Abstract
The present study is systematic rapid review on the nature of the relationship between the COVID-19 pandemic and child maltreatment. Database searches on December 28, 2020, identified 234 unique citations; 12 were ultimately included in our analysis. Included articles measured child maltreatment inclusive of physical, psychological, and sexual abuse, and child neglect during the COVID-19 pandemic. Compared with the prepandemic period, 5 articles found an increase in child maltreatment, 6 articles found a decrease, and 1 study found no difference. There existed variation in geography of study location, age of child maltreatment victims, and types of child maltreatment assessed.
Keywords: COVID-19, Pandemic, Child maltreatment, Abuse, Neglect
Key points
-
•
Findings of the included articles are mixed; 5 articles documented an increase in child maltreatment, 6 articles documented a decrease, and 1 study found no significant difference in child maltreatment rates.
-
•
Of the included articles, rates of child maltreatment reports decreased while hospital cases of child maltreatment increased, calling the accuracy of reporting during the COIVD-19 pandemic into question.
-
•
Most articles (11 of 12) did not include perspectives of children affected by child maltreatment.
It is estimated that each year more than 1 million children worldwide are victims of physical, sexual, or emotional violence. Collectively, this violence has been termed child maltreatment (CM) and defined by the World Health Organization as “the abuse and neglect that occurs to children under 18 years of age.”1 The impacts of CM are multifaceted, having short- and long-term consequences on a child’s attitudes and behaviors, as well as their mental and physical well-being.2, 3, 4, 5, 6 Increases in CM have been well-documented in association with increased parental stress,7 during and after recessions and epidemics, such as the Ebola and AIDS crises.8, 9, 10 Continuing to understand the situations that create, perpetuate, and amplify CM are of the utmost importance to then lower the rates of CM and decrease their impact. Thus, the ongoing coronavirus disease 2019 (COVID-19) pandemic and its subsequent impacts have become an area of interest and concern for linkages to CM.
The ongoing COVID-19 pandemic has permeated daily life and activities, with more than 2.3 million global deaths at the time of this publication.11 Mass lockdowns, stay-at-home orders, shelter-in-place orders, and general encouragement or enforcement to distance from anyone outside of the household have been implemented to mitigate COVID-19 infection rates, hospitalizations, and deaths.1 , 12 , 13 Although the infection and death rates do require drastic isolation measures, there may be negative impacts of such measures as well. The crisis, along with government-implemented isolating measures, have led to economic, psychological, and social hardship for people across the globe.14, 15, 16 These other effects of the pandemic, or the country’s response to it, might impact CM.
The pandemic has exacerbated factors that contribute to CM. For parents, quarantines and stay-at-home orders have led to high rates of unemployment, difficulties in relationships, increased rates of depression, and unsurmountable stress.17, 18, 19 Emerging research has suggested that parents experiencing pandemic-related social isolation report an increase in verbal aggression, physical punishment such as spanking or hitting, and neglectful behaviors toward their children.20 The COVID-19 pandemic has caused significant economic challenges and could have long lasting effects on the global economy.21 , 22 Last, more than 80% of children worldwide were affected by school closures during the pandemic.23 In some countries, educational personnel make up the largest proportion of reporters in cases of CM.24 Research has shown that because of school closures owing to the COVID-19 pandemic, there is a decrease in CM reports.25 Routine pediatric medical care has also decreased as a function of the COVID-19 pandemic, leaving fewer opportunities for health care providers to find out about and report a CM case. Although it is clear the COVID-19 pandemic has created a variety of circumstances that are known to be indicative of an increase in CM, the pandemic is still evolving, and currently available studies cannot fully assess the lasting impacts.
The examination of CM during the COVID-19 pandemic has proven to be difficult, with mixed reports of increased, decreased, or varied results in cases of child abuse and neglect.25 At a time when many victims are isolated within a violent household and are unable to disclose events while separated from the perpetrator,10 instances of CM are difficult to trace. Thus, a need to better understand and synthesize the existing literature surrounding the COVID-19 pandemic and CM is needed. To the authors’ knowledge, this is the first review of its kind to explore the current literature in this field of study and, therefore, this systematic rapid review aims to address (1) the types of study designs used to analyze an ongoing situation, (2) whether CM trends vary by reporting type, and (3) the sources (primary vs secondary) used to gain insight into CM. Synthesizing this information, all published during the pandemic, provides a glimpse into the academic dialogue on this topic in real time.
