Abstract
Background
Disease outbreaks and disasters can result in excess deaths and severe disruption of usual end-of-life care processes. We aimed to: i) synthesise evidence describing the experiences of health and social care staff providing end-of-life care during a disease outbreak or humanitarian disaster, ii) understand the impact on their mental health and wellbeing and, iii) identify means of support.
Methods
A systematic review with meta-synthesis was conducted including studies of health and social care staff providing end-of-life care during disease outbreaks (Ebola, COVID-19, SARs, MERs) or humanitarian disasters (2001–2020). MEDLINE (Ovid), Embase, PsycInfo, Web of Science, and grey literature databases were searched systematically, with forward and backward citation searching of included studies. Any research study designs, in any care settings, were included. Study quality was assessed using an appraisal tool relevant to each study design. Qualitative meta-synthesis was used to analyse the findings, which were then reported narratively. PROSPERO registration: CRD42020181444.
Results
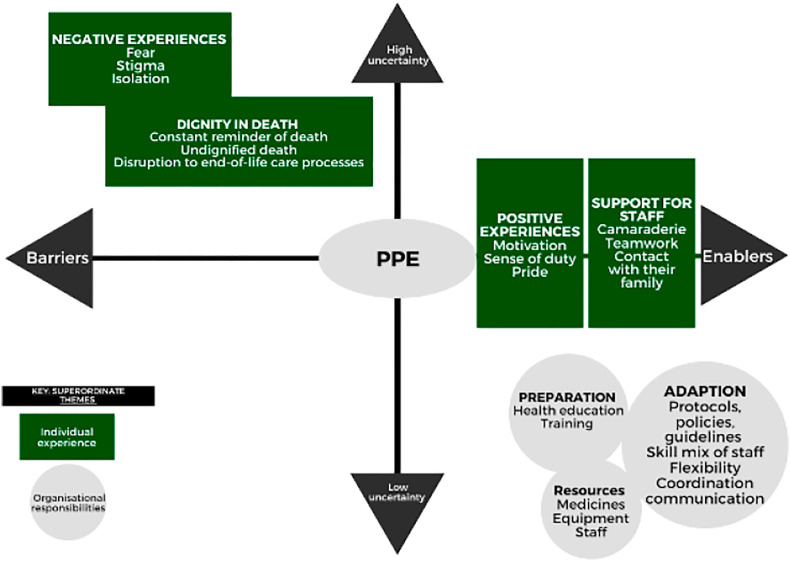
Nineteen studies were included, including 10 Ebola studies and two COVID-19 studies. The analysis generated two superordinate themes: individual experience and organisational responsibilities. Individual experience comprised four themes: dignity in death, positive experiences, negative experience and support for staff. Organisational responsibilities comprised four themes: preparation, adaption, resources, and Personal Protective Equipment (PPE).
Discussion
No studies quantitively measured the impact of providing end-of-life care on staff mental health and wellbeing, however qualitative studies described experiences in varied settings. Serious disease outbreaks and disasters can expose care staff to abnormally high levels of mortality and suffering. Health and social care systems need to proactively prepare for future events and enable peer support mechanisms that may help mitigate experiences of psychological distress in humanitarian crises.
Keywords: End-of-life care, Health care staff, Social care staff, Wellbeing, Humanitarian disaster, Pandemic, Mental health, COVID-19
1. Introduction
By March 2021, over 123 million cases of COVID-19 were recorded globally, with over 2,700,000 confirmed deaths. The outbreak exposed health and social care staff to chronic stress, uncertainty, and trauma (Greenberg et al., 2020). Many staff were redeployed to work in intensive and emergency care, increasing risk to themselves alongside limited preparation and rapidly changing protocols and polices (Dunn et al., 2020). Palliative and hospice care resources were in strained as the demand for end-of-life care increased, as did the demand for resources, including medicines, ventilators and end-of-life care trained staff (Arya et al., 2020; Kates et al., 2021).
Providing compassionate, person-centred, high-quality end-of-life care is a priority for healthcare staff. While health and social care staff will have had experience of end-of-life care and death, the intensity, frequency and the circumstances of COVID-19 deaths, often without families and with staff wearing full Personal Protective Equipment (PPE) was a likely source of distress and trauma (Pattison, 2020). Staff without specialist training or experience in emergency departments, intensive care or palliative and end-of-life care may have been more vulnerable to the traumatic exposure. During COVID-19 staff were repeatedly exposed to challenging circumstances in delivering end-of-life care including the practicalities of rapidly upskilling non-specialists, discussing end-of-life care with relatives remotely, limiting the number of visitors and patients dying alone (Tavabie and Ball, 2020). Many healthcare services across the world were faced with unprecedented resource and staffing shortages, limited access to essential testing and surveillance monitoring of outbreaks, distressing decisions, and adaptions to end-of-life care processes in the face of COVID-19 (Bertè, 2020; Kates et al., 2021). Staff working directly with COVID-19 patients and involved in diagnosis, treatment and care were at greater risk of symptoms of depression, anxiety, insomnia and distress (Lai et al., 2020). Many staff also experienced symptoms of burnout (Gemine et al., 2021; Tan et al., 2020) and have reported devastating impact of COVID-19 and social distancing on staff, patients and their families (Kates et al., 2021).
All healthcare settings have been impacted by COVID-19, but care homes, residential homes and nursing homes have seen the greatest increase in number of deaths and an estimated 40% of deaths have occurred in care homes internationally (Comas-Herrera et al., 2020). Staff who work in care homes have had a greater than usual exposure to death and dying and experienced an increased level of responsibility around end-of-life care, undertaking work that would usually be carried out by trained specialists (Martinsson et al., 2021). The work has been emotionally demanding and emerging evidence from COVID-19 suggests that care home staff have not had access to adequate support or training (Spacey et al., 2021).
Across settings, increased pressure has also enveloped managers and leaders, as they faced pandemic pressures, uncertainty, rapidly changing policies and staff occupational fatigue and burnout (Whelehan et al., 2021). Effective leadership is central to supporting staff morale, managing workforce challenges, high stress and uncertain circumstances (Harrington, 2021). During COVID-19, given the emotional demands that faced staff, applying compassionate leadership styles may have helped support staff mental wellbeing (Vogel and Flint, 2021; West and Chowla, 2017). More broadly, organisational culture was also forced to shift to be rapidly adaptable to change and collaboratively learning from other industries and humanitarian crises literature and expertise (Whelehan et al., 2021). Management and leadership approaches and organisational culture are important to the success and cohesion of health and social care teams, particularly during periods of increased pressure.
Literature exists that describes the experience of healthcare staff working in disease outbreaks and humanitarian disasters where they were exposed to high numbers of deaths. Research from the SARS outbreak (2003) found that healthcare staff were at risk of burnout, psychological distress and post-traumatic stress disorder (Maunder et al., 2006). Staff also reported how infectious disease control procedures (e.g., PPE, isolation) disrupted connectedness to patients and their families, alongside uncertainty in prognosis and preparing patients and families for end-of-life care (Leong et al., 2004). In previous Ebola outbreaks there have been significant healthcare staff infections and Ebola deaths disproportionately impacted staff (Evans et al., 2015; McDiarmid and Crestani, 2019; World Health Organisation (WHO), 2015). Staff in Ebola outbreaks have also reported stigmatisation, isolation, fear, stress and trauma from experiencing colleagues die (Hewlett and Hewlett, 2005; Raven et al., 2018). Moreover, relief workers deployed to humanitarian crises (including healthcare staff) are exposed to personal trauma and experience secondary trauma through witnessing the trauma of communities or colleagues, with Post Traumatic Stress Disorder (PTSD) estimates of 8%–43% (Connorton et al., 2012).
Previous pandemic literature and emerging COVID-19 evidence indicates the potential and substantial mental health and wellbeing impact of the pandemic on health and social care staff. The specific challenges, sensitive and emotive nature of end-of-life care during these circumstances may additionally compound or increase the impact on staff. Synthesising previous and emerging studies could enhance our understanding of how providing end-of-life care may impact the mental health and wellbeing of staff, across health and social care settings. Additionally, it could improve understanding of the effectiveness of organisational and individual strategies to ameliorate those impacts on staff, managers and leaders and across organisations, in high pressure, under-resourced, and uncertain periods such as pandemic disease outbreaks or humanitarian disasters.
