Key points.
-
•
Skin conditions that present to critical care are rare, but are associated with a high mortality.
-
•
Dermatological presentations requiring critical care often result from an underlying infection.
-
•
Patients who are systemically unwell or pyrexial with cutaneous involvement should be treated with a high index of suspicion for underlying infection.
-
•
Patients with non-infectious dermatoses may also present with fever and raised inflammatory markers, and require specialist care to improve outcome.
Learning objectives.
By reading this article, you should be able to:
-
•
Use the correct terminology when describing life-threatening dermatoses.
-
•
Assess a patient who is seriously unwell with a primary skin condition.
-
•
State which primary dermatoses may require critical care.
-
•
Summarise the management specific to these conditions.
Primary dermatological conditions that require critical care are rare, accounting for approximately 0.5% of critical care admissions per year. The most common dermatological conditions that require admission are those conditions associated with infections, such as necrotising fasciitis (NF) and cutaneous cellulitis, which lead to subsequent organ dysfunction.1 The mortality for patients admitted with a primary dermatological condition is high. However, patients with acute skin failure, such as Stevens–Johnson syndrome (SJS) or toxic epidermal necrolysis (TEN) in particular, have a critical care mortality rate of up to 35% and hospital mortality rate of up to 47%, comparable with other serious conditions, such as pneumonia (49%) and acute pancreatitis (42%). This subset of patients also tends to have longer durations of critical care and hospital stay than other adults admitted to intensive care.1
Given the high mortality of these patients, the intensivist should have a structured approach to the unwell patient presenting with a serious primary skin condition. This article will describe how to approach such a patient and review the primary skin conditions that may present to critical care.
How to approach the critically ill patient with cutaneous involvement
History
When approaching a critically ill patient with a dermatological condition, it is important to ascertain a comprehensive history (Table 1). Questions to consider include the following:
-
(i)
Where did the skin involvement start, has it spread and have there been any changes in morphology?
-
(ii)
Has the patient had any non-specific systemic flu-like symptoms, such as myalgia, arthralgia, abdominal pain, cough, sore throat, rhinorrhoea, headache or malaise? These symptoms may be present with a viral infection, but can also indicate severe cutaneous adverse reactions, such as TEN or SJS.
-
(iii)
Has the patient had other symptoms of intracranial involvement, such as headache or photophobia? This may raise your suspicion that the rash is caused by meningococcal infection, particularly if it appears purpuric on examination.
-
(iv)
Do they have involvement of mucosal surfaces, including the lips, oral cavity, conjunctiva, nasal mucosa, genitourinary tract (painful micturition), gastrointestinal tract (dysphagia or diarrhoea) or respiratory tract (cough, wheeze and shortness of breath)? This may indicate a severe cutaneous adverse reaction, such as TEN or SJS.
-
(v)
Have any new medications been introduced within the past 2 months? This may indicate that the rash is an adverse drug reaction.
-
(vi)
Has the patient had any wounds, bites or recent surgery, which would make infections, such as NF, more likely?
-
(vii)
Have they been travelling abroad, and if so where, when and for how long? This helps form a list of possible infectious causes, including dengue, chikungunya and Zika virus, which can all cause a maculopapular rash. Rickettsia infection can also cause diffuse skin lesions.
-
(viii)
Do they have an underlying inflammatory skin condition, or is there a family history of an inflammatory dermatosis?
-
(ix)
Could they be immunocompromised, or do they have any risk factors associated with blood-borne virus infection? This broadens the list of possible infectious causes of a rash and makes serious infection more likely.
-
(x)
Are they postpartum, or could they have a retained vaginal tampon? If so, consider toxic shock syndrome (TSS).
Table 1.
