Abstract
Background:
A detailed understanding of the anatomy of the quadriceps tendon (QT) is clinically relevant, owing to its increased use as a graft in anterior cruciate ligament reconstruction.
Purpose:
To qualitatively and quantitatively describe the anatomy of the QT in younger adult specimens.
Study Design:
Descriptive laboratory study.
Methods:
A total of 18 nonpaired cadaveric knees with a mean age of 30.1 years (range, 18-38 years) were utilized for this study. A 3-dimensional coordinate measuring system was used to assess the structural relationships between the different layers of the QT and their attachments to the patella, and QT thickness was measured medially, centrally, and laterally at 2-cm intervals from the patellar eminence line (PEL; defined as a straight line between the medial and lateral patellar eminences) and proximally.
Results:
In all specimens, 3 distinct layers formed the QT. The first (superficial) layer was formed by the rectus femoris, which was fused to the second layer with an unclearly defined direct attachment to the patella. The median length of the QT was 86.9 mm (range, 68.4-98.9 mm). The second (middle) layer consisted of the vastus medialis and vastus lateralis and was found to have fibers running in an oblique direction that attached on the patella. A “fuse point,” where the proximal part of the rectus femoris started to merge to the second layer, was identified at a median of 48.7 mm (range, 27.9-62.6 mm) from the PEL. The third (deep) layer consisted of the vastus intermedius. The median thickness of the graft centrally at 20, 40, 60, 80, and 100 mm from the PEL was 8.5, 7.2, 7.5, 6.5, and 5.4 mm, respectively.
Conclusion:
Overall, 3 different layers of the QT were consistently found in all specimens. The first layer was fused with the second layer, and the direction of the fibers of the second layer or the vastus medialis and vastus lateralis was oblique. The median length of the QT was 86.9 mm, and the thickness of the tendon diminished proximally.
Clinical Relevance:
This study allows for a better understanding of QT anatomy when harvesting the tendon as a graft for ligamentous reconstruction.
Keywords: quadriceps tendon, ACL, autograft, anatomy
There is no consensus in the literature concerning the optimal graft choice for anterior cruciate ligament (ACL) reconstruction. Currently, bone-patellar tendon-bone (BPTB) and hamstring tendon autografts are the most commonly used grafts for ACL reconstruction.5,11 The use of a BPTB graft leads to a higher incidence of donor site morbidity, including kneeling pain, graft harvest site pain, and sensory loss.16 Hamstring tendon grafts are associated with an increased risk of revision compared with BPTB grafts, and the greatest risk factor is younger age (<20 years).27 There is increasing interest in utilizing the quadriceps tendon (QT) in knee ligament reconstruction because of its reported biomechanical properties,30 lower donor-site morbidity versus the BPTB autograft,26 and greater risk of hamstring tendon graft failure.27,29 ACL reconstruction utilizing QT grafts in adults has led to improvements in knee function and patient-reported outcomes, with less donor-site morbidity.26 The use of the QT also provides a viable option in multiple ligament–injured knees when several grafts are needed for ligament reconstruction. Furthermore, a soft tissue QT graft has comparable biomechanical properties to those of a hamstring tendon graft33 and could be an alternative option for ACL reconstruction in the skeletally immature population.
There are numerous publications on the anatomy of the QT in older adult specimens, with some describing attachment sites on the patella and others describing different patterns of layering and dimensions of the tendon.1,14,18,22 However, there is a limited number of studies on QT anatomy in a younger population. A detailed understanding of the anatomy of the QT is clinically relevant because of its increased use as an ACL graft. This knowledge is essential during graft harvesting to avoid iatrogenic injuries, to determine the best location to harvest the graft, and to act as a foundation for improving surgical techniques.
The purpose of this study was to qualitatively and quantitatively describe the anatomy of the QT, including its size, its layers, and the relationship of the different layers as well as insertion sites on the patella in younger adult specimens. It was hypothesized that each of the QT attachments would have definable parameters and consistent relationships to one another as well as pertinent surgically relevant landmarks.