This review aimed to understand the impact of providing end-of-life care during a disease outbreak or humanitarian disaster on the mental health and wellbeing of health and social care staff, and to identify recommendations from staff for support, including practical and psychological supports.
2. Methods
The method followed six stages: defining the research question (as described in the study aims) and inclusion criteria, study selection, quality appraisal, extraction and presentation of data, analysis of the data and presentation of the synthesis (Lachal et al., 2017). The published protocol is available on PROSPERO (Registration ID: CRD42020181444). The review is reported following PRISMA guidelines (Moher et al., 2009).
2.1. Search strategy and inclusion criteria
MEDLINE (Ovid), Embase, PsychInfo and, Web of Science were searched for studies related to Ebola, COVID-19, SARs, MERs or humanitarian disasters, end-of-life care, health and social care staff, and mental health and wellbeing. In this review, we define end-of-life care using the National Institutes of Health definition:
“Care given to people who are near the end of life and have stopped treatment to cure or control their disease. End-of-life care includes physical, emotional, social, and spiritual support for patients and their families. The goal of end-of-life care is to control pain and other symptoms so the patient can be as comfortable as possible. End-of-life care may include palliative care, supportive care, and hospice care.” (National Cancer Institute and National Institutes of Health, 2021).
The search strategy is provided in Supplemental File. We completed grey literature searches in the Cochrane COVID-19 Study Register, PaLCHASE (Palliative Care in Humanitarian Aid Situations and Emergencies Network), Social Care Online and Lit-COVID. Forward and backward citation searching was completed on all included studies using Scopus (Relevo and Balshem, 2011).
We included studies of health and social care staff, disease outbreaks or humanitarian disasters, and end-of-life care using any study design (systematic reviews, RCT, Clinically Controlled Trial, feasibility, pilot, observational studies and, qualitative studies). Editorials, general discussion papers, commentaries, letters, book chapters, single case studies and case series, and non-English language studies were excluded. Search dates were restricted to January 2001–July 2020 to include recent outbreaks (e.g., 2003 SARS, 2012 MERS, and 2014–2016 Ebola outbreak) and disasters (including the September 11th, 2001, terrorist attack). Two reviewer's dual-screened all identified titles and abstracts; BP screened all full-text papers, second reviewers screened 30% of full-texts and all excluded full-text articles. Conflicts were resolved by KS.
2.2. Quality assessment
The Johanna Briggs Institute Critical Appraisal Tool for Qualitative Studies (Lockwood et al., 2015) was used to appraise the qualitative studies. The AACODS checklist (authority, accuracy, coverage, objectivity, date, significance) was used to appraise grey literature (Tyndall, 2010). The good practice in the conduct and reporting of survey research guidelines were used to appraise survey studies (Kelley et al., 2003). The Johanna Briggs Institute Critical Appraisal Tool for Systematic Reviews was used to appraise reviews (The Johanna Briggs Institute, 2017). The quality of included studies is presented to provide a view of the integrity of the included studies. Based on the quality appraisal, no study was excluded.
2.3. Data analysis
We used qualitative meta-synthesis methods to analyse and synthesise the studies identified in this systematic review (Lachal et al., 2017). The analysis involved careful reading of the included papers by the reviewers. BP extracted the study characteristics and data related to the three a priori aims into a predetermined data extraction form: outbreak or disaster context, workforce, setting, experience of providing end-of-life care, impact (using validated measures or qualitatively described) on staff mental health and wellbeing, and staff-identified supports onto a proforma. AZ checked the data extraction for accuracy and completeness. Thematic analysis was used to inductively develop themes from the extracted data related to the review's aims from each paper (Thomas and Harden, 2008). Emerging themes were compared across papers and reviewed and re-reviewed by the research team. The developed themes were inductively translated into a framework of two superordinate themes. Finally, the synthesis was expressed as an interpretation of the superordinate themes and sub-themes into a model.
3. Results
3.1. Study characteristics
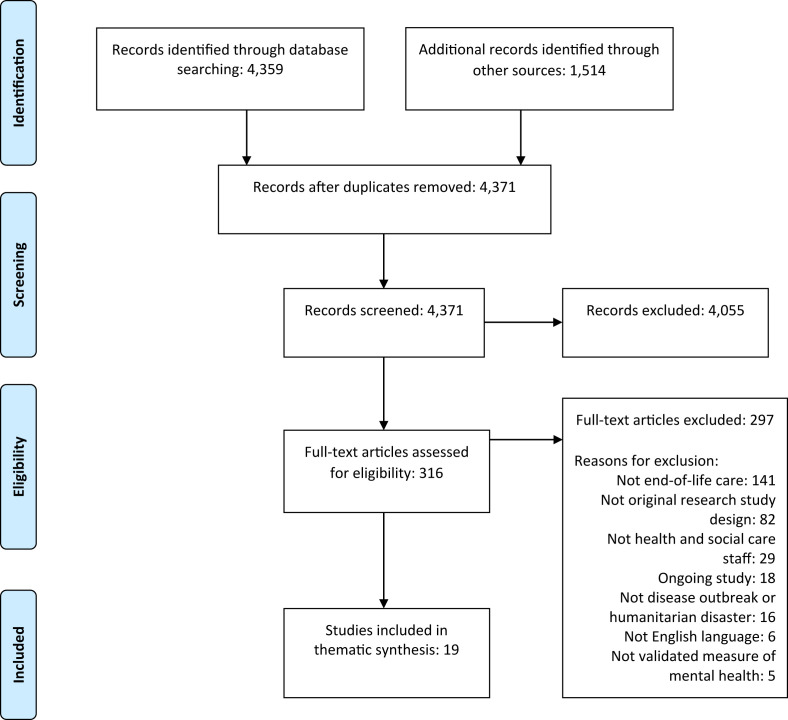
We screened 4892 titles and abstracts, assessed 316 full texts for eligibility and included 19 studies (Fig. 1, Fig. 2 ). Of the 19 included studies, 10 were studies of the Ebola outbreak (Andertun et al., 2017; Gershon et al., 2016; Hewlett and Hewlett, 2005; Langston et al., 2016; Locsin et al., 2009; Locsin and Matua, 2002; McCormack and Bamforth, 2019; Nouvet et al., 2018; Raven et al., 2018; Rubin et al., 2016), two were COVID-19 studies (Costantini et al., 2020; Gilissen et al., 2020), one was a SARs study (Leong et al., 2004), three were humanitarian disaster studies (Hunt, 2008; Matzo et al., 2009; Schneider et al., 2018), and three were studies of multiple disease outbreaks (Englert et al., 2019; Etkind et al., 2020; Jaakkimainen et al., 2014) including a rapid review of palliative care during pandemics (Etkind et al., 2020) (Table 1 ).
Fig. 1.
Flow of reports and studies into the synthesis.
Fig. 2.
Individual experiences and organisational responsibilities in terms of barriers and enablers to providing end-of-life care in circumstances of uncertainty.
Table 1.
End-of-Life Care during disease outbreaks or humanitarian disasters Systematic Review study characteristics (k = 19).