Methods
Article Inclusion and Exclusion Criteria
To be included, an article had to (1) include a measure of CM during the COVID-19 pandemic, (2) be published in a peer-reviewed journal, (3) be written in English, and (4) present original empirical findings (eg, no reviews, case studies, or news articles were eligible). Articles were excluded if they were inaccessible to reviewers or if they described the development of a tool or measure. Inaccessible articles are those that did not have a full-text download available or charged a fee.
Search Strategy
The systematic rapid review was conducted in accordance with the 2009 PRISMA statement.26 Two experienced research librarians independently conducted a literature search on December 28, 2020. Both developed their search strategies in MEDLINE, and translated these searches into Embase, PsycInfo, and CINAHL. The searches were based on a combination of terms related to “maltreatment” (eg, “physical abuse,” “sexual abuse,” “neglect”) AND “child” (eg, “adolescent,” “girl,” “boy,” “young”). It was limited to the COVID-19 pandemic and English language. After their separate searches, the librarians met to compare search results. Duplicate articles between databases and librarians were removed, and the remaining articles were sent to the study team.
Data Extraction
Two independent reviewers (G.F. and A.C.R.) conducted an abstract review of the resulting 234 unique articles. Reviewers indicated whether an article fit or did not fit the inclusion criteria, and each article they disagreed on was discussed among 3 reviewers (G.F., A.C.R., and A.R.) until consensus was reached. A total of 27 articles remained and were retrieved for full-text review and abstraction.
Quality Assessment
Three reviewers (G.F., A.C.R., and A.R.) used the National Institutes of Health National Heart, Lung, and Blood Institute Study Quality Assessment Toolbox27 to ensure that all of the included articles were free of significant bias.
Ethics
This study was not submitted to an institutional review board because a rapid literature review does not involve human participants.
Results
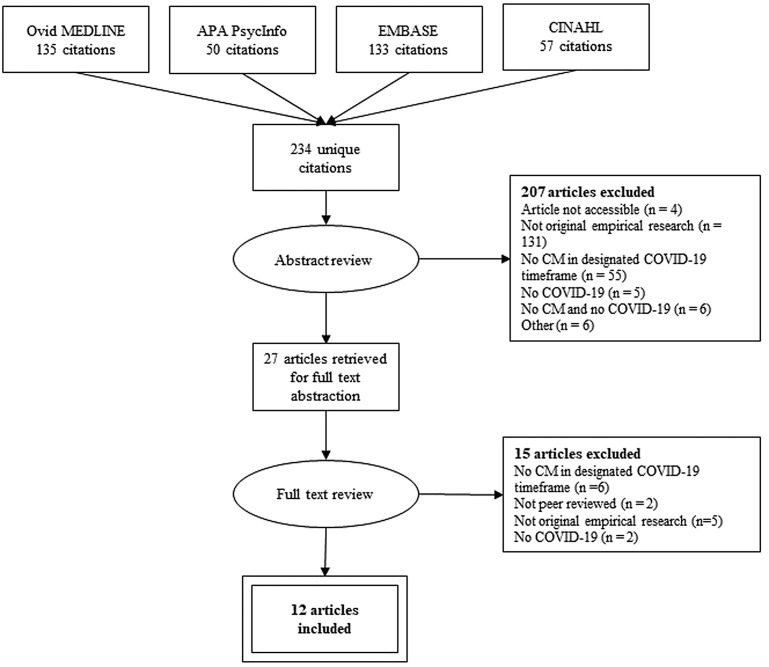
A total of 234 unique citations were generated from the databases. After the initial abstract screen, 207 articles were removed. Most commonly, articles were removed because they were not original empirical research (n = 131), meaning that they were either a letter to the editor, a viewpoint or debate piece, a review paper, or a news report. Articles were also excluded if they did not include any current child abuse (n = 55), meaning that child abuse was either not mentioned, not included in the statistical analysis, or that child abuse history was only used as a study inclusion factor for adult subjects. Articles that did not include COVID-19 (n = 5) and articles that included neither COVID-19 nor present child abuse (n = 6) were excluded as well. Other reasons for exclusion were that the article was not accessible to reviewers (n = 3 did not have a full-text download available, n = 1 charged a fee to view), only the abstract was published (n = 1), the article was an animal study (n = 1), the article was a program evaluation (n = 1), the research was conducted for development of a clinical tool (n = 1), or the article was a workshop description (n = 1). Each reason for exclusion with only 1 article is categorized as other in Fig. 1 .
Fig. 1.
PRISMA flowchart of the article identification, selection, and abstraction process. APA, American Psychological Association.