Differential diagnosis of an unwell patient with a fever and cutaneous involvement
|
Examination
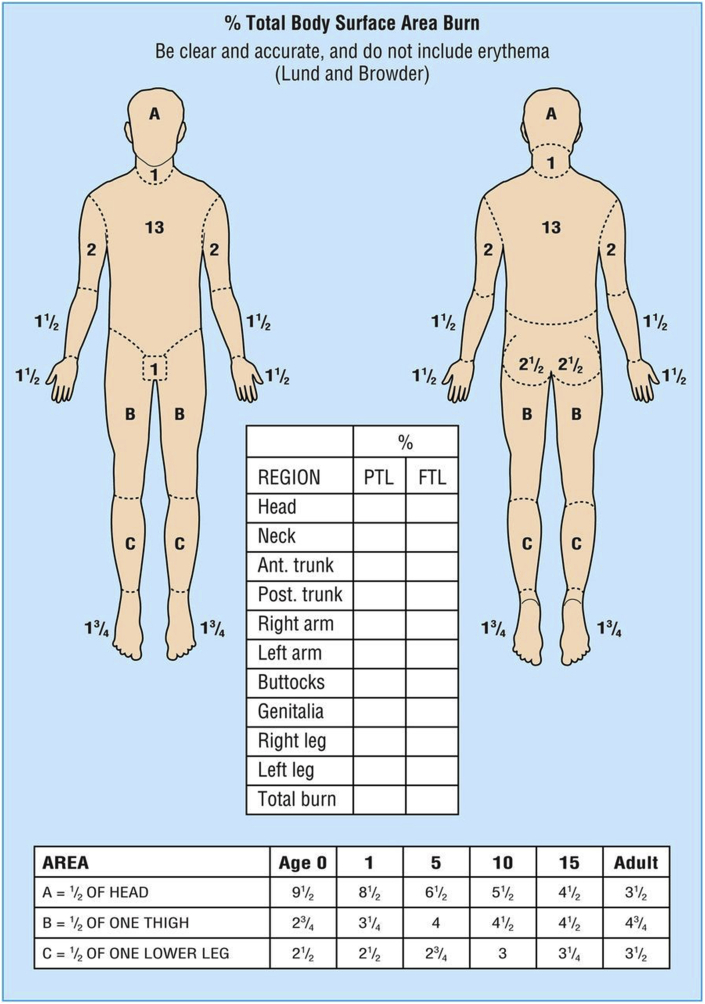
The physical examination of these patients should involve inspection and palpation of skin lesions, and the mucous membranes and eyes. Internationally agreed descriptive terms for the skin lesions observed should be used (Table 2).2 The extent of the cutaneous involvement will give an indication of the severity of the disease process, which can be quantified using the same method used in patients with burns (i.e. the Wallace ‘rule of nines’ or modified Lund–Browder charts [Fig. 1]).
Table 2.
Basic descriptive terms for cutaneous lesions2
| Term | Definition |
|---|---|
| Macule | Flat, circumscribed, non-palpable lesion that differs in colour from the surrounding skin; it can be any colour or shape (≤1 cm); referred to as a patch if >1 cm |
| Papule | Elevated, solid, palpable lesion that is ≤1 cm in diameter |
| Plaque | Circumscribed, palpable lesion >1 cm in diameter; most plaques are elevated; plaques may result from a coalescence of papules |
| Nodule | Elevated, solid, palpable lesion >1 cm usually located primarily in the dermis or subcutis; the greatest portion of the lesion may be exophytic or beneath the skin surface |
| Weal | Transient elevation of the skin caused by dermal oedema, often pale centrally with an erythematous rim |
| Vesicle | Circumscribed lesion ≤1 cm in diameter that contains liquid (clear, serous or haemorrhagic) |
| Bulla | Circumscribed lesion >1 cm in diameter that contains liquid (clear, serous or haemorrhagic) |
| Pustule | Circumscribed lesion that contains pus |
| Scale | Visible accumulation of keratin, forming a flat plate or flake |
| Crust | Dried serum, blood or pus on the surface of the skin |
| Erosion | Loss of either a portion of or the entire epidermis |
| Excoriation | Loss of the epidermis and a portion of the dermis caused by scratching or an exogenous injury |
| Ulcer | Full-thickness loss of the epidermis plus at least a portion of the dermis; it may extend into the subcutaneous tissue |
Fig 1.
Lund and Browder chart. PTL, partial thickness loss; FTL, full thickness loss.
It is also important to not only assess the integrity of the skin to aid diagnosis, but to be able to anticipate complications. For example, large areas of blistered, denuded or eroded skin can lead to fluid, protein and electrolyte loss; impaired thermoregulation; infection; and pain. The presence of mucous membrane involvement can indicate pulmonary or gastrointestinal disease.
Investigations
Blood samples should be sent for a full blood count, C-reactive protein and markers of renal and hepatic function. A coagulation and vasculitic screen should be considered if purpuric or vasculitic lesions are apparent. Bacterial and viral swabs of any blisters, erosions, pustules or crusts should be taken. If an infectious process is suspected, specific serological tests and cultures should also be requested. A skin biopsy may be required after a review by a dermatologist. If skin lesions suggest septic emboli, then echocardiography should be performed. Early liaison with a dermatologist is important to guide further investigation, as treatment is usually specific to the cause.3
General management of acute skin failure
From a dermatological perspective, acute skin failure is defined as total dysfunction of the skin and is considered a consequence of a number of primary dermatological disorders, including TEN and SJS.4
Regardless of aetiology, any patient with epidermal loss greater than 10% of his/her body surface area (BSA) should be referred to a specialist burns centre, as the cutaneous defect, and thus its management, is analogous to a burn. Acute skin failure is often complicated by sepsis and additional organ dysfunction, which is the most common cause of death in these patients.5 Box 1 describes the general management of life-threatening dermatoses.5,6
Box 1. General management of life-threatening dermatoses.5,6.
