Abstract
As treatment expansion in the opioid epidemic continues, it is important to examine how the makeup of individuals with opioid use disorder (OUD) is evolving. Treatment programs are increasingly utilizing buprenorphine, an effective OUD medication. This exploratory study examines sex and gender differences in psychosocial, clinical and substance use treatment characteristics of a clinical population in outpatient medication treatment for OUD with buprenorphine. This is a secondary data analysis from a cross-sectional survey study with retrospective medical record review conducted with patients recruited from an office-based opioid treatment clinic between July-September 2019. Participants on buprenorphine for at least 28 days at time of survey completion were included (n=133). Differences between men and women were explored with Pearson χ2 and Fisher’s Exact Tests for categorical variables and T-Tests for continuous variables. The sample was 55.6% women and nearly three-fourths Black (70.7%). Mean days in current treatment episode was 431.6 (SD=244.82). Women were younger and more likely to be unemployed, identify as a sexual minority, and live alone with children than men. More women than men had a psychiatric comorbidity. Women reported more prescription opioid misuse while men had more heroin only opioid use. More men reported comorbid alcohol use and a history of drug overdose. One-third of participants reported recent discrimination in a healthcare setting due to substance use. As buprenorphine-based outpatient treatment programs continue to expand, present study findings support evaluation of the unique needs of men and women in order to better tailor OUD-related services and improve treatment outcomes.
Keywords: sex and gender, buprenorphine, opioid use disorder (OUD), medication treatment for opioid use disorder (MOUD), addiction
The opioid crisis continues to be a public health concern. Across the United States, life expectancy is decreasing, largely due to opioid related deaths among young people (Woolf & Schoomaker, 2019). While more men than women are diagnosed with Opioid Use Disorder (OUD) and are dying from opioid related causes (Wilson et al., 2020), recently women have shown a more rapid increase in drug related deaths than men (CDC, 2018; Woolf & Schoomaker, 2019). From 1999 to 2010, overdose deaths increased 265% among men and 400% among women (CDC, 2018). With this change in the face of the opioid crisis (Marsh et al., 2018), we need more information to adequately address the specific needs of men and women seeking OUD treatment and entering recovery (Ling et al., 2019; Mazure & Fiellin, 2018).
Sex (biological constructs) and gender (social constructs) interact to influence health and medical diseases generally (Mauvais-Jarvis et al., 2020) as well as addiction risk, course, and treatment (McHugh et al., 2018). However, studies of sex and gender differences specific to OUD are limited and vary widely across different populations, treatment modalities, and measured outcomes (Saraiya et al., 2020). Most research in this area was completed prior to the opioid crisis or, if recent, used patient populations enrolled in clinical trials or residential treatment programs (Huhn et al., 2019). Further, given the more recent expansion of medication treatment for opioid use disorder (MOUD) with buprenorphine, the current body of literature on sex and gender differences in MOUD populations largely focuses on methadone (Bawor et al., 2015; Levine et al., 2015; van Reekum et al., 2020). Due to the interrelated relationship between sex and gender, the ability to separate the specific effects of each on disease is limited, and although gender is nonbinary, research among gender minorities within the field of addiction is lacking (Mauvais-Jarvis et al., 2020). Given these limitations, we just refer to men and women throughout the manuscript.
While buprenorphine and methadone are both forms of MOUD, treatment setting and clinical management differ (Blanco & Volkow, 2019; West et al., 2004). Additionally, studies have shown differences in characteristics of those who receive buprenorphine versus methadone. For example, individuals receiving MOUD with buprenorphine are more likely to be White, younger, healthier, and from a higher socioeconomic status than those receiving MOUD with methadone (Homayra et al., 2020; Rhee & Rosenheck, 2019). As office-based opioid treatment programs and buprenorphine prescribing providers continue to increase in response to the opioid crisis, more clinically relevant data focused on sex and gender differences among patients engaging in outpatient MOUD treatment with buprenorphine is urgently needed (Dick et al., 2015; Wakeman & Barnett, 2018).
According to the existing literature among those with OUD more broadly, women typically experience a more accelerated progression from onset of opioid use to treatment entry (Campbell et al., 2018; Hernandez-Avila et al., 2004; Lewis et al., 2014). Additionally, women tend to present to treatment with more severe medical and psychiatric comorbidities as well as social vulnerabilities such as being younger, unemployed, identifying as a sexual minority, and engaging in risky sex or drug use behaviors (Back et al., 2011; Bawor et al., 2015; Campbell et al., 2018; Herbeck et al., 2016; Unger et al., 2010). Historically, women have faced greater barriers to care than men including pregnancy, childcare responsibilities, lack of transportation, and stigma (Greenfield et al., 2007; Herbeck et al., 2016; Jancaitis et al., 2020). Men tend to present with more legal issues and more extensive substance use history (Back et al., 2011; Campbell et al., 2018). Once engaged in OUD treatment, women and men tend to have similar treatment outcomes (Levine et al., 2015), but recent literature suggests differences in social functioning outcomes (i.e., employment status, interpersonal conflicts, and criminal activity) persist in treatment (van Reekum et al., 2020). Additionally, recent data specific to buprenorphine treatment populations indicates women may have better outcomes than men though the underlying mechanism of this difference is unclear (Huhn et al., 2019).
Gold standard substance use disorder treatment utilizes a multidimensional model that addresses patients’ medical and psychosocial needs (NIDA, 2018; SAMHSA, 2019). In line with this model, incorporating sex and gender-informed services could help providers and public health officials improve treatment quality and optimize recovery outcomes. Treatment programs offering sex and gender-informed services have been shown to have high patient satisfaction and positive long-term outcomes (Greenfield et al., 2007; Polak et al., 2015). Sex and gender-informed services may contribute to improved outcomes, in part, due to varying complexities of treatment presentation profiles between men and women. Addressing medical and psychosocial issues through a sex and gender lens is warranted in order to expand the breadth and quality of treatment services for the increasing number of people with OUD, an area in need of further development (Terplan et al., 2015).
Although evidence suggests men and women with OUD differ across demographic, psychosocial, clinical, and substance use treatment characteristics, limited research has comprehensively explored sex and gender differences among a clinical population in outpatient MOUD with buprenorphine. Therefore, programs serving this population lack evidence to guide adoption of sex and gender-informed approaches. Given the distinctive treatment delivery method, clinical management, and characteristics of those receiving buprenorphine compared to other MOUD, it is unclear whether or not sex and gender differences identified in previous OUD populations will be replicated within this unique population. An important first step to fill this knowledge gap is to attain a comprehensive understanding of patient needs and how they differ between men and women. The primary objective of this exploratory study was to examine differences in the demographic, psychosocial, clinical, and substance use treatment characteristics between men and women engaged in outpatient MOUD with buprenorphine.