Of the remaining 27 full-text articles that were reviewed, 15 articles were excluded. Articles were removed because they had no current child abuse (n = 6), were not peer reviewed (n = 2), were not original empirical research (n = 5), or did not include COVID-19 (n = 2). A final count of 12 articles were ultimately included in this systematic rapid review, outlined in Table 1 . Each of these articles were deemed appropriate for inclusion based on the quality assessment measure.27 Overall, 10 articles received a score of good and 2 received a score of fair. According to the tool, “a ‘good’ study has the least risk of bias, and results are considered valid, while a ‘fair’ study is susceptible to some bias deemed not sufficient to invalidate its results.”27 None of the included articles were deemed poor, which would indicate significant bias.
Table 1.
Articles assessing CM during the COVID-19 pandemic
| Author (Year) | Study Design | Sample Source and Sample Size | Sample Characteristics | Data Time Frame (MM/DD/YYYY) | Child Maltreatment Operational Definition | Findings | NIH NHLBI Study Quality Assessment |
|---|---|---|---|---|---|---|---|
| Barboza (2020)21 | Negative binomial regression analysis of surveillance data |
|
|
07/24/2019–01/20/2020 compared to 01/21/2020–07/19/2020 |
|
Compared to the time period immediately preceeding it, there was a 7.95% decrease in the number of child abuse and neglect reports during the COVID-19 pandemic. | Good |
| Bérubé (2020)33 | Cross sectional analysis from a prospective longitudinal cohort |
|
85.7% Female; mean age = 40.2; no race data reported | 04/29/2020–05/10/2020 |
|
Compared to parents of children aged 0–12, parents of teenaged children were signifcantly less likely to be able to respond to their child's basic care needs (P<.001). | Fair |
| Chong (2020)34 | Retrospective review |
|
|
|
|
The hospital saw a greater proportion of child abuse-related emergencies during lockdown (44 children, 0.5% of emergencies) and post-lockdown (79%, 0.6%) compared to pre-DORSCON orange (36%, 0.2%) (P<.001). | Good |
| Degiorgio (2020)35 | Retrospective review |
|
|
|
|
Compared to the same period in 2019, there was a higher percentage of child abuse or social paediatric cases in 2020 (0.14% vs 3.5% of cases) (P<.001) | Good |
| Garstang (2020)36 | Retrospective review |
|
37% Female; median age = 69 mo; no race data reported | compared 03/2018–6/2018; 03/2019–6/2019; 03/2020–6/2020 |
|
Compared to the same period in 2018 and 2019, there was a decrease in CPME referrals in 2020 (39% reduction; 95% CI: (14%, 57%)). | Good |
| Kovler (2020)30 | Retrospective review |
|
|
compared 3/28/2018–04/27/2018; 3/28/2019–04/27/2019; 3/28/2020–04/27/2020 |
|
Compared to the same period in 2018 and 2019, there was a significantly higher proportion of trauma patients treated for child-abuse related injuries in 2020 (P = .009) | Good |
| Martins-Filho (2020)37 | Retrospective population-based study |
|
|
01/01/2019–06/30/2019 compared to 01/01/2019–06/30/2020 |
|
Compared to 2019, child physical injury decreased by 24.3% in 2020. Decreasing rates occurred in January, February, March, and May. | Good |
| Platt (2020)38 | Cross-sectional descriptive analysis |
|
-- | compared 01/01/2020–03/15/2020; 03/16/2020–05/31/2020 |
|
Compared to the period before the lockdown, there was a decrease of 55.3% in notifications during the isolation period (1192 vs 659 notifications). | Good |
| Rapoport (2020)31 | Retrospective analysis using SARIMA modeling |
|
– |
|
|
|
Good |
| Sidpra (2020)39 | Retrospective Review |
|
40% Female; mean age = 192 d (range = 17–401 d); no race data reported | compared 03/23/2020–04/23/2020 with incidence in the previous 3 y (no dates provided) |
|
Compared to the same period in the previous 3 years, there was a 1493% increase in cases of AHT between March 23 and April 23, 2020. | Good |
| Tierolf (2020)40 | mixed methods study: quantitative analysis is longitudinal, qualitative analysis is a sub-study |
|
|
∼1.5 y prior to 03/16/2020; 03/16/2020 -- ongoing parent study |
|
No significant difference in number of child abuse and neglect inclidents reported by parents or teenagers before the COVID-19 crisis and after 03/16/2020. | Fair |
| Whelan (2020)32 | Retrospective analysis using ARIMA modeling |
|
-- |
|
|
|
Good |
Abbreviations: AHT, abusive head trauma; ARIMA, auto regressive integrated moving average; CAN, child abuse and neglect; CI, confidence interval; COVID -19, coronavirus disease 2019; CPS, Child Protective Services; DORSCON, Disease Outbreak Response System Condition; EHR, electronic health record; ICD, International Classification of Diseases; MAVIPAN, "Ma vie et la pandemic au Québec"; MNBS, Multidimensional Neglectful Behavior Scale; NHLBI, National Heart, Lung, and Blood Institute; NIH, National Institutes of Health; SNOMED-CT, Systematized Nomenclature of Medicine -- Clinical Terms; SARIMA, seasonal auto regressive integrated moving average.
