Abstract
This cross-sectional study examines associations of nursing home characteristics with COVID-19 vaccination rates among nursing home staff and residents.
Vaccines have been instrumental in reducing COVID-19 cases and related deaths among US nursing home residents.1 However, low vaccination coverage among nursing home staff,2 who may introduce COVID-19 into facilities, could contribute to future outbreaks, especially in the presence of more transmissible variants.3,4 Maximizing vaccination coverage among nursing home staff and residents is critical because of the extreme vulnerability of this population to COVID-19, but little is known about which nursing homes have been successful at achieving high vaccination coverage.
Methods
We performed a cross-sectional analysis of federal National Healthcare Safety Network facility-level data through the week ending July 18, 2021, combined with other publicly available data sets (eMethods 1 in the Supplement). We examined the percentage of completed COVID-19 vaccinations among nursing home residents and different staff types at each facility, including all health care personnel eligible to work in the nursing home in the prior week, registered nurses and licensed practical nurses, certified nursing assistants (CNAs), therapists, and physicians and independent practitioners. Estimated means were weighted by the relevant population size (resident census and staff counts). Per Harvard University institutional policy, institutional review board approval and written informed consent were not required owing to use of publicly available data. This study was informed by the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines for cross-sectional studies.
We examined the association between weighted group vaccination coverage and facility characteristics using multivariate linear regressions. The regressions included state fixed effects to account for the state variation in vaccine availability and other policies. Facility characteristics of interest included ownership status, overall quality rating, demographic characteristics of residents and staff, percentage of direct care staff with more than 33 weeks (national median) of tenure, cumulative staff and resident COVID-19–related death rates, and county-level information, including adult vaccination coverage and the 2020 presidential election Republican vote margin (eMethods 2 in the Supplement). All statistical analyses were performed with Stata, version 16 (StataCorp), and 2-sided P < .05 was considered statistically significant.
Results
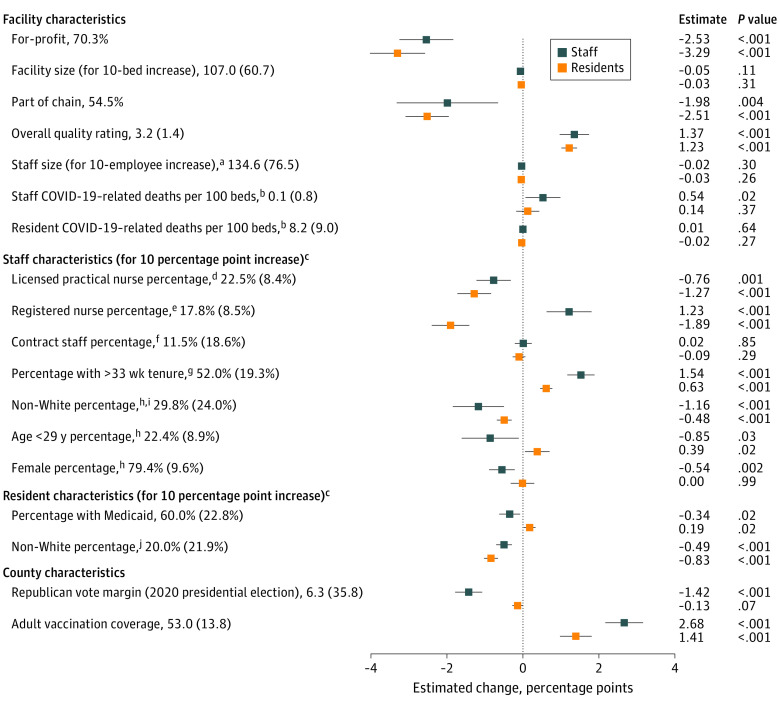
Among the more than 14 900 nursing homes reporting vaccination data by July 18, 2021, 60.0% of staff and 81.4% of residents were fully vaccinated on average (Figure 1). Average vaccination coverage was lowest among CNAs (49.2%) and registered nurses and licensed practical nurses (61.0%), with higher coverages noted among therapists (70.9%) and physicians and independent practitioners (77.3%).
Figure 1. Distribution of Completed Vaccination Coverage Among Nursing Home Residents and Staff.
Orange diamonds denote weighted estimates of average vaccination coverages for each group. Weights are obtained from the corresponding number of staff members or residents within each facility reported in the National Healthcare Safety Network data.
