Abstract
Background:
Despite advancements in operative techniques and the extraordinary number of procedures described for correcting hallux valgus (HV), there is still uncertainty as to why some patients thrive postoperatively whereas others do not. This study aimed to investigate whether the postoperative outcome of HV surgery could be predicted from patient demographics or functional impairment at the time of referral.
Methods:
The prospectively collected data, from 92 patients, were analyzed to determine whether patient demographics significantly influenced outcome 52 weeks after surgery. Potential relationships between socioeconomic deprivation and the outcome, as well as between preoperative functional impairment and postoperative improvement, were examined. The Manchester Oxford Foot Questionnaire (MOXFQ) and Scottish Index of Multiple Deprivation (SIMD) were used in this evaluation.
Results:
None of the demographics studied were found to be statistically significant determinants of outcome. Preoperative MOXFQ scores for patients from the most deprived areas were significantly worse at the time of referral. Patients living in the least deprived postcodes experienced the lowest improvement in MOXFQ scores. Patients from the most deprived SIMD quintile achieved significantly higher improvement in MOXFQ–walking and standing compared to those from the least deprived quintile. A strong positive correlation was found between the preoperative MOXFQ scores and the improvement in the scores postoperatively.
Conclusion:
In this patient cohort, demographics could not be used to predict the postoperative outcome at week 52. Socioeconomic disparities seem to influence the timing of patients seeking surgery. Lower preoperative MOXFQ scores strongly correlate with a lesser degree of postoperative improvement.
Level of Evidence:
Level III, retrospective study with prospective arm.
Keywords: hallux valgus, forecasting operative outcome, functional outcome after hallux valgus surgery, socioeconomic
Hallux valgus is the most common forefoot deformity worldwide, affecting up to a third of adults, with at least 100 procedures being described for correcting it.23 The high number of procedures testifies to the challenge in achieving consistently satisfactory, long-term outcomes. A recent systematic review and meta-analysis from 2020 investigating the effect of HV surgery on patient quality of life demonstrated that HV surgery decreases the extent to which patients perceive pain and improves the patients’ quality of life, with particular reference to both the physical and social domains.14 An earlier systematic review from 2018, of 229 studies reporting the outcome of 16 237 HV surgeries, concluded that HV surgery is generally consistent with regard to results, rates of complications, and unfavorable outcomes.4 Several studies have reported that only two-thirds of patients report complete satisfaction with the operative outcome.6,13 Indeed, Coetzee10 reported 45% as being dissatisfied with the surgical outcome at 6 months and 47% at 12 months.
To the best of our knowledge, no study has yet investigated whether the reason for HV surgery failing to achieve a disease settlement is influenced by patient characteristics. The aim of this study was to investigate whether the postoperative outcome in patients undergoing HV surgery could be predicted from their pretreatment demographics. It also investigated the potential effect of socioeconomic disparities on operative outcome and explored whether there was relationship between the preoperative functional condition of the patient and the degree of improvement postoperatively.
Materials and Methods
This is a retrospective study with a prospective arm. Caldicott Guardian approval was obtained from NHS Tayside and the University of Dundee. Data from 92 patients who had undergone correction osteotomy for HV deformity were retrospectively reviewed. The data covered procedures from 3 hospitals as indicated above, between March 2016 and November 2017.
Manchester Oxford Foot Questionnaire
The Manchester Oxford Foot Questionnaire (MOXFQ) is a reliable and valid, patient-reported outcome measure (PROM), originally developed for HV, which has been proven to be highly responsive to changes in functional condition and has shown a high rate of patient completion. A systematic review from 2014 identified MOXFQ as one of the best available PROMs for evaluating HV surgery outcomes.24 The MOXFQ consists of 3 modules that are scored individually; these are foot pain (5 questions), walking and standing, (7 questions), and social interaction (4 questions). The score for each module varies between 0 and 100, where 0 represents the best possible clinical condition and 100 the worst.11 All 3 elements were used to evaluate the functional condition of the patient, both preoperatively and postoperatively at week 52. The inclusion criterion was consenting patients who had undergone primary corrective surgery for HV and had filled in the MOXFQ. Patients who underwent a revision procedure for HV or those who underwent a second procedure on the same foot were excluded.
This study focused on the change in the score, reported by the patient at week 52, compared to the preoperative score. This change was calculated by subtracting the postoperative score from the preoperative score. A positive value of the change indicates an improvement, whereas a negative value signifies a worsening of the patient’s clinical condition postoperatively. A null change reflects no change in the score and hence no measurable changes in the clinical condition of the patient, despite the procedure.
