Abstract
Background
The COVID-19 pandemic has affected our lives in numerous ways. How youth have been impacted by the pandemic and which preexisting factors best relate to COVID-19 responses are of high importance for effective identification and treatment of those most vulnerable. Youth with pre-pandemic mental health difficulties such as attention-deficit/hyperactivity disorder (ADHD) could be at risk for worse well-being during and after the pandemic.
Methods
The current study tested potential risk factors (i.e., pre-pandemic mental health, age, and parental education) and their relationship to family experiences during early months of the COVID-19 pandemic. Participants were previously enrolled in an ongoing, yearly longitudinal study examining the relationship between mental health and executive functions in youth. Families with 1–4 annual pre-pandemic lab visits filled out an online COVID-19 survey in May–July 2020 to assess how the pandemic impacted their well-being (n = 135 youth).
Results
Youth pre-pandemic mental health difficulties, especially ADHD symptoms, related to worse well-being during the early pandemic. Trajectories of recent ADHD symptoms over time also predicted cognitive difficulties during the pandemic. We found that youth age was a strong predictor of pandemic response, with younger youth showing fewer negative responses. Parental education level buffered family economic impact during early COVID-19. Families showed synchrony in their pandemic responses.
Conclusions
Pre-pandemic ADHD severity and slope, youth age, and parental education (a proxy for socioeconomic status) were risk factors that influenced youth or family well-being early in the COVID-19 pandemic; this information can help identify those who may need more community and educational support.
Keywords: ADHD, Adolescent, COVID-19, Longitudinal, Mental health, Parent education
SEE COMMENTARY ON PAGE 244
COVID-19 was declared a pandemic by the World Health Organization in March of 2020. The remainder of 2020 posed significant challenges for youth and their families, with upheaval in numerous aspects of life, potentially impacting well-being. Well-being can refer to life satisfaction and a presence of overall positive emotions and moods (1). Given that higher well-being relates to better perceived health and fewer risky behaviors (2), identifying pre-pandemic factors that predict pandemic well-being can provide insights for interventions and inform resource allocation in future emergencies. The current study examined potential pre-pandemic risk factors that could contribute to worse well-being in youth during the early months of COVID-19, including youth mental health, youth age, and parental education.
Adverse life events that occur during childhood and adolescence, such as those potentially induced by the COVID-19 pandemic, impact physical and mental well-being throughout the life span (3). Children who experience a high level of early-life stress have shown deficits in cognitive functioning, which may persist into adulthood (4). Youth who live through a disaster can experience posttraumatic stress (5), higher levels of depression, anxiety, and panic disorder-related symptoms (6). When presented with a stressful live event such as the COVID-19 pandemic, children may have fewer coping and communication skills than adults, raising odds of trauma and distress (7). Knowing that adverse life events during childhood have potential for broad impacts on children’s health (during childhood and beyond), it is thus important to consider how the COVID-19 pandemic is affecting different aspects of youth well-being, by sampling their responses to the evolving situation.
Recent examination of general well-being in youth during COVID-19 found that 40% of parents indicated that their child was in distress during the pandemic (8). Similarly, parents reported higher rates of inattention, clinginess, irritability, and worry in their children during the pandemic (9). It has been speculated that youth with special needs or a preexisting mental illness prior to the pandemic are more vulnerable to distress during the COVID-19 pandemic (7); however, it is important to identify more specifically what mental health difficulties are risk factors for worse pandemic responses in order to better improve youth outcomes. Previous COVID-19 studies have largely focused on youth anxiety- and depression-related symptoms (10, 11, 12, 13, 14); however, youth with high attention-deficit/hyperactivity disorder (ADHD) burden before the pandemic might be particularly susceptible to the adverse effects of the pandemic. Childhood ADHD is predictive of both short- and long-term negative impacts on well-being. While childhood ADHD is predictive of worse educational outcomes in childhood (15, 16, 17, 18, 19), it is also linked to lower quality of life in adulthood (20), including worse occupational, economic, and social outcomes (21). The additional stress, unpredictability, and break in routine brought on by the COVID-19 pandemic could enhance existing problems for those with high levels of attention difficulties and predispose them to worse well-being during COVID-19. Examining preexisting factors such as ADHD symptomatology that influence general well-being may be crucial for understanding variability in youth response during the pandemic.
Additional risk factors for distress during the pandemic in youth include experiencing loss of a family member, having fewer resources within their family, having more exposure to mass media coverage on the pandemic, or having elevated stress because of changes in routine or living conditions (22). Having lower socioeconomic status (SES) is also linked to worse well-being during the COVID-19 pandemic. Lower-income and lower-middle income parents reported more financial hardships due to the pandemic (23) and more emotional distress for themselves and their children (24).
The present study used up to 4 years of annual in-person demographic and mental health data on 135 children and their families to inform our understanding of their responses to an online survey of overall well-being during early COVID-19 (May–July 2020). We examined 3 key potential pre-pandemic influences—mental health (especially ADHD symptoms), age, and socioeconomic measures (i.e., parental education levels)—on emotional, cognitive, and social aspects of youth self-report of well-being during the early days of the COVID-19 pandemic.
