Abstract
Objectives:
This study sought to identify coronavirus disease 2019 (COVID-19) risk communication materials distributed in Jamaica to mitigate the effects of the disease outbreak. It also sought to explore the effects of health risk communication on vulnerable groups in the context of the pandemic.
Methods:
A qualitative study was conducted, including a content analysis of health risk communications and in-depth interviews with 35 purposively selected elderly, physically disabled, persons with mental health disorders, representatives of government agencies, advocacy and service groups, and caregivers of the vulnerable. Axial coding was applied to data from the interviews, and all data were analyzed using the constant comparison technique.
Results:
Twelve of the 141 COVID-19 risk communication messages directly targeted the vulnerable. All participants were aware of the relevant risk communication and largely complied. Barriers to messaging awareness and compliance included inappropriate message medium for the deaf and blind, rural location, lack of Internet service or digital devices, limited technology skills, and limited connection to agencies that serve the vulnerable.
Conclusion:
The vulnerable are at increased risk in times of crisis. Accessibility of targeted information was inadequate for universal access to health information and support for vulnerable persons regardless of location and vulnerability.
Keywords: COVID-19, vulnerable, risk communication, access, equity
Misinformation during health emergencies such as coronavirus disease 2019 (COVID-19) often drives fear and anxiety, especially among marginalized and vulnerable communities.1 In Jamaica, a public risk communication campaign was mounted in response to the pandemic to allow the public to make informed decisions to mitigate the effects of a disease outbreak. This study documented the perspectives of the elderly, the physically disabled, and persons with mental health disorders as well as advocacy and service groups, and caregivers of the vulnerable on the effects of health risk communication in the context of the COVID-19 pandemic.
Risk communication is generally thought to be a 2-way process between the communicator and the target audience. The goal is to build trust, raise awareness, reach mutual agreements, and motivate action.2 This ideal is often not realized in the urgency created by crisis situations such as the COVID-19 pandemic. Effective risk communication considers how societal and cultural factors influence perceptions of risk including, how persons with special needs respond differently than the general public to risks.3 Many forms of risk communication are used, ranging from media and social media communications to mass communications and stakeholder and community engagement. Effective risk communication must also identify early on and subsequently manage rumors, misinformation, and other communications challenges.4
Vulnerable citizens are in dire need of effective risk communication during the pandemic.5,6 The COVID-19 Long-Term Care Situation in Jamaica7 showed that older persons, those with comorbidities, and persons with disabilities were at higher risk of infection due to limited mobility, difficulty understanding information, or challenges in practicing preventive measures. It has been reported that older adults and persons with comorbidities, such as noncommunicable diseases and asthma, are at higher risk of developing a severe form of the illness if infected with the novel coronavirus.8,9 Persons with disabilities may also be at higher risk of infection and are more likely to have an underlying health problem.10
A recent rapid review discusses the wide range of adverse effects on persons with physical disabilities.11 In response to the pandemic, the public health authorities have recommended behavioral changes, including hand-washing, sanitization, mask-wearing, and social distancing.10 Some of these behaviors pose a challenge to persons who are disabled, such as those who are visually impaired. Inability to adopt recommended behavioral changes can result in negative psychosocial effects on these patients.12 Alongside the public health measures that have been executed to limit the spread of COVID-19,13 there has been significant social isolation that has affected vulnerable groups. These measures have also been linked with psychological distress and mental illness.14 Many persons with pre-existing mental illnesses may even be at higher risk during the pandemic.15
The objectives of this study were to (i) identify and document the communications materials that contributed to improving the awareness of the target population; (ii) describe the lived experiences of the elderly, and persons with physical disabilities and those with mental disorders; and (iii) describe the strategies and interventions that authorities, family members and caregivers used to appropriately support the members of the vulnerable groups.
Methods
This study involved a media content analysis and semi-structured interviews with 25 purposively selected members of the vulnerable population (Table 1) and 10 key informants that work closely with them. A 9-member team including the 8 authors and a paid transcriptionist conducted the data collection and analysis. All 3 interviewers were female academics with postgraduate education and over 5 years of experience in conducting qualitative research. The media content analysis was conducted by 2 team members with media training.
Table 1.