Dawson et al12 established the concept of the minimal clinically important difference (MCID) for MOXFQ. MCID is defined as being “the smallest change in the measure that patients perceive as meaningful and which would cause clinicians to consider a change in the patient’s management.” They noted values of 12 for MOXFQ-pain, 16 for MOXFQ–walking and standing, and 24 for MOXFQ–social interaction. This concept provides an important tool for quantifying any improvement or deterioration in MOXFQ scores and was therefore used in this study.
Scottish Index of Multiple Deprivation
The Scottish Index of Multiple Deprivation (SIMD) is a statistical tool, used by the Scottish government, NHS Scotland, and other governmental bodies in Scotland, to support policy and decision making, which won the Royal Statistical Society’s Excellence in Official Statistics Awards in 2017.28 Several studies have used it in quantifying the association between socioeconomic deprivation and health issues, such as tobacco consumption and alcohol abuse.27 SMID was used in this study to quantify the level of social deprivation of the participants.
In Scotland, each household is located in 1 of 6976 data zones, linked to the postal code, which SIMD ranked from 1 to 6976 according to the level of social deprivation, where 1 is the most deprived and 6976 is the least. The level of deprivation is measured for each data zone in 7 domains. These are crime, education, health, employment, housing, income, and geographic access. Each data zone is ranked by domain. There is also a composite ranking for all of these domains, which was used in this study. For the purposes of analysis, the rankings were divided into 5 equal groups (quintiles). Group 1 represents the most deprived and group 5 the least deprived quintile.26
Patient Satisfaction
Patients were asked whether or not there had been improvement in the symptoms for which they had been treated. In addition, they were asked whether or not they were satisfied with the result of the treatment. Finally, patients rated their overall postoperative satisfaction on a scale of 0 to 10, where 10 is being fully satisfied and 0 is being completely dissatisfied.
Statistical Analysis
Statistical Package for Social Sciences (SPSS) version 22.0 (SPSS, Inc) was used for all statistical analysis in this study. The level of significance was set at P < .05.
A univariate regression analysis was undertaken in this study to predict the relative weight of several independent variables in predicting the change in postoperative MOXFQ scores and patient satisfaction. The independent variables were patient age, sex, obesity, level of socioeconomic deprivation, and 2 comorbidities (high blood pressure and smoking). The operative outcome was quantified using the change in MOXFQ scores and by the patient satisfaction rate they reported.
To test any isolated effect of socioeconomic factors on the outcome of HV surgery and patient satisfaction, the 5 SIMD quintiles were compared with one another. One-way analysis of variance (ANOVA) was used to compare preoperative MOXFQ scores and the change in these scores postoperatively. Patient satisfaction was also compared between the quintiles using nonparametric tests.
A bivariate correlation between preoperative MOXFQ scores and the improvement in the MOXFQ scores postoperatively was tested for significance using the Pearson correlation. After finding a positive correlation, the variables were then plotted to estimate the correlation curve. The correlation between preoperative scores and patient satisfaction was examined using the Spearman correlation.
Results
Demographics
Females predominated in the cohort with a 9:1 ratio compared to males. The number of smokers was 11 (12%), but it should be noted that this figure was self-reported. Table 1 illustrates the demographics of the cohort.
Table 1.
Descriptive Statistics of the Cohort Demographics.
| Characteristic | Value |
|---|---|
| Sex, No. (%) | |
| Female | 83 (90.2) |
| Male | 9 (9.8) |
| Total, No. (%) | 92 (100) |
| Age (range, 24-82), mean (SD), y | 57.86 (10.19) |
| Body mass index (range, 16.4-42.8), mean (SD), kg/m2 | 27.53 (4.57) |
| Comorbidities, No. (%) | |
| Normotensive | 67 (72.8) |
| Hypertensive | 25 (27.2) |
| Nonsmoker | 81 (88.0) |
| Smoker | 11 (12.0) |
Figure 1 illustrates the distribution of patients in the study by SIMD datazone rank (range, 129-6973).
Figure 1.