| Author (date) | Disease outbreak/humanitarian disaster | Country of outbreak/disaster | Study Design | Staff population | Setting |
|---|---|---|---|---|---|
| Andertun et al. (2018) | Ebola (2014–2015) | Sierra Leone | Qualitative narrative and focus group interviews (k=9) | Norwegian nurses and physician deployed to Sierra Leone | Ebola Treatment Centre |
| Costantini et al. (2020)a | Covid-19 | Italy | Cross-sectional telephone survey (k=16 hospices) | Hospice staff | Hospice |
| Englert et al. (2019) | Ebola, Marburg (multiple outbreaks from 2001 to 2017 | Uganda | Qualitative interview (k=41) | Healthcare workers | Hospital |
| Etkind et al. (2020)a | Covid-19, Ebola, SARs, Influenza - studies from year 2004–2020 | Studies included West Africa, Taiwan, Italy, U.S, Hong Kong and Singapore | Rapid Review and narrative synthesis (k=10 studies) | Hospice and palliative care staff | Hospice and palliative care settings |
| Gershon et al. (2016) | Ebola | West Africa | Qualitative interviews (k=16) | Healthcare volunteers from U.S. | Ebola Treatment Unit |
| Gillissen et al. (2020) | Covid-19 | International | Directed documentary and content analysis (k=21) | Nursing home staff | Nursing home |
| Hewlett and Hewlett (2005) | Ebola (1995, 2000–2001, 2003) | Democratic Republic of Congo (1995), Uganda (2000–2001) and Republic of Congo (2003) | Qualitative interviews and focus groups (k=10) | Nurses and healthcare workers | Not reported |
| Hunt (2008) | Humanitarian aid work in post-conflict zones | Africa, Asia, Central America and Eastern Europe | Qualitative interviews (k=10) | Nurses, physical therapist, physician and social workers | Various settings |
| Jaakkimainen et al. (2014) | SARS (2003), H1N1 (2009) | Canada | Quantitative survey (k=183) | GPs and Family Physicians | Community |
| Langston et al. (2016) | Ebola | Liberia | Mixed methods, qualitative and quantitative survey | Healthcare workers | Hospital |
| Leong et al. (2004) | SARs | Singapore | Qualitative interviews (k=8) | Palliative care workers | Hospitals |
| Locsin et al. (2002) | Ebola (2001) | Uganda | Qualitative written (k=7) narratives | Nurses | Hospital |
| Locsin et al. (2009) | Ebola (2001) | Uganda | Qualitative written narratives (k=15) | Nurses | Hospital |
| Matzo et al. (2009) | Mass casualty events | Not applicable | Qualitative interviews as part of a wider guideline development process | Palliative care experts | Various |
| McCormack et al. (2019) | Ebola (2014) | Sierra Leone | Qualitative interviews (k=5) | Red Cross Healthcare delegates – nurses and body handlers | Not reported |
| Nouvet et al. (2018) | Ebola (2014–2016) | New Guinea | Qualitative interviews (k=10) | Nurse, physicians | Ebola Treatment Centres |
| Raven et al. (2018) | Ebola (2004) | Sierra Leone | Qualitative interviews (k=25) | National and international healthcare workers | Ebola Treatment Centres, district and community hospitals |
| Rubin et al. (2016) | Ebola (2014–2015) | West Africa | Qualitative interviews (k=51) | UK Medical and laboratory staff | Not reported |
| Schneider et al. (2018) | Humanitarian emergency assistance | Cameroon, Central African Republic, Democratic Republic of the Congo, Iraq, Lebanon, Myanmar, Niger, South Sudan, Tanzania |
Qualitative interviews (k=15) | Expatriate humanitarian health workers - returning from clinical assignment with Médecins sans Frontières (MSF). | District hospital, HIV clinic, mobile clinics, primary health care, referral hospital, refugee camp |
Langston et al. (2016) and Matzo et al. (2009) did not report the number of participants included in their studies.
Etkind et al. (2020) is also a review and includes the study by Costantini et al. (2020).
3.2. Quality appraisal
Generally, the risk of bias for the qualitative studies was low, however, studies rarely reported their philosophical perspective, located the researcher culturally or theoretically and the influence of the researcher was not addressed. In the included grey literature, reporting of coverage, objectivity, and accuracy of the study was missing in Langston and colleagues’ abstract (Langston et al., 2016). There was a risk of bias associated with Etkind and colleagues (Etkind et al., 2020) review as they did not include quality appraisal or assess the likelihood of publication bias of the included studies (Table 2 ).
Table 2.
Quality appraisal of included studies.
| The Johanna Briggs Institute Critical Appraisal Tool for Systematic Reviews (The Johanna Briggs Institute, 2017). | |||||||||||
| Author (date) | Clear review question | Inclusion criteria | Search strategy | Adequate sources searched | Criteria for appraising studies | Critical appraisal | Data extraction | Appropriate methods to combine studies | Publication bias assessed | Policy and practice | New research |
|
Etkind et al. (2020) |
✓ |
✓ |
✓ |
✓ |
Χ |
Χ |
✓ |
✓ |
Χ |
✓ |
✓ |
| The Johanna Briggs Institute Critical Appraisal Tool for Qualitative Studies (Lockwood et al., 2015) | |||||||||||
|
Author (date) |
Philosophical perspective |
Research question and objective |
Data collection |
Data analysis |
Interpretation |
Locating the researcher |
Influence of/on researcher |
Participant voice |
Ethics |
Conclusions |
|
| Gillissen et al. (2020) | ✓ | ✓ | ✓ | ✓ | ✓ | Χ | Χ | ✓ | ✓ | ✓ | |
| Constantini et al. (2020) | – | ✓ | ✓ | – | ✓ | – | – | – | – | ✓ | |
| Rubin et al. (2016) | Χ | – | ✓ | – | ✓ | Χ | Χ | ✓ | ✓ | ✓ | |
| Leong et al. (2016) | Χ | – | ✓ | ✓ | ✓ | Χ | Χ | ✓ | ✓ | ✓ | |
| McCormack et al. (2019) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Englert et al. (2019) | ✓ | ✓ | ✓ | ✓ | Χ | Χ | ✓ | ✓ | ✓ | ✓ | |
| Gershon et al. (2016) | Χ | Χ | ✓ | – | ✓ | Χ | Χ | ✓ | ✓ | ✓ | |
| Matzo et al. (2009) | Χ | ✓ | ✓ | – | Χ | Χ | Χ | Χ | Χ | ✓ | |
| Raven et al. (2018) | Χ | ✓ | – | – | ✓ | Χ | Χ | ✓ | ✓ | ✓ | |
| Schneider et al. (2018) | Χ | – | ✓ | ✓ | ✓ | Χ | Χ | ✓ | ✓ | ✓ | |
| Locsin et al. (2009) | ✓ | ✓ | Χ | ✓ | ✓ | Χ | Χ | ✓ | Χ | ✓ | |
| Locsin et al. (2002) | ✓ | ✓ | ✓ | ✓ | ✓ | Χ | Χ | ✓ | ✓ | ✓ | |
| Hunt (2008) | ✓ | ✓ | ✓ | ✓ | ✓ | – | – | ✓ | ✓ | ✓ | |
| Hewlett and Hewlett (2005) | ✓ | ✓ | ✓ | ✓ | ✓ | – | – | ✓ | – | ✓ | |
|
Andertun et al. (2017) |
✓ |
✓ |
✓ |
✓ |
✓ |
– |
– |
✓ |
– |
✓ |
|
| The AACODS checklist (authority, accuracy, coverage, objectivity, date, significance) (Tyndall, 2010). | |||||||||||
|
Author (date) |
Authority |
Accuracy |
Coverage |
Objectivity |
Date |
Significance |
|||||
| Langston et al. (2018) | ✓ | Χ | Χ | Χ | ✓ | ✓ | |||||
|
Nouvet et al. (2018) |
✓ |
✓ |
✓ |
– |
✓ |
✓ |
|||||
| The good practice in the conduct and reporting of survey research guidelines (Kelley et al., 2003). | |||||||||||
|
Author (date) |
Purpose and aim |
Background and context |
Methods |
Sampling |
Data analysis |
Results |
Interpretation |
Conclusions |
|||
| Jaakimaainen et al. (2014) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
Quality appraisal of included studies, using study design relevant tools.
✓ = meets the criteria (yes), Χ = does not meet the criteria (no), - = unclear.
3.3. Thematic synthesis
Two superordinate themes were generated from the thematic analysis: individual experience and organisational responsibilities. Individual experience comprised four sub-themes: dignity in death, positive experiences, negative experiences and support for staff. Organisational responsibilities comprised of four sub-themes: adaption, preparation, resources, and PPE (Table 3 and quotes from themes in Supplemental File).
Table 3.
Superordinate themes and themes identified in each study.
| Subordinate themes |
Organisational responsibilities |
Individual experience |
||||||
|---|---|---|---|---|---|---|---|---|
| Higher order themes |
Adaption |
Preparation |
Resources |
PPE |
Dignity in death |
Positive experiences |
Negative experiences |
Support for staff |
| Author(s) date | ||||||||
| Andertun et al. (2017) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Costantini et al. (2020) | ✓ | ✓ | ✓ | |||||
| Englert et al. (2019) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Etkind et al. (2020) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Gershon et al. (2016) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Hewlett and Hewlett (2005) | ✓ | ✓ | ✓ | |||||
| Hunt (2008) | ✓ | ✓ | ||||||
| Jaakkimainen et al. (2014) | ✓ | ✓ | ||||||
| Langston et al. (2016) | ✓ | |||||||
| Leong et al. (2004) | ✓ | ✓ | ||||||
| Locsin et al. (2002) | ✓ | ✓ | ||||||
| Locsin et al. (2009) | ✓ | ✓ | ✓ | ✓ | ||||
| Matzo et al. (2009) | ✓ | ✓ | ✓ | |||||
| McCormack et al. (2019) | ✓ | ✓ | ✓ | |||||
| Nouvet et al. (2018) | ✓ | |||||||
| Raven et al. (2018) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Rubin et al. (2016) | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Schneider et al. (2018) | ✓ | ✓ | ✓ | |||||
| Gilissen et al. (2020) | ✓ | ✓ | ||||||
3.1.1. Individual experience
Individual experience consisted of four sub-themes that reflected the experience of healthcare staff providing end-of-life care during a pandemic or humanitarian disaster, the staff perception of the patient experience in these circumstances, and mechanisms to enable and support staff.