Methods and Materials
Participants
Participants in this report included 135 youth (mean age = 15.17 years, range = 9.4–22.1, 61 female, 70 male, 3 nonbinary, 1 prefer not to say), and 78 parents (mean age = 46.57, range = 32–67, 72 female) from 90 unique families from greater Austin, Texas. An additional 6 parents filled out a COVID-19 survey, but their child did not, and thus they were excluded from this set of analyses. At the time of the COVID-19 impacts survey, 30 youth were aged 18 or above, and 105 youth were younger than 18. All participants had at least 1 pre-pandemic time point of mental health and demographic measures from their participation in an ongoing, multiyear longitudinal study examining mental health (see Table S1 for comparison with those in that study who did not complete a COVID-19 survey). This was a community sample, over-recruited for mental health diagnoses; 72 youth had at least 1 mental health diagnosis, primarily ADHD (n = 59) (Table S2), and 34 youth reported being on psychotropic medication. All youth clinical diagnoses were reported by the parent at the most recent in-laboratory visit.
A subsample of participants (n = 113, mean age = 15.53 years, range = 9.9−22.1 years) who had at least 2 annual (but ranging from 2 to 4) pre-pandemic time points of ADHD symptom burden measures were used for a test of ADHD symptom burden change before COVID-19. For income, race, and ethnicity of the overall sample, please see Table S1.
All protocols were approved by the University of Texas at Austin Institutional Review Board. The pre-pandemic longitudinal study required participants to come into the laboratory for their visit; however, all COVID-19 measures were collected online through surveys. Parents provided informed consent, and youth provided informed assent before their participation in the study. Participating parents and youth were compensated at each time point.
Materials
Pre-COVID-19 Measures
Before the start of the COVID-19 pandemic, participants completed a battery of mental health measures in the laboratory (Table 1). Questionnaires were completed between November 13, 2016, and March 3, 2020 (Figure S1). We primarily used mental health data from each participant’s most recent in-laboratory visit for our analyses (ranging from year 1 to year 4 of data collection) (see Figure S2), but for longitudinal analyses, we compared using 2 to 4 available years of a participant’s mental health data (n = 113).
Table 1.
Pre-pandemic In-Laboratory Mental Health Measures Used to Derive Youth Composite Scores: Mental Health Burden and ADHD Symptom Burden
| Measure Name | Report Type | What It Measures | Sample Mean Most Recent POMS Score (n = 135) | Sample Range of Most Recent POMS Score (n = 135) |
|---|---|---|---|---|
| CBCL | Parent report on youth <18 years | Behavioral and emotional problems (internalizing and externalizing difficulties) | 0.13 (n = 124) | Min = 0 Max = 0.48 |
| ASR | Youth self-report >18 years | Internalizing/externalizing problems | 0.27 (n = 11) | Min = 0.15 Max = 0.43 |
| Conners-3 Self-Report Short Version | Youth self-report <18 years | ADHD symptomatology and common comorbid problems | 0.28 (n = 120) | Min = 0 Max = 0.72 |
| CAARS Short Version | Youth self-report >18 years | Adult ADHD symptomatology or related problems | 0.35 (n = 15) | Min = 0.18 Max = 0.58 |
| Conners-3 Parent Short Version | Parent report on youth <18 years | ADHD symptomatology and common comorbid problems | 0.27 (n = 124) | Min = 0 Max = 0.84 |
ADHD, attention-deficit/hyperactivity disorder; ASR, Adult Self-Report; CAARS, Conners’ Adult ADHD Rating Scale; CBCL, Child Behavior Checklist; Max, maximum; Min, minimum; POMS, percent of maximum scaling.
Percent of maximum scaling (POMS) score [(the participant’s score − the minimum possible score)/(the maximum possible score − the minimum possible score)] was calculated for each pre-COVID-19 mental health measure. For all mental health measures, a higher score indicated a higher level of symptom burden. A mental health symptom burden variable was derived from the POMS score of the parent report Child Behavior Checklist (25) if participants were younger than 18 years, and the POMS score of the Adult Self-Report (26) otherwise. A self-report ADHD symptom burden variable was derived from the POMS score of the Conners-3 self-report (27) if participants were younger than 18 years at the time of its completion, and the POMS score of the Conners’ Adult ADHD Rating Scale self-report (28) otherwise. Parent report of youth ADHD symptom burden was derived from the POMS score of the Conners-3 parent report (27) about the youth (n = 124).
COVID-19 Impact Measures
The parent and youth COVID-19 impact measures were completed separately online between May 21, 2020, and July 22, 2020. Youth completed a subset of the COVID-19 Adolescent Symptom and Psychological Experience Questionnaire (CASPE) (29). A total subscore was calculated for each of the CASPE subcategories for each individual (emotional, cognitive, social, and direct experience related to COVID-19) (Table 2). Higher scores for the emotional, cognitive, and direct experiences subcategories indicated greater impact on well-being from COVID-19, and a higher score in the social subcategory indicated more time spent socializing online. z scores were computed for each CASPE subcategory.
Table 2.
CASPE Subcategories and Scoring
| Subcategories | No. of Items in Subcategory | Range of Raw Score Per Subcategory | Example Item | Scoring of Items in Subcategory |
|---|---|---|---|---|
| Cognitive Well-being | 3 | Min = 12 Max = 61 |
In the past 7 days, including today, to what extent have you experienced the following: zoning out. | Items about negative cognitive outcomes were coded on a scale of 1 (very slightly or not at all) to 5 (extremely), and positive items were reverse coded. |
| Emotional Well-being | 7 | Min = 28 Max = 140 |
The COVID-19 outbreak has changed and disrupted many existing plans. In the past 7 days, including today, how stressful do you find these disruptions to be? | Items about negative emotional outcomes were coded on scale of 1 (very slightly or not at all/not at all) to 5 (extremely/a great deal), and positive items were reverse coded. |
| Social Well-being | 2 | Min = 2 Max = 10 |
Since your school has closed, how often do you talk/chat with friends online (including on your cell phone, on social media, or through online gaming)? | Items were scored so that spending more time socializing resulted in a higher score, and spending less time socializing resulted in a lower score. |
| Direct Experiences Related to COVID-19 | 11 | Min = 6 Max = 41 |
Overall, how much has the COVID-19 outbreak, and the resulting changes to daily life, affected your life in a negative/positive way? | More exposure to infections, death, and hardships during the COVID-19 pandemic resulted in a higher score. |
The CASPE survey was used to assess youth responses to the COVID-19 pandemic. Subcategories reflect different aspects of well-being that could be impacted by the COVID-19 pandemic. CASPE, Covid-19 Adolescent Symptom and Psychological Experience Questionnaire; Max, maximum; Min, minimum.