-
•
Immediate referral to a burns centre.
-
•
Where applicable, a severity-of-illness score for toxic epidermal necrolysis should be calculated within the first 24 h of admission.
-
•
Strict barrier nursing to reduce nosocomial infections.
-
•
Insert i.v. lines through non-lesional skin if possible.
-
•
Use usual indicators for fluid therapy. Fluid requirements likely to be less than the Parkland formula predicts. Consider the use of albumin in the resuscitation phase.7
-
•
Careful handling of the patient’s skin to lessen the extent of epidermal detachment.
-
•
Avoidance of the use of sphygmomanometer cuffs, adhesive dressings, electrocardiography leads and identification wrist tags.
-
•
Take swabs for bacterial and candidal culture from three areas of lesional skin on alternate days throughout the acute phase. Take viral swabs if herpes virus infection is suspected.
-
•
Give systemic antibiotics only if there are clinical signs of infection.
-
•
In patients with diarrhoea, consider a faecal management system to prevent faecal soiling of wounds.
-
•
Pay strict attention to background and procedural pain/sedation requirements.
-
•
Early patient-specific nutrition.
-
•Regular multidisciplinary team (MDT) review of the need for surgical intervention, which may include:
-
∘Removal of necrotic/loose infected epidermis and cleaning of wounds using a topical antimicrobial agent (e.g. betadine or chlorhexidine) under general anaesthetic.
-
∘VersaJet (Drytac, Bristol, UK) debridement.
-
∘Physiological closure with BIOBRANE (Smith+Nephew, Watford, UK)/allograft/xenograft skin in patients with early presentation involving non-infected and large confluent areas
-
∘
Alt-text: Box 1
Primary skin conditions presenting to critical care
Infectious conditions
Infectious conditions leading to sepsis and organ failure are responsible for the majority of primary dermatological presentations to critical care.1 Early treatment with antibiotics and surgical source control forms the mainstay of treatment.
Necrotising fasciitis
Necrotising fasciitis results from a bacterial infection affecting the soft tissue and fascia. Toxin and enzyme release from the bacteria causes localised thrombosis and necrosis, which subsequently spread as the condition progresses. Initial signs and symptoms may be non-specific and include swelling, erythema, pain and tachycardia. Pain that is disproportionate to superficial appearance, skin discoloration (ecchymosis), blisters or bullae, necrosis, crepitus or subcutaneous gas can all ensue as the infection progresses, and also systemic signs and symptoms, including fever and flu-like symptoms to septic shock.7
Early diagnosis of this condition is important to prevent tissue loss and subsequent morbidity and mortality. A high index of suspicion for NF should be considered in patients with a soft tissue infection and risk factors, including obesity, diabetes mellitus, immunosuppression and i.v. drug use. The most common causative agents for NF are polymicrobial (Type 1), haemolytic Streptococcus A or Staphylococcus aureus (Type 2) and Clostridium sp. (Type 3). Prompt and complete surgical debridement plus appropriate antimicrobial therapy in conjunction with supportive care are required.7
Cellulitis and erysipelas
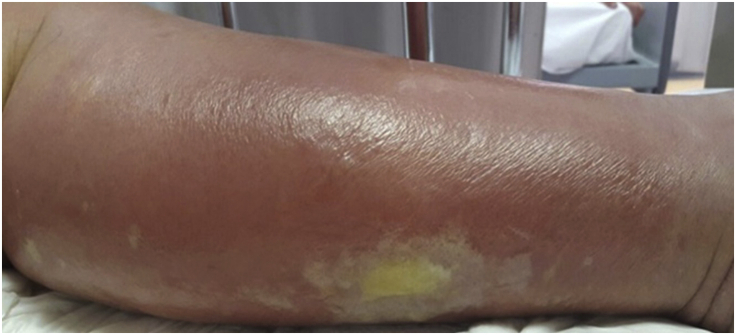
Cellulitis is a bacterial infection in the lower dermis and subcutaneous fat. Erysipelas is a superficial form of cellulitis affecting the upper dermis and superficial lymphatics. Cellulitis classically presents as unilateral spreading erythema that may or may not be well demarcated, accompanied by systemic symptoms, including pyrexia. The affected area may be painful and warm to the touch. Cutaneous lymphatic oedema causing a peau d'orange (orange peel) appearance can occur, and also vesicles, bullae, ecchymoses and even petechiae. In erysipelas, the affected skin has a raised border and is characteristically red, firm and swollen. The skin may blister and become necrotic. Erysipelas typically affects the lower limbs, but it can also affect the face. Cellulitis also typically affects the lower extremities, but it can occur anywhere, including the upper limbs in i.v. drug users or in those with in situ i.v. cannulae (Fig. 2).