Profile of vulnerable participants
| Group | Type | Location | Age (y) Males |
Age (y) Females |
Total |
|---|---|---|---|---|---|
| Elderly | In home for aged | Kingston | 66, 70 | 40 | 3 |
| Urban community dwelling | St. Mary, Kingston | 64, 70, 72 | 3 | ||
| Rural community dwelling | Clarendon, St. Mary | 70, 75 | 70 | 3 | |
| Physically disabled | Blind | Clarendon, Kingston | 63 | 25, 55 | 3 |
| Persons in wheelchair – institution-based | Kingston | 27, 50 | 55 | 3 | |
| Persons in wheelchair – community-based | Kingston, St. Mary | 60 | 50, 54 | 3 | |
| Deaf | St. Mary, Kingston | 25, 29 | 2 | ||
| Mentally ill | Referred from community mental health | Kingston | 40 | 35 | 2 |
| Community resident | Kingston | 30 | 35, 45 | 3 | |
| TOTAL | 25 | ||||
The interview guide was developed by the team, pilot tested, and adjusted based on feedback. Interviews lasted between 40 and 60 min, were audio-recorded, and transcribed verbatim. Transcripts were checked by the interviewers for accuracy but were not shared with participants.
Members of the vulnerable populations were contacted by telephone and interviewed privately using a combination of Zoom and face-to-face sessions. There was only one refusal by a vulnerable participant. None of the participants was familiar to the interviewers before data collection.
One key informant from each of the 10 selected rural and urban agencies and serving vulnerable groups (Table 2) was asked to describe the strategies and interventions they used to support the vulnerable groups during the COVID-19 pandemic. They were also asked to indicate any observed gaps or challenges in the response to these groups.
Table 2.
Key informants agencies and organizations
| Vulnerable group | Key informant organization |
|---|---|
| Persons in wheelchair | Paralympic association |
| Persons in wheelchair | Community-based rehabilitation |
| Mentally ill | Community mental health services |
| Persons in wheelchair | Council for persons with disabilities |
| Blind | School for the blind |
| Blind | Society for the blind |
| Elderly | Local government and community development |
| Deaf | Association for the deaf |
Ethical approval was obtained from the ethical review boards of the Ministry of Health and Wellness (MOHW), of the University of the West Indies and of the Pan American Health Organization (PAHO). All participants provided informed consent and were made aware that the study was motivated by Ministry of Health and its partners’ need to document the effects of the pandemic on specific groups and their responses to health interventions.
Videos, audio materials, and print media that were classified by the production agency as created to respond to the COVID-19 pandemic were analyzed for content focused on raising the public’s awareness of COVID-19, preparation and risk mitigation, including messages directed to the target groups within this study. Materials were included only if they were produced by the Jamaica Ministries of Health and Wellness, Education, Youth and Information, Local Government, PAHO or the United Nations Children Fund (UNICEF) and distributed by means of traditional and digital platforms at least once during the defined study period between March 4, 2020, and September 30, 2020. To verify the reliability of the list of media items to be included in the study the two media trained researchers independently searched for content fitting the inclusion criteria using paid subscriptions and historical searches of online placements, with a 95% inter-rater agreement.
Data Analysis Media Content
Media content from all sources was sorted to eliminate duplication resulting in a reduction from 202 to 166 unique items. A content analysis data abstraction form (Supplementary Appendix 1) was used to log media content including the title; author; target audience; medium; aim of the message; thematic area; tone; accessibility; use of language; frequency of distribution and duration. The data were then summarized on a spreadsheet according to sources of the messages, the intended audience, the medium, and the thematic area of the message. These sub-groupings allowed for ease of comparison with the findings from the semi-structured interviews with the vulnerable group members and key informants.
Data Analysis Semi-structured Interviews
All 35 interviews were transcribed, de-identified, and uploaded into the Dedoose software program (www.dedoose.com) for analysis. Five members of the research team each coded a transcript independently applying open coding (labeling concepts based on their properties). Discussion between independent coders led to the development of a 21-item codebook with definitions (Supplementary Appendix 2). The list of codes was uploaded where axial coding (application of predefined codes) was applied to the transcripts, yielding 1171 coded excerpts. Triangulation of the data analysis process was applied to reduce bias and improve reliability. As such, the coded data from all sources were grouped, and each investigator assigned a set of codes to analyze for overarching categories across codes. Patterns and themes that emerged from the data were agreed on. Supporting quotations were exported from the software into an Excel spreadsheet and team members discussed the most appropriate to illustrate each theme and sub-theme.