No studies quantitatively measured staff mental health and wellbeing, but there were qualitative descriptions of the negative and positive impact that providing end-of-life care had on staff.
3.1.1.1. Dignity in death
Staff were exposed to high levels of mortality and described patients experiencing undignified deaths and dying alone or with staff in full PPE (Andertun et al., 2017; Costantini et al., 2020; Gershon et al., 2016; Locsin and Matua, 2002; Rubin et al., 2016). Staff reported scrambling for time to share with dying persons to try and ensure they were not alone in their last moments (McCormack and Bamforth, 2019; Gershon et al., 2016), as described:
“It's one thing to die alone, and then it's another thing to die in an environment where it's hot and dark, and there's plastic tarps and chlorine smell, and you're on a cot as people come in wearing these big suits and leaving. And to die that way after suffering for days by yourself … I remember that very vividly.” (US Health Care Worker, voluntary deployment in West Africa Ebola outbreak, Gershon et al., 2016)
During Ebola outbreaks, staff reported the constant reminder and exposure to death and suffering (Andertun et al., 2017). In a COVID-19 staff survey, staff reported difficulty of maintaining the humanity of palliative care and that, in some circumstances, COVID-19 patients were dying in ICU without palliative care (Costantini et al., 2020). Healthcare staff were likely to be the last person to speak with the patient before they died, therefore delivering compassionate care and being there for them was very important to the staff (Locsin et al., 2009; McCormack and Bamforth, 2019). In the SARs outbreak staff described a sense of powerlessness, hopelessness, and frustration when faced with dying patients and families who were not able to pay their last respects (Leong et al., 2004). During disease outbreaks, usual end-of-life care processes were disturbed (Andertun et al., 2017; Gershon et al., 2016) and usual cultural practices related to health and the role of the community and family in dying matters were also affected (Hunt, 2008). An understanding of local beliefs around bereavement processes was considered essential to developing care that resonated with local communities (Hewlett and Hewlett, 2005; Nouvet et al., 2018).
3.1.1.2. Negative experiences
Fear was a predominant emotional response reported when working in the Ebola and COVID-19 outbreak (Andertun et al., 2017; Costantini et al., 2020; Hewlett and Hewlett, 2005; Locsin and Matua, 2002; McCormack and Bamforth, 2019). Fear was associated with the psychological threat of infection of themselves or the potential of infecting others at home or in their communities (McCormack and Bamforth, 2019). There was also a reported sense of fear of relatives or colleagues dying of Ebola virus disease (Locsin and Matua, 2002). Staff in the Ebola outbreaks experienced stigmatisation from their relatives and communities (Englert et al., 2019; Hewlett and Hewlett, 2005), as described:
“I had this whole questioning of myself and my role in humanitarian response … and then just the stigmatization following all of it … You know I kind of came to the fact that all of this is dirty, and humanitarian response is going to have some of its dirtiness. Nothing is as altruistic, clean and fair as you think it is. Everything is complicated and not everybody is in it for the purpose of helping each other out.” (Healthcare volunteer, West Africa, 2014–2015 Ebola outbreak, Gershon et al., 2016)
3.1.1.3. Positive experiences (motivations)
Healthcare staff were dedicated to their patients (Locsin et al., 2009, Hewlett and Hewlett, 2005; McCormack and Bamforth, 2019). Staff described positive motivation to help and a sense of satisfaction in their work (Rubin et al., 2016). Several positive experiences resulting from working during the Ebola outbreak were reported, including motivation, job satisfaction, camaraderie, pride, privilege, respect and admiration (Andertun et al., 2017; Englert et al., 2019; Langston et al., 2016; McCormack and Bamforth, 2019; Rubin et al., 2016). This is exemplified by one health worker after working in an Ebola outbreak:
“I think, professionally it would be the highlight of my working career, I do not think I would ever do anything as—as difficult, yet rewarding… it was unlike any other environment… it tested your—your skills, your resilience … your adaptability… the impact of what you were doing was quite apparent, and… it does feel like I did something good.” (International Red Cross/Red Crescent health worker, 2014 Ebola Outbreak, McCormack & Bamforth, 2019).
3.1.1.4. Support for staff
Team and peer support were important and support from managers or leaders helped staff feel more confident (Raven et al., 2018). Staff used social media groups, religious practice and contact with family as key supports (Rubin et al., 2016). Being able to communicate with their relatives helped to ease their own and others’ fears (Andertun et al., 2017; Rubin et al., 2016). Support to help staff transition back into their usual working roles after a period of deployment was identified as important (Gershon et al., 2016). As described:
“Sometimes all you need is a phone-call home to make you feel better” (UK Public Health or Non-Governmental Organisation Staff member deployed in West Africa, 2014 Ebola outbreak, Rubin et al., 2016).
3.1.2. Organisational responsibilities
Four themes comprised the superordinate theme of organisational responsibilities to enable staff to provide end-of-life care and support their mental health and wellbeing during a pandemic disease outbreak or humanitarian disaster.
3.1.2.1. Preparation
Preparatory training for staff and community health education were crucial. Training enabled healthcare staff to understand pandemic disease care, triage and PPE protocols, and overcome fear (Raven et al., 2018; Rubin et al., 2016). During outbreaks, training was desired for education on viruses, containment procedures and techniques (Englert et al., 2019; Hewlett and Hewlett, 2005). Cultural competency training was important prior to deployment (for international staff) (Gershon et al., 2016; Schneider et al., 2018). In humanitarian emergency assistance, key training was requested about the means and indications for palliative care in these contexts, including pain control guidelines (Schneider et al., 2018).
“I would have liked to know the indications for palliative care in this context, to have an idea about the availability of means and possibilities, also at the referral centre. Which indications in the context where I am sent to, are clearly palliative?” (Expatriate humanitarian health worker, Paediatrician in Niger, Schneider et al., 2018).
Many national staff working in the Ebola outbreak were less experienced in using pain relief (Nouvet et al., 2018; Schneider et al., 2018). In healthcare settings the inclusion of skills training for non-specialist staff in communication, bereavement and psychological support were identified as important in national and local pandemic planning where many casualties are anticipated (Etkind et al., 2020; Matzo et al., 2009).
In addition to education for staff, health education for local communities about viruses and disease containment strategies was helpful and supported staff in managing their roles and community cohesion (Englert et al., 2019; Matzo et al., 2009). Community health education about the virus helped to build trust in healthcare staff and the disease containment procedures (Englert et al., 2019).
3.1.2.2. Adaption
Adapting and adhering to policies, protocols and guidelines and flexibility among health systems to adapt and redeploy resources to where there is greatest demand, was important in disease outbreaks and disaster planning (Costantini et al., 2020; Etkind et al., 2020; Locsin et al., 2009; Matzo et al., 2009). At the start of COVID-19 outbreak in March 2020, guidance for end-of-life care was missing, causing distressing circumstances:
“Guidance on care for people dying from COVID-19 is missing”, while one physician noted “People with this infection are dying in ICU very badly, without any kind of palliative care support”. (Physician in Hospice Care Setting, Italy, COVID-19. Constantini et al., 2020).
To meet the demands of the Ebola and COVID-19 outbreaks, continuous reflection and conscientious practice of PPE use, working as a team and guideline adherence was required (Etkind et al., 2020; Locsin et al., 2009). During COVID-19 and SARs outbreaks, visitor policies, procedures for care and visitation after death policies were adjusted (Costantini et al., 2020; Etkind et al., 2020; Leong et al., 2004), and hospices banned or limited visitor numbers (Costantini et al., 2020). During COVID-19, some hospices also provided daily telephone support for families (Etkind et al., 2020). One study reviewed palliative care guidelines in nursing homes considering COVID-19 and identified that although they had been adapted, many lacked essential aspects of palliative care (Gilissen et al., 2020).