Sample Characteristics
Reflective of the global scale of the COVID-19 pandemic, there is geographic diversity among the included articles. Four evaluations took place in the United States,28, 29, 30, 31 and the other 8 are from outside of the United States, including Brazil, the Netherlands, and the UK.32, 33, 34, 35, 36, 37, 38, 39 The articles ranged in sample size, with the smallest sample including 12 children,38 the median 2 samples including 392 children in one31 and 414 parents in the other,32 and the largest sample coming from hospital records of CM for 58,367 children.33 Of the articles, one was a survey of parents,32 and one included responses from children.39 All other articles synthesized information from child abuse reporting or presentation to a hospital. Maltreated children were from all age groups. At the youngest end of the spectrum, Sidpra and associates38 looked at children from 17 days to 401 days old, with a mean age of 192 days. Conversely, Platt and colleagues37 included children aged 0 to 19 years, based on the 2002 definition the authors used to define children and adolescents. Three articles did not report a mean age or age range.30 , 31 , 38
Study Designs
A variety of study designs were used to assess the relationship between the COVID-19 pandemic and CM. The most common study design was retrospective review. Six articles used this method.29 , 33, 34, 35, 36 , 38 Two articles use retrospective data to compare forecasted trends in CM to actual reports of CM.30 , 31 One was a cross-sectional analysis of survey data,32 and another was a cross-sectional analysis of violence notifications.37
Definition of Child Maltreatment
CM was operationalized with some nuance across articles. Some relied solely on diagnostic codes,33 , 34 whereas others also considered suspicions or allegations of maltreatment.29 , 30 , 35 , 37 , 38 Additionally, the scope of CM varied: 11 of the articles included physical abuse against a child,28, 29, 30, 31 , 33, 34, 35, 36, 37, 38, 39 7 were inclusive of child neglect,28 , 30, 31, 32 , 35 , 37 , 39 and 2 included psychological abuse.37 , 39
Qualitative Synthesis of Findings
Overall, 5 articles documented increased CM, 6 articles documented decreased CM, and 1 article found no significant difference in CM trends between the prepandemic period and during the pandemic.
Setting of reports
Four articles discussed incidence of CM in a hospital setting.29 , 33 , 34 , 38 Six articles discussed incidence of CM from crime reports and Child Protective Services reports.28 , 30 , 31 , 35, 36, 37 Each of the 4 articles that generated reports from a hospital setting found an increased incidence of CM. Contrastingly, each of the 6 articles based on crime and Child Protective Services reports found a decreased incidence of CM.
Forecasted versus actual
Two articles comparing forecasted versus actual trends in CM reports.30 , 31 These articles used similar modeling techniques (seasonal autoregressive integrated moving average and autoregressive integrated moving average), in different settings. Rapoport and associates31 examined New York City, and Whelan and coworkers32 examined the state of Oklahoma. Both analyses found significantly less allegations during the COVID-19 pandemic than expected. Rapoport and coworkers31 saw less reports than expected from March to May 2020, and Whelan and colleagues32 saw less reports than expected in February and April to June 2020.
Discussion
This study used systematic rapid review methodology to explore the impact of the COVID-19 pandemic on CM. The variability in findings across the included articles expose the complexity of this relationship, especially as the situation is developing in real time. The type of study design, the report setting, and the source of the information on the CM were explored and are discussed in detail elsewhere in this article.
The most common study design used was retrospective review, where researchers compared trends in CM from previous time periods with a time period during the lockdown. The lockdown period was defined differently across articles, with one using “COVID Wave One” and the timepoint of interest,34 another using Disease Outbreak Response System Condition, or DORSCON, stages,33 and still others defining date ranges of a few months at the height of the lockdown orders.28 , 30 , 31 Thus, data cannot be directly compared owing to differing date ranges.