Results
Media Content Review
Analysis of 166 pieces of risk communication revealed that 141 met the inclusion criteria; 70% of the content was directed to the general public, with 98 messages distributed across multiple platforms. The MOHW was the most prolific producer of public service announcements (PSAs) with a total of 37 items, produced alone, or in collaboration with UNICEF, PAHO/WHO, and the Ministry of Education Youth and Information. Two-thirds of messages that targeted the study population were directed to the elderly, ie, persons 65 years and older (12), the mentally ill (3), persons with disabilities (2). Persons with mental health challenges were targeted in four messages, while those with physical challenges were targeted in one feature newspaper article and one social media post.
Qualitative Interviews
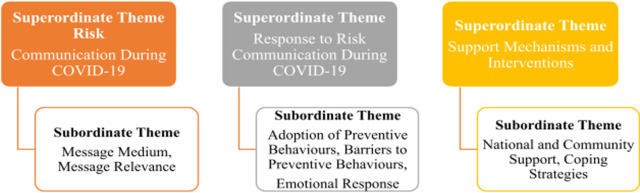
Three major or superordinate themes emerged from the analysis of the data from key informants and vulnerable group members (Figure 1). Risk Communication During COVID-19, Responses to Risk Communication During COVID-19, and Support Mechanisms and Interventions were the themes emerging from participants’ recall of COVID-19 related messaging, significant events, stressors, and supports that occurred during the pandemic. These major themes converged around subthemes that focused on specific aspects of participants’ accounts of the COVID-19 experiences specific to their vulnerabilities (Figure 1). Each theme and subtheme are further elaborated.
Figure 1.
Superordinate and subordinate themes.
Superordinate Theme: Risk Communication During COVID-19
All vulnerable groups indicated awareness of the COVID-19 communication messages, such as social distancing, hand sanitization, and wearing masks, produced by the MOHW, and less so the international agencies. The elderly gave more reports of messaging being relevant than other groups. Participants noted that messages on how COVID-19 is spread and prevented were frequently aired in traditional electronic media and on social media. “Sometimes it’s almost every day we get information.” (Person in a wheelchair).
Key informants (KIs) made references to having to filter some of this type of communication for the vulnerable population, particularly the blind and deaf, to ensure they received credible information.
“They would look for resources where they can get them, they relied heavily upon the internet… they were having trouble figuring out reliable sources of information like WHO, CDC, Ministry of Health compared to other areas … a lot of our time was spent trying to make sure that our constituents were getting clear information.” (KI- Physically challenged).
Subordinate Theme: Message Medium
Most of the vulnerable participants reported receiving their information by means of traditional electronic sources, with the radio being the primary source of information, followed by television. Other sources of information were social media, printed newspapers, and family and friends. The message source appeared to be varied based on the age and vulnerability of the respondent. For instance, elderly persons and those who were blind, reported getting most COVID-19-related messages from the radio, as they were in the habit of listening to the radio as a source of information. “I use the radio for my company, it is right at my head most of the time” (Blind respondent).
Younger vulnerable participants reported receiving information by means of social media or through their own network of friends with similar disabilities. In addition, some vulnerable participants were sources of information for other persons within their networks. “It was me mainly sharing the information because I’m always on the computer, the Internet and stuff like those” (Person in a wheelchair).
The medium of the messaging was crucial for the Blind and Deaf community due to their specific communication needs. “Smartphones come with the talkback feature that you can activate. I have it so I can read everything.” (Blind respondent). Agencies that serve deaf individuals were also able use specialized mobile apps to communicate with their constituents.
The medium and pace of communication about lockdowns and quarantine measures were particularly challenging for the deaf community. Often instructions had to be redirected through the medium of the agencies and communication to employers also facilitated.
“The fact that quarantine and lockdown orders took a few days to get online was a frustrating experience for us. As soon as press conferences were done, we began to see messages asking could you please explain this to me.” (KI - Deaf agency)
Printed materials were the least suitable for all groups including the deaf because their communication relied a lot on facial expressions. “The video is just much more fluid - so much more understandable for the community than a lot of written text.” (KI - Deaf Agency).