3.1.2.3. Resources
Limited equipment, supplies and resources affected the ability to provide end-of-life care (Gershon et al., 2016; Jaakkimainen et al., 2014; Schneider et al., 2018). Staff witnessed patient suffering due to drug (pain medication) and resource shortages (Gershon et al., 2016). International staff working in humanitarian emergency assistance described frustration at knowing how to reduce patient pain and suffering but not having the resources available to do so (Schneider et al., 2018). At the start of the Ebola outbreak, staff reported a lack of necessary equipment, supplies, laboratories, and PPE, and poor infection control practices (Raven et al., 2018).
“You need to have the necessary equipment to fight. What has been the problem is that even when there is this readiness of facing this battle, we have not been given the proper equipment to fight. (Health Worker, Sierra Leone, Ebola Outbreak, 2013–2015, Raven et al., 2018).
Access to medical supplies, medications, equipment, laboratories, space and, supplies of trusted PPE was identified as essential for management of events where there were expected to be many casualties (e.g., terrorist attacks, pandemic disease outbreaks) (Andertun et al., 2017; Englert et al., 2019; Etkind et al., 2020; Gershon et al., 2016; Hewlett and Hewlett, 2005; Matzo et al., 2009; Raven et al., 2018; Rubin et al., 2016).
3.1.2.4. PPE
As well as being identified as an essential resource, PPE enabled staff to create meaningful connection with patients who were dying. PPE provided a necessary protective barrier that enabled staff to provide care to patients and wearing PPE, alongside strict disease containment protocols, helped staff feel safe and protected (Andertun et al., 2017; Leong et al., 2004). However, PPE created distance between the staff and dying patients, making staff unrecognisable, and restricted the means of communication; eye contact and gestures became central to communication (Andertun et al., 2017; Leong et al., 2004). As described by one healthcare worker, PPE was a necessary protective barrier:
“Maybe the suit gave you limitations but maybe it protected you and your heart and your head a little bit from all of that suffering.” (International Red Cross/Red Crescent health worker, 2014 Ebola outbreak, McKormack et al., 2019).
3.1.3. Model of the impact of providing end-of-life care during a pandemic disease outbreak or humanitarian disaster
The two superordinate themes of individual experience and organisational responsibilities and their comprising themes formed a model presented in Fig. 2. The model encompasses individual experience and organisational responsibilities in terms of barriers and enablers to providing end-of-life care in challenging circumstances of uncertainty, such as those of a pandemic disease outbreak.
The staff experience of fear, stigma and isolation were barriers to providing end-of-life care and were associated with high levels of uncertainty around the disease, with negative impacts on staff (Andertun et al., 2017; Costantini et al., 2020; Englert et al., 2019; Hewlett and Hewlett, 2005; Locsin, 2002; McCormack and Bamforth, 2019). There were several organisational responsibilities that enabled staff and reduced the sense of uncertainty, including access to resources such as pain relief, PPE, and other essential equipment, adapting by changing policies, protocols and guidelines, and providing preparatory training and health education (Englert et al., 2019; Hewlett and Hewlett, 2005; Gershon et al., 2016; Schneider et al., 2018). Despite the high levels of uncertainty around the events, staff were motivated, and they experienced support from their team, people in leadership roles, and communication with their relatives helped (Andertun et al., 2017; Raven et al., 2018; Rubin et al., 2016).
The model depicts the dual opposing consequences of PPE being a barrier in positively protecting staff whilst negatively creating a sense of distance from patients. PPE was both a barrier and enabler to creating meaningful connections between staff and their patients in disease outbreaks. In times of uncertainty PPE helped staff to feel safe. Whilst PPE was an essential physical barrier between the staff and patients, it also enabled them to provide care with a sense of security (Andertun et al., 2017; Leong et al., 2004).
4. Discussion
This review of 19 studies identified two superordinate themes that contributed to the understanding of the impact of providing end-of-life care during a pandemic or humanitarian disaster on the mental health and wellbeing of health and social care staff: individual experience and organisational responsibilities. During pandemics or humanitarian disasters, there were intense and individualised experiences of the event. These included the perception of the patient experience and the challenging circumstances in which staff strove to provide compassionate and dignified end-of-life care. Staff experienced fear and stigma and were exposed to high levels of mortality. Patients, their families, and staff were affected by severely disrupted end-of-life experiences and processes. Social support for staff from relatives and colleagues helped them feel supported and motivated.
Organisational responsibilities that enabled and supported staff in their roles included preparation and adaption of procedures, policies and resources, training, and health education. The review highlights adequate PPE as a crucial resource in reducing fear and enabling connection to the patient, supporting end-of-life processes, and provision of compassionate end-of-life care.
Access to and use of PPE was integral for the safety and wellbeing of healthcare staff providing end-of-life care and for the patient and family experience of care. As in previous outbreaks, there were critical shortages of PPE supplies for staff working at the forefront of the COVID-19 outbreak (Iqbal and Chaudhuri, 2020; Ranney et al., 2020; Royal College of Nursing, 2020; Zhang et al., 2020). PPE was a necessity for staff to reduce the sense of fear from infection and enabling compassionate end-of-life care for patients, although PPE did act as a barrier to usual demonstrations of compassion.
None of the studies eligible for inclusion quantitively measured mental health and wellbeing of health and social care staff providing end-of-life care. However, particularly during COVID-19, staff mental health was highlighted internationally. Several studies reported that staff experienced posttraumatic stress, psychological distress, sleep disturbances, symptoms of anxiety, depression, and burnout (Kisely et al., 2020; Pappa et al., 2020; Zhang et al., 2020). However, as in our review, staff in the COVID-19 pandemic also reported experiences of a shared sense of duty, motivation, team camaraderie, and the prospect of posttraumatic growth (Greenberg et al., 2020). Studies emerging from COVID-19 also identify staff motivation and determination to provide dignified deaths to patients, including communicating with patients using gestures or touch (when safe), using technology to connect patients with relatives, and striving to ensure no one died alone (Franchini et al., 2021; Mitchinson et al., 2021). The long-term repercussions of COVID-19 on staff mental health in the context of pressurised health systems is not yet known. Future studies need to understand both the barriers and enablers to mental health and wellbeing of all staff across healthcare contexts to prepare for future events, in addition to objectively measuring mental health and wellbeing impacts.
In the UK, around 30% of COVID-19 deaths have occurred in care homes (Office for National Statistics, 2020). However, we found limited evidence from hospice, residential care or nursing care homes in this review, with one study in a hospice setting (Costantini et al., 2020; Etkind et al., 2020) and two based in nursing homes (Etkind et al., 2020; Gilissen et al., 2020). The lack of evidence may occur due to the unprecedented nature of pandemic outbreaks affecting these settings. However, these populations are often living with physical and mental comorbidities and may be at greater risk of harm or mortality in instances of a disease outbreak or humanitarian disaster (Matzo et al., 2009). Health and social care systems have been severely affected by austerity measures, widening inequity in health and access to services (Marmot et al., 2020). Staff have been confronted with underfunded, under-resourced and understaffed working environments, and COVID-19 emphasised disparities in provision of health and social care. People living in care, nursing or residential homes were deeply affected by policies and decisions throughout COVID-19 regarding testing and hospital discharge. Both health and social care staff require and deserve equal opportunity for support, preparation, and training provided by their organisations. Future studies should seek to determine the experiences of social care staff and end-of-life care during COVID-19 and identify appropriate support and preparation mechanisms.
Our review findings are largely based on previous events or outbreaks in varied health systems. However, our findings clearly resonate with the experience of staff throughout the global COVID-19 outbreak, reporting that factors associated with higher levels of burnout in staff are modifiable, including training and PPE (Gemine et al., 2021; Tan et al., 2020). COVID-19 studies also suggest the impact of re-deployment on staff burnout (Denning et al., 2021; Gemine et al., 2021; Tan et al., 2020). Some healthcare staff included in studies in our review were voluntarily re-deployed and the challenges of providing usual approaches to care in different contexts and working in high-risk areas were identified. Many healthcare staff were redeployed during COVID-19, including into high-risk areas (Dunn et al., 2020; Ezzat et al., 2021). Healthcare systems across the world were pushed and strained; supporting staff during and after an outbreak was essential. Future practice planning should consider what has been learned from previous outbreaks and what can be learned from COVID-19 to ensure that support is appropriate, timely and accessible, for all.