Methods
Participants and Design
The current exploratory study is a secondary analysis of a cross-sectional survey study coupled with medical record review. The parent study recruited a convenience sample of patients (n=162; 97% response rate) from an outpatient substance use disorder treatment clinic affiliated with an academic medical center to complete a voluntary, electronic survey between July and September 2019 assessing reproductive and sexual health needs. Study participants were English-speaking and at least 18 years old. Participants who were unable to read had the option to have the survey read aloud by a research assistant in a private space (n=6). Survey completion took an average of 40 minutes, and participants were compensated $20. A retrospective medical record chart abstraction was also conducted for these participants. Virginia Commonwealth University’s Institutional Review Board approved the study, and participants provided verbal consent.
For the current secondary data analytic study, participants were limited to those who were diagnosed with OUD and engaged in MOUD with buprenorphine resulting in a sample size of n=133 (59 cisgender men and 74 cisgender women) participants. Patients were considered engaged in treatment after they had been on MOUD with buprenorphine for at least 28 days as that allowed time for the patient to become stabilized on a therapeutic dose of buprenorphine and have at least one follow-up visit with an addiction provider.
Survey Measures
Demographic and Psychosocial Characteristics
Demographic items included gender (cisgender man, cisgender woman, transgender man, transgender woman, other), sex assigned at birth (male, female, other), age, race, employment, income, education, sexual orientation, and living arrangement. Psychosocial items were asked with reference to the past 12 months. Unsafe housing (yes/no) was defined as not feeling safe to leave or return to your neighborhood and/or feeling afraid of being hurt in your residence. Homelessness (yes/no) was defined as living on the street, in a shelter, in a single room occupancy hotel, or in a car. Food, utility, and childcare insecurity (all yes/no) were assessed using items from the Health Leads Social Determinants of Health Screening Tool (Health Leads, 2016). Insecurities were defined as limited access to adequate food, difficulty paying utility bills and power shut offs, and inability to secure childcare when needed.
The 18-item Medical Outcomes Study Social Support Survey developed for patients with chronic medical conditions was used to assess current social support (Sherbourne and Stewart, 1993). The 5-point frequency scale (1-none of the time to 5-all of the time) results in average scores ranging from 1 to 5 with higher mean scores indicating more social support.
Clinical Characteristics and Substance Use History
Risk behaviors and healthcare characteristics were also assessed considering the past 12 months. A series of yes/no items asked about the following: exchange of sex for money or drugs and sharing needles, healthcare access (defined as seeing a provider other than an addiction provider at least once), healthcare barriers such as cost, transportation, and unsafe housing, and discrimination as measured by the item: “Have you ever felt you were treated unfairly getting health care services?”
Two four-item Patient-Reported Outcomes Measurement Information System (PROMIS) measures assessed current (past seven days) anxiety and depression symptomatology. Each uses a 5-point frequency scale (1-never to 5-always); total scores range from 4 to 20. For both PROMIS scales, a T-score conversion was used (Health Measures, 2020). Norms for the scales are based on US population estimates, with a mean T-score of 50 (SD = 10). For chronic pain, one item asked: “Do you currently suffer from any type of chronic pain?” (yes/no). Lastly, participants reported number of lifetime substance use disorder treatment episodes, excluding the current episode.
Medical Record Chart Review
Clinical Characteristics and Substance Use Disorder Treatment
Clinical intake assessments were reviewed to obtain insurance status, psychiatric and medical comorbidity diagnoses, psychiatric medications, laboratory test results, substance use history, and treatment characteristics. Urine toxicology and breathalyzer results were extracted. Opioid use items at intake included: type of opioid use, route, frequency, age of use onset, and history of overdose (yes/no). Use of additional substances was documented. Lifetime polysubstance (yes/no) use was defined as any self-reported prior or current use of non-prescribed opioids and non-opioid substances (excluding tobacco). Polysubstance use at intake (yes/no) was operationalized using urine toxicology and breathalyzer results. Participants that had a positive urine toxicology result for non-prescribed opioids and another non-opioid substance as well as those who had a positive urine toxicology for non-prescribed opioids and a positive breathalyzer were coded as “yes” for polysubstance use at intake. Prior substance use treatments (i.e., inpatient/residential, intensive outpatient, medication, mental health services, and self-help groups) and treatment regimens initiated at the first visit were reviewed including initial buprenorphine dosage, medication for comorbid substance use, and mental health services. Length of current treatment episode was the number of days between the date of buprenorphine induction or initial clinic visit date through the survey date.
Data Analysis
Descriptive statistics were generated. Comparisons between men and women were made using Pearson χ2 and Fisher’s Exact tests for categorical variables and T-tests for continuous variables. In order to account for multiple comparisons, significance was set at 0.01. Because this is an exploratory study to identify future areas of study, we also noted variables with a p-value between 0.05 and 0.01. The Winsorizing method was used to minimize the effect of outliers in the number of treatment episodes variable (Tukey, 1961). Statistical analyses were performed using SPSS version 26 (IBM, 2019).
Results
Demographic and Psychosocial Characteristics
Table 1 presents demographic and psychosocial characteristics for the total sample (N=133; 59 men, 74 women). Similar to the demographics of the treatment population for the target clinic, most participants identified as Black, were unemployed, and had public insurance. Mean age was 43.4 (SD=12.4) years. Women were younger than men, more likely to be unemployed, and identify as a sexual minority. Women were also four times more likely to live alone with children and three times more likely to experience childcare insecurity than men, while men were more likely than women to live completely alone. Additional psychosocial and risk behavior variables did not differ between men and women.
Table 1.