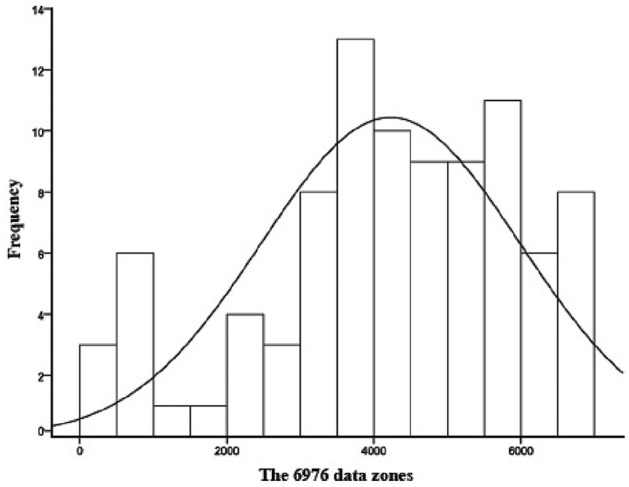
The distribution of patients over the 6976 data zones related to the Scottish Index of Multiple Deprivation.
Patient Demographics Influencing Operative Outcome and Patient Satisfaction
The results of the multiple univariate regression analysis showed that none of the independent variables had a predictive value of statistical significance in forecasting the change in MOXFQ scores or patient satisfaction rate postoperatively. P value was greater than .05 for all variables. Table 2 shows the related P values from each analysis.
Table 2.
P Values From Multiple Univariate Regression Analysis, Assessing the Relative Weight of Individual Demographic Characteristics in Determining Postoperative Change in MOXFQ Scores and Patient Satisfaction.
| Characteristic | Change in MOXFQ | Satisfaction rate | ||
|---|---|---|---|---|
| Pain | Walking and standing | Social interaction | ||
| Sex | 0.99 | 0.33 | 0.82 | 0.93 |
| Age | 0.90 | 0.75 | 0.67 | 0.49 |
| BMI | 0.89 | 0.43 | 0.76 | 0.83 |
| Hypertension | 0.52 | 0.51 | 0.07 | 0.67 |
| Smoking | 0.98 | 0.98 | 0.61 | 0.73 |
| SIMD | 0.70 | 0.054 | 0.68 | 0.98 |
Abbreviations: BMI, body mass index; MOXFQ, Manchester Oxford Foot Questionnaire; SIMD, Scottish Index of Multiple Deprivation.
Level of Social Deprivation Influencing Operative Outcome and Patient Satisfaction
Comparing the preoperative MOXFQ scores between the quintiles showed an overall tendency for patients located in the most deprived quintile to have higher scores. Statistically significant differences were found between the first and fifth quintiles in preoperative MOXFQ-pain and MOXFQ–walking and standing at P = .003 and .001, respectively. In addition, the P value was .053 when comparing the MOXFQ–social interaction preoperative scores between the first and the fifth quintiles. Similarly, statistically significant differences were found in MOXFQ-pain between the third and fifth quintiles (P = .02) and in MOXFQ–walking and standing between the first and third (P = .02) and between the fourth and fifth quintiles (P = .03). Figure 2 shows the means for the preoperative scores of the different categories of MOXFQ in the SIMD quintiles.
Figure 2.

Error bars showing the mean preoperative Manchester Oxford Foot Questionnaire (MOXFQ) scores by Scottish Index of Multiple Deprivation (SIMD) quintile. Statistically significant differences were found between the first and fifth and between the first and third SIMD quintiles for MOXFQ–walking and standing. Confidence interval 95%.
Given the numbers available, no statistically significant difference could be detected between the SIMD quintiles either in the change of MOXFQ-pain or in the change in MOXFQ–social interaction scores. However, there were statistically significant differences between the first and fifth, as well as first and third, SIMD quintiles in regard to the change in MOXFQ–walking and standing, with a P value of .03 and .02, respectively. A tendency was observed of patients from the most deprived quintile achieving a higher change in their MOXFQ-pain scores compared to those who lived in the least deprived quintile, but this was not statistically significant. Figure 3 shows the means for the change of different categories of MOXFQ scores in the SIMD quintiles.
Figure 3.

Error bars showing the mean change in Manchester Oxford Foot Questionnaire (MOXFQ) scores by Scottish Index of Multiple Deprivation (SIMD) quintile. Statistically significant differences were found between the first and fifth SIMD quintiles for MOXFQ-pain and MOXFQ–walking and standing. Confidence interval 95%.
Follow-up Scores and Patient Satisfaction
Only 1 patient had a zero score for MOXFQ-pain preoperatively. Both MOXFQ–walking and standing and MOXFQ–social interaction had 5 patients with zero scores preoperatively. None of the patients had zero scores in all categories of the MOXFQ simultaneously.