Fig 2.
Cellulitis of the lower limb.
Cellulitis is one of the most common dermatological conditions that requires admission to critical care.1 In the majority of patients, it can be treated in a ward environment with oral antibiotics, but should the resultant sepsis lead to organ dysfunction and shock, critical care will be required to provide intensive supportive therapy. Septic shock from the skin infection can lead to other organ involvement, such as necrotising or haemorrhagic pneumonia, bone involvement with osteomyelitis, meningitis and endocarditis.
Cellulitis is most commonly caused by staphylococcal bacteria, including methicillin-sensitive (MSSA) and methicillin-resistant S. aureus (MRSA) or Group A streptococci (often Streptococcus pyogenes). It has also been associated with Groups B, C and G streptococci. If purulent cellulitis is identified (presence of a pustule, abscess or purulent drainage), the causative organism is likely to be S. aureus. Resistant strains, such as MRSA, are an increasing problem in healthcare facilities and should be screened for on admission to critical care and considered when choosing antimicrobial therapy in patients with a skin infection.8 If a patient presents with flu-like illness and necrotising skin infection, Panton–Valentine leucocidin S. aureus should be suspected. Panton–Valentine leucocidin is an exotoxin produced by virulent strains of both MSSA and MRSA, and can lead to haemorrhagic pneumonia in addition to severe skin infection.9
Prompt treatment with antimicrobials is required in cases of cellulitis; the choice of drug depends on the severity of the infectious process and other factors, such as the presence of pus, a history of trauma or animal bite, positive microbiology tests and the patient's risk of immunosuppression. Patients with non-purulent cellulitis and no risk factors for MRSA colonisation can be managed with antibiotics that cover beta-haemolytic streptococci and MSSA. Patients presenting with cellulitis causing sepsis may require broad-spectrum antibiotics, and discussion with local microbiologists is advised.10 For adults who have had treatment in hospital for at least two separate episodes of cellulitis or erysipelas in the previous 12 months, a trial of prophylactic antibiotics could be considered.11
Toxic shock syndrome
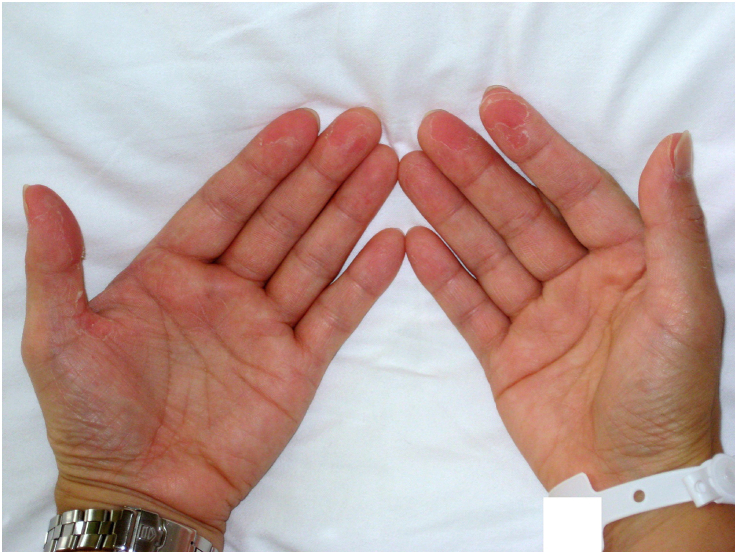
Toxic shock syndrome is a severe condition associated with exotoxin release secondary to staphylococcal or streptococcal infection. It presents with a rapidly developing fever, rash (diffuse macular erythroderma), hypotension and multi-organ dysfunction. Shedding of the skin, particularly of the hands and feet, is seen 1–2 weeks after the onset of the illness (Fig. 3). The diagnostic criteria for staphylococcal scalded skin syndrome are outlined in Box 2.12
Fig 3.
Desquamation of the hands after toxic shock syndrome.
Box 2. Clinical criteria for staphylococcal toxic shock syndrome (US Centers for Disease Control and Prevention).12.
An illness with the following clinical manifestations:
(i) Fever: temperature greater than or equal to 38.9°C.
(ii) Rash: diffuse macular erythroderma.