Subordinate Theme: Message Relevance
Respondents across all vulnerabilities reported that though messages were generally relevant, most messages did not contain information applicable to their specific vulnerability. “I don’t think they targeting any particular group it was just general information for the entire public.” (Elderly participant). For example, blind participants noted that there was no reference to sanitizing canes which are vital to the mobility of the Blind in any of the numerous messages encouraging sanitization.
“Blind persons use canes to navigate but no messages were given about sanitizing the cane, such as finding an appropriate solution that could be used to sanitize the cane after coming off the road or a public space.” (KI - Blind)
References were made to the need for specific messaging catering to the needs of vulnerable groups, particularly how to cope with the emotional and financial aspects of COVID-19.
Superordinate Theme: Response to Risk Communication During COVID-19
Most vulnerable participants reported adopting preventive behaviors, such as mask-wearing, social distancing, hand sanitization, and staying home. Staying at home was most consistently adopted by the elderly and physically disabled. The action mentioned most frequently was sanitizing and washing hands.
Subordinate Theme: Adoption of Preventive Behaviors
All vulnerable participants reported adopting at least one, or all the behaviors, encouraged to reduce their risk of contracting the disease.
“The other day … I was going into the taxi from the hospital, I asked the driver “how much you bring in the back?” He said only three and I asked “everybody in the back in their mask?” The lady that followed me, said “yes” I said “ok we can take that taxi.” (Blind – rural participant).
Key informants from all agencies reported that preventive behaviors were adopted by their groups regardless of the vulnerability. “They understand that they are vulnerable… therefore, it is imperative and nonnegotiable for them to follow the protocols.” (KI - Persons in wheelchairs).
Wearing masks and social distancing were reportedly the most difficult preventive behaviors to adopt. The reasons given for this varied among the target populations. Some persons felt discomfort in wearing masks in the hot temperatures while for some, respiratory issues were made worse by mask-wearing. “Wearing of the mask would have been hardest … some physically challenged would have already had respiratory challenges.” (KI - Persons in wheelchairs). Deaf participants reported that mask-wearing interfered with their ability to communicate effectively because much of their communication involves facial expressions and body language. Reported barriers to adopting the recommended preventive behaviors included acute mental conditions, inflexible living arrangements of those in institutions and involuntary exposure to COVID-19 from the actions of others. The mentally ill in institutions also had specific challenges related to self-harm related to wall mounted hand sanitizers. “For example when they tell us to put sanitizer in a facility. You don’t do that for people who are mentally ill because they will pull them off and hurt each other.” (KI - Mentally ill).
Where there were barriers to carrying out preventive behavior based on a specific vulnerability, attempts were made to overcome them including avoiding public spaces.
Subordinate Theme: Emotional Response
The volume and frequency of risk communication messages, tone of the messages, uncertainty about their economic well-being, food insecurity, and isolation brought on by quarantine and stay-at-home orders led to feelings or fear, anxiety, and sadness among vulnerable persons in this study. Participants used expressions such as “overwhelming,” “overpowering,” “frightening,” “stressful,” “shocking,” “panicked,” and “nerve-wracking” to describe their emotions in relation to the COVID-19 communication. “I think it was too much at one point. That’s why it panic mi because it was over and over.” (Blind participant).
Fear and anxiety led persons to delay or avoid seeking health care or going out to socialize.
“I have a medical issue that I’m supposed to have addressed in town for a while now. I have not done it. Every time I say I’m going and I think about the seriousness of COVID. I just back off.” (Elderly rural participant).
Persons with comorbidities expressed fatalism related to COVID-19 infection based on the information communicated about risk and the people who died from COVID-19. “…based on my risk mi know seh if mi shoulda attract it now mi nah go survive.” (Person in a wheelchair).
Persons with mental conditions were reported to have relapsed due to the stresses of coping with COVID-19. “…saw an increase in persons presenting with depression and a number of persons who were relapsing even though they had been stable for a long time.” (KI - Mentally ill).