Parents completed a subset of the Epidemic-Pandemic Impacts Inventory (EPII) (30). A total score was calculated for each of the EPII subcategories and z-scored across the sample (Table 3). A higher score for each subcategory on the EPII indicated greater impact from the pandemic.
Table 3.
EPII Subcategories and Scoring
| Subcategories | No. of Items in Subcategory | Range of Raw Score Per Subcategory | Example Item | Scoring of Items in Subcategory |
|---|---|---|---|---|
| Parent Work and Employment Since COVID-19 | 11 | Min = 0 Max = 22 |
Had to continue to work even though in close contact with people who might be infected (e.g., customers, patients, co-workers). | Check Yes (Me) if you were impacted: 1 point Check Yes (Person in Home) if another person (or people) in your home were impacted: 1 point |
| Parent Home Life Since COVID-19 | 11 | Min = 0 Max = 22 |
More conflict with a child or harsher in disciplining a child or children. | Check Yes (Me) if you were impacted: 1 point Check Yes (Person in Home) if another person (or people) in your home were impacted: 1 point |
| Parent Social Activities Since COVID-19 | 9 | Min = 0 Max = 18 |
Unable to visit loved one in a care facility (e.g., nursing home, group home). | Check Yes (Me) if you were impacted: 1 point Check Yes (Person in Home) if another person (or people) in your home were impacted: 1 point |
| Parent Economic Situation Since COVID-19 | 3 | Min = 0 Max = 6 |
Unable to pay important bills like rent or utilities. | Check Yes (Me) if you were impacted: 1 point Check Yes (Person in Home) if another person (or people) in your home were impacted: 1 point |
| Parent Emotional and Physical Health and Well-being in COVID-19 | 13 | Min = 0 Max = 39 |
Unable to access mental health treatment or therapy. | Check Yes (Me) if you were impacted: 1 point Check Yes (Child in Home) if a child in the home was impacted: 1 point Check Yes (Adult in Home) if another adult in the home was impacted: 1 point |
| Parent Physical Distancing and Infection History Since COVID-19 | 13 | Min = 0 Max = 26 |
Isolated or quarantined due to possible exposure to COVID-19. | Check Yes (Me) if you were impacted: 1 point Check Yes (Person in Home) if another person (or people) in your home were impacted: 1 point |
| Parent Positive Change Since COVID-19 | 18 | Min = 0 Max = 36 |
More quality time with a partner or spouse. | Check Yes (Me) if you were impacted: 1 point Check Yes (Person in Home) if another person (or people) in your home were impacted: 1 point |
EPII survey was used to assess parent responses to the COVID-19 pandemic. Subcategories reflect different aspects of well-being that could be impacted by the COVID-19 pandemic.
EPII, Epidemic-Pandemic Impacts Inventory; Max, maximum; Min, minimum.
Demographic Measures
Participants’ self-reported age and gender information were collected at the time of the COVID-19 Impact Survey. Participants’ racial and ethnic information and SES measures, including father’s and mother’s education levels, were collected at their most recent pre-pandemic in-laboratory visit.
Statistical Approach
All results were corrected using false discovery rate (31), unless otherwise noted. For the number of false discovery rate corrections per analysis, see Table S3.
Comparisons Using the Most Recent Pre-pandemic Time Point
We used linear regression models to test how pre-pandemic composite mental health burden and ADHD symptom burden scores related to youth COVID-19 outcomes on the CASPE subcategories while accounting for youth age. We used linear regression to test whether youth age at the time of the COVID-19 survey predicted scores on subcategories of the CASPE. Parents’ education level was examined separately (mother’s and father’s education level) and together by calculating a mean parental education score. We used linear regression to examine whether education levels predicted parent responses on the EPII survey and whether parent education levels predicted youth CASPE responses.
In addition, we examined whether parents and youth in a household were in sync during the pandemic. We used linear regression to examine whether parent scores on the EPII subscales predicted youth outcomes on the CASPE survey. For our approach to sibling data, internal validity measures on the CASPE subscores, and quality assurance of all models please see Supplemental Methods.
Comparisons Using Pre-pandemic ADHD Trajectories
A subset of participants completed the ADHD symptom burden measure (n = 113) during at least 2 annual pre-pandemic visits but ranged from having 2 to 4 pre-pandemic time points. We quantified the trajectory of participants’ mental health symptoms over the years using the ADHD symptom burden composite self-report measure. To identify a participant’s mental health trajectory before the pandemic (i.e., slope of ADHD symptom burden before the pandemic), we used a random slope model to calculate the slope of ADHD symptom burden across time points per participant. We then modeled the ADHD symptom burden slope predicting COVID-19 outcomes measures (CASPE), while controlling for level of ADHD symptom burden at time point 1.