The rising trends of CM in hospitals and falling trends of CM crime reports during the COVID-19 pandemic is concerning. This trend begets the question of whether reporting is accurate during this time. Access to mandated reporters such as school teachers has been severely limited owing to stay-at-home orders and the transition to virtual schooling, leading to an underreporting of CM.40 Additionally, during the COVID-19 pandemic, there was an increased hesitancy to visit hospitals and clinics.41, 42, 43 The fear of going to the hospital for issues unrelated to COVID-19 could have different implications: less contact with medical professionals who are mandated reporters or only the most severe cases presenting to the hospital. Telemedicine replaced in-person visits for many medical professionals at the height of the pandemic, and providers may have missed usual warning signs of CM. The hospital-based articles included in the present review, however, reported an increase in CM cases, potentially contradicting this hypothesis.29 , 33 , 34 , 38
The articles presented here are predominantly secondary reports. Articles relied on crime reports, health record data, and surveys of parents to understand CM. Just 1 article reported surveying children (aged 3–18 years), but only reported data from the teenagers in the study.39 It was also unclear whether children were completing surveys away from parental influence. Other reports, like the allegations of abuse documented by Rapoport and associates,31 also primarily came from adults such as law enforcement, social services, educational personnel, and caregivers. There is absence of information directly from the children affected by CM, despite how useful it could be. Past year incidence data collected directly from young children and adolescents are both reliable and developmentally appropriate, meaning that they have the cognitive capacity to recall and understand instances of CM.44 The reliance on physical evidence of maltreatment in many of our included articles could result in the underreporting of CM cases, particularly cases where bruises or injuries have healed, where psychological or sexual abuse occurred, or where neglect was involved.29 , 33 , 34 , 38
When parents were surveyed,32 no comparative analyses by sex were completed. Mothers and fathers of children affected by CM were analyzed together as a unit, despite the possibility that parental perspective could vary by gender. It is well-known that parent sex is associated with likelihood of abusing a child and typology of maltreatment committed, although the results are mixed across countries and cultures.45, 46, 47, 48 Sex is also implicated in the relationship between parenting stress and CM potential.49
The associations shown here are subject to confounding. One potential confounder in the relationship between the COVID-19 pandemic and CM is parental stress. It is known that parental stress is a major risk factor of CM.50, 51, 52 Parental stress also increased during the COVID-19 pandemic: fear of the virus, job loss, new rules and mandates, and transitions to virtual work and schooling, among other stressors, were rampant during this time.4 , 18 Additionally, it is documented that economic hardship is a predictor of child neglect.53, 54, 55, 56 The mass layoffs, financial threats to small businesses, and sometimes minimal relief from governments during the COVID-19 pandemic could all be sources of economic hardship for parents.
The greatest strength of the present study is the rigor with which it was conducted at every stage. A.R. trained G.F. and A.C.R. extensively in data abstraction and article selection using the PRISMA method. Three reviewers took part in the multi-pronged article selection process, and all selected articles were screened for quality assurance using the National Institutes of Health National Heart, Lung, and Blood Institute Study Quality Assessment Toolbox.27 A limitation of our study is that it was conducted during the ongoing COVID-19 pandemic. Thus, it is likely that additional articles will be published on this topic as the COVID-19 pandemic develops, and of the articles that are included here, some have small sample sizes.36 , 38 This factor could impact the potential for generalizability to larger samples or populations.
Summary
The global nature of the COVID-19 pandemic warrants future research conducted by geography. Different countries, states, and even different cities define and handle CM cases differently. This variability could contribute to different rates of reporting and incidence of CM. Policy implications on the accuracy of reports should be explored, as should the efficacy of policy measures on CM prevention.
Clinics care points
-
•
Children are particularly vulnerable during the COVID-19 pandemic because stay-at-home orders, minimized access to mandated reporters, and increased parental stress may be associated with increased CM.
-
•
Providers should take extra care to ask children whether CM is occurring in the home and give examples of the different types of CM. Some children, especially those affected by neglect or psychological violence, may not show visible signs of CM. Other children may not know that what they are experiencing is CM.
-
•
Discourse on school, daycare, church, and other institutional reopenings should include special considerations for children at risk of CM and children with a history of CM victimization.
Acknowledgments
The authors acknowledge Brianna Andre and Steven Moore from the Sladen Library at Henry Ford Hospital for their assistance with the literature search.
Disclosure
The authors of this publication declare that they have no relevant or material financial interests that relate to the research described in this paper.