This study focused on the change in the score from preoperative to week 52 postoperatively. The change in MOXFQ-pain scores exhibited a negative value in 11 patients (12%; ie, a deterioration in their scores), whereas 76 patients (82.6%) had a positive value (ie, an improvement in their scores). In 5 patients (5.4%), there was no change in scores. Similarly, the change in MOXFQ–walking and standing scores exhibited a negative value in 17 patients (18.5%), a positive value in 69 patients (75%), and no change in 6 patients (6.5%). Likewise, the change in MOXFQ–social interaction scores exhibited a negative value in 17 patients (18.5%), a positive value in 72 patients (78.3%), and no change in 3 patients (3.3%).
There were 28 patients (30.4%) who exhibited a change in the MOXFQ score for pain, which was under the MCID related to the MOXFQ-pain score. Similarly, 39 patients (42.4%) exhibited changes below the MICD in their MOXFQ–walking and standing scores, and 40 patients (43.5%) exhibited changes below MICD in their MOXFQ–social interaction scores.
The data analysis revealed that 79 patients (87.8%) had experienced some improvement postoperatively, and 11 patients (12.2%) had not. However, only 62 patients (67.4%) were satisfied with the outcome. The dissatisfaction rate was 32.6% (30 patients).
The mean for the satisfaction score, on the 0 to 10 scale, was 7.41, with only 66.7% of patients rating their satisfaction as equivalent to 7 or above.
Overall, 20 patients (21.7%) had changes in their scores that were less than the MCID in all 3 domains of the MOXFQ. For those 20 patients, the mean satisfaction rate, on the 0 to 10 scale, was 4.95, with 16 of them (80%) being dissatisfied with the operative outcome.
Examination of the Relationship Between Preoperative Scores, Postoperative Scores Improvement, and Patient Satisfaction
A positive linear correlation was found between the preoperative MOXFQ-pain score and the change in the score postoperatively (P < .001). Pearson correlation coefficient was 0.402, and R2 was 0.161.
A positive linear correlation was similarly found between the preoperative MOXFQ–walking and standing score and the change in the score postoperatively (P < .001). Pearson correlation coefficient was 0.549, and R2 was 0.302. A positive linear correlation was similarly found between the preoperative MOXFQ–social interaction score and the change in the score postoperatively (P < .001). Pearson correlation coefficient was 0.583, and R2 was 0.340. Figures 4 to 6 illustrate the estimated correlation curves.
Figures 4.
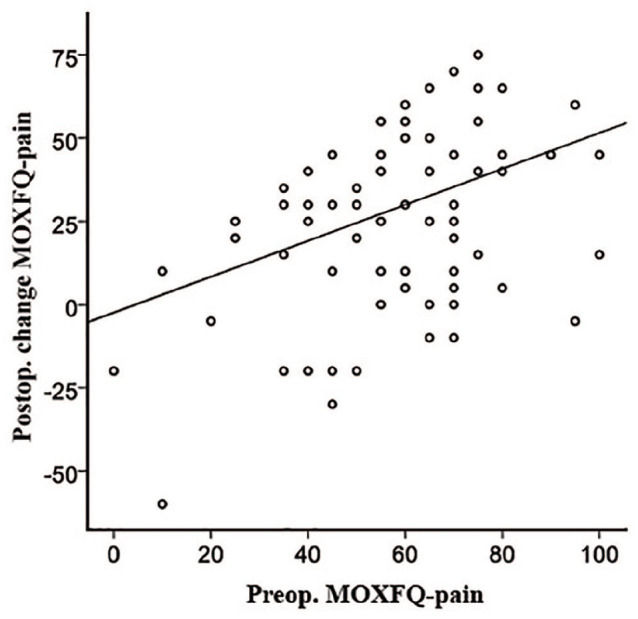
Graphical representation of the relationship between preoperative MOXFQ-pain score and postoperative change in MOXFQ-pain score at week 52. Strong positive linear correlation was found between Preop. MOXFQ-pain and its change postoperatively.
Figures 5.

Graphical representation of the relationship between preoperative MOXFQ-walking and standing score and postoperative change in MOXFQ-walking and standing score at week 52. Strong positive linear correlation was found between Preop. MOXFQ-walking and standing and its change postoperatively.
Figures 6.

Graphical representation of the relationship between preoperative MOXFQ-social interaction score and postoperative change in MOXFQ-social interaction score at week 52. Strong positive linear correlation was found between Preop. MOXFQ- social interaction score and its change postoperatively.