Results
Mental Health and COVID-19 Reactions in Youth
ADHD Youth Self-report and Parent Report
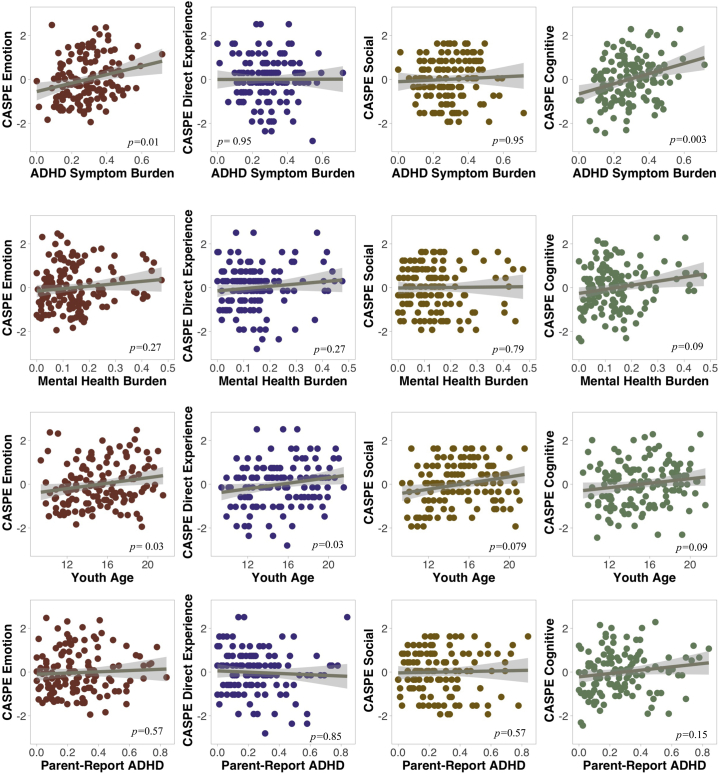
We examined whether pre-pandemic ADHD symptom burden influenced well-being during early stages of the pandemic (Figure 1). Youth and parent report of pre-pandemic youth ADHD burden was correlated at r = 0.44. Youth self-report of ADHD burden from the participant’s most recent pre-COVID-19 laboratory visit significantly contributed to worse cognitive experiences during the COVID-19 pandemic (β = 2.22, R2 = 0.10, p = .003) and poorer emotional experiences (β = 1.81, R2 = 0.10, p = .01). See Table S3 for nonsignificant comparisons.
Figure 1.
Predictors of youth COVID-19 Adolescent Symptom and Psychological Experience Questionnaire (CASPE) subcategories. Graphs show how youth self-report attention-deficit/hyperactivity disorder (ADHD) symptom burden, mental health burden, age, and parent report of child ADHD symptom burden relate to the 4 z-scored CASPE subcategories (emotion, direct experience, social, cognitive). Regression analyses of youth self-report ADHD symptom burden, mental health burden, and parent report of child ADHD symptom burden controlled for age (Figure 1 shows raw data points, not controlled for age). p values reflect false discovery rate multiple comparison correction.
Parent report of child ADHD symptom burden for youth <18 years before the pandemic was significant before multiple comparison correction for the cognitive subcategory on the CASPE survey (β = 0.97, R2 = 0.06, uncorrected p = .04) but did not survive multiple comparison correction (adjusted p = .15). See Table S3 for nonsignificant comparisons.
Overall Mental Health Symptom Burden
Mental health symptom burden also contributed to poorer cognitive well-being (after controlling for youth age) before multiple comparison correction (β = 1.83, R2 = 0.06, uncorrected p = .02; adjusted p = .09) (Figure 1). See Table S3 for nonsignificant comparisons.
Age Relationships to COVID-19 Reactions in Youth
We tested whether youth age predicted well-being during early stages of the COVID-19 pandemic (Figure 1). Age significantly predicted emotional (β = 0.07, R2 = 0.04, p = .03) and direct (β = 0.07, R2 = 0.05, p = .03) experiences related to COVID-19, such that older youth reported worse emotional well-being and more direct experiences related to COVID-19. Youth age also marginally predicted the CASPE social subcategory (β = 0.05, R2 = 0.03, p = .079), such that older youth had a higher score on the CASPE social well-being subcategory, meaning that they engaged more socially online than younger participants.
Parent Education Levels and COVID-19 Outcomes
We examined how parent education level, a proxy for SES, impacted parent and youth well-being during the COVID-19 pandemic. Parent mean education level significantly predicted their score on the EPII COVID-19 economic situation subscale (β = −0.13, R2 = 0.06, p = .04), such that higher education across parents related to less negative economic impact during the early stages of the pandemic. Father’s education level also significantly predicted parent scores on the EPII COVID-19 economic situation subscale (β = −0.13, R2 = 0.09, p = .03), such that higher levels of father’s education related to less negative economic impact. For results that did not survive multiple comparison correction, see Table S3.
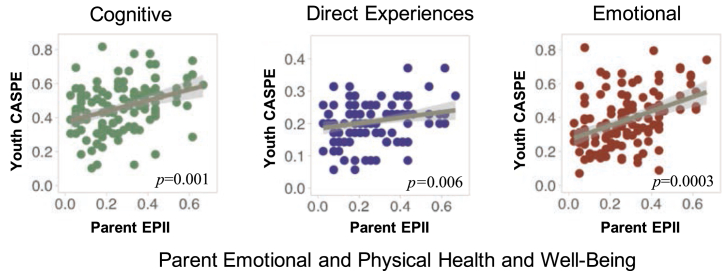
Synchrony Between Parent and Youth COVID-19 Reactions
To examine whether parents and their youth had similar experiences during the pandemic, we compared parent responses on the EPII with their children’s responses on the CASPE. Parent self-reported EPII scores on the emotional and physical health and well-being in COVID-19 subscale were significantly related with their children’s cognitive (β = 0.35, R2 = 0.14, p = .001), emotional (β = 0.41, R2 = 0.19, p = .0003), and direct (β = 0.30, R2 = 0.10, p = .006) experiences related to COVID-19, such that parents with worse well-being during the pandemic also had children with worse well-being and more direct experiences related to COVID-19 (Figure 2). We ran the same analysis with one randomly selected child per family instead of averaging across siblings in a family, and the significance and direction of the results did not change.