Demographic and Psychosocial Characteristics of an Outpatient MOUD with Buprenorphine Sample
| Demographic and Psychosocial Characteristics | Total N (%) N=133 |
Men N (%) N=59 |
Women N (%) N=74 |
P-Value |
|---|---|---|---|---|
| Age (Mean ± SD) | 43.4 ± 12.4 | 46.7 ± 12.4 | 40.9 ± 11.8 | .007 ** |
| Race | ||||
| Black | 94 (70.7) | 43 (72.9) | 51 (68.9) | |
| White | 31 (23.3) | 11 (18.6) | 20 (27.0) | .345 |
| Other | 8 (6.0) | 5 (8.5) | 3 (4.1) | |
| Insurancea | ||||
| Public | 76 (57.1) | 33 (55.9) | 43 (58.1) | .670 |
| Private | 14 (10.5) | 5 (8.5) | 9 (12.2) | |
| None | 43 (32.3) | 21 (35.6) | 22 (29.7) | |
| Employment | ||||
| Unemployed | 97 (72.9) | 36 (61.0) | 61 (82.4) | .006 ** |
| Employed | 36 (27.1) | 23 (39.0) | 13 (17.6) | |
| Annual Household Income | ||||
| < $5,000 | 63 (47.4) | 25 (42.4) | 38 (51.3) | |
| $5,000 to 10,000 | 23 (17.3) | 10 (16.9) | 13 (17.6) | .437 |
| > $10,000 | 42 (31.6) | 22 (37.3) | 20 (27.0) | |
| Not Reported | 5 (3.8) | 2 (3.4) | 3 (4.1) | |
| Education | ||||
| < high school degree | 29 (21.8) | 15 (25.4) | 14 (18.9) | |
| High school degree/equivalent | 65 (48.9) | 28 (47.5) | 37 (50.0) | .652 |
| > high school degree | 39 (29.3) | 16 (27.1) | 23 (31.1) | |
| Sexual orientation | ||||
| Straight/heterosexual | 105 (78.9) | 54 (91.5) | 51 (68.9) | |
| Gay or lesbian | 9 (6.8) | 1 (17) | 8 (10.8) | .006 ** |
| Bisexual/other | 19 (14.3) | 4 (6.8) | 15 (20.3) | |
| Living Arrangement | ||||
| With a sexual partner | 36 (27.9) | 15 (25.9) | 21 (29.6) | |
| With children alone | 14 (10.9) | 2 (3.4) | 12 (16.9) | .002 ** |
| With family/friends | 45 (34.9) | 19 (32.8) | 26 (36.6) | |
| Alone | 21 (16.3) | 17 (29.3) | 4 (5.6) | |
| Other | 13 (10.1) | 5 (8.6) | 8 (11.3) | |
| Homeless | 46 (35.1) | 23 (39.0) | 23 (31.9) | .401 |
| Unsafe housing | 58 (44.3) | 30 (52.6) | 28 (37.8) | .091 |
| Food insecurity | 69 (53.5) | 29 (52.7) | 40 (54.1) | .881 |
| Utility insecurity | 29 (22.3) | 13 (23.2) | 16 (21.6) | .829 |
| Childcare insecurity | 20 (15.4) | 4 (7.0) | 16 (21.9) | .044* |
| Social support score (range 0–5; Mean ± SD) | 3.5 ± 1.1 | 3.3 ± 1.1 | 3.6 ± 1.0 | .151 |
| Drug and sex risk behaviors | ||||
| Exchange sex for drugs or money | 22 (17.6) | 8 (14.3) | 14 (20.3) | .381 |
| Shared needles | 9 (7.3) | 3 (5.4) | 6 (8.8) | .511 |
| See healthcare provider once/12mos | 113 (86.3) | 48 (84.2) | 65 (87.8) | .550 |
| Barriers to healthcare | ||||
| Transportation | 41 (31.8) | 14 (25.0) | 27 (37.0) | .147 |
| Cost | 35 (26.9) | 15 (26.8) | 20 (27.0) | .975 |
| Unsafe neighborhood | 25 (19.5) | 14 (25.5) | 11 (15.1) | .142 |
| Any barrier (≥1 barrier) | 68 (51.1) | 27 (45.8) | 41 (55.4) | .269 |
Note. MOUD, medication treatment for opioid use disorder; SD, standard deviation
Significance at p=0.05;
Significance at p=0.01
Data was self-reported in survey except for insurance status which was abstracted from medical record.
Healthcare access, barriers to healthcare, and recent discrimination in a healthcare setting did not differ between men and women. Most participants had seen a non-addiction healthcare provider at least once in the previous 12 months (Table 1). About half of both men and women endorsed at least one barrier to receiving healthcare, and nearly half experienced recent discrimination in a healthcare setting, most commonly due to drug and alcohol use (30.7%; Figure 1).
Figure 1. Percentage of Participants in Outpatient MOUD with Buprenorphine who Reported Discrimination in Healthcare Setting within Past 12 Months, by Gender.
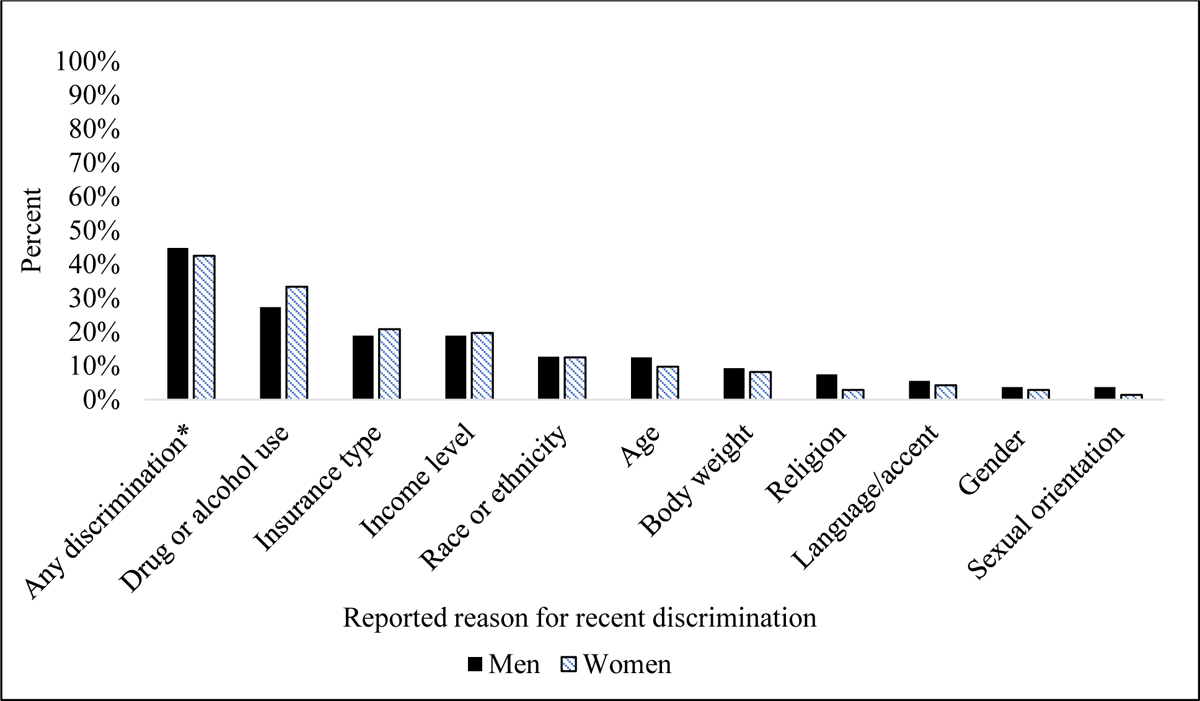
Note. Responses to the question “In the past 12 months, have you ever felt you were treated unfairly in getting healthcare services because of any of the following?”