Methods
Specimen Preparation
There were 2 groups of specimens utilized in this study. The first group was used to evaluate qualitative anatomy, pertaining to the different layers, and quantitative anatomy, with a focus on insertion sites of the QT, and the second group was used to evaluate the thickness of the QT. We included 10 cadaveric nonpaired knees (5 female and 5 male; 6 right and 4 left knees) with a mean age of 30.7 years (range, 18-38 years) in the first group and 8 cadaveric nonpaired knees (4 female and 4 male; 4 right and 4 left knees) with a mean age of 30.6 years (range, 18-37 years) in the second group. All the knees in this study were nonpaired, fresh-frozen human cadaveric knees with no history of injuries, surgery, or degenerative changes. There was a minimum of 20 cm of QT and quadriceps muscle measured from the patella in each specimen. All cadaveric specimens had been donated to a tissue bank for the purpose of medical research and then purchased by our institution.
The specimens were stored at –20°C and thawed at room temperature on the day of testing. After dissection of the skin and subcutaneous tissue, the muscle-tendon units forming the QT, the insertion on the patella, and the medial and lateral structures were identified. In the first group, the skin and subcutaneous tissue were dissected off the specimens. Each specimen was fixed in a custom-made aluminum block secured to a table and mounted using two 6-mm drill pins transfixed across the femur (Figure 1).
Figure 1.
Custom-made aluminum block with the specimen fixed at 45° of knee flexion. (A) The specimen was affixed to the block using 6-mm drill pins, and knee flexion was secured using 2.4-mm transfixed pins. (B) Quadriceps muscle tensioned using a 5-kg counterweight.
Using an outside-in dissection approach, the different layers and muscle groups of the QT and surrounding tissue were identified. The patellar eminence line (PEL) was defined for the purpose of this study. The medial and lateral patellar eminences were easily identified bony structures in all specimens. These were used as bony landmarks, and the PEL was defined as a straight line between the medial and lateral patellar eminences. The eminences and line were reproducible in all specimens. The PEL was used as a “baseline” for measuring distances of the QT.
The central (rectus femoris [RF] and vastus intermedius [VI] muscles), lateral (vastus lateralis [VL]), and medial (vastus medialis [VM]) muscle groups were sutured using No. 2 FiberWire (Arthrex) at the proximal end of the specimen, and each muscle group was tensioned using a 5-kg weight over a 90° pulley, which resulted in uniform tension throughout the different muscle groups and enabled dissection to be performed (Figure 2).
Figure 2.

Custom-made aluminum block with a specimen. Quadriceps muscle secured using suture in the vastus medialis muscle, vastus lateralis muscle, vastus intermedius muscle, and rectus femoris muscle and tensioned using a 5-kg weight over a pulley system.
The tibiofemoral joint was transfixed at 45°, and the patella was transfixed to the femur using 2 crossing 2.4-mm Kirschner pins at this angle to engage the patella in the trochlea and to avoid motion during data collection (Figure 1).
In the second group, using detailed outside-in and inside-out dissection, the QT specimens were prepared and mounted on an ACL graft preparation board (Arthrex), tensioned using a handheld weight measuring device at 5 kg, and fixed in this position using calipers (Fowler High Precision), and QT thickness was measured centrally, medially, and laterally and at predetermined sections 20, 40, 60, 80, and 100 mm from the PEL (Figure 3).
Figure 3.

Dissected full-thickness knee extensor component. Setup for thickness measurement of the quadriceps tendon.