(iii) Desquamation: 1–2 weeks after onset of rash.
(iv) Hypotension: systolic blood pressure ≤90 mmHg for adults or less than fifth percentile by age for children aged <16 yrs.
- (v) Multisystem involvement (three or more of the following organ systems):
-
•Gastrointestinal: vomiting or diarrhoea at onset of illness
-
•Muscular: severe myalgia or creatine phosphokinase level at least twice the upper limit of normal
-
•Mucous membrane: vaginal, oropharyngeal or conjunctival hyperaemia
-
•Renal: blood urea nitrogen or creatinine at least twice the upper limit of normal for laboratory or urinary sediment with pyuria (≥ 5 leucocytes per high-power field) in the absence of urinary tract infection
-
•Hepatic: total bilirubin, alanine aminotransferase enzyme or aspartate aminotransferase enzyme levels at least twice the upper limit of normal for laboratory
-
•Haematologic: platelets <100,000 mm–3.
-
•CNS: disorientation or alterations in consciousness without focal neurological signs when fever and hypotension are absent
-
•
Laboratory criteria for diagnosis:
- Negative results on the following tests, if obtained:
-
•Blood or cerebrospinal fluid cultures (blood culture may be positive for Staphylococcus aureus)
-
•Negative serologies for Rocky Mountain spotted fever, leptospirosis or measles
-
•
- Case classification:
-
•Probable
-
•
- A case that meets the laboratory criteria and in which four of the five clinical criteria described previously are present.
-
•Confirmed
-
•
A case that meets the laboratory criteria and in which all five of the clinical criteria described previously are present, including desquamation, unless the patient dies before desquamation occurs.
Alt-text: Box 2
Staphylococcal TSS from MSSA or MRSA strains is caused by TSS toxin-1 (TSST-1). Patients with clinical TSS lack the corresponding antibody to TSST-1. Antibodies usually develop in 90–95% of the population by the fourth decade, making TSS a condition of the young.13
Streptococcal TSS results from invasive infection with a strain that has the ability to release pyrogenic exotoxins (superantigens) and virulence factors that activate the immune system to release inflammatory cytokines. It was originally described in 1980 when an association with vaginal tampon use was made; now, non-tampon-related causes account for more than half of cases. A proportion of these are post-partum related, but entry of the pathogen from many different sites has been described in both men and women, and includes the skin, vagina and pharynx. In at least half of streptococcal TSS cases, no site of entry is found.13
Complications include haemolytic anaemia, disseminated intravascular coagulation and multiple organ dysfunction. The use of ultrasound, CT and MRI can aid in the diagnosis and quantification of invasive infections. However, where surgical intervention is required, this should not be delayed whilst awaiting further imaging.
Source control with surgical debridement of the infected area may be required, particularly in streptococcal TSS. Samples of tissue should be sent for microbiological testing at the time of surgery. Empirical antibiotic therapy should be commenced immediately according to local guidelines. This therapy will usually include a broad-spectrum antibiotic with the addition of clindamycin. (Clindamycin inhibits exotoxin synthesis via its action on the 50S subunit of the bacterial ribosome.) Vancomycin should be considered where there is suspicion of staphylococcal TSS. These regimens should be rationalised once a causative organism is identified.
The routine use of i.v. immunoglobulins is not recommended because evidence of efficacy is limited, although it should be considered in those with severe, unresponsive disease.14
Drug-related skin conditions
Stevens–Johnson syndrome and toxic epidermal necrolysis
Stevens–Johnson syndrome and TEN are part of a spectrum of rare and potentially fatal acute skin conditions characterised by severe mucocutaneous reactions, epidermal loss and systemic disturbance. Drugs are the causative agent in up to 85% of cases, with a latency period of 4–28 days from drug initiation. Antibiotics are the most common precipitants, including sulphonamides and beta lactams. Allopurinol, anticonvulsants and NSAIDs have also been implicated. Infections, including cytomegalovirus and mycoplasma, are the next most common trigger. In addition, acute graft vs host disease can result in TEN and is usually fatal.15
