. Educ 12, 16 (2012). 10.1186/1472-6920-12-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Modi JN, Anshu, Gupta P, Singh T: Teaching and assessing professionalism in the Indian context. Indian Pediatr. 51, 881–888 (2014). 10.1007/s13312-014-0521-x [DOI] [PubMed] [Google Scholar]
- 11.Lipkin M, Quill TE, Napodano RJ: The medical interview: a core curriculum for residencies in internal medicine. Ann. Inter. Med 100, 277–284 (1984). 10.7326/0003-4819-100-2-277 [DOI] [PubMed] [Google Scholar]
- 12.Smith RC, et al. : The effectiveness of intensive training for residents in interviewing. A randomized, controlled study. Ann. Inter. Med 128, 118–126 (1998). 10.7326/0003-4819-128-2-199801150-00008 [DOI] [PubMed] [Google Scholar]
- 13.Duffy FD, et al. : Assessing competence in communication and interpersonal skills: the Kalamazoo II Report. Acad. Med 79, 495–507 (2004) [DOI] [PubMed] [Google Scholar]
- 14.Haidet P, et al. : Medical student attitudes toward the doctor–patient relationship. Med. Educ 36, 568–574 (2002). 10.1046/j.1365-2923.2002.01233.x [DOI] [PubMed] [Google Scholar]
- 15.Silverman J: Teaching clinical communication: a mainstream activity or just a minority sport? Patient Educ. Couns 76, 361–367 (2009). 10.1016/j.pec.2009.06.011 [DOI] [PubMed] [Google Scholar]
- 16.Rao JK, Anderson LA, Inui TS, Frankel RM: Communication interventions make a difference in conversations between physicians and patients: a systematic review of the evidence. Med. Care 45, 340–349 (2007). 10.1097/01.mlr.0000254516.04961.d5 [DOI] [PubMed] [Google Scholar]
- 17.Chessman AW, Blue AV, Gilbert GE, Carey M, Mainous AG: Assessing students’ communication and interpersonal skills across evaluation settings. Fam. Med 35, 643–648 (2003) [PubMed] [Google Scholar]
- 18.Choudhary A, Gupta V: Teaching communications skills to medical students: introducing the fine art of medical practice. Int. J. Appl. Basic Med. Res 5, S41–S44 (2015). 10.4103/2229-516X.162273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Świątoniowska-Lonc N, Polański J, Tański W, Jankowska-Polańska B: Impact of satisfaction with physician–patient communication on self-care and adherence in patients with hypertension: cross-sectional study. BMC Health Serv. Res 20 (2020). 10.1186/s12913-020-05912-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Epstein RM, Fiscella K, Lesser CS, Stange KC: Why the nation needs a policy push on patient-centered health care. Health Aff. 29, 1489–1495 (2010) [DOI] [PubMed] [Google Scholar]
- 21.Ali MR: Online virtual standardized patient for communication skills training. In: Proceedings of the 24th International Conference on Intelligent user Interfaces: Companion, pp. 155–156 (2019) [Google Scholar]
- 22.Skeels M, Tan DS: Identifying opportunities for inpatient-centric technology. In: Proceedings of the 1st ACM International Health Informatics Symposium, pp. 580–589. Association for Computing Machinery, New York (2010). 10.1145/1882992.1883087 [DOI] [Google Scholar]
- 23.Deandrea S, Montanari M, Moja L, Apolone G: Prevalence of undertreatment in cancer pain. A review of published literature. Ann. Oncol 19, 1985–1991 (2008). 10.1093/annonc/mdn419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Institute of Medicine (US) Committee on Quality of Health Care in America: To Err is Human: Building a Safer Health System. National Academies Press (US), Washington (DC) (2000) [PubMed] [Google Scholar]
- 25.Al-Busaidi AS: Field guide to the difficult patient interview. Sultan Qaboos Univ. Med. J 10, 285–286 (2010) [Google Scholar]
- 26.Riley JL, Gordan VV, Hudak-Boss SE, Fellows JL, Rindal DB, Gilbert GH: Concordance between patient satisfaction and the dentist’s view: findings from The National Dental Practice-Based Research Network. J. Am. Dent. Assoc 145, 355–362 (2014). 10.14219/jada.2013.32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bansal M, Gupta N, Saini GK, Sharma N: Satisfaction level among patients visiting a rural dental institution toward rendered dental treatment in Haryana, North India. J. Educ. Health Promot 7 (2018). 10.4103/jehp.jehp_20_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schoenfelder T: Patient satisfaction: a valid indicator for the quality of primary care? Primary Health Care 02 (2012). 10.4172/2167-1079.1000e106 [DOI] [Google Scholar]