Data Collection
Using the Coordinate Measuring Machine (First Group)
A portable coordinate measuring machine (Romer Absolute Arm; Hexagon Manufacturing Intelligence) was utilized to accurately measure the attachment areas as well as the QT location in relation to established anatomic landmarks. The following landmarks were defined for the superficial layer: QT border, QT attachment to the patella, medial patellar eminence, and lateral patellar eminence; for the middle layer: VM obliquus (VMO) border, VL border, and VL + VMO attachment to the patella; and for the deep layer: vastus intermedius (VI) border and VI attachment to the patella. This method has been validated and utilized in previous studies.17,36 Qualitative anatomy was documented. The length and width of the tendon and the layers of the different muscle-tendon groups at the attachment to the patella as well as the location of the different muscle fuse points were recorded.
Using Calipers to Determine Tendon Thickness (Second Group)
Using an ACL graft preparation board (Arthrex), the specimens were clamped at the proximal part of the patellar tendon and the QT at 12 cm proximal to the PEL. The specimens were tensioned using a handheld weight measuring device (Guangzhou Weiheng Electronics) at 5-kg tension and then fixed. The PEL was identified, and in a proximal direction, measurements were taken at 20, 40, 60, 80, and 100 mm from the PEL. A perpendicular line was drawn at each point using a surgical marking pen. The thickness of the specimens was measured at each drawn line from a medial direction, central-to-lateral direction, and distal-to-proximal direction using calipers (Fowler High Precision). Qualitative anatomy was documented and recorded.
Statistical Analysis
Data are reported as medians and ranges to summarize quantitative anatomic measurements across specimens. Because of the limited availability of younger adult specimens, a total of 18 specimens was chosen based on feasibility. Similar studies13,14,28,34 have had a sample size of 12 to 20 specimens.
Results
The QT was identified in all specimens as 3 distinct layers: superficial (first layer), middle (second layer), and deep (third layer). Qualitatively, tendon fibers of the rectus femoris (RF) blended with the fascia and coursed distally. The second layer consisted of VL tendon fibers, which coursed medially, and VM tendon fibers, which coursed laterally, until they merged distally, where their fibers crossed to form one inseparable tissue “blend”; however, we were still able to visualize/identify the fiber direction from the VL and VM. The third deepest layer was identified as the VI tendon that coursed in a uniform distal direction to the proximal patella. The PEL, from which QT distances were measured, was a median length of 49.3 mm (range, 40.4-55.4 mm).
Layers of the QT
First Layer
The superficial layer was identified and isolated (Figure 4). This layer consisted of the RF with a fascia/bursa structure superficial to the RF, coursing in a diagonal direction from the VL and toward the medial aspect of the patella. Dissecting from a proximal-to-distal direction, the proximal part of the RF was not attached to the deeper layer and was separated from the second layer by fatty tissue. In the more distal part, the fatty tissue faded, and the first layer (RF) fused with the second layer (VL + VM) of the QT at a median length of 48.7 mm (range, 27.9-62.6 mm) from the PEL; we referred to this as the “fuse point.” From the fuse point and distally to the patella, where the RF fibers appeared to fade, was considered the attachment site for the first layer. The tissue connection between the first and second layers from the fuse point and distally could easily be separated via simple dissection. The fusion of the first and second layers continued toward the patella. No distinct or well-defined bony attachment of the RF fibers on the patella was observed in any of the specimens. The RF was “peeled” off as part of the diagonal prepatellar fascia and bursa. This site had a median width of 41.6 mm (range, 32.5-49.7 mm). The median length of the RF from the PEL, in a proximal direction, to where the muscle belly of the RF attached was 86.9 mm (range, 68.4-98.9 mm) centrally, 114.5 mm (range, 71.9-163.3 mm) medially, and 151.9 mm (range, 95.6-179.7 mm) laterally. When the muscle belly was removed, the tendon continued in a proximal direction to where the specimens were cut.
Figure 4.
The first layer of the quadriceps tendon (QT), consisting of the rectus femoris muscle (RF). VL, vastus lateralis muscle; VMO, vastus medialis obliquus muscle.