References
- 1.WHO Coronavirus Disease Dashboard Listings of WHO's response to covid-19. World Health Organization. https://covid19.who.int/ Available at: Accessed February 08, 2021.
- 2.Dube S.R., Anda R.F., Felitti V.J., et al. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. JAMA. 2001;286(24):3089–3096. doi: 10.1001/jama.286.24.3089. [DOI] [PubMed] [Google Scholar]
- 3.Felitti V.J., Anda R.F., Nordenberg D., et al. Reprint of: relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the adverse childhood experiences (ACE) study. Am J Prev Med. 2019;56(6):774–786. doi: 10.1016/j.amepre.2019.04.001. [DOI] [PubMed] [Google Scholar]
- 4.Hailes H.P., Yu R., Danese A., et al. Long-term outcomes of childhood sexual abuse: an umbrella review. Lancet Psychiatry. 2019;6(10):830–839. doi: 10.1016/S2215-0366(19)30286-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hemmingsson E., Johansson K., Reynisdottir S. Effects of childhood abuse on adult obesity: a systematic review and meta-analysis. Obes Rev. 2014;15(11):882–893. doi: 10.1111/obr.12216. [DOI] [PubMed] [Google Scholar]
- 6.Hughes K., Bellis M.A., Hardcastle K.A., et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017;2(8):e356–e366. doi: 10.1016/S2468-2667(17)30118-4. [DOI] [PubMed] [Google Scholar]
- 7.Norman R.E., Byambaa M., De R., et al. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Med. 2012;9(11):e1001349. doi: 10.1371/journal.pmed.1001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crouch J.L., Behl L.E. Relationships among parental beliefs in corporal punishment, reported stress, and physical child abuse potential. Child Abuse Neglect. 2001;25(3):413–419. doi: 10.1016/s0145-2134(00)00256-8. [DOI] [PubMed] [Google Scholar]
- 9.Kontos M., Moris D., Davakis S., et al. Physical abuse in the era of financial crisis in Greece. Ann Transl Med. 2017;5(7):155. doi: 10.21037/atm.2017.03.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peterman A., Potts A., O'Donnell M., et al. vol. 528. Center for Global Development; Washington, DC: 2020. (Pandemics and violence against women and children). [Google Scholar]
- 11.Wood J.N., French B., Fromkin J., et al. Association of pediatric abusive head trauma rates with macroeconomic indicators. Acad Pediatr. 2016;16(3):224–232. doi: 10.1016/j.acap.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 12.Koh D. COVID-19 lockdowns throughout the world. Occup Med. 2020;70(5):322. [Google Scholar]
- 13.Moris D., Schizas D. Lockdown during COVID-19: the Greek success. In Vivo. 2020;34(3 suppl):1695–1699. doi: 10.21873/invivo.11963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang K., Vilches T.N., Tariq M., et al. The impact of mask-wearing and shelter-in-place on COVID-19 outbreaks in the United States. Int J Infect Dis. 2020;101:334–341. doi: 10.1016/j.ijid.2020.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tull M.T., Edmonds K.A., Scamaldo K.M., et al. Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Res. 2020;289:113098. doi: 10.1016/j.psychres.2020.113098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wilson J.M., Lee J., Fitzgerald H.N., et al. Job insecurity and financial concern during the COVID-19 pandemic are associated with worse mental health. J Occup Environ Med. 2020;62(9):686–691. doi: 10.1097/JOM.0000000000001962. [DOI] [PubMed] [Google Scholar]
- 17.Xiong J., Lipsitz O., Nasri F., et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affective Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brown S.M., Doom J.R., Lechuga-Peña S., et al. Stress and parenting during the global COVID-19 pandemic [Article] Child Abuse Neglect. 2020;110(Pt 2):104699. doi: 10.1016/j.chiabu.2020.104699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Griffith A.K. Parental burnout and child maltreatment during the covid-19 pandemic. J Fam Violence. 2020:1–7. doi: 10.1007/s10896-020-00172-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patrick S.W., Henkhaus L.E., Zickafoose J.S., et al. Well-being of parents and children during the COVID-19 pandemic: a national survey. Pediatrics. 2020;146(4) doi: 10.1542/peds.2020-016824. e2020016824. [DOI] [PubMed] [Google Scholar]
- 21.Lee S.J., Ward K.P., Lee J.Y., et al. Parental social isolation and child maltreatment risk during the COVID-19 pandemic. J Fam Violence. 2020:1–12. doi: 10.1007/s10896-020-00244-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ceylan R.F., Ozkan B., Mulazimogullari E. Historical evidence for economic effects of COVID-19. Eur J Health Econ. 2020;21(6):817–823. doi: 10.1007/s10198-020-01206-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Medel-Herrero A., Shumway M., Smiley-Jewell S., et al. The impact of the Great Recession on California domestic violence events, and related hospitalizations and emergency service visits. Prev Med. 2020;139:106186. doi: 10.1016/j.ypmed.2020.106186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.UNESCO COVID-19 impact on education. https://en.unesco.org/covid19/educationrespons Available at: Accessed January 3, 2021.