The onus of maintaining staff mental health and wellbeing lies not with the individual, rather, a whole system approach is needed. Our review identified several individual and organisational areas of need to enable staff, to support their mental health and wellbeing and to facilitate delivery of quality end-of-life care for patients and their families. Many health care staff demonstrated commitment and tenacity in the face of COVID-19. New teams were brought together, staff were redeployed into different roles, facing new experiences and challenges. As we found in our review, COVID-19 highlighted the importance of peer and team support (Maben and Bridges, 2020). Schwartz Rounds have been used for some time in non-pandemic conditions in the UK and Ireland as a regular space for reflective practice into the emotional impact of their roles and for reflection on ethical challenges (Flanagan et al., 2020). In periods of crisis usual Schwartz Round approaches are not possible as staff need time for reflective practice between the event(s) and sharing their story (Rose et al., 2002). However, Schwartz Round approaches were adapted for COVID-19, with core features used in “Team Time”, virtual formats, with smaller and existing teams, with careful selection of stories by experienced facilitators (Groves, 2020). Adapted approaches to support staff require evaluation of effects, feasibility, acceptability and relevant context-specific factors.
In response to the increased numbers of healthcare staff involved in end-of-life care during COVID-19, useful resources have been developed to support staff with less experience in these caring roles and under uncertain circumstances of COVID-19. The Royal College of Nursing, for example, have created a module including essential information on end-of-life care and additional information on individual staff self-care and wellbeing support (Royal College of Nursing, 2021). This includes key priorities of end-of-life care, including recognising patients in end-of-life care phase, communicating with key people, involving the dying person and their relatives in end-of-life care, and support for the patient, their relatives, and for staff. Integrating staff wellbeing into information provision about end-of-life care processes helps to recognise the impact that this may have on staff, enabling them to seek support for themselves. Although, it is also important to ensure that staff feel supported within their teams and by their organisation.
In the context of high levels of burnout and stress in pandemic disease healthcare settings, effective leadership and a recognition of the human and relational role of managers are key (Gibiino et al., 2020). In line with our findings, previous literature suggests this ought to include developing a sense of belonging and value for staff, working collaboratively within teams, recognising progress and celebrating moments of success, using technology to facilitate communication (e.g., when staff isolated from their relatives to reduce risk of infection) (Gibiino et al., 2020). Moreover, a manager can embody the value of maintaining time for self-care and supporting their wellbeing, in doing so this is both supportive for the manager and can set a precedent for staff (Gibiino et al., 2020; Markey et al., 2021). These principles are important for managers during and in the recovery period of COVID-19.
Emergency preparedness policies should include minimum standards of support available for staff exposed to traumatic circumstances, including pandemic disease outbreaks, humanitarian disasters, and terrorist attacks. Research with humanitarian aid workers identified that perceived organisational support and supervision and support within a team may alleviate the experience of anxiety, depression, and distress (Aldamman et al., 2019; Lopes Cardozo et al., 2012). Previous studies suggested psychosocial training in the workplace to educate staff around mental health, to reduce stigma, and enabling staff to develop supportive peer networks (Brooks et al., 2019). Research should evaluate the effectiveness of approaches organisations take to support staff, such as through adapting policies and enabling peer support during COVID-19 to develop the evidence base to inform emergency preparedness interventions and policies for the future.
4.1. Limitations
There are notable limitations to our review. Firstly, due to the currency of the COVID-19 pandemic, the findings of our review were necessarily largely based on previous pandemics of disease outbreaks and events. The impact of COVID-19 is emerging and there will be further opportunities to understand the experience of, and impacts on, staff in this pandemic. Secondly, we did not specifically define mental health and wellbeing but included studies based on their use of validated mental health and wellbeing measures and there were no studies that quantitively measured the mental health or wellbeing impact on staff who were providing end-of-life care during a pandemic or humanitarian disaster. Further, we applied our personal interpretation of the qualitative studies referring to staff experiences, to deduct the experiences relevant to staff mental wellbeing. Future research is required to understand the impact on mental health outcomes, including post-traumatic stress and post-traumatic growth, and occupational outcomes such as staff retention and job satisfaction. Mental health, physical health, and wellbeing protective factors should also be identified so that these can be rapidly deployed in the event of a pandemic or humanitarian disaster. Thirdly, although a wide range of databases and grey literature sources were searched, we did not include non-English language studies and thus it is possible that some studies, including emerging COVID-19 studies, may have been missed.
4.2. Conclusion
When health systems are put under pressure, health and social care staff are at the forefront in responding to the challenge. In pandemic disease outbreaks or disasters, end-of-life care processes are disrupted for staff, patients and their families. When staff are supported, resourced and trained for these events, they feel prepared, motivated and enabled to continue to deliver quality, compassionate care. Individual, team and system-level supports are required in order to ensure staff feel supported and are prepared to enable compassion and dignity for patients, when end-of-life processes are disrupted.
Author contributions
Bryony Porter: Conceptualization, Methodology, Running Searches, Screening Papers, Quality Appraisal, Formal analysis, Writing – original draft, Writing – review & editing. Amy Zile: Screening Papers, Quality Appraisal, Writing – Reviewing and Editing. Guy Peryer: Conceptualization, Methodology, Screening Papers, Formal analysis, Writing – Reviewing and Editing. Morag Farquhar: Conceptualization, Methodology, Screening Papers, Formal analysis, Writing – Reviewing and Editing. Kristy Sanderson: Conceptualization, Formal analysis, Methodology, Screening Papers, Writing – Reviewing and Editing.
Declaration of competing interest
None.
Acknowledgements
This research has been made possible by a collaboration across the NIHR Applied Research Collaboration East of England Mental Health Over the Life Course theme (BP, KS), Palliative and End-of-Life Care theme (GP, MF), and Inclusive Involvement in Research for Practice Led Health and Social Care (GP). KS is Lead of Workforce Sustainability Research Group for University of East Anglia Health and Social Care Partners. This is a summary of research funded by the National Institute for Health Research (NIHR) Applied Research Collaboration East of England. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2021.114397.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Aldamman K., Tamrakar T., Dinesen C., Wiedemann N., Murphy J., Hansen M., Elsiddig Badr E., Reid T., Vallières F. Caring for the mental health of humanitarian volunteers in traumatic contexts: the importance of organisational support. Eur. J. Psychotraumatol. 2019;10:1694811. doi: 10.1080/20008198.2019.1694811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andertun S., Hörnsten Å., Hajdarevic S. Ebola virus disease: caring for patients in Sierra Leone – a qualitative study. J. Adv. Nurs. 2017;73:643–652. doi: 10.1111/jan.13167. [DOI] [PubMed] [Google Scholar]