Second Layer
The middle layer was identified deep to the first layer. This layer included the VM and VL and was a more complex layer that merged fibers from both muscles and tendons in a crossing pattern and where the fibers of the VM and VL blended as they coursed distally toward the patella (Figure 5A). The VM and VL blended together at a median distance of 85.5 mm (range, 52.0-109.0 mm) proximal from the PEL. The structures continued in a distal direction toward the patella, but fibers from both the VM and VL crossed paths from the point where they blended. The fiber structures were identifiable but not able to be separated via dissection. Fatty infiltration was observed in the tendinous part of this layer, especially when approaching the patella. On the proximal part of the VL tendon-muscle fiber complex, a distinct separation of layers of the VL was observed, with a more superficial layer and a deeper layer that could be completely separated during dissection, creating a seemingly 2-layer VL structure (Figure 5B).
Figure 5.

The second layer of the quadriceps tendon. (A) Tendon fiber direction and distal merging of the vastus medialis obliquus muscle (VMO) and vastus lateralis muscle (VL). (B) A double layer of the VL. VI, vastus intermedius muscle.
The tendon consisting of a blend of VM and VL fibers attached to the proximal part of the patella with a bony attachment and had a median thickness of 5.4 mm (range, 4.6-9.6 mm) and median width of 34.7 mm (range, 31.2-43.2 mm). The median attachment area was 212.2 mm2 (range, 117.2-244.5 mm2) at the attachment site on the patella. The median distance of the attachment site from the PEL was 2.6 mm (range, 0.6-6.9 mm).
Third Layer
The deep layer, consisting of the VI, was observed as a homogenous structure with fibers coursing in a parallel direction to the tendon (Figure 6). The tendon had a slight hourglass shape, with a median thickness of 7.5 mm (range, 4.3-9.9 mm), median width of 34.9 mm (range, 23.2-38.8 mm), and median attachment area of 211.2 mm2 (range, 157.9-349.6 mm2) at the patella. The median distance of the attachment site from the PEL was 8.7 mm (range, 6.2-11.7 mm), just proximal to the insertion of the second layer fibers on the patella.
Figure 6.
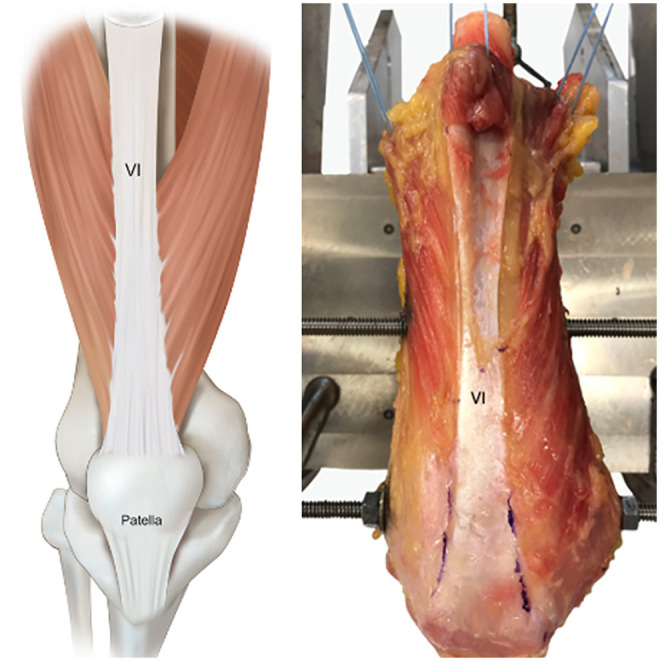
The third layer of the quadriceps tendon, consisting of the vastus intermedius muscle (VI).
Thickness of the QT
The QT was the thickest centrally and distally (closest to the patella), with a median thickness of 8.5 mm (range, 6.0-10.8 mm), and thinnest proximally, with a median thickness of 5.4 mm (range, 3.2-7.3 mm) (Figure 7).
Figure 7.
Thickness of the dissected quadriceps tendon attached to the patella. Measurements from 100 mm to the patellar eminence line (PEL) in 20-mm increments in a proximal-to-distal direction at the lateral and medial borders as well as centrally.