Residents within the nursing homes reported that their reduced access to food following quarantine caused fear and anxiety as their individual servings of food was packaged and delivered. This meant they were not able to then get more food if they became hungry between the scheduled mealtimes which was different than the situation before being quarantined when they were able to get seconds if so desired when meals were served in a buffet arrangement. “By the time eight o clock come, we’re hungry and going to bed hungry.” (Elderly in home for the aged).
Loss of income and fear sometimes led to sadness in vulnerable respondents. “I’m at home I start have to live off the little money that I saved. I really can’t get any jobs now, based on the career that I have.” (Person in a wheelchair).
Elderly respondents felt sadness and depression associated with isolation and quarantine and the inability to access services such as agency organized entertainment programs for senior citizens. Others were more depressed by not having money than the confinement. “Even right now I can’t go to the bank …” (Elderly in a quarantined home for the aged).
Some persons reported lack of connection to persons with similar vulnerabilities due to the closure of facilities and programs as generating feelings of disconnection and depression. “So, within our community there is a very emotional, I don’t want to call it void, but there is something that’s missing …” (KI - Agency for the deaf).
Superordinate Theme: Support Mechanisms and Interventions
Agencies were key to communicating information and advocating for support for vulnerable groups with communication challenges, particularly the deaf and blind as reported earlier in this report. Agencies actively implemented actions to facilitate access to COVID-19 support for members.
“Every week PATH sends something for the children …to eat… the children are all over the country, they cannot come here to pick up …because of the distance… we plan to send our driver to drop the stuff in those places where, we …have rural locations.” (KI - Agency for the deaf).
Innovations to enable vulnerable groups to remain informed and independently functional were adopted by the agencies that served the vulnerable groups. Some were technical in nature. “…we got some financial institutions to make an effort to put things in place to meet the needs of the visually-impaired is a significant achievement.” (KI - Agency for the blind).
COVID-19 protocols led to disconnection of the vulnerable to some services particularly related to agencies that serve them. Schools for the blind and deaf were physically closed. Online delivery affected many who did not have access to the Internet or suitable devices similar to the general population.
“… we know a number of students already struggle with having access to … tablets, computers, or even internet, there are ways around that. With the deaf community the additional problem comes into place with the fact that most families have little to no knowledge to communicate using sign language …” (KI - Agency for the deaf).
Subordinate Theme: National and Community Support
Government agencies, community organizations and agencies that serve vulnerable groups reportedly provided limited support mechanisms for coping with the COVID-19 pandemic. This included remote access to services which allowed vulnerable persons to be able to conduct business.
“Persons needed the interaction with people who have challenges like themselves… this was limited since the curtailing of some of our activities, many don’t have the devices nor the online navigation skills to keep in touch.” (KI – Blind).
Community support was reported mainly from churches, neighbors, and family members. For some, these were the usual sources of support pre-COVID-19, while for others the help was stimulated by the epidemic.
Subordinate Theme: Coping Strategies
Vulnerable participants reported that staying busy, keeping their minds occupied through music, and attending church, helped them to cope with COVID-19. “…Pray a lot …Right through di day”; “ turn on the radio, listen music, play games on mi phone.” (Elderly urban participant). Other coping methods used by the elderly included exercise, gardening, weaving, and hand embroidery. Younger vulnerable persons reported resorting to Internet, social media, and other forms of technology as well as watching movies. “… mi just go pon social media and see what a gwaan… a little television but mostly the phone.” (Young person in a wheelchair).
There were reports of personal and emotional support from friends, family members, church members, and community leaders. “My younger family call and say aunty stay inside, wear you mask and suh on.” (Elderly participant). Personal and emotional support from families and agencies included paying for medications, visiting, calling by telephone, and distribution of care packages. “… we are in touch with the children and know their needs and concerns.” (KI – Blind).