MOUD, medication treatment for opioid use disorder
* “Any discrimination” includes participants who reported discrimination in ≥1 category.
Clinical Characteristics
Clinical characteristics are summarized in Table 2. Most participants had a diagnosis of at least one psychiatric comorbidity. Current anxiety and depressive symptoms as measured by the PROMIS did not vary by between men and women. Although not significant, women were diagnosed with more psychiatric comorbidities than men with higher rates of depression, anxiety, and Post-traumatic Stress Disorder (PTSD).
Table 2.
Clinical Characteristics of an Outpatient MOUD with Buprenorphine Sample
| Clinical Characteristics | Total N (%) N=133 |
Men N (%) N=59 |
Women N (%) N=74 |
P-Value |
|---|---|---|---|---|
| Psychiatric Comorbidity Diagnosis | ||||
| Depressive Disorder | 65 (49.2) | 23 (39.0) | 42 (57.5) | .034* |
| Anxiety/Panic Disorder | 41 (31.1) | 12 (20.3) | 29 (39.7) | .017* |
| Bipolar Disorder | 19 (14.4) | 8 (13.6) | 11 (15.1) | .806 |
| Post-traumatic Stress Disorder | 18 (13.5) | 6 (10.2) | 12 (16.2) | .311 |
| Attention Deficit Disorder | 8 (6.1) | 3 (5.1) | 5 (6.8) | .731 |
| Other | 13 (9.8) | 6 (10.2) | 7 (9.5) | .891 |
| Total number of psychiatric conditions (Mean ± SD) | 1.23 ± 1.15 | .98 ± 1.03 | 1.43 ± 1.21 | .024* |
| Psychiatric medication (initial visit) | 55 (41.4) | 19 (32.2) | 36 (48.6) | .056 |
| aPROMIS (Mean ± SD) | ||||
| Depression | 55.0 (10.4) | 54.8 (9.9) | 55.2 (10.8) | .865 |
| Anxiety | 56.5 (11.9) | 55.8 (12.2) | 57.0 (11.7) | .596 |
| aSelf-reported chronic pain | 47 (38.2) | 23 (41.8) | 24 (35.3) | .459 |
| Chronic medical conditions | ||||
| Medical comorbidity | 99 (74.4) | 45 (76.3) | 54 (73.0) | .665 |
| Pain comorbidity | 39 (29.3) | 16 (27.1) | 23 (31.1) | .618 |
| Infectious disease comorbidity | 48 (36.1) | 22 (37.3) | 26 (35.1) | .797 |
| Total number of medical conditions (Mean ± SD) | 2.23 ± 1.85 | 2.22 ± 1.67 | 2.24 ± 1.98 | .944 |
| Positive Hepatitis C Antibody | 62 (53.4) | 31 (59.6) | 31 (48.4) | .230 |
Note. MOUD, medication treatment for opioid use disorder; SD, standard deviation; PROMIS, Patient-Reported Outcomes Measurement Information System
Significance at p=0.05;
Significance at p=0.01
Data included in table was abstracted from participant medical records except for PROMIS Anxiety and PROMIS depression scores and self-reported chronic pain which was collected via survey.
Medical conditions also did not vary between men and women (Table 2). Overall, nearly three-fourths of patients had at least one chronic medical comorbidity diagnosis. Mean number of chronic medical conditions was 2.23 (SD=1.85). Several reported chronic pain and/or had a pain diagnosis.
Substance Use and Treatment History
Table 3 presents substance use and treatment history data. Most participants were using illicit or misusing prescription opioids daily at treatment entry. Overall, heroin only use was most common. Although not significant, more women than men reported prescription opioid misuse only or both heroin use and prescription misuse. Men were nearly twice as likely to report a history of overdose compared to women. Among both men and women, most participants self-reported lifetime polysubstance use, and many participants had a past history of substance use treatment. Differences emerged between men and women for comorbid alcohol use with more men than women reporting any lifetime use.
Table 3.
Substance Use and Treatment History Characteristics for an Outpatient MOUD with Buprenorphine Sample
| Substance Use and Treatment History Characteristics | Total N (%) N=133 |
Men N (%) N=59 |
Women N (%) N=74 |
P-Value |
|---|---|---|---|---|
| Type of opioid use | .053 | |||
| Heroin only | 91 (68.4) | 46 (78.0) | 45 (60.8) | |
| Prescription opioid only | 12 (9.0) | 2 (3.4) | 10 (13.5) | |
| Both | 30 (22.6) | 11 (18.6) | 19 (25.7) | |
| Route of opioid use | ||||
| Injection | 66 (49.6) | 31 (52.5) | 35 (47.3) | .548 |
| Nasal | 74 (55.6) | 34 (57.6) | 40 (54.1) | .680 |
| Oral | 27 (20.3) | 9 (15.3) | 18 (24.3) | .196 |
| Daily opioid use at treatment entry (illicit or Rx misuse) | 105 (80.2) | 49 (84.5) | 56 (76.7) | .268 |
| Age onset opioid use (Mean ± SD) | 25.1 ± 10.0 | 24.8 ± 10.1 | 25.4 ± 9.9 | .729 |
| History overdose | 31 (39.2) | 18 (51.4) | 13 (29.5) | .048* |
| Lifetime substance use | ||||
| Tobacco use | 114 (88.4) | 48 (87.3) | 66 (89.2) | .737 |
| Cocaine use | 101 (77.1) | 42 (73.7) | 59 (79.7) | .414 |
| Alcohol use | 69 (53.5) | 38 (67.9) | 31 (42.5) | .004 ** |
| Cannabis use | 61 (47.7) | 27 (49.1) | 34 (46.6) | .778 |
| Benzodiazepine use | 14 (11.0) | 4 (7.5) | 10 (13.5) | .393 |
| Amphetamine misuse | 6 (4.8) | 4 (7.4) | 2 (2.8) | .401 |
| aLifetime polysubstance use | 125 (94.0) | 56 (94.9) | 69 (93.2) | .687 |
| b# Lifetime treatment episodes [Mean (range)] | 3 (0 – 13) | 3.4 (0 – 13) | 2.7 (0 – 12) | .150 |
| Prior inpatient/residential treatment | 53 (39.8) | 25 (42.4) | 28 (37.8) | .596 |
| Prior intensive outpatient treatment | 12 (9.0) | 5 (8.5) | 7 (9.5) | .844 |
| Prior medication for OUD | ||||
| Buprenorphine | 38 (28.6) | 15 (25.4) | 23 (31.1) | .473 |
| Methadone | 38 (28.6) | 14 (23.7) | 24 (32.4) | .270 |
| Other | 2 (1.5) | 1 (17) | 1 (14) | 1.000 |
| Prior mental health services | 15 (11.3) | 9 (15.3) | 6 (8.1) | .196 |
| Prior self-help group (AA/NA) | 18 (13.5) | 10 (16.9) | 8 (10.8) | .304 |
Note. MOUD, medication treatment for opioid use disorder; OUD, Opioid Use Disorder; SD, standard deviation; SUD, Substance Use Disorder; AA, Alcoholics Anonymous; NA, Narcotics Anonymous
Significance at p=0.05;
Significance at p=0.01
Participants who reported previous or current use of at least one nonopioid substance (excluding tobacco) in addition to opioids. Variable used as a proxy for lifetime polysubstance use.