Discussion
The most important finding of this study was the consistent identification of each layer of the QT and its orientation, with the most superficial fibers originating from the RF; the deepest layer, from the VI; and the intermediate layer, from the VL and VM. Furthermore, the consistent identification of 2 distinct layers of the VL suggests that this structure differs from its current representation in the medical literature, with this occurrence only having been noted in a few prior studies.2,7,34 Previous studies have described a bilaminar, trilaminar, and tetralaminar organization composing the QT, but the most common description of the trilaminar organization14 was confirmed following our consistent identification of these 3 layers within each specimen. Given that anatomic descriptions of the QT have been variable within and across studies, we believe that this phenomenon could be the result of previous studies having dissected both fresh and formalin-preserved specimens with large age variations, with some studies having specimens with an average age of ≥78 years, and, therefore, age-related degenerative changes in both the differentiation of layers and possibly thickness of the QT could have been present.1,14,25,34
In the present study, the mean length of the QT was 86.9 mm (range, 68.4-98.9 mm), and the tendon was thickest at its patellar insertion than proximally. These were similar findings to those in the study by Lippe et al,25 with a mean ± standard deviation QT length of 88.3 ± 8.4 mm. The tendon became thinner in a proximal direction from the patella. These findings suggest that when harvesting the QT, a periosteal sleeve from the patella or a patellar bone block should be considered to optimize graft length. An adequate graft length is important in ACL reconstruction to optimize graft fixation and graft incorporation into the tunnel because inadequate fixation can lead to ACL reconstruction failure.
Although the BPTB is often regarded as the gold standard graft for ACL reconstruction,4,9 it has been associated with patellar tendon ruptures,3 patellar fractures,6,15 anterior knee pain,16 and difficulty in kneeling.21 This has encouraged orthopaedic surgeons to search for a more optimal graft choice. The QT was found to be of adequate substance that possesses mechanical properties sufficient for restoring the ACL after an injury32 earlier in the literature, and recent studies have displayed less donor site morbidity10,12,18,19,26 and similar postoperative outcomes relative to BPTB grafts. In a recent systematic review by Slone et al,31 the International Knee Documentation Committee score was roughly equivalent between BPTB and QT autografts,12,19,20,26 with 1 exception in which the BPTB was favored in terms of both patient satisfaction and International Knee Documentation Committee scores compared with the QT.10 Furthermore, comparative studies found no difference in the Lysholm score,10,19,20 postoperative quadriceps strength,12 range of motion,10,12,19 and the Knee injury and Osteoarthritis Outcome Score.26 However, in a newly published registry study by Lind et al24 comparing failure rates among QT, BPTB, and hamstring tendon grafts, revision rates were reported as 4.7%, 1.4%, and 2.3%, respectively. This study, therefore, has questioned the use of the QT for ACL grafts relative to BPTB and hamstring tendon grafts. However, a follow-up study by the same group evaluated low- and high-volume ACL surgery centers and reported on similar failure rates for both the QT (2.9%) and BPTB (2.3%) for high-volume centers.23 Widner et al35 compared large cohorts of QT, BPTB, and hamstring tendon autografts and found no significant differences in failure rates.
Concerning the QT graft for ACL reconstruction, Lippe et al25 recommended harvesting the graft slightly lateral to the midline of the QT insertion on the patella, as this is the thickest part of the tendon. Complications unique to QT autografts consist of possible postoperative hematomas after the perforation of vessels or deep punctures from full-thickness harvest. To prevent this, we suggest centralizing the graft harvest within the QT and performing partial-thickness harvest.31 Patellar fractures have been reported when the QT is harvested with a bone plug.8 Fu and Schulte9 recommended harvesting the QT from the midline because of an increased risk of patellar fractures when harvesting the graft more medially or laterally. Furthermore, in the same study, it was recommended not to harvest >50% of the length or depth of the patella to reduce the risk of a patellar fracture. The decreasing thickness of the QT in a proximal, as well as a medial and lateral, direction would suggest central harvest of the QT. A graft with a bone plug will ensure that the graft is long enough for use in ACL reconstruction.