Signs and symptoms include a prodromal illness for several days, including fever, sore throat and malaise, followed by the abrupt development of painful erythematous skin across the trunk, face and limbs. A prodromal skin rash may start as macules, progress to targetoid lesions and blisters, with the blisters then merging together to produce sheet-like areas of skin loss. Blisters and erosions can appear with minimal skin manipulation known as Nikolsky's sign (dislodgement of the epidermis with the application of direct pressure). The erythema is followed by extensive cutaneous and mucosal necrosis within 2–3 days. Mucosal involvement can be widespread and include the eyes, oropharynx, gastrointestinal and respiratory tract. Signs and symptoms involving <10% of the body surface are classified as SJS. If 10–30% of BSA is affected, it is classified as TEN/SJS overlap.15
These conditions can be life threatening with a mortality of up to 30%. Immediate drug cessation is imperative, as this reduces mortality.5 Complications include septic shock and multiple organ failure, fluid and electrolyte disturbance, gastrointestinal perforation and thromboembolic phenomenon. Studies have not demonstrated efficacy of any one intervention over supportive care alone in SJS/TEN, although i.v. immunoglobulins, corticosteroids and cyclosporin are commonly used. Supportive care includes addressing nutrition; appropriate replacement of fluids; temperature maintenance; pain relief; and specific care for eyes, mouth, genitals and lungs. The skin may require dressings and topical antiseptics with the avoidance of deroofing the lesions. Antibiotics should be used in caution and only in response to infection. Treatment with corticosteroids is controversial, with no proven benefit.5
Drug rash, eosinophilia and systemic symptoms syndrome
Drug rash, eosinophilia and systemic symptoms syndrome (also known as drug hypersensitivity syndrome) is a severe, life-threatening adverse drug reaction. It presents with a short history of fever and malaise followed by the development of a morbilliform rash initially involving the face. The rash may then extend to the trunk and lower limbs, and can also progress to an exfoliative dermatitis. Multisystem involvement can occur with the lymphatic, haematological and hepatic systems most commonly affected. Causative agents are identified in approximately 80% of cases with anticonvulsants, antimicrobials, antivirals and NSAIDs, all being implicated in its development. The lag phase between commencing the drug and the onset of symptoms is 2–6 weeks, typically longer than other adverse drug reactions. Treatment involves immediate cessation of the causative agent and commencement of high-dose steroids, alongside supportive therapy for other organ involvement. The estimated mortality is 10%.16
Immune mediated
Erythema multiforme
Erythema multiforme (EM) is a rare immune-mediated skin disorder characterised by the development of widespread polymorphous lesions that erupt over 24 h. Once thought to be part of the SJS/TEN spectrum, it is now regarded as a distinct condition.
Target lesions are typical of EM with a dark centre, a pale pink and oedematous middle ring and a bright red outermost ring (Fig. 4). There are two forms: minor and major. In EM minor, there are no prodromal symptoms. However, in EM major, systemic symptoms, such as pyrexia and joint pain, and mucosal involvement may be seen. The most common cause for EM is infection (90%), particularly herpes simplex virus or Mycoplasma pneumoniae. It may also be caused by drugs (10%), most commonly sulphonamides, anticonvulsants, allopurinol and antibiotics.17
Fig 4.
Target lesions affecting the trunk and limbs in an infant.
The condition is usually self-limiting, but severe cases involving the gastrointestinal tract or airway may require critical care. Treatment comprises supportive care, steroids in some cases, antiviral or antibacterial medications in the acute phase if an infective trigger is suspected and stopping causative agents in drug-induced EM.18
Pemphigus vulgaris
Pemphigus vulgaris (PV) is a rare, immunoglobulin G-mediated autoimmune condition, in which destruction of desmosomal proteins in the epidermis causes widespread intraepithelial and mucocutaneous blistering (Fig. 5).19
Fig 5.
Extensive pemphigus vulgaris.
Those patients with severe disease requiring critical care admission have a mortality in excess of 40%.1 It classically presents in the third to sixth decade of life with blistering of the oral mucosa. This progresses to cutaneous blistering over weeks to months, most commonly on the upper chest, back, scalp and face. The lesions rupture easily and can cause painful erosions, making adequate nutrition difficult when there is oral involvement. The application of lateral mechanical pressure on the skin can also induce a positive Nikolsky's sign with blistering caused by dislodgement of the upper epidermis from the lower epidermis.