Data included in table was abstracted from participant medical records except for Lifetime number of treatment episodes which was self-reported in survey.
Current Substance Use Treatment Episode
Average length of the current treatment episode was 431.6 days (SD=244.82), and it did not differ between men and women. Treatment characteristics are summarized in Table 4. At treatment entry, over half of men and women tested positive for illicit use or prescription misuse of opioids in addition to another illicit substance or alcohol use. The most common opioids for which participants tested positive were non-treatment buprenorphine and morphine. Additionally, nearly half of participants tested positive for cocaine. The average initial buprenorphine treatment regimen was 15.0 mg (SD=5.2) per day. Men and women did not differ significantly by urine toxicology results, initial buprenorphine regimen, or initial mental health services (Table 4). While men and women were equally likely to initiate mental health services, including individual and group therapy, men were almost four times more likely to report attending self-help groups, such as Alcoholics Anonymous (AA) or Narcotics Anonymous (NA).
Table 4.
Characteristics at Initial Visit of Current Substance Use Treatment Episode for an Outpatient MOUD with Buprenorphine Sample
| Substance Use Treatment Characteristics at Initial Visit | Total N (%) N=133 |
Men N (%) N=59 |
Women N (%) N=74 |
P-Value |
|---|---|---|---|---|
| aFirst Treatment Episode | 19 (15.6) | 5 (9.8) | 14 (20.0) | .128 |
| Urine toxicology screen results | ||||
| Positive buprenorphine | 75 (56.4) | 34 (57.6) | 41 (55.4) | .797 |
| Positive morphine | 65 (48.9) | 31 (52.5) | 34 (45.9) | .450 |
| Positive cocaine | 62 (46.6) | 27 (45.8) | 35 (47.3) | .860 |
| Positive THC (cannabis) | 33 (24.8) | 15 (25.4) | 18 (24.3) | .884 |
| Positive benzodiazepine | 11 (8.3) | 3 (5.2) | 8 (10.8) | .346 |
| Positive oxycodone | 9 (6.8) | 2 (3.4) | 7 (9.5) | .297 |
| Positive methadone | 9 (6.8) | 3 (5.2) | 6 (8.1) | .731 |
| Positive methamphetamine | 3 (2.3) | 1 (17) | 2 (2.7) | 1.00 |
| Positive amphetamine | 2 (1.5) | 0 (0.0) | 2 (2.7) | .503 |
| Breathalyzer (% BAC) [median (range)] | 0.0 (0.0 – 3.2) | 0.0 (0.0 – 3.2) | 0.0 (0.0 – 0.0) | .168 |
| bPolysubstance use at intake | 81 (60.9) | 32 (54.2) | 49 (66.2) | .160 |
| Initial buprenorphine treatment regimen (mg; mean ± SD) | 15.0 ± 5.2 | 15.8 ± 5.1 | 14.3 ± 5.2 | .097 |
| Initial mental health services | ||||
| Individual therapy | 61 (61.6) | 29 (67.4) | 32 (57.1) | .296 |
| Group therapy | 59 (59.6) | 23 (53.5) | 36 (64.3) | .278 |
| Self-help group (AA/NA) | 18 (18.2) | 13 (30.2) | 5 (8.9) | .006 ** |
Note. MOUD, medication treatment for opioid use disorder; THC, Tetrahydrocannabinol; BAC, blood alcohol concentration; SD, standard deviation; SUD, Substance Use Disorder; AA, Alcoholics Anonymous; NA, Narcotics Anonymous
Significance at p=0.05;
Significance at p=0.01
Data included in table was abstracted from participant medical records except for “First treatment episode” which was self-reported in survey.
Participants who tested positive on urine toxicology screen for more than one substance (opioids + another illicit substance) or who tested positive on urine toxicology screen for opioids and tested positive on breathalyzer for alcohol. Variable used as a proxy for polysubstance use at intake.
Discussion
This exploratory study found differences between men and women in the treatment-based sample of individuals in outpatient MOUD with buprenorphine. Similar to previous research on sex and gender differences among OUD clinical trial or residential treatment populations, our findings suggest women engaged in treatment have more biopsychosocial vulnerabilities than men (Back et al., 2011; Campbell et al., 2018). For example, women were more likely to be unemployed, identify as a sexual minority, live alone with children, and experience difficulties securing childcare than men. While psychiatric and medical comorbidities were common among all participants, more women than men were diagnosed with psychiatric comorbidities. Findings highlight the need for sex and gender-informed services in order to accommodate the complex nature of profiles specific to men and women throughout OUD treatment.
Providing comprehensive services, such as housing, social support, and childcare services, alongside substance use disorder treatment provides optimal outcomes across both men and women. However, men and women differ in their needs and the services they utilize to support their recovery. For instance, when provided comprehensive support services, women tend to engage more than men which is likely reflective of the higher burden of poor psychosocial support for women (Marsh et al., 2004). Onsite sex and gender-specific services and support systems, such as a mom’s recovery group and therapy sessions with childcare, could be helpful for parenting women given their unique needs and the lower likelihood of seeking outside support from traditional self-help groups, such as AA or NA. Integration of such support services into treatment programs may increase service utilization and in turn improve OUD treatment outcomes (Elms et al., 2018).