Limitations
The risk communication referenced in this study was limited to those distributed between March and September 2020. Additionally, the findings articulate the views of the vulnerable groups included in this study and is not intended to reflect the views of all vulnerable groups
Discussion
The findings of this study suggest that risk communication was frequently shared and that vulnerable persons had access to and were able to act on the information provided. It is noteworthy that, of the 141 COVID-19 risk communication messages identified and analyzed in this study, 12 focused on the most vulnerable members of the community, leaving significant gaps especially for those who are mentally ill and the deaf. Agencies that serve the vulnerable were able to fill some of the gaps in communication by providing access to suitable formats and medium of communication or acted as intermediaries in implementing appropriate risk prevention measures. Risk communication research indicates that audience involvement aimed at identifying the needs of specific populations, including vulnerable groups, is an essential component of the response to epidemics.2,3 It is also clear that access to relief measures and mental health care of vulnerable groups needs to be given more prominence and should be based on participatory research.15,16 It is recommended that agencies that serve vulnerable persons be enabled through the MOHW and its stakeholders to provide official risk communication during health emergencies, through partnerships, collaboration, and capacity building. Vulnerable groups should systematically be involved in facilitating communication, including providing suggestions for adjusting risk communication to meet their specific needs.
Vulnerable participants signaled the essentialness of social contact for emotional and social support including goods and services for daily living given the reduced access to church, community members, and friends, during the pandemic. The reported barriers to access included being in a rural location, limited Internet service or digital devices, poor digital literacy, and limited connection to governmental or nongovernmental agencies that serve the specific vulnerability. Sharing information about barriers to information and services is vital to improving the responses of the government and nongovernmental sectors responsible for mounting the national COVID-19 response.17 Many support agencies were able to implement innovations to improve their ability to serve vulnerable groups, which is likely to foster competence in following the protocols. Thus, vulnerable persons now have new ways of accessing services that were not previously available to them. However, not all innovations were nationally available.
Issues of equity such as financial stressors and suitable communication media are often ignored.18,19 The economic fallout resulting from the pandemic was exacerbated for the vulnerable groups who expressed concerns about being the first to be let go by employers due to contraction of business resulting from the epidemic. Many lost income and did not qualify for some care initiatives as their sources of income and employment were often informal. In addition, the ability to go to work during the lockdown was a concern for the deaf community because of challenges communicating with enforcers of the lockdown orders. Considerations of the communication needs of the deaf community must be prioritized.20,21 Policy-makers and academics should give high regard for equity and inclusion when responding to epidemics.20,22 In the Jamaican context, more research is needed on the role of risk communication with specific research agendas set in conjunction with vulnerable populations.23 Findings should be incorporated in the production, dissemination, and evaluation of the risk communication output.
The findings of this study have been shared with the participating agencies.
Conclusions
Considering that the elderly and those with disabilities are at greater risk in times of crisis, the accessibility of targeted information was inadequate to provide universal access to health information and support for vulnerable persons regardless of location. This pandemic has highlighted the need to overcome structural inequalities that limit access to information and services for society’s more vulnerable groups.
Acknowledgments
This study was conceptualized by the Communications sub-group of the Essential National Health Research Committee convened by the Jamaica Ministry of Health and funded by PAHO/WHO Office for Jamaica, Bermuda and The Cayman Islands. The authors also acknowledge the valuable contributions of all the participants.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/dmp.2021.225.
click here to view supplementary material
Conflicts of Interest
The authors declare that there is no conflict of interest.
References
- 1.Srivastava KC, Shrivastava D, Chhabra KG, et al. Facade of media and social media during covid-19: a review. Int J Res Pharm Sci. 2020;11(Special Issue 1). doi: 10.26452/ijrps.v11iSPL1.2288. [DOI]
- 2.Steelman TA, McCaffrey S.Best practices in risk and crisis communication: implications for natural hazards management. Nat Hazards. 2012;65:683-705. doi: 10.1007/s11069-012-0386-z [DOI] [Google Scholar]
- 3.Palenchar MJ. Risk communication. In: Robert L. Heath ed. Encyclopedia of Public Relations. Vol. 1. Thousand Oaks: SAGE Publications, Inc; 2005:753-755. doi: 10.4135/9781412952545.n377 [DOI] [Google Scholar]
- 4.Xiang D, Kontos C, Veloudaki A, et al. Risk communication in the time of an epidemic or pandemic. An introduction to risk communication during pandemics and epidemics 2017 ASSET Paper Series 5. http://www.asset-scienceinsociety.eu/sites/default/files/paper_series_5_-_risk_communication_in_time_of_an_epidemic_or_pandemic.pdf. Accessed August 8, 2021.