Figure 2.
Parent and child well-being are in sync. Graphs show how parent emotional and physical health and well-being (Epidemic-Pandemic Impacts Inventory [EPII] subcategory) is related to youth cognitive and emotional well-being and the amount of direct experiences with the pandemic that youth endorsed during early stages of COVID-19. CASPE, COVID-19 Adolescent Symptom and Psychological Experience Questionnaire.
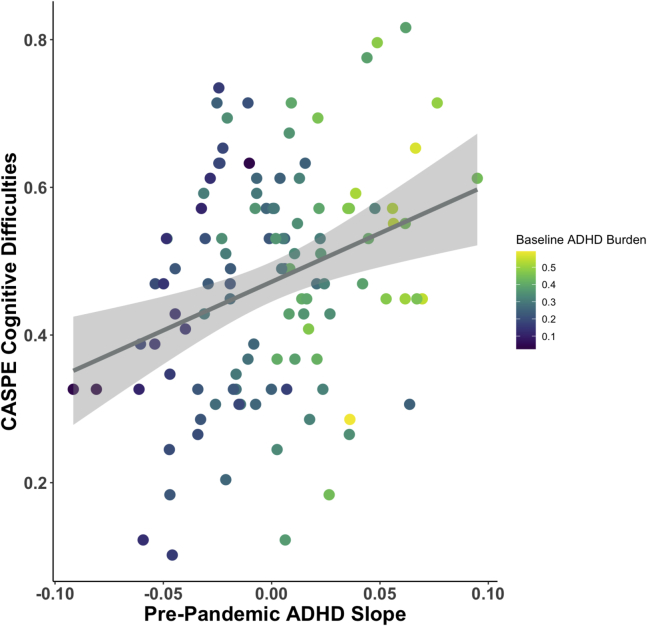
Longitudinal Analysis of Relationship Between ADHD and Youth COVID-19 Outcomes
We next investigated the relationships between self-report ADHD ratings and COVID-19 responses in a subsample of youth participants with at least 2 time points of pre-pandemic mental health data. We found that the slope of pre-pandemic self-report ADHD symptom burden related to CASPE cognitive well-being (β = 1.74, R2 = 0.10, p = .009) while controlling for baseline (time point one) levels of ADHD symptom burden, such that those with larger (worsening) ADHD symptom burden slopes had worse cognitive well-being during the pandemic (Figure 3). Those whose symptom burden was getting worse were the ones who experienced more cognitive distress during early stages of the pandemic, controlling for initial ADHD severity. ADHD symptom burden slope did not predict the CASPE emotional well-being subcategory.
Figure 3.
Pre-pandemic attention-deficit/hyperactivity disorder (ADHD) slope predicts cognitive difficulties during the pandemic. Those with bigger increases in ADHD symptom burden (larger, positive slopes) between their 2 to 4 pre-pandemic visits had higher scores on the COVID-19 Adolescent Symptom and Psychological Experience Questionnaire (CASPE) cognitive well-being subcategory (i.e., worsening symptom burden during pre-pandemic time points related to more cognitive difficulties during early stages of the pandemic), even after controlling for baseline levels of ADHD burden from time point 1.
Discussion
Preexisting Mental Health Difficulties Make Youth More Vulnerable
Previous research suggests that youth with preexisting mental health difficulties might be more susceptible to experiencing worse mental health during the COVID-19 pandemic. Most of the present research on pre-pandemic mental health and responses to the COVID-19 pandemic in youth have focused on anxiety and depression symptoms (10,11); however, knowledge is more limited as to how ADHD symptomatology related to early pandemic well-being (32,33). We found that higher levels of pre-pandemic ADHD symptomatology related to worse reports of cognitive and emotional well-being by youth during early stages of the pandemic. The negative cognitive impact of COVID-19 was more strongly related to child self-report than parent report of pre-pandemic attention problems. This impact was largely specific to ADHD symptoms, as our general mental health measure had a weaker effect. ADHD is known to impact well-being for youth throughout their life span (19, 20, 21); the added stress of coping with sudden lifestyle and educational changes due to the pandemic could be particularly burdensome for youth and families with ADHD.
The impact of ADHD on cognitive experiences during the pandemic was not limited to the most recent data. Self-report of worsening ADHD symptoms over 2 to 4 years before the pandemic related to worse cognitive well-being during early stages of the pandemic, even after controlling for baseline levels of ADHD symptom burden at year 1. These results suggest that those perceiving worsening attention difficulties were also less equipped to deal with the sudden stress and lifestyle changes brought on by the pandemic. These results suggest that both recent ADHD symptoms and recent pre-pandemic changes in the severity of these issues have an impact on how well one responds to the pandemic.