In addition to provision of support services to help address structural barriers including childcare and transportation, it is equally important to address attitudinal barriers as well, namely stigma. Notably, nearly half of participants experienced recent mistreatment in a healthcare setting, with discrimination due to drug and alcohol use being most common. Unfortunately, stigma against individuals with OUD is prevalent both in society at large and within the healthcare community (Volkow, 2020). Fear of judgment and mistreatment because of one’s substance use commonly deters individuals from seeking health services (MacAfee et al., 2020) and may also compromise treatment outcomes. Pregnant and parenting women are particularly susceptible to the stigma and discrimination associated with addiction (Haug et al., 2017). Expanded education efforts and stigma-reduction strategies regarding OUD and evidence-based OUD treatments among healthcare providers are needed (Avery et al., 2019; McGinty & Barry, 2020). Decreasing stigma within the healthcare community could have positive impacts on the overall health of people with OUD.
Because addiction is a chronic disease that often benefits from long term treatment, it is common for patients with substance use disorders to have multiple treatment episodes during their disease course (Kelly & William, 2011). Our findings reflect this chronic disease model with most participants reporting prior receipt of multiple substance use treatment services. Nearly all participants reported daily use of opioids (illicit or prescription misuse) prior to treatment initiation, and heroin use was prevalent among all participants. Additionally, women were more likely than men to have reported a history of only prescription opioid misuse or both prescription opioid misuse and heroin use. These findings are consistent with contemporary epidemiologic data illustrating the evolving trends of the opioid epidemic. Women continue to experience consequences from the first wave of the opioid epidemic—prescription opioid misuse—in addition to the second wave—heroin use (CDC, 2020). Specifically, the decrease in prescription opioid misuse is occurring more slowly for women than men while the increase in heroin use is occurring more rapidly for women compared to men (Marsh et al, 2018). In this cross-sectional study, more men reported a history of overdose than women which is consistent with previous research (Wilson et al., 2020). However, emerging epidemiologic data indicate overdose deaths are increasing at a faster rate for women than men, highlighting how maturing trends in substance use are critical to consider as we face the opioid crisis (CDC, 2018; Woolf & Schoomaker, 2019).
Polysubstance use is associated with worse treatment outcomes for individuals with OUD (Hedegaard et al., 2018; Samples et al., 2018; VanHouten et al., 2019; Weinstein et al., 2017). Within our sample, self-reported lifetime polysubstance use and polysubstance use at intake were common. Cocaine and tobacco use were the most commonly used substances in addition to opioids for both men and women. Men were more likely than women to report comorbid alcohol use similar to previous studies among people with OUD (Campbell et al., 2018). However, it is critical to note that alcohol use disorder remains the most common substance use disorder not only for men but also for women (Martin et al., 2020). Given these differences, assessment and treatment approaches targeting polysubstance use for individuals with OUD should incorporate sex and gender with other patient factors to optimize outcomes.
The standard of care for OUD treatment is multimodal, combining medication (e.g., buprenorphine, methadone) with other tailored services such as mental health, social work and recovery support (NIDA, 2018). Among our sample, all participants initiated a buprenorphine treatment regimen, and 3 in 4 participants also initiated mental health services. These findings are encouraging considering the high prevalence of comorbid psychiatric diagnoses among this population. While depression and anxiety were the most common psychiatric comorbidities overall, women were more likely than men to have these diagnoses. Additionally, PTSD was relatively common, with approximately 1 in 6 participants diagnosed (more women than men). Evidence suggests that trauma-informed, integrated interventions that address both OUD and psychiatric conditions simultaneously improve treatment outcomes (Marsden et al., 2019; Najavits et al., 2002). More work is needed to improve screening and address co-occurring psychiatric conditions among individuals with OUD, particularly women, given the tragic association between psychiatric comorbidities and opioid overdose deaths including suicide (Fendrich et al., 2019; Oquendo & Volkow, 2019).
There are several limitations to this study. First and foremost, given our small sample size, multiple comparisons may have increased the likelihood of Type I error; however, to help control for this limitation we set significance at 0.01. Additionally, our small sample size may have impacted the ability to detect statistically significant differences. Because of these limitations, findings should be interpreted as preliminary; future hypothesis-driven studies are needed to further clarify differences between men and women within this unique population. Participants self-selected into this convenience sample from one outpatient clinic, and only patients who remained engaged in MOUD with buprenorphine for at least 28 days were included in analyses. Findings may not be representative of those who chose not to participate in the study and may not generalize to individuals who are engaged with alternative treatment modalities, who do not remain engaged in treatment, or who are non-treatment seeking. Gender identity was assessed in the survey, but no participants identified as a gender minority. Thus, our analyses were limited to a cisgender conceptualization of gender identity. The cross-sectional nature of our survey limits our ability to determine causality. Social desirability bias may have skewed our results as the survey was completely by self-report and asked about several sensitive issues. Information bias is highly probable for the variables obtained from our chart review given the retrospective design, constrained variables available for abstraction, and information limited by provider documentation and patient report at intake assessment. Despite these limitations, to our knowledge, this study is the first to describe differences between men and women among a patient population engaged in outpatient MOUD with buprenorphine. Therefore, findings are more clinically applicable than previous studies.
Conclusions
Overall, differences between men and women were identified among this clinical sample of patients engaged in outpatient MOUD with buprenorphine. Women had more biopsychosocial vulnerabilities including psychiatric comorbidities, while men tended to have more severe addiction profiles including a history of more overdoses compared to women. These findings complement previous research findings based on OUD patient populations within experimental, residential, and methadone treatment settings and identify future areas of study within this unique population. Furthermore, they reiterate the importance of sex and gender-informed multidimensional outpatient treatment services that address both medical and psychosocial needs of patients (Mazure & Fiellin, 2018). As office-based opioid treatment programs and buprenorphine prescribing providers continue to increase in response to the opioid crisis, incorporating a sex and gender-informed lens is imperative to support recovery-based OUD treatment services.
What is the significance of this article for the general public?
Focusing on the NIH mandate to consider sex and gender in research and clinical practice, we explored differences between men and women in the growing clinical population of patients in outpatient buprenorphine treatment for opioid use disorder (OUD). Findings complement prior research within alternative treatment settings illustrating important variations in clinical and psychosocial characteristics between men and women. Within the opioid crisis, incorporating sex and gender-informed, multidimensional services, such as integrated mental health treatment, is imperative to support recovery-based OUD treatment.