- 5.World Health Organization. Communicating risk in public health emergencies. A WHO guideline for emergency risk communication (ERC) policy and practice https://www.who.int/news-room/q-a-detail/emergencies-risk-communication. Published January 10, 2018. Accessed February 2, 2021. [PubMed]
- 6.Ministry of Health & Wellness. Psychosocial support for persons affected by novel coronavirus 2019. A Protocol for care. 2020. www.moh.gov.jm/covid19/covid-19-resources-and-protocols. Accessed August 23, 2020.
- 7.International Long Term Care Policy Network. The COVID-19 long-term care situation in Jamaica. https://ltccovid.org/wp-content/uploads/2020/05/The-COVID-19-Long-Term-Care-situation-in-Jamaica-25-May-2020-1.pdf. Accessed August 9, 2021.
- 8.Azarpazhooh MR, Morovatdar N, Avan A, et al. COVID-19 pandemic and burden of non-communicable diseases: an ecological study on data of 185 countries. J Stroke Cerebrovasc Dis. 2020;29(9):105089. doi: 10.1016/j.jstrokecerebrovasdis.2020.105089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ejaz H, Abdullah A, Azza Z, et al. COVID-19 and comorbidities: deleterious impact on infected patients. J Infect Public Health 2020;13(12):1833-1839. doi: 10.1016/j.jiph.2020.07.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Park J.Unraveling the invisible but harmful impact of COVID-19 on deaf older adults and older adults with hearing loss. J Gerontol Soc Work. 2020;63(6-7):598-601. doi: 10.1080/01634372.2020.1799282 [DOI] [PubMed] [Google Scholar]
- 11.Lebrasseur A, Fortin-Bédard N, Lettre J, et al. Impact of COVID-19 on people with physical disabilities: a rapid review. Disabil Health J. 2021;14(1):101014. doi: 10.1016/j.dhjo.2020.101014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Turk MA, McDermott S.The COVID-19 pandemic and people with disability. Disabil Health J. 2020;13(3):100944. doi: 10.1016/j.dhjo.2020.100944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van Bavel JJ, Baicker K, Boggio PS, et al. Using social and behavioral science to support COVID-19 pandemic response. Nat Hum Behav. 2020;4(5):460-471. doi: 10.1038/s41562-020-0884-z [DOI] [PubMed] [Google Scholar]
- 14.Adhikari SP, Meng S, Wu YJ, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty. 2020;9(1):29. doi: 10.1186/s40249-020-00646-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bao Y, Sun Y, Meng S, et al. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395(10224):e37-e38. doi: 10.1016/S0140-6736(20)30309-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yao H, Chen JH, Xu YF.Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020;7(4):e21. doi: 10.1016/S2215-0366(20)30090-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Porat T, Nyrup R, Calvo RA, et al. Public health and risk communication during COVID-19-Enhancing psychological needs to promote sustainable behavior change. Front Public Health. 2020;8:573397. doi: 10.3389/fpubh.2020.573397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wieland ML, Asiedu GB, Lantz K, et al. Leveraging community engaged research partnerships for crisis and emergency risk communication to vulnerable populations in the COVID-19 pandemic. J Clin Transl Sci. 2020;5(1):e6. doi: 10.1017/cts.2020.47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abrams EM, Greenhawt M.Risk communication during COVID-19. J Allergy Clin Immunol Pract. 2020;8(6):1791-1794. doi: 10.1016/j.jaip.2020.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mesa Vieira C, Franco OH, Gómez Restrepo C, et al. COVID-19: the forgotten priorities of the pandemic. Maturitas. 2020;136:38-41. doi: 10.1016/j.maturitas.2020.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clark-Ginsberg A, Petrun Sayers EL.Communication missteps during COVID-19 hurt those already most at risk. J Conting Crisis Manag. 2020. doi: 10.1111/1468-5973.12304 [DOI]
- 22.Grote H, Izagaren F.Covid-19: the communication needs of D/deaf healthcare workers and patients are being forgotten. BMJ. 2020;369:m2372. doi: 10.1136/bmj.m2372. [DOI] [PubMed] [Google Scholar]
- 23.Wang Z, Tang K.Combating COVID-19: health equity matters. Nat Med. 2020;26(4):458. doi: 10.1038/s41591-020-0823-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/dmp.2021.225.
click here to view supplementary material