Discussion
Despite the high number of procedures described to surgically treat HV deformity, there remains uncertainty as to why some patients thrive postoperatively, while others do not. Since these elective procedures involve a considerable financial burden on the National Health Service, it is important to clarify the uncertainty regarding this issue.
The value of PROMs in guiding a decision-making process that enhances a patient-centered and collaborative approach is increasing tremendously in foot and ankle research.2,3 A recent study succeeded in identifying a preoperative Patient-Reported Outcome Measurement Instrumentation System (PROMIS) threshold score for HV, over which the failure of surgery to achieve a meaningful improvement in the patient’s clinical situation can be reliably predicted.18
Our findings showed that patient demographics do not seem to have a palpable effect on the outcome of HV surgery, but socioeconomic disparities appear to play a defining role not only in how far the disease will develop before surgical help is sought but perhaps also in the subsequent efficacy of surgical intervention. Finally, our findings demonstrated a substantial correlation between the stage of disease preoperatively and the measurable improvement after surgery.
Demographics Analysis
The analysis of patient demographics demonstrated that women predominated in the study, with 90.2% of the cohort. This translates as 1 male to every 9 females. Other studies reported a ratio of approximately 1 male for every 15 females.17,21 Furthermore, it is worth mentioning that the percentage of smokers in the present study (12%) does not correlate with the officially reported smoking rate in Scotland, which was 21% in 2016 and 18% in 2017.25
Patient Demographics Influencing Surgical Outcome
Poor operative outcome or patient dissatisfaction related to HV surgery is multifactorial. Baseline demographics, including sex, age, obesity, comorbidities, or socioeconomic factors, as well as patient expectation, may all contribute toward the outcome to some extent. Several studies have focused on the effect of only one of these factors on operative outcome or patient satisfaction and showed inconsistent results. While current literature on HV suggests that sex may not be a risk factor for poor operative outcome, studies that assessed the influence of age on the outcome showed rather conflicting findings.8,13,15,17,20,30-32 The effect of obesity on the outcome has also been assessed by a limited number of studies. Chen et al7 suggested that obese patients experienced a greater improvement postoperatively than normal-weight patients. Milczarek et al19 found that obese patient achieved significantly lower American Orthopaedic Foot & Ankle Society (AOFAS) scores compared to the normal-weight group, but their pain and satisfaction ratings were comparable. Kromuszczyńska et al16 assessed functional outcome 6 months after scarf osteotomy and found no significant difference in AOFAS scores between patients with or without comorbidities.
This study is unique, in that it is the first to address the simultaneous effects of multiple patient demographic characteristics on operative outcome after HV surgery. Statistical analysis was used to identify the relative weight and influence of sex, age, obesity, comorbidities, and level of social deprivation on the prediction of both postoperative functional improvement and patient satisfaction.
Our findings indicate that none of the variables studied, when considered together, showed significant value in predicting operative outcome or patient satisfaction after HV surgery. Hence, with the available cohort, no statistical method could be identified to predict the outcome of HV surgery based on patient demographics. Efforts should be made to verify these results on a larger cohort.
Influence of Socioeconomic Deprivation on Operative Outcome and Patient Satisfaction
An interesting pattern emerged when examining whether patients from different socioeconomic backgrounds would experience significantly different outcomes and satisfaction levels after HV surgery. Patients who were from the most socioeconomically deprived areas, showed an overall propensity toward achieving a greater change in their MOXFQ scores postoperatively. However, this was only statistically significant in the walking and standing category of the MOXFQ.
To the best of our knowledge, this study is the first to assess the effect of socioeconomic disparities on the outcome of HV surgery. Similar studies into knee and hip arthroplasty have demonstrated that lower household income does have a predictive value for poorer functional outcomes and lower patient satisfaction levels postoperatively.1,5 In contrast to this, however, our findings demonstrated that patients who lived in the most deprived SIMD quintiles achieved significantly greater improvement after HV surgery. Considering the fact that this group of patients had significantly worse preoperative scores, their greater improvement is hardly surprising. Interestingly, patients who lived in the least deprived SIMD quintiles had significantly better preoperative scores but tended to report significantly less improvement postoperatively.