The present study has some limitations inherent to a cadaveric study design. Although a detailed dissection was performed to clearly visualize the anatomic attachments and fiber orientations, distances were calculated as absolute 3-dimensional vector norms, which do not provide directional information. Additionally, there were a limited number of cadaveric knees, and, therefore, subanalyses according to sex and age were not conducted.
Conclusion
The findings of this study provide qualitative and quantitative data on the QT and its bony attachments. There were 3 different layers of the QT consistently found in all specimens. The first layer was fused with the second layer, and the direction of the fibers of the second layer or the VM and VL was oblique. The median length of the QT was 86.9 mm, and the thickness of the tendon diminished proximally.
Footnotes
Final revision submitted April 6, 2021; accepted May 4, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: Funding was provided by a research grant from Smith & Nephew. M.S. has received research support and educational consulting fees from Smith & Nephew. J.C. has received research support from Arthrex, Conmed Linvatec, Ossur, and Smith & Nephew; consulting fees from Arthrex, DePuy, Ossur, and Smith & Nephew; speaking fees from Conmed Linvatec; and hospitality payments from Stryker. R.F.L. has received research support from Arthrex, Conmed Linvatec, Ossur, and Smith & Nephew; consulting fees from Arthrex, Ossur, and Smith & Nephew; and royalties from Arthrex, Ossur, and Smith & Nephew. M.L. has received research support from Arthrex, Regentis, Novartis, and Smith & Nephew and educational consulting fees from Smith & Nephew. L.E. has received research support from Arthrex, Smith & Nephew, and Zimmer Biomet and consulting fees from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1.Andrikoula S, Tokis A, Vasiliadis HS, Georgoulis A. The extensor mechanism of the knee joint: an anatomical study. Knee Surg Sports Traumatol Arthrosc. 2006;14(3):214–220. [DOI] [PubMed] [Google Scholar]
- 2.Bevilaqua Grossi D, Pedro VM, Bérzin F. Functional analysis of the patellar stabilizers. Acta Ortop Bras. 2004;12(2):99–104. [Google Scholar]
- 3.Bonamo JJ, Krinick RM, Sporn AA. Rupture of the patellar ligament after use of its central third for anterior cruciate reconstruction: a report of two cases. J Bone Joint Surg Am. 1984;66(8):1294–1297. [PubMed] [Google Scholar]
- 4.Carmichael JR, Cross MJ. Why bone-patella tendon-bone grafts should still be considered the gold standard for anterior cruciate ligament reconstruction. Br J Sports Med. 2009;43(5):323–325. [DOI] [PubMed] [Google Scholar]
- 5.Cerulli G, Placella G, Sebastiani E, Tei MM, Speziali A, Manfreda F. ACL reconstruction: choosing the graft. Joints. 2013;1(1):18–24. [PMC free article] [PubMed] [Google Scholar]
- 6.Christen B, Jakob RP. Fractures associated with patellar ligament grafts in cruciate ligament surgery. J Bone Joint Surg Br. 1992;74(4):617–619. [DOI] [PubMed] [Google Scholar]
- 7.Farahmand F, Sejiavongse W, Amis AA. Quantitative study of the quadriceps muscles and trochlear groove geometry related to instability of the patellofemoral joint. J Orthop Res. 1998;16(1):136–143. [DOI] [PubMed] [Google Scholar]
- 8.Fu FH, Rabuck SJ, West RV, Tashman S, Irrgang JJ. Patellar fractures after the harvest of a quadriceps tendon autograft with a bone block: a case series. Orthop J Sports Med. 2019;7(3):2325967119829051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fu FH, Schulte KR. Anterior cruciate ligament surgery 1996: state of the art? Clin Orthop Relat Res. 1996;(325):19–24. [DOI] [PubMed] [Google Scholar]