Treatment should focus on decreasing blister formation, preventing infection and promoting healing of pre-existing blisters. Corticosteroids are used in an attempt to control the disease with either oral prednisolone or pulsed methylprednisolone in severe cases. Adjuvant immunosuppressive therapies may be used in the initial phase for their steroid-sparing effect and in later phases to maintain remission. Plasma exchange or i.v. immunoglobulin therapy can be given when immunosuppressant therapy has failed.19
A patient with PV may require admission to critical care for the management of a number of issues, including pain, infection, adverse effects of drug treatment, delirium, electrolyte and fluid derangement and nutrition. Fulminant organ failure may also occur.20
Inflammatory dermatoses
Acute generalised pustular psoriasis
Acute generalised pustular psoriasis (AGPP) is a rare inflammatory skin disease that presents with sudden onset of widespread sterile pustules on a background of erythematous tender skin. It develops with concomitant systemic symptoms, such as fever, headache, loss of appetite, nausea, muscle weakness and malaise. A full blood count may show anaemia, neutrophilia or lymphopenia. Ten percent of patients with AGPP have a preceding history of more conventional plaque psoriasis. The aetiology is not fully understood, but it has been linked to the abrupt withdrawal of steroid therapy, medications (such as ramipril, rituximab, clopidogrel, amoxicillin, lithium, aspirin and NSAIDS), infections (including cytomegalovirus), Epstein–Barr and varicella zoster, and has also been reported in pregnancy. Specific gene mutations have been identified with abnormalities in cytokine signalling.21
Severe AGPP can be life threatening and requires specialist treatment to prevent further fluid loss and maintain body temperature and electrolyte balance. Systemic treatment includes immunosuppressants, such as methotrexate or cyclosporin, an oral retinoid (acitretin) or biological agents (such as infliximab, etanercept, adalimumab and ustekinumab). Systemic steroid therapy carries the risk of worsening the condition, but can be used in some cases under the strict guidance of a dermatologist.21 Critical care may be required to manage the fluid and electrolyte disturbances, support multiple organ failure and treat any secondary infection or complications of drug therapy.
Erythroderma (exfoliative dermatitis)
Erythroderma is the term used to describe an inflammatory condition causing widespread erythema and oedema affecting over 90% of the skin surface. It often precedes or is associated with exfoliation (peeling/scaling) of the skin resulting in ‘exfoliative dermatitis’. Erythroderma is most often seen in patients with a pre-existing dermatological condition that has worsened, for example psoriasis, atopic dermatitis, pityriasis rubra pilaris, immunobullous disease or cutaneous T-cell lymphoma (Sezary syndrome). It has also been described in psoriasis after rapid cessation of systemic steroids or other immunosuppressive treatment. In addition, erythroderma may be secondary to a drug reaction, or a sign or symptom of a systemic condition, such as a haematological malignancy, graft vs host disease, human immunodeficiency virus infection and internal malignancies. Critical care may be required because of complications relating to the loss of the skin barrier, including heat loss, fluid and electrolyte imbalance, hypoalbuminaemia and sepsis.22
Management centres on treating the underlying skin condition, for example using steroids for dermatitis or methotrexate for psoriasis. Supportive care includes antibiotics for systemic infection, the application of wet wraps or emollients to maintain skin moisture and careful management of fluids and electrolytes.22
Summary
Life-threatening dermatoses are thankfully rare, but are associated with a high morbidity and mortality. Such conditions require a multidisciplinary approach to not only the diagnosis, but also the management strategies used. Medical skin loss in this context may require multiple organ support, and critical care stay is likely to be longer than average.
Declaration of interests
The authors declare that they have no conflicts of interest.
Biographies
Sarah Marsh FRCA FFICM is a consultant in anaesthesia and intensive care medicine at Harrogate District Hospital. She is the course director for the Faculty of Intensive Care Medicine's exam preparatory course and is vice-chair of both the Women in Intensive Care Medicine group and the newly formed Education Sub-Committee at The Faculty of Intensive Care Medicine.
Matt Bromley BSc FRCA FFICM is a specialty registrar in anaesthesia and intensive care medicine at Leeds Teaching Hospitals NHS Trust. He has an interest in education and produces the podcasts for the Education Sub-Committee at The Faculty of Intensive Care Medicine.
Alison Layton FRCP is a consultant dermatologist at Harrogate and District NHS Foundation Trust and honorary professor at Hull York Medical School. She is also the specialty lead for dermatology for the Yorkshire and Humber Clinical Research Network.
Matrix codes: 1B04, 2C01, 3C00
MCQs
The associated MCQs (to support CME/CPD activity) will be accessible at www.bjaed.org/cme/home by subscribers to BJA Education.