- 29.Keating NL, Gandhi TK, Orav EJ, Bates DW, Ayanian JZ: Patient characteristics and experiences associated with trust in specialist physicians. Arch. Int. Med 164, 1015–1020 (2004). 10.1001/archinte.164.9.1015 [DOI] [PubMed] [Google Scholar]
- 30.Świątoniowska N, Sarzyńska K, Szymańska-Chabowska A, Jankowska-Polańska B: The role of education in type 2 diabetes treatment. Diab. Res. Clin. Pract 151, 237–246 (2019). 10.1016/j.diabres.2019.04.004 [DOI] [PubMed] [Google Scholar]
- 31.Epstein RM, Hundert EM: Defining and assessing professional competence. JAMA 287, 226–235 (2002). 10.1001/jama.287.2.226 [DOI] [PubMed] [Google Scholar]
- 32.Gürler G, Delilbaşı Ç, Kaçar İ: Patients’ perceptions and preferences of oral and maxillofacial surgeons in a university dental hospital. Eur. Oral Res 52, 137–142 (2018). 10.26650/eor.2018.483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mitchell ST, et al. : Satisfaction with dental care among patients who receive invasive or non-invasive treatment for non-cavitated early dental caries: findings from one region of the National Dental PBRN. BMC Oral Health 17 (2017). 10.1186/s12903-017-0363-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gruber T: What is an Ontology? https://web.archive.org/web/20100716004426/http://www-ksl.stanford.edu/kst/what-is-an-ontology.html [Google Scholar]
- 35.Feilmayr C, Wöß W: An analysis of ontologies and their success factors for application to business. Data Knowl. Eng 101, 1–23 (2016) [Google Scholar]
- 36.W3C Owl Working Group and others: OWL 2 Web Ontology Language Document Overview, 2nd edn. http://www.w3.org/TR/owl2-overview/. Accessed 09 July 2014 [Google Scholar]
- 37.Brickley D, Guha RV, McBride B: RDF Primer. https://www.w3.org/TR/rdf-schema/. Accessed 01 Jan 2021 [Google Scholar]
- 38.Klyne G, Carroll JJ, McBride B: Resource Description Framework (RDF) 1.1 Concepts and Abstract Syntax. https://www.w3.org/TR/rdf11-concepts/. Accessed 01 Jan 2021 [Google Scholar]
- 39.Barr A: The Handbook of Artificial Intelligence. William Kaufmann, Inc. (1981) [Google Scholar]
- 40.Gil Y: Description logics and planning. AI Mag. 26, 73–73 (2005) [Google Scholar]
- 41.Giacomo GD, Iocchi L, Nardi D, Rosati R: Description logic-based framework for planning with sensing actions. In: Proceedings of the 1997 International Workshop on Description Logics (1997) [Google Scholar]
- 42.Sirin E, Parsia B, Wu D, Hendler J, Nau D: HTN planning for web service composition using SHOP2. J. Web Semant 1, 377–396 (2004) [Google Scholar]
- 43.Kuter U, Sirin E, Nau D, Parsia B, Hendler J: Information gathering during planning for web service composition. In: International Semantic Web Conference, pp. 335–349 (2004) [Google Scholar]
- 44.McIlraith S, Son TC: Adapting golog for composition of semantic web services. Kr 2, 2 (2002) [Google Scholar]
- 45.Sohrabi S, McIlraith SA: Preference-based web service composition: a middle ground between execution and search. In: Patel-Schneider PF, et al. (eds.) ISWC 2010. LNCS, vol. 6496, pp. 713–729. Springer, Heidelberg: (2010). 10.1007/978-3-642-17746-0_45 [DOI] [Google Scholar]
- 46.De Giacomo G, Iocchi L, Nardi D, Rosati R: A theory and implementation of cognitive mobile robots. J. Logic Comput 9, 759–785 (1999) [Google Scholar]
- 47.Levesque HJ, Reiter R, Lespérance Y, Lin F, Scherl RB: GOLOG: a logic programming language for dynamic domains. J. Logic Program 31, 59–83 (1997) [Google Scholar]
- 48.Lespérance Y, Levesque HJ, Lin F, Marcu D, Reiter R, Scherl RB: A logical approach to high-level robot programming–a progress report. In: Control of the Physical World by Intelligent Systems, Papers From the 1994 AAAI Fall Symposium, pp. 79–85 (1994) [Google Scholar]
- 49.Hartanto R, Hertzberg J: Fusing DL reasoning with HTN planning. In: Dengel AR, Berns K, Breuel TM, Bomarius F, Roth-Berghofer TR (eds.) KI 2008. LNCS (LNAI), vol. 5243, pp. 62–69. Springer, Heidelberg: (2008). 10.1007/978-3-540-85845-4_8 [DOI] [Google Scholar]
- 50.Waibel M, et al. : Roboearth. IEEE Rob. Autom. Mag 18, 69–82 (2011) [Google Scholar]
- 51.Tenorth M, Beetz M: KnowRob: a knowledge processing infrastructure for cognitionenabled robots. Int. J. Rob. Res 32, 566–590 (2013) [Google Scholar]