- 10.Gorschewsky O, Klakow A, Pütz A, Mahn H, Neumann W. Clinical comparison of the autologous quadriceps tendon (BQT) and the autologous patella tendon (BPTB) for the reconstruction of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2007;15(11):1284–1292. [DOI] [PubMed] [Google Scholar]
- 11.Granan L-P, Forssblad M, Lind M, Engebretsen L. The Scandinavian ACL registries 2004–2007: baseline epidemiology. Acta Orthop. 2009;80(5):563–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Han HS, Seong SC, Lee S, Lee MC. Anterior cruciate ligament reconstruction: quadriceps versus patellar autograft. Clin Orthop Relat Res. 2008;466(1):198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harris NL, Smith DA, Lamoreaux L, Purnell M. Central quadriceps tendon for anterior cruciate ligament reconstruction, part I: morphometric and biomechanical evaluation. Am J Sports Med. 1997;25(1):23–28. [DOI] [PubMed] [Google Scholar]
- 14.Iriuchishima T, Shirakura K, Yorifuji H, Fu FH. Anatomical evaluation of the rectus femoris tendon and its related structures. Arch Orthop Trauma Surg. 2012;132(11):1665–1668. [DOI] [PubMed] [Google Scholar]
- 15.Järvelä T, Kannus P, Järvinen M. Anterior knee pain 7 years after an anterior cruciate ligament reconstruction with a bone-patellar tendon-bone autograft. Scand J Med Sci Sports. 2000;10(4):221–227. [DOI] [PubMed] [Google Scholar]
- 16.Kartus J, Magnusson L, Stener S, Brandsson S, Eriksson BI, Karlsson J. Complications following arthroscopic anterior cruciate ligament reconstruction: a 2-5-year follow-up of 604 patients with special emphasis on anterior knee pain. Knee Surg Sports Traumatol Arthrosc. 1999;7(1):2–8. [DOI] [PubMed] [Google Scholar]
- 17.Kennedy NI, Wijdicks CA, Goldsmith MT, et al. Kinematic analysis of the posterior cruciate ligament, part 1: the individual and collective function of the anterolateral and posteromedial bundles. Am J Sports Med. 2013;41(12):2828–2838. [DOI] [PubMed] [Google Scholar]
- 18.Kim S-J, Chang J-H, Kim T-W, Jo S-B, Oh K-S. Anterior cruciate ligament reconstruction with use of a single or double-bundle technique in patients with generalized ligamentous laxity. J Bone Joint Surg Am. 2009;91(2):257–262. [DOI] [PubMed] [Google Scholar]
- 19.Kim S-J, Kumar P, Oh K-S. Anterior cruciate ligament reconstruction: autogenous quadriceps tendon-bone compared with bone-patellar tendon-bone grafts at 2-year follow-up. Arthroscopy. 2009;25(2):137–144. [DOI] [PubMed] [Google Scholar]
- 20.Kim S-J, Lee S-K, Choi CH, Kim S-H, Kim S-H, Jung M. Graft selection in anterior cruciate ligament reconstruction for smoking patients. Am J Sports Med. 2014;42(1):166–172. [DOI] [PubMed] [Google Scholar]
- 21.Laxdal G, Kartus J, Hansson L, Heidvall M, Ejerhed L, Karlsson J. A prospective randomized comparison of bone-patellar tendon-bone and hamstring grafts for anterior cruciate ligament reconstruction. Arthroscopy. 2005;21(1):34–42. [DOI] [PubMed] [Google Scholar]
- 22.Lie MM, Risberg MA, Storheim K, Engebretsen L, Øiestad BE. What’s the rate of knee osteoarthritis 10 years after anterior cruciate ligament injury? An updated systematic review. Br J Sports Med. 2019;53(18):1162–1167. [DOI] [PubMed] [Google Scholar]