- 25.Child Welfare Information Gateway . U.S. Department of Health and Human Services, Children’s Bureau; Washington, DC: 2003. The role of educators in preventing and responding to child abuse and neglect. [Google Scholar]
- 26.Sharma A., Borah S.B. Covid-19 and domestic violence: an indirect path to social and economic crisis. J Fam Violence. 2020:1–7. doi: 10.1007/s10896-020-00188-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moher D., Altman D.G., Liberati A., et al. PRISMA statement. Epidemiology. 2011;22(1):128. doi: 10.1097/EDE.0b013e3181fe7825. [DOI] [PubMed] [Google Scholar]
- 28.Quality assessment tool for observational cohort and cross-sectional studies. National Heart Lung and Blood Institute; 2014. https://www.nhlbi.nih.gov/node/80102 Available at: [Google Scholar]
- 29.Barboza G.E., Schiamberg L.B., Pachl L. A spatiotemporal analysis of the impact of COVID-19 on child abuse and neglect in the city of Los Angeles, California. Child Abuse Neglect. 2021;116(Pt 2):104740. doi: 10.1016/j.chiabu.2020.104740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kovler M.L., Ziegfeld S., Ryan L.M., et al. Increased proportion of physical child abuse injuries at a level I pediatric trauma center during the Covid-19 pandemic. Child Abuse Neglect. 2021;116(Pt 2):104756. doi: 10.1016/j.chiabu.2020.104756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rapoport E., Reisert H., Schoeman E., et al. Reporting of child maltreatment during the SARS-CoV-2 pandemic in New York City from March to May 2020. Child Abuse Neglect. 2021;116(Pt 2):104719. doi: 10.1016/j.chiabu.2020.104719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Whelan J., Hartwell M., Chesher T., et al. Deviations in criminal filings of child abuse and neglect during COVID-19 from forecasted models: an analysis of the state of Oklahoma, USA. Child Abuse Neglect. 2021;116(Pt 2):104863. doi: 10.1016/j.chiabu.2020.104863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bérubé A., Clément M.È., Lafantaisie V., et al. How societal responses to COVID-19 could contribute to child neglect. Child Abuse Neglect. 2020;116(Pt 2):104761. doi: 10.1016/j.chiabu.2020.104761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chong S.L., Soo J.S.L., Allen J.C., et al. Impact of COVID-19 on pediatric emergencies and hospitalizations in Singapore. BMC Pediatr. 2020;20(1):562. doi: 10.1186/s12887-020-02469-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Degiorgio S., Grech N., Dimech Y.M., et al. COVID-19 related acute decline in paediatric admissions in Malta, a population-based study. Early Hum Dev. 2020:105251. doi: 10.1016/j.earlhumdev.2020.105251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Garstang J., Debelle G., Anand I., et al. Effect of COVID-19 lockdown on child protection medical assessments: a retrospective observational study in Birmingham, UK. BMJ Open. 2020;10(9):e042867. doi: 10.1136/bmjopen-2020-042867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Martins Filho P.R., Damascena N.P., Lage R.C.M., et al. Decrease in child abuse notifications during COVID-19 outbreak: a reason for worry or celebration? J Paediatrics Child Health. 2020;56(12):1980–1981. doi: 10.1111/jpc.15213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Platt V.B., Guedert J.M., Coelho E.B.S. Violence against children and adolescents: notification and alert in times of pandemic. Rev Paul Pediatr. 2020;39:e2020267. doi: 10.1590/1984-0462/2021/39/2020267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sidpra J., Abomeli D., Hameed B., et al. Rise in the incidence of abusive head trauma during the COVID-19 pandemic [Letter] Arch Dis Child. 2021;106(3):e14. doi: 10.1136/archdischild-2020-319872. [DOI] [PubMed] [Google Scholar]
- 40.Tierolf B., Geurts E., Steketee M. Domestic violence in families in The Netherlands during the coronavirus crisis: a mixed method study. Child Abuse Neglect. 2021;116(Pt 2):104800. doi: 10.1016/j.chiabu.2020.104800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Baron E.J., Goldstein E.G., Wallace C.T. Suffering in silence: how COVID-19 school closures inhibit the reporting of child maltreatment. J Public Econ. 2020;190:104258. doi: 10.1016/j.jpubeco.2020.104258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.American Heart Association News . 2020. Is it safe to go to the hospital during COVID-19 pandemic? Doctors say yes.www.heart.orghttps://www.heart.org/en/news/2020/05/04/is-it-safe-to-go-to-the-hospital-during-covid-19-pandemic-doctors-say-yes Available at: [Google Scholar]