These findings suggest that patients from the most deprived areas report significantly higher levels of impairment in their functional status at the time of referral, in stark contrast to those from the least deprived quintiles. It is therefore evident that more economically deprived patients tend to have HV surgery at a later stage in the course of their disease, which echoes the findings of similar studies conducted into knee and hip replacement.22 As the reasons for this are beyond the scope of this study, one can only speculate that it may be the lack of access to medical services that leads patients from the most deprived areas to delay accessing medical assistance until their condition has become more advanced.
Follow-up Scores and Patient Satisfaction
This study focused on the change in the patients’ MOXFQ scores at week 52 postoperatively, compared to their preoperative scores. This change was calculated by subtracting the patients’ postoperative scores from their preoperative ones, thus reflecting the perceived clinical improvement or deterioration of the patients’ clinical condition.
Our findings showed that the percentage of patients who exhibited a change under the MCID for MOXFQ-pain was 25.6%, as opposed to 35.8% for walking and standing and 36.8% for social interaction. There were 20 patients (18.4%) for whom changes in the scores, across all 3 domains of the MOXFQ, were below the specific MCID. As expected, the mean satisfaction score for these patients, on the 0 to 10 scale, was low at 4.95. However, 5 of these 20 patients (25%) stated that they were still satisfied with the outcome, scoring their satisfaction above the average for the cohort. Interestingly, however, one 75-year-old female patient stated that she was not satisfied with the outcome but scored her satisfaction at 8.
This apparent contradiction was also reported in other studies and could be partly explained by the substantial differences in patient expectations from HV surgery.2 Choi et al8 suggested that male patients may have less expectation fulfillment after HV surgery. Tai et al29 noted variation in patient expectations from HV surgery based on both age and sex. They found that male patients prioritized return to work over bunion pain and cosmesis, whereas female patients attached greater importance to bunion pain and improvement in forefoot appearance. The same study showed that patients younger than 40 years expected the surgery to improve their walking, reduce pain, and facilitate shoe comfort, whereas in patients older than 60 years, the most crucial expectation was to improve overall mobility.
Relationship Between Preoperative Scores and Postoperative Score Improvement
The clinical potential of this study was revealed through an examination of the relationship between preoperative MOXFQ scores and their improvement postoperatively. On each of the 3 MOXFQ scales, strong positive linear correlation was found. P values were all lower than .001. This correlation signifies that the change in the score postoperatively is proportional to the preoperative score. In other words, the lower the preoperative MOXFQ score at the time of surgery, the less the improvement in the postoperative score.
The R2 value indicates the percentage of the cohort that the linear correlation accounts for. It was 0.16 for MOXFQ-pain, 0.30 for MOXFQ–walking and standing, and 0.34 for MOXFQ–social interaction. A low R2 value does not necessarily mean a weak correlation, as this can be distorted by extreme values of the variables.
Overall, these strong linear correlations suggest a tendency for patients with worse preoperative scores to experience a greater reduction in their perceived level of pain and a greater improvement in their functional condition, compared to those with better scores. The importance of this point must be explained to patients who are considering HV surgery, and the surgeon should bear this in mind when offering surgery as an option.
Strengths and Weaknesses
One criticism that could reasonably be leveled at this study is that it was, of necessity, based upon the SIMD. Although the SIMD is a well-accredited tool for governmental, evidence-based policy making, it has also been subject to certain criticisms, including that the inherently rigid geographic divisions used in delineating the various socioeconomic groups may not accurately reflect the heterogeneous levels of social deprivation in any given quintile.9 Also, since patient numbers in each SIMD quintile are relatively small, caution is needed in the interpretation of the results.
On the other hand, to the best of our knowledge, this is the first study to assess the simultaneous effect of multiple demographic characteristics on the outcome of HV surgery and to have analyzed the relationship between socioeconomic deprivation and HV surgical outcome. Furthermore, it is the first study to positively establish a correlation between patient functional status before HV surgery and their subsequent functional improvement. Future research could focus on verifying these findings in a larger cohort.
Conclusions
This study has demonstrated that patient demographics cannot be used to predict either operative outcome or patient satisfaction at week 52 postoperatively. Nevertheless, a strong and viable correlation was established between patient functional status before surgery and their functional improvement postoperatively. Evidence from this study suggests that patients from the most deprived SIMD quintiles tend to have the worst MOXFQ scores at the time of referral and that this higher level of preoperative functional impairment strongly correlates with greater improvement after surgery.
The authors recommend more emphasis to be placed on addressing patient expectations when offering corrective procedures for HV, as well as a standardized usage and interpretation of a reliable PROM as an essential component in preoperative patient evaluation.