- 23.Lind M, Strauss MJ, Nielsen T, Engebretsen L. Low surgical routine increases revision rates after quadriceps tendon autograft for anterior cruciate ligament reconstruction: results from the Danish Knee Ligament Reconstruction Registry. Knee Surg Sports Traumatol Arthrosc. 2021;29(6):1880–1886. [DOI] [PubMed] [Google Scholar]
- 24.Lind M, Strauss MJ, Nielsen T, Engebretsen L. Quadriceps tendon autograft for anterior cruciate ligament reconstruction is associated with high revision rates: results from the Danish Knee Ligament Registry. Knee Surg Sports Traumatol Arthrosc. 2020;28(7):2163–2169. [DOI] [PubMed] [Google Scholar]
- 25.Lippe J, Armstrong A, Fulkerson JP. Anatomic guidelines for harvesting a quadriceps free tendon autograft for anterior cruciate ligament reconstruction. Arthroscopy. 2012;28(7):980–984. [DOI] [PubMed] [Google Scholar]
- 26.Lund B, Nielsen T, Faunø P, Christiansen SE, Lind M. Is quadriceps tendon a better graft choice than patellar tendon? A prospective randomized study. Arthroscopy. 2014;30(5):593–598. [DOI] [PubMed] [Google Scholar]
- 27.Persson A, Fjeldsgaard K, Gjertsen J-E, et al. Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: a study of 12,643 patients from the Norwegian Cruciate Ligament Registry, 2004-2012. Am J Sports Med. 2014;42(2):285–291. [DOI] [PubMed] [Google Scholar]
- 28.Potage D, Duparc F, D’Utruy A, Courage O, Roussignol X. Mapping the quadriceps tendon: an anatomic and morphometric study to guide tendon harvesting. Surg Radiol Anat. 2015;37(9):1063–1067. [DOI] [PubMed] [Google Scholar]
- 29.Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind M. Comparison of hamstring tendon and patellar tendon grafts in anterior cruciate ligament reconstruction in a nationwide population-based cohort study: results from the Danish Registry of Knee Ligament Reconstruction. Am J Sports Med. 2014;42(2):278–284. [DOI] [PubMed] [Google Scholar]
- 30.Shani RH, Umpierez E, Nasert M, Hiza EA, Xerogeanes J. Biomechanical comparison of quadriceps and patellar tendon grafts in anterior cruciate ligament reconstruction. Arthroscopy. 2016;32(1):71–75. [DOI] [PubMed] [Google Scholar]
- 31.Slone HS, Romine SE, Premkumar A, Xerogeanes JW. Quadriceps tendon autograft for anterior cruciate ligament reconstruction: a comprehensive review of current literature and systematic review of clinical results. Arthroscopy. 2015;31(3):541–554. [DOI] [PubMed] [Google Scholar]
- 32.Stäubli HU, Jakob RP. Central quadriceps tendon for anterior cruciate ligament reconstruction, part I: morphometric and biochemical evaluation. Am J Sports Med. 1997;25(5):725–727. [PubMed] [Google Scholar]
- 33.Urchek R, Karas S. Biomechanical comparison of quadriceps and 6-strand hamstring tendon grafts in anterior cruciate ligament reconstruction. Orthop J Sports Med. 2019;7(10):2325967119879113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Waligora AC, Johanson NA, Hirsch BE. Clinical anatomy of the quadriceps femoris and extensor apparatus of the knee. Clin Orthop Relat Res. 2009;467(12):3297–3306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Widner M, Dunleavy M, Lynch S. Outcomes following ACL reconstruction based on graft type: are all grafts equivalent? Curr Rev Musculoskelet Med. 2019;12(4):460–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wijdicks CA, Kennedy NI, Goldsmith MT, et al. Kinematic analysis of the posterior cruciate ligament, part 2: a comparison of anatomic single- versus double-bundle reconstruction. Am J Sports Med. 2013;41(12):2839–2848. [DOI] [PubMed] [Google Scholar]