- 43.Weiner S. 2020. Go to the hospital if you need emergency care, even in the era of COVID-19. Harvard Health Blog.https://www.health.harvard.edu/blog/go-to-the-hospital-if-you-need-emergency-care-even-in-the-era-of-covid-19-2020050519760 Available at: [Google Scholar]
- 44.HealthPartners . 2020. Is it safe to get health care during COVID-19?: HealthPartners. HealthPartners Blog.https://www.healthpartners.com/blog/what-were-doing-to-help-you-get-care-safely-during-covid-19/ Available at: [Google Scholar]
- 45.Mathews B., Pacella R., Dunne M.P., et al. Improving measurement of child abuse and neglect: a systematic review and analysis of national prevalence studies. PLoS One. 2020;15(1):e0227884. doi: 10.1371/journal.pone.0227884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cui N., Xue J., Connolly C.A., et al. Does the gender of parent or child matter in child maltreatment in China? Child Abuse Neglect. 2016;54:1–9. doi: 10.1016/j.chiabu.2016.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Middel F., López M.L., Fluke J., et al. The effects of migrant background and parent gender on child protection decision-making: an intersectional analysis. Child Abuse Neglect. 2020;104:104479. doi: 10.1016/j.chiabu.2020.104479. [DOI] [PubMed] [Google Scholar]
- 48.Romero-Martínez A., Figueiredo B., Moya-Albiol L. Childhood history of abuse and child abuse potential: the role of parent's gender and timing of childhood abuse. Child Abuse Neglect. 2014;38(3):510–516. doi: 10.1016/j.chiabu.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 49.Wolf J.P. Parent gender as a moderator: the relationships between social support, collective efficacy, and child physical abuse in a community sample. Child Maltreat. 2015;20(2):125. doi: 10.1177/1077559514562606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Miragoli S., Balzarotti S., Camisasca E., et al. Parents’ perception of child behavior, parenting stress, and child abuse potential: Individual and partner influences. Child Abuse Neglect. 2018;84:146–156. doi: 10.1016/j.chiabu.2018.07.034. [DOI] [PubMed] [Google Scholar]
- 51.Whipple E.E., Webster-Stratton C. The role of parental stress in physically abusive families. Child Abuse Neglect. 1991;15(3):279–291. doi: 10.1016/0145-2134(91)90072-l. [DOI] [PubMed] [Google Scholar]
- 52.Chung G., Lanier P., Wong P.Y.J. Mediating effects of parental stress on harsh parenting and parent-child relationship during coronavirus (covid-19) pandemic in Singapore. J Fam Violence. 2020:1–12. doi: 10.1007/s10896-020-00200-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Guterman N.B., Lee S.J., Taylor C.A., et al. Parental perceptions of neighborhood processes, stress, personal control, and risk for physical child abuse and neglect. Child Abuse Neglect. 2009;33(12):897–906. doi: 10.1016/j.chiabu.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 54.Berger L.M., Font S.A., Slack K.S., et al. Income and child maltreatment in unmarried families: evidence from the earned income tax credit. Rev Econ Household. 2017;15(4):1345–1372. doi: 10.1007/s11150-016-9346-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lawson M., Piel M.H., Simon M. Child maltreatment during the COVID-19 pandemic: consequences of parental job loss on psychological and physical abuse towards children. Child Abuse Neglect. 2020;110(Pt 2):104709. doi: 10.1016/j.chiabu.2020.104709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lefebvre R., Fallon B., Van Wert M., et al. Examining the relationship between economic hardship and child maltreatment using data from the Ontario Incidence Study of Reported Child Abuse and Neglect-2013 (OIS-2013) Behav Sci. 2017;7(1):6. doi: 10.3390/bs7010006. [DOI] [PMC free article] [PubMed] [Google Scholar]