Supplemental Material
Supplemental material, sj-pdf-1-fai-10.1177_10711007211002498 for Forecasting Posttreatment Outcome of Hallux Valgus Surgery Patients by Amjad Sawah, Stepanka Zemenova, Russel Haque, David Ridley, MSc, BSc, Rami J. Abboud, Weijie Wang and Fraser Harrold in Foot & Ankle International
Acknowledgments
We thank David Lawrence Wilson for his help and support.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Amjad Sawah, MD, MCh Orth,  https://orcid.org/0000-0003-4459-8852
https://orcid.org/0000-0003-4459-8852
References
- 1.Allen Butler R, Rosenzweig S, Myers L, Barrack R. The Frank Stinchfield Award: the impact of socioeconomic factors on outcome after THA: a prospective, randomized study. Clin Orthop Relat Res. 2011;469(2):339-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson MR, Baumhauer JF, DiGiovanni BF, et al. determining success or failure after foot and ankle surgery using Patient Acceptable Symptom State (PASS) and Patient Reported Outcome Information System (PROMIS). Foot Ankle Int. 2018;39(8):894-902. [DOI] [PubMed] [Google Scholar]
- 3.Anderson MR, Houck JR, Saltzman CL, et al. Validation and generalizability of preoperative PROMIS scores to predict postoperative success in foot and ankle patients. Foot Ankle Int. 2018;39(7):763-770. [DOI] [PubMed] [Google Scholar]
- 4.Barg A, Harmer JR, Presson AP, Zhang C, Lackey M, Saltzman CL.Unfavorable outcomes following surgical treatment of hallux valgus deformity: a systematic literature review. J Bone Joint Surg Am. 2018;100(18):1563-1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barrack R, Ruh E, Chen J, et al. Impact of socioeconomic factors on outcome of total knee arthroplasty. Clin Orthop Relat Res. 2014;472(1):86-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berg RP, Olsthoorn PG, Poll RG.Scarf osteotomy in hallux valgus: a review of 72 cases. Acta Orthop Belg. 2007;73(2):219-223. [PubMed] [Google Scholar]
- 7.Chen JY, Lee MJ, Rikhraj K, et al. Effect of obesity on outcome of hallux valgus surgery. Foot Ankle Int. 2015;36(9):1078-1083. [DOI] [PubMed] [Google Scholar]
- 8.Choi GW, Kim HJ, Kim TW, Lee JW, Park SB, Kim JK.Sex-related differences in outcomes after hallux valgus surgery. Yonsei Med J. 2015;56(2):466-473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clelland D, Hill C.Deprivation, policy and rurality: the limitations and applications of area-based deprivation indices in Scotland. Local Economy. 2019;34(1):33-50. [Google Scholar]
- 10.Coetzee JC.Scarf osteotomy for hallux valgus repair: the dark side. Foot Ankle Int. 2003;24(1):29-33. [DOI] [PubMed] [Google Scholar]
- 11.Dawson J, Coffey J, Doll H, et al. A patient-based questionnaire to assess outcomes of foot surgery: validation in the context of surgery for hallux valgus. Qual Life Res. 2006;15(7):1211-1222. [DOI] [PubMed] [Google Scholar]
- 12.Dawson J, Doll H, Coffey J, et al. Responsiveness and minimally important change for the Manchester-Oxford Foot Questionnaire (MOXFQ) compared with AOFAS and SF-36 assessments following surgery for hallux valgus. Osteoarthritis Cartilage. 2007;15(8):918-931. [DOI] [PubMed] [Google Scholar]
- 13.Hattrup SJ, Johnson KA.Chevron osteotomy: analysis of factors in patients’ dissatisfaction. Foot Ankle. 1985;5(6):327-332. [DOI] [PubMed] [Google Scholar]
- 14.Hernández-Castillejo LE, Martínez Vizcaíno V, Garrido-Miguel M, Cavero-Redondo I, Pozuelo-Carrascosa DP, Álvarez-Bueno C.Effectiveness of hallux valgus surgery on patient quality of life: a systematic review and meta-analysis. Acta Orthop. 2020;91(4):450-456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson KA.Chevron osteotomy of the first metatarsal: patient selection and technique. Contemp Orthop. 1981;3:707-711. [Google Scholar]