- 52.Lemaignan S, Ros R, Mösenlechner L, Alami R, Beetz M: ORO, a knowledge management platform for cognitive architectures in robotics. In: 2010 IEEE/RSJ International Conference on Intelligent Robots and Systems, pp. 3548–3553 (2010) [Google Scholar]
- 53.Carnell S, Halan S, Crary M, Madhavan A, Lok B: Adapting virtual patient interviews for interviewing skills training of novice healthcare students. In: Brinkman W-P, Broekens J, Heylen D. (eds.) IVA 2015. LNCS (LNAI), vol. 9238, pp. 50–59. Springer, Cham: (2015). 10.1007/978-3-319-21996-7_5 [DOI] [Google Scholar]
- 54.Wiehagen GB: Medical simulation and training: breakthroughs and barriers. In: Proceedings of the 2008 Summer Computer Simulation Conference, pp. 1–7. Society for Modeling & Simulation International, Vista, CA (2008) [Google Scholar]
- 55.Carnell S, Lok B, James MT, Su JK: Predicting student success in communication skills learning scenarios with virtual humans. In: Proceedings of the 9th International Conference on Learning Analytics & Knowledge, pp. 436–440. Association for Computing Machinery, New York (2019). 10.1145/3303772.3303828 [DOI] [Google Scholar]
- 56.Yedidia MJ: Effect of communications training on medical student performance. JAMA 290, 1157 (2003). 10.1001/jama.290.9.1157 [DOI] [PubMed] [Google Scholar]
- 57.Makoul G: Essential elements of communication in medical encounters: The Kalamazoo consensus statement. Acad. Med 76, 390–393 (2001) [DOI] [PubMed] [Google Scholar]
- 58.Novack DH, Volk G, Drossman DA, Lipkin M Jr.: Medical interviewing and interpersonal skills teaching in US medical schools: progress, problems, and promise. JAMA 269, 2101–2105 (1993). 10.1001/jama.1993.03500160071034 [DOI] [PubMed] [Google Scholar]
- 59.Aspegren K: BEME Guide No. 2: teaching and learning communication skills in medicine-a review with quality grading of articles. Med. Teach 21, 563–570 (1999). 10.1080/01421599978979 [DOI] [PubMed] [Google Scholar]
- 60.Stevens A, et al. : The use of virtual patients to teach medical students history taking and communication skills. Am. J. Surg 191, 806–811 (2006). 10.1016/j.amjsurg.2006.03.002 [DOI] [PubMed] [Google Scholar]
- 61.Lehman L, Lu C, Mathews J, Tanwani A: Use of a Smart Speaker Device to Simulate Doctor-Patient Communication in Health Professions Education. Biomedical Engineering, Capstone Design., Cockrell School of Engineering - The University of Texas at Austin (2018) [Google Scholar]
- 62.Amith M, Roberts K, Tao C: Conceiving an application ontology to model patient human papillomavirus vaccine counseling for dialogue management. BMC Bioinform. 20, 1–16 (2019) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Amith M, et al. : Examining potential usability and health beliefs among young adults using a conversational agent for HPV vaccine counseling. AMIA Summits Transl. Sci. Proc 2020, 43 (2020) [PMC free article] [PubMed] [Google Scholar]
- 64.Amith M, et al. : Early usability assessment of a conversational agent for HPV vaccination. Stud. Health Technol. Inform, 17–23 (2019). 10.3233/978-1-61499-951-5-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Amith M, et al. : Conversational ontology operator: patient-centric vaccine dialogue management engine for spoken conversational agents. BMC Med. Inform. Decis. Mak 20, 259 (2020). 10.1186/s12911-020-01267-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Manning CD, Surdeanu M, Bauer J, Finkel JR, Bethard S, McClosky D: The stanford CoreNLP natural language processing toolkit. In: ACL (System Demonstrations), pp. 55–60 (2014) [Google Scholar]
- 67.Horridge M, Bechhofer S: The OWL API: a Java API for OWL ontologies. Semant. Web 2, 11–21 (2011) [Google Scholar]
- 68.Eclipse Foundation: Eclipse RDF4J (2019) [Google Scholar]
- 69.Glimm B, Horrocks I, Motik B, Stoilos G, Wang Z: HermiT: an OWL 2 reasoner. J. Autom. Reason 53, 245–269 (2014) [Google Scholar]
- 70.diagrams.net:draw.io. (2020)
- 71.Musen MA: The protégé project: a look back and a look forward. AI Matters 1, 4–12 (2015). 10.1145/2757001.2757003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Maupome G, Holcomb C, Schrader S: Clinician-patient small talk: comparing fourth-year dental students and practicing dentists in a standardized patient encounter. J. Dent. Educ 80, 1349–1356 (2016) [PubMed] [Google Scholar]