- Arya A., Buchman S., Gagnon B., Downar J. Pandemic palliative care: beyond ventilators and saving lives. CMAJ (Can. Med. Assoc. J.) 2020;192:E400–E404. doi: 10.1503/cmaj.200465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertè R. 2020. COVID-19: the Role of Palliative Care Had to Be Adapted to Manage This “Ultra-emergency” - the BMJ.https://blogs.bmj.com/bmj/2020/03/31/COVID-19-the-role-of-palliative-care-had-to-be-adapted-to-manage-this-ultra-emergency/ [WWW Document]. BMJ Opin. [Google Scholar]
- Brooks S.K., Rubin G.J., Greenberg N. Traumatic stress within disaster-exposed occupations: overview of the literature and suggestions for the management of traumatic stress in the workplace. Br. Med. Bull. 2019;129:35–51. doi: 10.1093/bmb/ldy040. [DOI] [PubMed] [Google Scholar]
- Comas-Herrera A., Zalakaín J., Lemmon E., Henderson D., Litwin C., Hsu A.T., Schmidt A.E., Arling G., Kruse F., Fernández J.-L., Voor A. Article in LTCCOVID.Org, International Long-Term Care Policy Network. CPEC-LSE; 2020. Mortality associated with COVID-19 in care homes: international evidence. [Google Scholar]
- Connorton E., Perry M.J., Hemenway D., Miller M. Humanitarian relief workers and trauma-related mental illness. Epidemiol. Rev. 2012 doi: 10.1093/epirev/mxr026. [DOI] [PubMed] [Google Scholar]
- Costantini M., Sleeman K.E., Peruselli C., Higginson I.J. Response and role of palliative care during the COVID-19 pandemic: a national telephone survey of hospices in Italy. Palliat. Med. 2020 doi: 10.1177/0269216320920780. 026921632092078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denning M., Goh E.T., Almonte M., Scott A., Martin G., Clarke J., Sounderajah V., Markar S., Przybylowicz J., Beatty J.W., Flott K., Mason S., Chidambaram S., Yalamanchili S., Zbikowska G., Wells M., Purkayastha S., Kinross J., Kanneganti A., Sharma V., Tan B., Chan Y.H., Sia C.-H., Chua Y.X., Sim K., Lim L., Tan L., Tan M., Ooi S., Fedorowski J., Dykowska G. Determinants of burnout and other aspects of psychological well-being in healthcare workers during the COVID-19 pandemic: a multinational cross-sectional study. PloS One. 2021;16 doi: 10.1371/journal.pone.0238666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn M., Sheehan M., Hordern J., Turnham H.L., Wilkinson D. “Your country needs you”: the ethics of allocating staff to high-risk clinical roles in the management of patients with COVID-19. J. Med. Ethics. 2020;46:436–440. doi: 10.1136/medethics-2020-106284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Englert E.G., Kiwanuka R., Neubauer L.C. “When I die, let me be the last.” Community health worker perspectives on past Ebola and Marburg outbreaks in Uganda. Global Publ. Health. 2019;14:1182–1192. doi: 10.1080/17441692.2018.1552306. [DOI] [PubMed] [Google Scholar]
- Etkind S.N., Bone A.E., Lovell N., Cripps R.L., Harding R., Higginson I.J., Sleeman K.E. The role and response of palliative care and hospice services in epidemics and pandemics: a rapid review to inform practice during the COVID-19 pandemic. J. Pain Symptom Manag. 2020 doi: 10.1016/j.jpainsymman.2020.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans D.K., Goldstein M., Popova A. Health-care worker mortality and the legacy of the Ebola epidemic. Lancet Glob. Heal. 2015;3:e439–e440. doi: 10.1016/S2214-109X(15)00065-0. [DOI] [PubMed] [Google Scholar]
- Ezzat A., Li Y., Holt J., Komorowski M. The global mental health burden of COVID-19 on critical care staff. Br. J. Nurs. 2021;30:634–642. doi: 10.12968/bjon.2021.30.11.634. [DOI] [PubMed] [Google Scholar]
- Flanagan E., Chadwick R., Goodrich J., Ford C., Wickens R. Reflection for all healthcare staff: a national evaluation of Schwartz Rounds. J. Interprof. Care. 2020;34 doi: 10.1080/13561820.2019.1636008. [DOI] [PubMed] [Google Scholar]
- Franchini L., Varani S., Ostan R., Bocchi I., Pannuti R., Biasco G., Bruera E. Home palliative care professionals perception of challenges during the COVID-19 outbreak: a qualitative study. Palliat. Med. 2021;35:862–874. doi: 10.1177/02692163211008732. [DOI] [PubMed] [Google Scholar]
- Gemine R., Davies G.R., Tarrant S., Davies R.M., James M., Lewis K. Factors associated with work-related burnout in NHS staff during COVID-19: a cross-sectional mixed methods study. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-042591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gershon R., Dernehl L.A., Nwankwo E., Zhi Q., Qureshi K. Experiences and psychosocial impact of West Africa ebola deployment on US health care volunteers. PLoS Curr. 2016;8 doi: 10.1371/currents.outbreaks.c7afaae124e35d2da39ee7e07291b6b5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibiino G., Rugo M., Maffoni M., Giardini A., Clinici I., Maugeri S., Pavia I. Back to the future: five forgotten lessons for the healthcare managers of today. Int. J. Qual. Health Care. 2020;4:275–277. doi: 10.1093/intqhc/mzaa021. [DOI] [PubMed] [Google Scholar]
- Gilissen J., Pivodic L., Unroe K.T., Block L. Van den. International COVID-19 palliative care guidance for nursing homes leaves key themes unaddressed. J. Pain Symptom Manag. 2020 doi: 10.1016/j.jpainsymman.2020.04.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg N., Docherty M., Gnanapragasam S., Wessely S. Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. BMJ. 2020;368:m1211. doi: 10.1136/bmj.m1211. [DOI] [PubMed] [Google Scholar]
- Groves J. 2020. Team Time’ - Reflecting Together on the COVID Crisis. Point Care Found. [Google Scholar]
- Harrington A. Understanding effective nurse leadership styles during the COVID-19 pandemic. Nurs. Stand. 2021;36:45–50. doi: 10.7748/NS.2021.E11601. [DOI] [PubMed] [Google Scholar]
- Hewlett B.L., Hewlett B.S. Providing care and facing death: nursing during Ebola outbreaks in central Africa. J. Transcult. Nurs. Off. J. Transcult. Nurs. Soc. 2005;16:289–297. doi: 10.1177/1043659605278935. [DOI] [PubMed] [Google Scholar]
- Hunt M.R. Ethics beyond borders: how health professionals experience ethics in humanitarian assistance and development work. Develop. World Bioeth. 2008;8:59–69. doi: 10.1111/j.1471-8847.2006.00153.x. [DOI] [PubMed] [Google Scholar]
- Iqbal M.R., Chaudhuri A. COVID-19: results of a national survey of United Kingdom healthcare professionals' perceptions of current management strategy – a cross-sectional questionnaire study. Int. J. Surg. 2020;79:156–161. doi: 10.1016/j.ijsu.2020.05.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaakkimainen R., Bondy S., Parkovnick M., Barnsley J. How infectious disease outbreaks affect community-based primary care physicians: comparing the SARS and H1N1 epidemics. Can. Fam. Physician. 2014;60:917–925. [PMC free article] [PubMed] [Google Scholar]
- Kates J., Gerolamo A., Pogorzelska-Maziarz M. The impact of COVID-19 on the hospice and palliative care workforce. Publ. Health Nurs. 2021;38:459–463. doi: 10.1111/PHN.12827. [DOI] [PubMed] [Google Scholar]
- Kelley K., Clark B., Brown V., Sitzia J. Methodology Matters Good practice in the conduct and reporting of survey research. Int. J. Qual. Health Care. 2003;15:261–266. doi: 10.1093/intqhc/mzg031. [DOI] [PubMed] [Google Scholar]
- Kisely S., Warren N., McMahon L., Dalais C., Henry I., Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369:m1642. doi: 10.1136/bmj.m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachal J., Revah-Levy A., Orri M., Moro M.R. Metasynthesis: an original method to synthesize qualitative literature in psychiatry. Front. Psychiatr. 2017;8:269. doi: 10.3389/fpsyt.2017.00269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020 doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langston A., Senkungu J., Miller L., Jones T. Health care worker motivation one year after the ebola outbreak in Liberia. Am. J. Trop. Med. Hyg., 65th Annual Meeting of the American Society of Tropical Medicine and Hygiene, ASTMH. 2016;95:456. doi: 10.4269/ajtmh.abstract2016. [DOI] [Google Scholar]
- Leong I.Y.-O.O., Lee A.O.-K.K., Ng T.W., Lee L.B., Koh N.Y., Yap E., Guay S., Ng L.M. The challenge of providing holistic care in a viral epidemic: opportunities for palliative care. Palliat. Med. 2004;18:12–18. doi: 10.1191/0269216304pm859oa. [DOI] [PubMed] [Google Scholar]