References
- 1.George S.M.C., Harrison D.A., Welch C.A., Nolan K.M., Freidmann P.S. Dermatological conditions in intensive care: a secondary analysis of the intensive care national audit & Research centre (ICNARC) case mix programme database. Crit Care. 2008;12:S1. doi: 10.1186/cc6141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nast A., Griffiths C., Hay R., Sterry W., Bolognia J. The 2016 International League of Dermatological Societies’ revised glossary for the description of cutaneous lesions. Br J Dermatol. 2016;174:1351–1358. doi: 10.1111/bjd.14419. [DOI] [PubMed] [Google Scholar]
- 3.Oakley A. 2016. Fever and a rash.https://dermnetnz.org/topics/fever-and-a-rash/ Available from: [Google Scholar]
- 4.Inadmadar A.C., Palit A. Acute skin failure: concept, causes, consequences and care. Indian J Dermatol Venereol Leprol. 2005;71:379–385. doi: 10.4103/0378-6323.18007. [DOI] [PubMed] [Google Scholar]
- 5.Creamer D., Walsh S., Dziewulski P.U.K. Guidelines for the management of Stevens–Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016;174:1194–1227. doi: 10.1111/bjd.14530. [DOI] [PubMed] [Google Scholar]
- 6.Navickis R.J., Greenhalgh D.G., Wilkes M.M. Albumin in burn shock resuscitation: a meta-analysis of controlled clinical studies. J Burn Care Res. 2016;37:e268–e278. doi: 10.1097/BCR.0000000000000201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davoudian P., Flint N.J. Necrotizing fasciitis. BJA Educ. 2012;12:245–250. [Google Scholar]
- 8.Raff A.B., Kroshinsky D. Cellulitis: a review. JAMA. 2016;316:325–337. doi: 10.1001/jama.2016.8825. [DOI] [PubMed] [Google Scholar]
- 9.Morgan A.J., Glossop A.J. Severe community acquired pneumonia. BJA Educ. 2016;16:167–172. doi: 10.1093/bjaed/mkv052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stevens D.L., Bisno A.L., Chambers H.F. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014;59:e10–52. doi: 10.1093/cid/ciu444. [DOI] [PubMed] [Google Scholar]
- 11.National Institute for Health and Care Excellence . 2019. Cellulitis and erysipelas: antimicrobial prescribing.https://www.nice.org.uk/guidance/ng141/resources/cellulitis-and-erysipelas-antimicrobial-prescribing-pdf-66141774778309 Clinical guideline NG141. Available from: [Google Scholar]
- 12.Centers for Disease Control and Prevention. Toxic shock syndrome (other than streptococcal) (TSS) 2011 case definition. 2011. Available from https://wwwn.cdc.gov/nndss/conditions/toxic-shock-syndrome-other-than-streptococcal/case-definition/2011/(accessed 14 May 2021).
- 13.Khayr W. 2020. Toxic shock syndrome. BMJ best practice.https://bestpractice.bmj.com/topics/en-gb/329 Available from: [Google Scholar]
- 14.Schmitz M., Roux X., Huttner B., Pugin J. Streptococcal toxic shock syndrome in the intensive care unit. Ann Intensive Care. 2018;8:88. doi: 10.1186/s13613-018-0438-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yau F., Emerson B. ‘Medical skin loss’: Stevens–Johnson syndrome/toxic epidermal necrolysis and staphylococcal scalded skin syndrome. BJA Educ. 2016;16:79–86. [Google Scholar]
- 16.Scrace B., Fityan A., Bigham C. Drug reactions with eosinophilia and systemic symptoms. BJA Educ. 2020;20:65–71. doi: 10.1016/j.bjae.2019.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sokumbi O., Wetter D.A. Clinical features, diagnosis, and treatment of erythema multiforme: a review for the practicing dermatologist. Int J Dermatol. 2012;51:889–902. doi: 10.1111/j.1365-4632.2011.05348.x. [DOI] [PubMed] [Google Scholar]
- 18.Lerch M., Mainetti C., Beretta-Piccoli B.T., Harr T. Current perspectives on erythema multiforme. Clin Rev Allergy Immunol. 2018;54:177–184. doi: 10.1007/s12016-017-8667-7. [DOI] [PubMed] [Google Scholar]
- 19.Harman K., Brown D., Exton L. British Association of Dermatologists’ guidelines for the management of pemphigus vulgaris 2017. Br J Dermatol. 2017;177:1170–1201. doi: 10.1111/bjd.15930. [DOI] [PubMed] [Google Scholar]
- 20.Miletta N., Miller M.E., Lam T., Chung K.K., Hivnor C. The management of pemphigus vulgaris in a burn intensive care unit: a case report and treatment review. J Burn Care Res. 2014;35:e357–e363. doi: 10.1097/BCR.0000000000000049. [DOI] [PubMed] [Google Scholar]
- 21.Hoegler K., John A., Handler M., Schwartz R. Generalized pustular psoriasis: a review and update on treatment. J Eur Acad Dermatol Venereol. 2018;32:1645–1651. doi: 10.1111/jdv.14949. [DOI] [PubMed] [Google Scholar]
- 22.Sehgal V.N., Srivastava G. In: Emergency dermatology. Wolf R., Davidovici B.B., Parish J.L., Parish L.C., editors. Cambridge University Press; Cambridge: 2010. Erythroderma/exfoliative dermatitis; pp. 202–214. [Google Scholar]