Financial Acknowledgements:
This work was supported by Clinical and Translational Science Awards (UL1TR002649 and KL2TR002648); Training in the Pharmacology of Abused Drugs (PI: W. Dewey; T32DA007027)
Footnotes
Disclosure of Interest: The authors report no conflicts of interest.
References
- Avery J, Knoepflmacher D, Mauer E, Kast KA, Greiner M, Avery J, Penzner JB (2019). Improvement in residents’ attitudes toward individuals with substance use disorders following an online training module on stigma. HSS J, 15(1), 31–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Back SE, Payne RL, Wahlquist AH, Carter RE, Stroud Z, Haynes L, Hillhouse M, Brady KT, & Ling W (2011). Comparative profiles of men and women with opioid dependences: Results from a national multisite effectiveness trial. Am J Drug Alcohol Abuse, 37, 313–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bawor M, Dennis BB, Varenbut M, Daiter J, Marsh DC, Plater C, Worster A, Steiner M, Anglin R, Pare G, Desai D, Thabane L, & Samaan Z (2015). Sex differences in substance use, health, and social functioning among opioid users receiving methadone treatment: A multicenter cohort study. Biology of Sex Differences, 6(21), 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, & Volkow ND (2019). Management of opioid use disorder in the USA: present status and future directions. Lancet, 393(10182), 1760–1772. [DOI] [PubMed] [Google Scholar]
- Campbell ANC, Barbosa-Leiker C, Hatch-Maillette M, Mennenga SE, Pavlicova M, Scodes J, Saraiya T, Mitchell SG, Rotrosen J, Novo R, Nunes EV, & Greenfield SF (2018). Brief report: Gender differences in demographic and clinical characteristics of patients with Opioid Use Disorder entering a comparative effectiveness medication trial. Am J Addict, 27, 465–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2018). Prescription painkiller overdoses: A growing epidemic, especially among women. Accessed on3/20/20. Available at https://www.cdc.gov/vitalsigns/prescriptionpainkilleroverdoses/index.html
- Dick AW, Pacula RL, Gordon AJ, Sorbero M, Burns RM, Leslie DL, & Stein BD (2015). Increasing potential access to opioid agonist treatment in the U.S. treatment shortage areas. Health Aff, 34(6), 1028–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elms N, Link K, Newman A, Brogly SB, & for the Kingston House of Recovery for Women and Children. (2018). Need for women-centered treatment for substance use disorders: results from focus group discussions. Harm Reduct J, 15(1), 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fendrich M, Becker J, & Hernandez-Meier J (2019). Psychiatric symptoms and recent overdose among people who use heroin or other opioids: Results from a secondary analysis of an intervention study. Addictive Behaviors Reports, 10, Article 100212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield SF, Trucco EM, McHugh RK, Lincoln M, & Gallop RJ (2007). The women’s recovery group study: A stage I trial of women-focused group therapy for substance use disorders versus mixed-gender group drug counseling. Drug Alcohol Dependence, 90, 39–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haug N, Osomo R, Yanovitch M and Svikis DS (2017). Biopsychosocial approach to the management of drug and alcohol use in pregnancy. In Edozien L & O’Brien P (Eds.). Biopsychosocial Factors in Obstetrics and Gynecology. Cambridge University Press. [Google Scholar]
- Health Leads. (2016). Social needs screening toolkit. Accessed3/20/20. Available at: https://nopren.org/wp-content/uploads/2016/12/Health-Leads-Screening-Toolkit-July-2016.pdf
- Health Measures. (2020). PROMIS scoring manuals. Accessed7/7/20. Available at https://www.healthmeasures.net/index.php?option=com_content&view=article&id=180&Itemid=994.
- Hedegaard H, Bastian BA, Trinidad JP, Spencer M, & Warner M (2018). Drugs most frequently involved in drug overdose deaths: United States, 2011–2016. Natl Vital Stat Rep, 67(9), 1–14. [PubMed] [Google Scholar]
- Herbeck DM, Jeter KE, Cousins SJ, Abdelmaksoud R, & Crèvecoeur-MacPhail D (2016) Gender differences in treatment and clinical characteristics among patients receiving extended release naltrexone. Journal of Addictive Diseases, 35(4), 305–314. [DOI] [PubMed] [Google Scholar]
- Hernandez-Avila CA, Rounsaville BJ, & Kranzler HR (2004). Opioid-, cannabis-, and alcohol-dependent women show more rapid progression to substance abuse treatment. Drug Alcohol Dependence, 74, 265–272. [DOI] [PubMed] [Google Scholar]
- Homayra F, Hongdilokkul N, Piske M, Pearce LA, Zhou H, Min JE, Krebs E, & Nosyk B (2020). Determinants of selection into buprenorphine/naloxone among people initiating opioid agonist treatment in British Columbia. Drug and alcohol dependence, 207, 107798. [DOI] [PubMed] [Google Scholar]
- Huhn AS, Berry MS, & Dunn KE (2019). Review: Sex-based differences in treatment outcomes for persons with Opioid Use Disorder. Am J Addict, 28(4), 246–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corporation. (2019). IBM SPSS Statistics for Macintosh, Version 26.0. Armonk, NY: IBM Corp [Google Scholar]
- Jancaitis B, Kelpin S, Masho S, May J, Haug N, & Svikis D (2020). Factors associated with treatment retention in pregnant women with opioid use disorders prescribed methadone or electing non-pharmacological treatment. Women Health, 60(1), 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JFW & William L (2011). Addiction and recovery management: Theory, research and practice. New York, NY, Humana Press. [Google Scholar]
- Levine AR, Lundahl LH, Ledgerwood DM, Lisieski M, Rhodes GL, & Greenwalkd MK (2015). Gender-specific predictors of retention and opioid abstinence during methadone maintenance treatment. J Substance Abuse Treatment, 54, 37–43. [DOI] [PubMed] [Google Scholar]
- Lewis B, Hoffman LA, & Nixon SJ (2014). Sex differences in drug use among polysubstance users. Drug Alcohol Depend, 145, 127–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ling S, Mangaoil R, Cleverley K, Sproule B, & Puts M (2019). A systematic review of sex differences in treatment outcomes among people with opioid use disorder receiving buprenorphine maintenance versus other treatment conditions. Drug Alcohol Depend, 197, 168–182. [DOI] [PubMed] [Google Scholar]