- 16.Kromuszczyńska J, Kołodziej Ł, Jurewicz A.Wound healing complications in patients with and without systemic diseases following hallux valgus surgery. PLoS One. 2018;13(6):e0197981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lim WSR, Liow MHL, Rikhraj IS, Goh GS-H, Koo K. The effect of gender in hallux valgus surgery: a propensity score matched study. Foot Ankle Surg. 2019;25(5):670-673. [DOI] [PubMed] [Google Scholar]
- 18.MacDonald A, Houck J, Baumhauer JF.Role of patient-reported outcome measures on predicting outcome of bunion surgery. Foot Ankle Int. 2020;41(2):133-139. [DOI] [PubMed] [Google Scholar]
- 19.Milczarek MA, Milczarek JJ, Tomasik B, Laganowski P, Nowak K, Domzalski M.Being overweight has limited effect on SCARF osteotomy outcome for hallux valgus correction. Int Orthop. 2017;41(4):765-772. [DOI] [PubMed] [Google Scholar]
- 20.Milnes HL, Kilmartin TE, Dunlop G.A pilot study to explore if the age that women undergo hallux valgus surgery influences the post-operative range of motion and level of satisfaction. Foot. 2010;20(4):109-113. [DOI] [PubMed] [Google Scholar]
- 21.Nery C, Coughlin MJ, Baumfeld D, Ballerini FJ, Kobata S.Hallux valgus in males—part 1: demographics, etiology, and comparative radiology. Foot Ankle Int. 2013;34(5):629-635. [DOI] [PubMed] [Google Scholar]
- 22.Neuburger J, Hutchings A, Allwood D, Black N, van der Meulen JH.Sociodemographic differences in the severity and duration of disease amongst patients undergoing hip or knee replacement surgery. J Public Health. 2012;34(3):421-429. [DOI] [PubMed] [Google Scholar]
- 23.Nix S, Smith M, Vicenzino B.Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. J Foot Ankle Res. 2010;3:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schrier JC, Palmen LN, Verheyen CC, Jansen J, Koeter S.Patient-reported outcome measures in hallux valgus surgery: a review of literature. Foot Ankle Surg. 2015;21(1):11-15. [DOI] [PubMed] [Google Scholar]
- 25.Scottish Government. Scottish Health Survey main report 2016 and 2017. https://www.gov.scot/publications/scottish-health-survey-2016-volume-1-main-report/pages/18/https://www.gov.scot/publications/scottish-health-survey-2017-volume-1-main-report/pages/62/. Accessed Sepember 2020.
- 26.Scottish Government. Scottish Index of Multiple Deprivation 2016 and 2020. https://www.gov.scot/publications/scottish-index-multiple-deprivation-2016/https://www.gov.scot/collections/scottish-index-of-multiple-deprivation-2020/. Accessed Sepember 2020.
- 27.Scottish Government. Scottish Health Survey 2018 main report - revised 2020. https://www.gov.scot/publications/scottish-health-survey-2018-volume-1-main-report/pages/24/. Accessed Sepember 2020.
- 28.Statistical Excellence Award Winners 2017. 2021. The Royal Statistical Society. https://rss.org.uk/RSS/media/File-library/Events/Awards/Winners-booklet2017.pdf. Accessed November 2021.
- 29.Tai C, Ridgeway S, Ramachandran M, Ng VA, Devic N, Singh D.Patient expectations for hallux valgus surgery. J Orthop Surg. 2008;16(1):91-95. [DOI] [PubMed] [Google Scholar]
- 30.Tollison ME, Baxter DE.Combination chevron plus akin osteotomy for hallux valgus: should age be a limiting factor? Foot Ankle Int. 1997;18(8):477-481. [DOI] [PubMed] [Google Scholar]
- 31.Trnka HJ, Hofstaetter SG, Hofstaetter JG, Gruber F, Adams SB, Jr, Easley ME.Intermediate-term results of the Ludloff osteotomy in one hundred and eleven feet. J Bone Joint Surg Am. 2008;90(3):531-539. [DOI] [PubMed] [Google Scholar]
- 32.Trnka HJ, Zembsch A, Easley ME, Salzer M, Ritschl P, Myerson MS.The chevron osteotomy for correction of hallux valgus: comparison of findings after two and five years of follow-up. J Bone Joint Surg Am. 2000;82(10):1373-1378. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-fai-10.1177_10711007211002498 for Forecasting Posttreatment Outcome of Hallux Valgus Surgery Patients by Amjad Sawah, Stepanka Zemenova, Russel Haque, David Ridley, MSc, BSc, Rami J. Abboud, Weijie Wang and Fraser Harrold in Foot & Ankle International