Asking youth about cognitive experiences during the pandemic inherently aligns well with mental health surveys from pre-pandemic times (e.g., one CASPE cognitive question: how often in the last 7 days have you had racing thoughts?). Thus, the concordance between pre-pandemic ADHD symptoms and early pandemic cognitive difficulties highlight the persistence of attention difficulties many youth experienced both before and during the early pandemic. While ADHD is often characterized as a disorder of attention difficulties, our ADHD symptom burden measure considers many aspects of ADHD (inattention, hyperactivity/impulsivity, family and peer relations, learning problems, defiance/aggression). Even with some degree of overlap between the pre-pandemic Conners-3 and pandemic CASPE measures, it is still interesting that those with higher levels of pre-pandemic ADHD burden were the ones who reported higher scores on the CASPE cognitive well-being subcategory. It is reasonable to believe that those who had lower levels of ADHD burden before the pandemic could report higher levels of cognitive distress during a life-altering stressful event, such as COVID-19, because of the abrupt shift in day-to-day function for everyone. Having high levels of ADHD burden should not be considered a precursor to experiencing cognitive difficulties during a pandemic. Yet, we find that those experiencing prior difficulties are also those most vulnerable to experiencing cognitive and emotional difficulties in the pandemic, and that these difficulties were similar across family members. Future studies should probe the family circumstances that related the most to ongoing difficulties both during and after the pandemic to see whether these results persist.
Older Youth Were More Vulnerable to Early Pandemic Impacts
We examined whether age related to youth well-being during the pandemic. Older youth experienced worse emotional outcomes and encountered more direct experiences with the pandemic but also appeared to socialize online at a higher rate than younger youth. These results are consistent with previous research on college students that suggests that they experienced worse well-being and mental health during the COVID-19 pandemic than older adults (34, 35, 36). Older youth may be more aware of the consequences of the COVID-19 pandemic on our society, as they have likely had more direct encounters with the COVID-19 pandemic. They may not stay at their parents’ home and are out in the world more frequently, because of either work or schooling circumstances; they may be less sheltered from COVID-19 impacts by their families, despite our findings of similar experiences across family members.
Parent Education Predicts COVID-19 Economic Challenges
We examined the role of parent education level, as a proxy for socioeconomic status, on COVID-19 related outcomes and found that higher levels of parent education were predictive of higher levels of economic well-being during the early stages of the pandemic. These results are consistent with previous COVID-19 studies showing that lower SES parents experienced more financial hardship during the pandemic (23). Our CASPE relations to parental education early in the pandemic were not significant, unlike previous work (37), suggesting that SES impacts need to be further interrogated, possibly with a more diverse economic sample or over a longer pandemic timeframe.
Family COVID-19 Experiences Are in Sync
We found synchrony in well-being occurring within households. Parents who reported worse emotional and physical well-being during early stages of the COVID-19 pandemic had youth who also reported worse emotional and cognitive well-being, as well as more direct experiences with the pandemic. This suggests that parents’ responses to the pandemic influence the child’s response to the pandemic, or vice versa, and that similar genetic and environmental circumstances within a family lead parents and youth to respond in a similar manner. This is consistent with pre-pandemic literature that suggests that youth well-being is heavily influenced by family well-being (38), and more specifically, that a mother’s physical and psychological well-being influences a child’s well-being (39).
More broadly, mother’s depression symptoms have been found to be in synchrony with youth nonclinical levels of depression, even through changes in mother’s treatment response (40). This finding and our results suggest that when implementing interventions surrounding COVID-19, treating one family member may help the whole family. Our strong synchrony results were collected during a unique time when families spent more time together than pre-COVID-19 and were perhaps unable to rely on other support systems (i.e., friends, coworkers). Future work could test to see whether pre-pandemic to early pandemic synchrony in families differs, and whether this synchrony persists past early stages of the pandemic, when lockdown measures abated.
Limitations
A limitation of our work is that our pre-pandemic mental health measures were not collected during the pandemic; we collected the EPII and CASPE as brief measures of well-being, which are (as yet) unpublished measures created for the current pandemic. We chose the EPII and CASPE instead of the lengthy original measures, because we were interested in COVID-19 stressors and responses in our participating families, rather than mental health (e.g., ADHD symptomatology) change per se, and for potential pooling of consistent COVID-19 measures across different labs. Given the novelty of the EPII and CASPE (as they were created specifically for the COVID-19 pandemic), the validity of these measures as psychometrics has yet to be established. More research is needed on how mental health changed from pre-pandemic to pandemic time and, specifically, how ADHD symptomatology changed from pre-pandemic to pandemic time.
In addition, our selections from the CASPE social subcategory only consisted of 2 items; future research should incorporate a wider range of items to obtain a more comprehensive assessment of how the COVID-19 pandemic affects youth social well-being (33). Finally, we used continuous measures of mental health and ADHD burden in this community sample, rather than the presence or absence of diagnostic labels, to study the impact of mental health difficulties on pandemic experiences. Researchers with pre-pandemic measures of a particular diagnostic group could interrogate specific diagnoses and COVID-19 well-being in more detail. We now have a second time point of COVID data and families returning for in-lab collections; these data could enhance and clarify these results.
Conclusions
We tested pre-pandemic influences on youth and family well-being during early parts of the COVID-19 pandemic. Worse reactions to the pandemic were associated with higher pre-pandemic ADHD burden, older youth age, and lower parental education. ADHD symptoms and their recent trajectory related to worse early COVID-19 cognitive and emotional responses in youth, similar to a growing body of work highlighting the interaction of the pandemic with symptoms of anxiety and depression. Synchrony was seen across child and parent responses, which suggests improving parental well-being may improve youth outlook. Pre-pandemic data help us understand diverse experiences of families and youth during the pandemic. A nuanced understanding of the myriad of contributors to youth well-being early in COVID-19 may help identify those at highest risk for poor outcomes and help to target specific interventions or resources.