- MacAfee LK, Harfmann RF, Cannon LM, Minadeo L, Kolenic G, Kusunoki Y, & Dalton VK (2020). Substance use treatment patient and provider perspectives on accessing sexual and reproductive health services: Barriers, facilitators, and the need for integration of care. Subst Use Misuse, 55(1), 95–107. [DOI] [PubMed] [Google Scholar]
- Marsden J, Stillwell G, James K, Shearer J, Byford S, Hellier J, Kelleher M, Kelly J, Murphy C, & Mitcheson L (2019). Efficacy and cost-effectiveness of an adjunctive personalized psychosocial intervention in treatment-resistant maintenance opioid agonist therapy: A pragmatic, open-label, randomized controlled trial. Lancet Psychiatry, 6(5), 391–402. [DOI] [PubMed] [Google Scholar]
- Marsh JC, Park K, Lin Y, & Bersamira C (2018). Gender differences in trends for heroin use and nonmedical prescription opioid use, 2007–2014. Journal of Substance Abuse Treatment, 27, 79–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsh JC, Cao D, & Aunno TD (2004). Gender differences in the impact of comprehensive services in substance abuse treatment. J Subst Abuse Treat, 27(4), 289–300. [DOI] [PubMed] [Google Scholar]
- Martin CE, Scialli A, & Terplan M (2020). Unmet substance use disorder treatment need among reproductive age women. Drug Alcohol Depend, 206(1), 107679. [DOI] [PubMed] [Google Scholar]
- Mauvais-Jarvis F, Merz NB, Barnes PJ, Brinton RD, Carrero JJ, DeMeo DL..& Suzuki A (2020). Sex and gender: modifiers of health, disease, and medicine. Lancet, 396(10250), 565–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazure CM & Fiellin DA. (2018). Women and opioids: something different is happening here. Lancet, 392(10141), 9–11. [DOI] [PubMed] [Google Scholar]
- McGinty EE & Barry CL (2020). Stigma reduction to combat the addiction crisis - developing an evidence base. New England Journal of Medicine, 382(14), 1291–1292. [DOI] [PubMed] [Google Scholar]
- McHugh RK, Votaw VR, Sugarman DE, & Greenfield SF (2018). Sex and gender differences in substance use disorders. Clinical Psychology Review, 66, 12–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Najavits LM (2002). Seeking safety: A treatment manual for PTSD and substance abuse. Guilford Press, NY. [DOI] [PubMed] [Google Scholar]
- National Institute on Drug Abuse. (2018). Principles of drug addiction treatment: A research-based guide, third edition. Accessed on3/20/20. Available at https://www.drugabuse.gov/publications/principles-drug-addiction-treatment-research-based-guide-third-edition/principles-effective-treatment
- Oquendo MA, & Volkow ND (2019). Suicide: A silent contributor to opioid-overdose deaths. N Engl J Med, 378, 1567–1569. [DOI] [PubMed] [Google Scholar]
- Polak K, Haug NA, Drachenberg HE, & Svikis DS (2015). Gender considerations in addiction: Implications for treatment. Curr Treat Options Psychiatry, 2(3), 326–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhee TG, & Rosenheck RA (2019). Buprenorphine prescribing for opioid use disorder in medical practices: can office-based out-patient care address the opiate crisis in the United States? Addiction, 114(11), 1992–1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samples H, Williams AR, Olfson M, & Crystal S (2018). Risk factors for discontinuation of buprenorphine treatment for opioid use disorders in a multi-state sample of Medicaid enrollees. J Subst Abuse Treat, 95, 9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saraiya TC, Pavlicova M, Hu M, Nunes EV, Hien DA, & Campbell ANC (2020). Exploring gender differences among treatment-seekers who use opioids versus alcohol and other drugs. Women Health, 60(7), 821–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherbourne C,D & Stewart A (1993). The MOS Social Support Survey. Santa Monica, CA: RAND Corporation. https://www.rand.org/pubs/reprints/RP218.html. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2019). Recovery and recovery support. Accessed on1/15/20. Available at: https://www.samhsa.gov/find-help/recovery.
- Terplan M, Longinaker N, & Appel L (2015). Women-centered drug treatment services and need in the US, 2002–2009. American Journal of Public Health, 105(11), e50–e54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tukey JW (1961). Statistical and quantitative methodology. In Ray DP (Ed.), In Trends in Social Sciences. New York: Philosophical Library. [Google Scholar]
- Unger A, Jung E, Winklbaur B, & Fischer G (2010). Gender issues in the pharmacotherapy of opioid-addicted women: buprenorphine. Journal of Addictive Diseases, 29(2), 217–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Reekum EA, Rosic T, Hudson J, Sanger N, Marsh DC, Worster A, … & Samaan Z (2020). Social functioning outcomes in men and women receiving medication-assisted treatment for opioid use disorder. Biology of Sex Differences, 11, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanHouten JP, Rudd RA, Ballesteros MF, & Mack KA (2019). Drug Overdose Deaths Among Women Aged 30–64 Years — United States, 1999–2017. Morb Mortal Wkly Rep, 68, 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND (2020). Stigma and the toll of addiction. New England Journal of Medicine, 382(14), 1289–1290. [DOI] [PubMed] [Google Scholar]
- Wakeman SE & Barnett ML. (2018). Primary care and the opioid-overdose crisis-buprenorphine myths and realities. N Engl J Med, 379(1), 1–4. [DOI] [PubMed] [Google Scholar]
- Weinstein ZM, Kim HW, Cheng DM, Quinn E, Hui D, Labelle CT, Drainoni M, Bachman SS, & Samet JH (2017). Long-term retention in office based opioid treatment with buprenorphine. J Subst Abuse Treat, 74, 65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West JC, Kosten T, Wilk J, Svikis DS, Triffleman E, Rae DS, Narrow WE, Duffy FF and Regier DA (2004). Challenges in increasing access to buprenorphine treatment for opiate addiction. American Journal on Addictions, 13(Suplm 1), S8–16. [DOI] [PubMed] [Google Scholar]
- Wilson N, Kariisa M, Seth P, Smith H, & Davis NL (2020). Drug and opioid-involved overdose deaths: United States, 2017–2018. Morb Mortal Wkly Rep, 69(11), 290–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf SH & Schoomaker H (2019). Life expectancy and mortality rates in the United States, 1959–2017. JAMA, 322(20), 1996–2016. [DOI] [PMC free article] [PubMed] [Google Scholar]


