To the Editor:
Patients hospitalized for severe coronavirus disease 2019 (COVID-19) may present with persistent symptoms and functional impairment for months after infection.1 , 2 A proportion of those patients may need further hospitalization for rehabilitation or proper care transition.3 However, little is known about outcomes after such hospitalizations.4 We assessed long-term outcomes of patients admitted to a post-acute care facility (PACF) after a severe COVID-19 hospitalization.
Our study evaluated a cohort of patients with severe COVID-19 treated at a 60-bed private PACF in Brazil. Data were collected at PACF admission, discharge, and follow-up by telephone. Functional status was assessed by modified Barthel Index (20-100 points).5 Mental health symptoms and quality of life were assessed by the Hospital Anxiety and Depression Scale (HADS) and the EQ-5D-3L score, respectively. Categorical variables with repeated measures were compared with Friedman test and a P value <.05 was considered significant. This study was approved by the institutional review board (Hospital das Clinicas da Faculdade de Medicina da Universidade de Sao Paulo (HCFMUSP), number 43277021.7.0000.0068), and informed consent was obtained from participants.
We report the first 100 patients admitted at the PACF after severe COVID-19 from April 2020 to April 2021. Follow-up was performed until June 8, 2021.
Patients were admitted to the PACF from 12 different hospitals, with a median (interquartile range) of 33 (23-42) days from symptom onset. The mean age was 65 ± 15 years, and 63 (63%) were male. Mean Charlson Comorbidity Index was 2.5 ± 1.9, and 86 (86%) were independent for all activities of daily living before hospitalization. Patients were hospitalized for 32 (24-42) days before transition to PACF, and 91 (91%) were admitted in the intensive care unit, 79 (79%) received invasive mechanical ventilation, and 3 (3%) received extracorporeal membrane oxygenation during the original hospitalization.
At admission to the PACF, 41 (41%) patients were in use of tracheostomy tube, 52 (52%) with tube feeding, 63 (63%) needed oxygen supplementation, and 5 (5%) were mechanically ventilated. Median PACF length of stay was 28 (15-46) days. Nine (9%) patients were readmitted to an acute care hospital due to clinical deterioration and 12 (12%) patients died during PACF hospitalization.
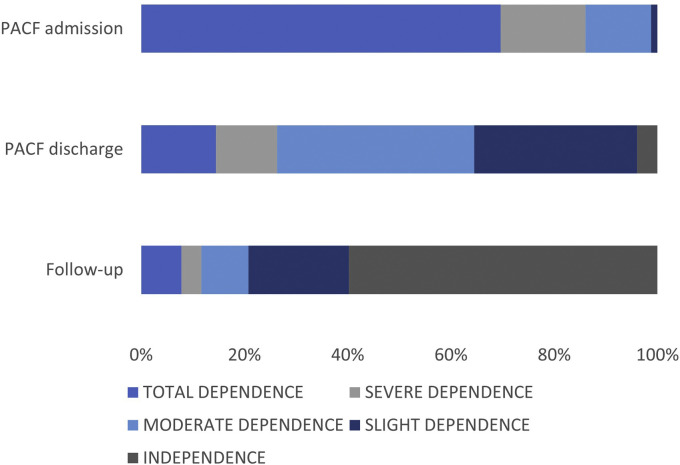
At follow-up, for a median (interquartile range) of 54 (40-91) days after PACF discharge and 142 (109-276) days after symptom onset, of the 79 patients discharged alive, 2 (2.5%) died, 12 (15%) were readmitted to an acute care hospital, and 70 (88%) reported at least 1 persistent symptom (Table 1 ). Of the 45 patients with active work life before hospitalization, 19 (42%) returned to previous level of work during the follow-up period. At follow-up, mean ± SD scores for modified Barthel Index, EQ-5D-3L, and Hospital Anxiety and Depression Scale anxiety and depression subscale scores were 87 ± 27, 0.69 ± 0.27, 3.55 ± 4.62, and 3.13 ± 5.18, respectively. Participants rated perceived quality of life as much worse, worse, similar, better, and much better in 14 (18%), 29 (38%), 15 (19%), 18 (23%), and 1 (1%), respectively. At PACF admission, 70 (88%) were totally or severely dependent, whereas at discharge and follow-up 21 (26%) and 10 (12%) remained totally or severely dependent (P < .001), respectively (Figure 1 ).
Table 1.
Functional Status, Burden of Symptoms, and Quality of Life at Follow-up (n = 79)
| Characteristics | Value |
|---|---|
| MBI∗, mean ± SD | 43.4 ± 12 |
| EQ-5D-3L score†, mean ± SD | 0.69 ± 0.27 |
| HADS‡ anxiety, mean ± SD | 3.55 ± 4.62 |
| HADS depression, mean ± SD | 3.13 ± 5.28 |
| Prolonged symptoms, n (%) | |
| Dyspnea | 19 (23) |
| Cough | 38 (46) |
| Pain | 40 (48) |
| Fatigue | 50 (60) |
| Anosmia | 6 (7) |
| Headache | 20 (24) |
| Perceived quality of life as compared to before COVID-19, n (%) | |
| Much worse | 18 (22) |
| Worse | 29 (35) |
| Similar | 15 (18) |
| Better | 20 (24) |
| Much better | 1 (1) |
HADS, Hospital Anxiety and Depression Scale; MBI, modified Barthel Index.
Modified Barthel Index (20-100, with 20 being complete dependence and 100 being complete independence).
EQ-5D-3L health state index scores generally range from less than 0 (where 0 is a health state equivalent to death; negative values indicate a state worse than death) to 1 (perfect health).
HADS is assessed in 2 dimensions: anxiety and depression. Each dimension scores from 0 to 21 (higher scores indicating greater chance of symptoms). A score ≥9 is usually interpreted as a cutoff.
Fig. 1.
Functional status, as measured by the modified Barthel Index (MBI) at post-acute care facility (PACF) admission, discharge, and after follow-up (P < .001). The MBI was categorized as total dependence if equal to 20; severe dependence, if between 21 and 60; moderate dependence, if between 61 and 90; mild dependence, if between 91 and 99; independence, if equal to 100.5
Overall, in this cohort of relatively young and previously fit patients admitted to PACF after severe COVID-19, functional status was severely impaired at PACF admission, improved at discharge, and was sustained during follow-up, but there was a high burden of symptoms and perceived lower quality of life among survivors.
Footnotes
JGRR has received a fee for a lecture on post-acute care of COVID-19 patients by Nestle, unrelated to the present study. The other authors declare no conflicts of interest.
References
- 1.Carfi A., Bernabei R., Landi F. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324:603–605. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Aly Z., Xie Y., Bowe B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature. 2021;594:259–264. doi: 10.1038/s41586-021-03553-9. [DOI] [PubMed] [Google Scholar]
- 3.Chopra V., Flanders S.A., O'Malley M. Sixty-day outcomes among patients hospitalized with COVID-19. Ann Intern Med. 2021;174:576–578. doi: 10.7326/M20-5661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Piquet V., Luczak C., Seiler F. Do patients with COVID-19 benefit from rehabilitation? Functional outcomes of the first 100 patients in a COVID-19 rehabilitation unit. Arch Phys Med Rehabil. 2021;102:1067–1074. doi: 10.1016/j.apmr.2021.01.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shah S., Vanclay F., Cooper B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol. 1989;42:703–709. doi: 10.1016/0895-4356(89)90065-6. [DOI] [PubMed] [Google Scholar]