- Lockwood C., Munn Z., Porritt K. Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. Int. J. Evididenced Based Healthc. 2015;13:179–187. doi: 10.1097/XEB.0000000000000062. [DOI] [PubMed] [Google Scholar]
- Locsin R.C. Ebola at Mbarara, Uganda: aesthetic expressions of the lived worlds of people waiting to know. Nurs. Sci. Q. 2002;15:123–130. doi: 10.1177/089431840201500209. [DOI] [PubMed] [Google Scholar]
- Locsin R.C., Kongsuwan W., Nambozi G. Ugandan nurses' experience of caring for persons dying from Ebola Hemorrhagic Fever. Int. J. Hum. Caring. 2009;13:26–32. [Google Scholar]
- Locsin R.C., Matua A.G. The lived experience of waiting-to-know: ebola at Mbarara, Uganda--hoping for life, anticipating death. J. Adv. Nurs. 2002;37:173–181. doi: 10.1046/j.1365-2648.2002.02069.x. [DOI] [PubMed] [Google Scholar]
- Lopes Cardozo B., Gotway Crawford C., Eriksson C., Zhu J., Sabin M., Ager A., Foy D., Snider L., Scholte W., Kaiser R., Olff M., Rijnen B., Simon W. Psychological distress, depression, anxiety, and burnout among international humanitarian aid workers: a longitudinal study. PloS One. 2012;7 doi: 10.1371/journal.pone.0044948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maben J., Bridges J. COVID-19: supporting nurses' psychological and mental health. J. Clin. Nurs. 2020 doi: 10.1111/jocn.15307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markey K., Ventura C.A.A., Donnell C.O., Doody O. Cultivating ethical leadership in the recovery of COVID-19. J. Nurs. Manag. 2021 doi: 10.1111/jonm.13191. [DOI] [PubMed] [Google Scholar]
- Marmot M., Allen J., Boyce T., Goldblatt P., Morrison J. 2020. Health Equity in England: the Marmot Review 10 Years on. (London) [DOI] [PubMed] [Google Scholar]
- Martinsson L., Strang P., Bergström J., Lundström S. Were clinical routines for good end-of-life care maintained in hospitals and nursing homes during the first three months of the outbreak of COVID-19? A national register study. J. Pain Symptom Manag. 2021;61:e11–e19. doi: 10.1016/J.JPAINSYMMAN.2020.09.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matzo M., Wilkinson A., Lynn J., Gatto M., Phillips S. Palliative care considerations in mass casualty events with scarce resources. Biosecurity and Bioterrorism. 2009;7:199–210. doi: 10.1089/bsp.2009.0017. [DOI] [PubMed] [Google Scholar]
- Maunder R.G., Lancee W.J., Balderson K.E., Bennett J.P., Borgundvaag B., Evans S., Fernandes C.M.B., Goldbloom D.S., Gupta M., Hunter J.J., Hall L.M.G., Nagle L.M., Pain C., Peczeniuk S.S., Raymond G., Read N., Rourke S.B., Steinberg R.J., Stewart T.E., VanDeVelde-Coke S., Veldhorst G.G., Wasylenki D.A. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg. Infect. Dis. 2006;12 doi: 10.3201/eid1212.060584. 1924–1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCormack L., Bamforth S. Finding authenticity in an altruistic identity: the “lived” experience of health care humanitarians deployed to the 2014 Ebola crisis. Traumatology. 2019;25:289–296. doi: 10.1037/trm0000171. [DOI] [Google Scholar]
- McDiarmid M., Crestani R. Duty of care and health worker protections in the age of Ebola: lessons from Médecins Sans Frontières. BMJ Glob. Heal. 2019;4 doi: 10.1136/BMJGH-2019-001593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchinson L., Dowrick A., Buck C., Hoernke K., Martin S., Vanderslott S., Robinson H., Rankl F., Manby L., Lewis-Jackson S., Vindrola-Padros C. Missing the human connection: a rapid appraisal of healthcare workers' perceptions and experiences of providing palliative care during the COVID-19 pandemic. Palliat. Med. 2021;35:852–861. doi: 10.1177/02692163211004228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6 doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Cancer Institute, National Institutes of Health . NCI Dictionaries; 2021. End-of-Life care. [Google Scholar]
- Nouvet E., Sivaram M., Bezanson K., Krishnaraj G., Hunt M., de Laat S., Sanger S., Banfield L., Rodriguez P.F.E., Schwartz L.J. Palliative care in humanitarian crises: a review of the literature. J. Int. Humanit. Action. 2018;3:1–14. doi: 10.1186/s41018-018-0033-8. [DOI] [Google Scholar]
- Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pattison N. End-of-life decisions and care in the midst of a global coronavirus (COVID-19) pandemic. Intensive Crit. Care Nurs. 2020 doi: 10.1016/j.iccn.2020.102862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranney M.L., Griffeth V., Jha A.K. Critical supply shortages - the need for ventilators and personal protective equipment during the COVID-19 pandemic. N. Engl. J. Med. 2020 doi: 10.1056/NEJMp2006141. [DOI] [PubMed] [Google Scholar]
- Raven J., Wurie H., Witter S. Health workers' experiences of coping with the Ebola epidemic in Sierra Leone's health system: a qualitative study. BMC Health Serv. Res. 2018;18:251. doi: 10.1186/s12913-018-3072-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Relevo R., Balshem H. Finding evidence for comparing medical interventions: AHRQ and the effective health care program. J. Clin. Epidemiol. 2011 doi: 10.1016/j.jclinepi.2010.11.022. [DOI] [PubMed] [Google Scholar]
- Rose S., Bisson J., Churchill R., Wessely S. Psychological debriefing for preventing post traumatic stress disorder (PTSD) Cochrane Database Syst. Rev. 2002 doi: 10.1002/14651858.CD000560. [DOI] [PubMed] [Google Scholar]
- Royal College of Nursing . 2021. (End of Life Care and Wellbeing for the Nursing and Midwifery Workforce). [Google Scholar]
- Royal College of Nursing . 2020. Second Personal Protective Equipment Survey of UK Nursing Staff Report : Use and Availability of PPE during the. [Google Scholar]
- Rubin G.J., Harper S., Williams P.D., Ostrom S., Bredbere S., Amlot R., Greenberg N. How to support staff deploying on overseas humanitarian work: a qualitative analysis of responder views about the 2014/15 West African Ebola outbreak. Eur. J. Psychotraumatol. 2016;7:30933. doi: 10.3402/ejpt.v7.30933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider M., Chappuis F., Pautex S. How do expatriate health workers cope with needs to provide palliative care in humanitarian emergency assistance? A qualitative study with in-depth interviews. Palliat. Med. 2018;32:1567–1574. doi: 10.1177/0269216318794091. [DOI] [PubMed] [Google Scholar]
- Spacey A., Porter S., Board M., Scammell J. 2021. Impact of the COVID-19 Pandemic on End of Life Care Delivery in Care Homes: A Mixed Method Systematic Review. 10.1177/02692163211029806. [DOI] [PubMed] [Google Scholar]
- Tan B.Y.Q., Kanneganti A., Lim L.J.H., Tan M., Chua Y.X., Tan L., Sia C.H., Denning M., Goh E.T., Purkayastha S., Kinross J., Sim K., Chan Y.H., Ooi S.B.S. Burnout and associated factors among health care workers in Singapore during the COVID-19 pandemic. J. Am. Med. Dir. Assoc. 2020;21:1751–1758. doi: 10.1016/j.jamda.2020.09.035. e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tavabie S., Ball K. BMJ Support. Palliat. Care Blog. 2020. Perspectives on dying from COVID-19: waiting for the storm – BMJ supportive & palliative care. [Google Scholar]
- The Johanna Briggs Institute . vol. 2. 2017. (Checklist for Systematic Reviews and Research Syntheses Critical Appraisal Checklist for Systematic Reviews and Research Syntheses). [Google Scholar]
- Tyndall J. Flinders Univ.; 2010. The AACODS Checklist. [Google Scholar]
- Vogel S., Flint B. Compassionate leadership: how to support your team when fixing the problem seems impossible. Nurs. Manag. 2021;28:32–41. doi: 10.7748/NM.2021.E1967. [DOI] [PubMed] [Google Scholar]
- West M.A., Chowla R. Compassionate leadership for compassionate health care. Compass. 2017:237–257. doi: 10.4324/9781315564296-14. [DOI] [Google Scholar]
- Whelehan D.F., Algeo N., Brown D.A. Leadership through crisis: fighting the fatigue pandemic in healthcare during COVID-19. BMJ Lead. 2021;5:108–112. doi: 10.1136/LEADER-2020-000419. [DOI] [Google Scholar]
- World Health Organization . 2015. Health Worker Ebola Infections in Guinea, Liberia and Sierra Leone: a Preliminary Report 21 May 2015. (WHO) [Google Scholar]
- Zhang Q., Cheng S., Cheng Q. Experience summary of a COVID-19 designated community hospital and its operation model. Panminerva Med. 2020 doi: 10.23736/S0031-0808.20.03908-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.