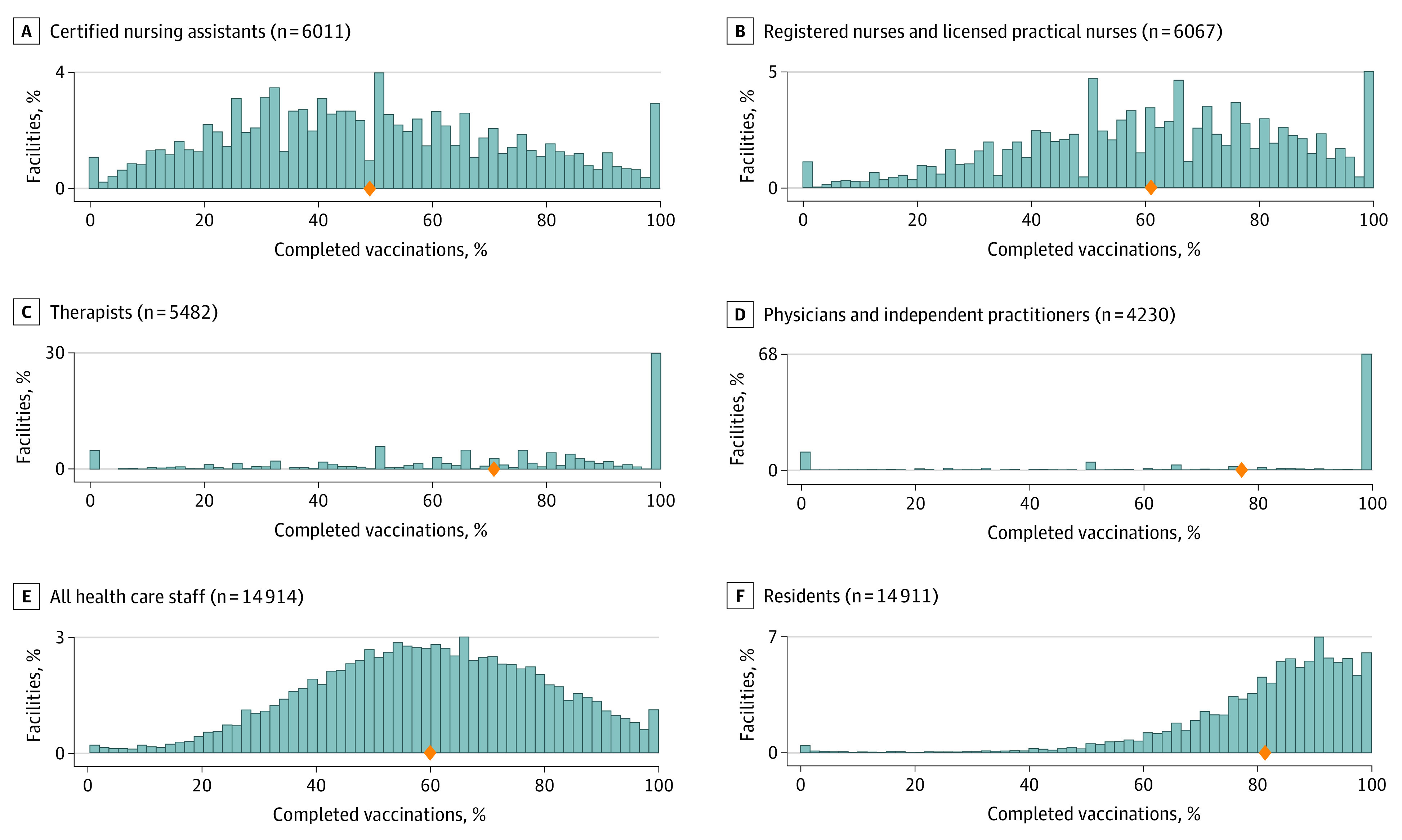
After adjustment, for-profit ownership was associated with a decrease of 2.5 (95% CI, −3.2 to 1.8) and 3.3 (95% CI, −4.0 to 2.6) percentage points for staff and resident vaccination coverages, respectively, compared with nonprofit facilities (Figure 2). Each additional Medicare star rating was associated with a 1.4 (95% CI, 1.0-1.8) and 1.2 (95% CI, 1.0-1.4) percentage point increase in staff and resident vaccination coverages, respectively. A 10 percentage point increase in longer-tenured staff was associated with increases of 1.5 (95% CI, 1.2-1.9) and 0.6 (95% CI, 0.5-0.8) percentage points in staff and resident vaccination coverages, respectively. Greater percentages of staff and residents who were non-White (ie, American Indian or Alaska Native, Asian, Black, Pacific Islander or Native Hawaiian, and 2 or more races) were associated with lower vaccination coverages for both groups (Figure 2). A 10 percentage point increase in the county adult vaccination coverage was associated with increases of 2.7 (95% CI, 2.2-3.2) and 1.4 (95% CI, 1.0-1.8) percentage points in staff and resident vaccination coverages, respectively, while a 10 percentage point increase in Republican vote margin in the 2020 presidential election was associated with a decrease of 1.4 (95% CI, −1.8 to −1.1) percentage points in staff vaccination coverage.
Figure 2. Estimated Changes in Resident and Health Care Staff Vaccination Coverages by Selected Nursing Home Characteristics.