Acknowledgments and Disclosures
This study was supported by the Brain & Behavior Research Foundation Young Investigator Award and University of Texas start-up funds (to JAC).
We thank all of the families who have participated in this research. We also thank Tehila Nugiel and Annie Zheng for significant help with the longitudinal study data collection and design. We would like to acknowledge all of the (primarily undergraduate) research assistants who aided in collection of the COVID-19 survey data and/or pre-pandemic data collections over the past several years, including Alice Aizza, Phoebe Anderson, Jessica Berry, Nikita Batra, Kinsey Bickham, Delayna Bradshaw, Janchira Charoenworawat, Andre Ferreira, Neyra Garcia, AnnaCarolina Garza, Anushka George, Ashley Jacob, Kyle Katigbak, Joy Lee, Kumail Mahesri, Miriam Ortega, Lea Ann Thomas, Madison Tuazon, Dr. Khushboo Verma, Marie Vu, and Tiffany Wang.
The authors report no biomedical financial interests or potential conflicts of interest.
Footnotes
Supplementary material cited in this article is available online at https://doi.org/10.1016/j.bpsgos.2021.08.003.
Supplementary Material
References
- 1.Diener E. Subjective well-being. The science of happiness and a proposal for a national index. Am Psychol. 2000;55:34–43. [PubMed] [Google Scholar]
- 2.Hoyt L.T., Chase-Lansdale P.L., McDade T.W., Adam E.K. Positive youth, healthy adults: Does positive well-being in adolescence predict better perceived health and fewer risky health behaviors in young adulthood? J Adolesc Health. 2012;50:66–73. doi: 10.1016/j.jadohealth.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Middlebrooks J.S., Audage N.C. National Center for Injury Prevention and Control of the Centers for Disease Control and Prevention; College Park: 2008. The Effects of Childhood Stress on Health Across the Lifespan. [Google Scholar]
- 4.Hedges D.W., Woon F.L. Early-life stress and cognitive outcome. Psychopharmacology. 2011;214:121–130. doi: 10.1007/s00213-010-2090-6. [DOI] [PubMed] [Google Scholar]
- 5.Furr J.M., Comer J.S., Edmunds J.M., Kendall P.C. Disasters and youth: A meta-analytic examination of posttraumatic stress. J Consult Clin Psychol. 2010;78:765–780. doi: 10.1037/a0021482. [DOI] [PubMed] [Google Scholar]
- 6.Kar N. Psychological impact of disasters on children: Review of assessment and interventions. World J Pediatr. 2009;5:5–11. doi: 10.1007/s12519-009-0001-x. [DOI] [PubMed] [Google Scholar]
- 7.Imran N., Zeshan M., Pervaiz Z. Mental health considerations for children & adolescents in COVID-19 Pandemic. Pak J Med Sci. 2020;36:S67–S72. doi: 10.12669/pjms.36.COVID19-S4.2759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosen Z., Weinberger-Litman S.L., Rosenzweig C., Rosmarin D.H., Muennig P., Carmody E.R., et al. Anxiety and distress among the first community quarantined in the U.S due to COVID-19: Psychological implications for the unfolding crisis. PsyArXiv. 2020 doi: 10.31234/osf.io/7eq8c. [DOI] [Google Scholar]
- 9.Jiao W.Y., Wang L.N., Liu J., Fang S.F., Jiao F.Y., Pettoello-Mantovani M., Somekh E. Behavioral and emotional disorders in children during the COVID-19 epidemic. J Pediatr. 2020;221:264–266.e1. doi: 10.1016/j.jpeds.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xie X., Xue Q., Zhou Y., Zhu K., Liu Q., Zhang J., Song R. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. 2020;174:898–900. doi: 10.1001/jamapediatrics.2020.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barendse M., Flannery J.E., Cavanagh C., Aristizabal M., Becker S.P., Berger E., et al. Longitudinal change in adolescent depression and anxiety symptoms from before to during the COVID-19 pandemic: A collaborative of 12 samples from 3 countries. PsyArXiv. 2021 doi: 10.31234/osf.io/hn7us. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pan K.Y., Kok A.A.L., Eikelenboom M., Horsfall M., Jörg F., Luteijn R.A., et al. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: A longitudinal study of three Dutch case-control cohorts. Lancet Psychiatry. 2021;8:121–129. doi: 10.1016/S2215-0366(20)30491-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gassman-Pines A., Ananat E.O., Fitz-Henley J., 2nd COVID-19 and parent-child psychological well-being. Pediatrics. 2020;146 doi: 10.1542/peds.2020-007294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patrick S.W., Henkhaus L.E., Zickafoose J.S., Lovell K., Halvorson A., Loch S., et al. Well-being of parents and children during the COVID-19 pandemic: A national survey. Pediatrics. 2020;146 doi: 10.1542/peds.2020-016824. [DOI] [PubMed] [Google Scholar]
- 15.Biederman J., Faraone S., Milberger S., Guite J., Mick E., Chen L., et al. A prospective 4-year follow-up study of attention-deficit hyperactivity and related disorders. Arch Gen Psychiatry. 1996;53:437–446. doi: 10.1001/archpsyc.1996.01830050073012. [DOI] [PubMed] [Google Scholar]
- 16.Barry T.D., Lyman R.D., Klinger L.G. Academic underachievement and attention-deficit/hyperactivity disorder: The negative impact of symptom severity on school performance. J Sch Psychol. 2002;40:259–283. [Google Scholar]