The Figure presents adjusted marginal changes and associated 95% CIs in resident and health care staff vaccination coverages as a function of nursing home characteristics using the most recent week of vaccination data available for each facility (n = 14 900) through the week ending July 18, 2021. Unless otherwise indicated, data in the left column are mean (SD) values. Marginal changes in coverage are estimated using linear regressions that include the variables presented here and state fixed effects. Models are weighted by resident and staff sizes with clustered standard errors. See eMethods 2 in the Supplement for full specification.
aDefined as the total number of unique employees who worked in a facility in the fourth quarter of 2020.
bTotal number of reported COVID-19–related deaths as of July 11, 2021, per 100 beds in the facility.
cAll estimates presented in this category are scaled to reflect the marginal change in vaccination coverage for every 10 percentage point increase in the characteristics of interest.
dDefined as the percentage of total direct care workers who were licensed practical nurses in the fourth quarter of 2020.
eDefined as the percentage of total direct care workers who were registered nurses in the fourth quarter of 2020.
fDefined as the percentage of direct care workers classified as a contract worker in the fourth quarter of 2020.
gDefined as the percentage of direct care workers who had a work history at their current facility greater than the national median (33 weeks) in the fourth quarter of 2020.
hEstimated using the 2018 Longitudinal Employer-Household Dynamics Origin-Destination Employment Statistics data.
iNon-White race includes race categories of American Indian or Alaska Native, Asian, Black, Pacific Islander or Native Hawaiian, and 2 or more races. Individuals identifying as White race and Hispanic ethnicity are not included in this category.
jNon-White race includes race categories of American Indian or Alaska Native, Asian, Black, and Pacific Islander or Native Hawaiian. Individuals identifying as White race and Hispanic ethnicity are not included in this category.
Discussion
Results of this cross-sectional study demonstrate that COVID-19 vaccination coverage among health care staff in nursing homes lagged relative to resident coverage, with the lowest coverage among CNAs, who constitute the majority of direct caregivers. We found that nonprofit and nonchain nursing homes, facilities with higher Medicare star ratings, and facilities with longer-tenured staff achieved greater vaccine coverage, suggesting that organizational characteristics, including ownership structure, quality, and ability to retain staff, may be key in facilities’ ability to vaccinate residents and staff.5 However, the present findings suggest that facilities are also subject to broader challenges to vaccine acceptance in the community because facility coverages were strongly associated with county-wide vaccination coverage and staff coverage was strongly associated with 2020 presidential election voting patterns.
President Biden recently announced that the US Department of Health and Human Services is developing new requirements that nursing homes mandate COVID-19 vaccinations for staff as a condition for receiving reimbursement from Medicare and Medicaid.6 This study provides information about the scope of current vaccine refusal, the key correlates of low vaccine take-up, and the types of facilities most likely to be affected by this new requirement. This analysis is limited by the potential for unobserved confounders, which limits generalizability of the findings, and by the use of facility-level data, which limits our precision in estimating individual-level correlates of take-up.
eMethods 1. Supplementary Detail on Data Sources and Sample
eMethods 2. Supplementary Details on Methods
eReferences
References
- 1.White EM, Yang X, Blackman C, Feifer RA, Gravenstein S, Mor V. Incident SARS-CoV-2 infection among mRNA-vaccinated and unvaccinated nursing home residents. N Engl J Med. 2021;385(5):474-476. doi: 10.1056/NEJMc2104849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gharpure R, Patel A, Link-Gelles R. First-dose COVID-19 vaccination coverage among skilled nursing facility residents and staff. JAMA. 2021;325(16):1670-1671. doi: 10.1001/jama.2021.2352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shen K. Relationship between nursing home COVID-19 outbreaks and staff neighborhood characteristics. medRxiv. Preprint posted online December 6, 2020.doi: 10.1101/2020.09.10.20192203 [DOI] [PMC free article] [PubMed]
- 4.McGarry BE, Gandhi AD, Grabowski DC, Barnett ML. Larger nursing home staff size linked to higher number of COVID-19 cases in 2020. Health Aff (Millwood). 2021;40(8):1261-1269. doi: 10.1377/hlthaff.2021.00323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.White EM, Wetle TF, Reddy A, Baier RR. Front-line nursing home staff experiences during the COVID-19 pandemic. J Am Med Dir Assoc. 2021;22(1):199-203. doi: 10.1016/j.jamda.2020.11.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.President Biden to announce new actions to protect Americans from COVID-19 and help state and local leaders fight the virus. News release. The White House. August 18, 2021. Accessed September 1, 2021. https://www.whitehouse.gov/briefing-room/statements-releases/2021/08/18/fact-sheet-president-biden-to-announce-new-actions-to-protect-americans-from-covid-19-and-help-state-and-local-leaders-fight-the-virus/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods 1. Supplementary Detail on Data Sources and Sample
eMethods 2. Supplementary Details on Methods
eReferences