- 17.Hinshaw S.P. Externalizing behavior problems and academic underachievement in childhood and adolescence: Causal relationships and underlying mechanisms. Psychol Bull. 1992;111:127–155. doi: 10.1037/0033-2909.111.1.127. [DOI] [PubMed] [Google Scholar]
- 18.Fergusson D.M., Horwood L.J., Lynskey M.T. The effects of conduct disorder and attention deficit in middle childhood on offending and scholastic ability at age 13. J Child Psychol Psychiatry. 1993;34:899–916. doi: 10.1111/j.1469-7610.1993.tb01097.x. [DOI] [PubMed] [Google Scholar]
- 19.Schiavone N., Virta M., Leppämäki S., Launes J., Vanninen R., Tuulio-Henriksson A., et al. ADHD and subthreshold symptoms in childhood and life outcomes at 40 years in a prospective birth-risk cohort. Psychiatry Res. 2019;281:112574. doi: 10.1016/j.psychres.2019.112574. [DOI] [PubMed] [Google Scholar]
- 20.Yang H.N., Tai Y.M., Yang L.K., Gau S.S.F. Prediction of childhood ADHD symptoms to quality of life in young adults: Adult ADHD and anxiety/depression as mediators. Res Dev Disabil. 2013;34:3168–3181. doi: 10.1016/j.ridd.2013.06.011. [DOI] [PubMed] [Google Scholar]
- 21.Klein R.G., Mannuzza S., Olazagasti M.A.R., Roizen E., Hutchison J.A., Lashua E.C., Castellanos F.X. Clinical and functional outcome of childhood attention-deficit/hyperactivity disorder 33 years later. Arch Gen Psychiatry. 2012;69:1295–1303. doi: 10.1001/archgenpsychiatry.2012.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention Helping children cope with emergencies. https://www.cdc.gov/childrenindisasters/helping-children-cope.html Available at:
- 23.Chen C.Y.-C., Byrne E., Vélez T. Impact of the 2020 pandemic of COVID-19 on families with school-aged children in the United States: Roles of income level and race [published online ahead of print Mar 12] J Fam Issues. 2021 doi: 10.1177/0192513X21994153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Center for Translational Neuroscience A hardship chain reaction: Financial difficulties are stressing families’ and young children’s wellbeing during the pandemic, and it could get a lot worse. https://medium.com/rapid-ec-project/a-hardship-chain-reaction-3c3f3577b30 Available at: Accessed February 10, 2021.
- 25.Achenbach T.M., Rescorla L.A. University of Vermont, Research Center for Children, Youth, & Families; Burlington: 2001. Manual for the ASEBA School-Age Forms & Profiles. [Google Scholar]
- 26.Achenbach T.M., Rescorla L.A. University of Vermont, Research Center for Children, Youth, & Families; Burlington: 2003. Manual for the ASEBA Adult Forms & Profiles. [Google Scholar]
- 27.Conners C.K. Conners 3. 3rd ed. Multi-Health Systems; Toronto: 2008. [Google Scholar]
- 28.Conners C.K., Erhardt D., Sparrow E. Multi-Health Systems; Toronto: 1999. CAARS. Adult ADHD Rating Scales. Technical manual. [Google Scholar]
- 29.Ladouceur C.D. 2020. COVID-19 Adolescent Symptom & Psychological Experience Questionnaire. [Google Scholar]
- 30.Grasso D.J., Briggs-Gowan M.J., Ford J.D., Carter A.S. University of Connecticut School of Medicine; Farmington: 2020. The Epidemic–Pandemic Impacts Inventory (EPII) [Google Scholar]
- 31.Benjamini Y., Hochberg Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J R Stat Soc B (Methodol) 1995;57:289–300. [Google Scholar]
- 32.Zhang J., Shuai L., Yu H., Wang Z., Qiu M., Lu L., et al. Acute stress, behavioural symptoms and mood states among school-age children with attention-deficit/hyperactive disorder during the COVID-19 outbreak. Asian J Psychiatr. 2020;51:102077. doi: 10.1016/j.ajp.2020.102077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sciberras E., Patel P., Stokes M.A., Coghill D., Middeldorp C.M., Bellgrove M.A., et al. Physical health, media use, and mental health in children and adolescents with ADHD during the COVID-19 pandemic in Australia [published online ahead of print Dec 17] J Atten Disord. 2020 doi: 10.1177/1087054720978549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Odriozola-González P., Planchuelo-Gómez Á., Irurtia M.J., de Luis-García R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res. 2020;290:113108. doi: 10.1016/j.psychres.2020.113108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kecojevic A., Basch C.H., Sullivan M., Davi N.K. The impact of the COVID-19 epidemic on mental health of undergraduate students in New Jersey, cross-sectional study. PLoS One. 2020;15 doi: 10.1371/journal.pone.0239696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chaudry A., Wimer C. Poverty is not just an indicator: The relationship between income, poverty, and child well-being. Acad Pediatr. 2016;16:S23–S29. doi: 10.1016/j.acap.2015.12.010. [DOI] [PubMed] [Google Scholar]
- 38.Newland L.A. Family well-being, parenting, and child well-being: Pathways to healthy adjustment. Clin Psychol. 2015;19:3–14. [Google Scholar]
- 39.McKeown K., Haase T., Pratschke J. Ceifin Centre and Department of Social and Family Affairs; 2003. Family Well-Being: What Makes a Difference? Shannon. 5. [Google Scholar]
- 40.Garber J., Ciesla J.A., McCauley E., Diamond G., Schloredt K.A. Remission of depression in parents: Links to healthy functioning in their children. Child Dev. 2011;82:226–243. doi: 10.1111/j.1467-8624.2010.01552.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.