Key Points
Question
Were environmental changes during the outbreak of COVID-19 associated with increased development of myopia in young schoolchildren in China?
Findings
In this observational study longitudinally monitoring 2114 students from grade 2 to grade 3, myopia incidence doubled from November and December 2019 to November and December 2020 compared with the same period from 2018 to 2019. The proportion of children without myopia and with spherical equivalent refraction greater than −0.50 D and less than or equal to +0.50 D in grade 3 had increased by 18% by November and December 2020 compared with the same period in 2019.
Meaning
These data suggest that development of myopia in young Chinese schoolchildren may have increased during the COVID-19 outbreak; the long-term impact of environmental changes during the COVID-19 outbreak period on the development of myopia in children needs further investigation.
This observational study investigates changes in development of myopia in young Chinese schoolchildren during the outbreak of COVID-19.
Abstract
Importance
During the outbreak of COVID-19, outdoor activities were limited and digital learning increased. Concerns have arisen regarding the impact of these environmental changes on the development of myopia.
Objective
To investigate changes in the development of myopia in young Chinese schoolchildren during the outbreak of COVID-19.
Design, Setting, and Participants
In this observational study, 2 groups of students from 12 primary schools in Guangzhou, China, were prospectively enrolled and monitored from grade 2 to grade 3. Comparisons between the exposure and nonexposure groups were made to evaluate any association between environmental changes during the COVID-19 outbreak period and development of myopia. The exposure group received complete eye examinations in November and December 2019 and November and December 2020. The nonexposure group received examinations in November and December 2018 and November and December 2019.
Main Outcomes and Measures
Changes in cycloplegic spherical equivalent refraction (SER), axial length (AL) elongation, and myopia incidence from grade 2 to grade 3.
Results
Among the 2679 eligible students in grade 2 (mean [SD] age, 7.76 [0.32] years; 1422 [53.1%] male), 2114 (1060 in the nonexposure group and 1054 in the exposure group) were reexamined in grade 3. Compared with the period from November and December 2018 to November and December 2019, the shift of SER, AL elongation, and myopia incidence from grade 2 to grade 3 from November and December 2019 to November and December 2020 was 0.36 D greater (95% CI, 0.32-0.41; P < .001), 0.08 mm faster (95% CI, 0.06-0.10; P < .001), and 7.9% higher (95% CI, 5.1%-10.6%; P < .001), respectively. In grade 3 students, the prevalence of myopia increased from 13.3% (141 of 1060 students) in November and December 2019 to 20.8% (219 of 1054 students) in November and December 2020 (difference [95% CI], 7.5% [4.3-10.7]; P < .001); the proportion of children without myopia and with SER greater than −0.50 D and less than or equal to +0.50 D increased from 31.1% (286 of 919 students) to 49.0% (409 of 835 students) (difference [95% CI], 17.9% [13.3-22.4]; P < .001).
Conclusions and Relevance
In this study, development of myopia increased during the COVID-19 outbreak period in young schoolchildren in China. Consequently, myopia prevalence and the proportion of children without myopia who were at risk of developing myopia increased. Future studies are needed to investigate long-term changes in myopia development after the COVID-19 pandemic.
Introduction
In December 2019, a novel coronavirus epidemic emerged in China and became a worldwide pandemic within several months. In response to the COVID-19 outbreak, many governments ordered strict quarantine and lockdown measures. Home confinement was imposed on an unprecedented scale. Schools and universities were closed nationwide and online courses were delivered. Following these efforts, the pandemic was effectively contained in China, as well as in some other areas of the world, by September 2020. However, factoring in the prolonged execution time of the measures, concerns have arisen over their collateral impact on children’s health.1 Specifically, there have been concerns that reduced outdoor activities and increased digital screen time might worsen the global burden of myopia.2,3,4
Based on a cross-sectional design and refraction without cycloplegia, Wang et al5 recently provided evidence on changes in distribution of refraction after the outbreak of COVID-19 in schoolchildren in China. Compared with previous years, the spherical equivalent refraction (SER) among Chinese children aged 6 to 8 years was approximately 0.3 D more myopic and the prevalence of myopia increased by around 10% to 16% in 2020. In children 9 years and older, the differences appeared to be negligible. The study results indicated that it is likely only young schoolchildren, being in the critical period of myopia development, were sensitive to certain environmental changes during this period.
Using longitudinal data on cycloplegic refraction and axial length (AL), the present study investigated changes in the development of myopia in young schoolchildren in China during the COVID-19 outbreak period. Myopia incidence, SER change, and AL elongation from grade 2 to grade 3 were calculated and compared between November and December 2018 to November and December 2019 and November and December 2019 to November and December 2020. Distribution of refractive errors in grade 3 students in November and December 2020 was determined and compared with that in November and December 2019.
Methods
Study Population
An ongoing prospective study was launched in November 2018, aimed at determining the distributions and annual changes in refraction and AL in Chinese schoolchildren. The study was approved by the Sun Yat-Sen University School of Public Health institutional review board and conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from parents or guardians after the study purposes and contents were explained in school seminars. No compensation or incentives were offered for participation.
The present study analyzed a subset of these data, aiming to evaluate the association between environmental changes during the COVID-19 outbreak period and development of myopia in young schoolchildren. The same approval and consent apply to the present study.
In November and December 2018, the study invited all grade 1 and grade 2 students from 12 primary schools in Guangzhou to participate. The schools were randomly selected from the primary schools in the Panyu and Huadu districts, which are socioeconomically ranked fourth and eighth, respectively, among the 11 districts of the city according to 2018 census data. The response rate was 75.8% (3365 of 4437), and 3176 students were successfully assessed for eligibility. A total of 132 students were excluded because of history of ocular surgery or having ocular disorders such as tropia and amblyopia (Figure 1). Follow-up examinations were performed annually in November and December. As of December 2020, 3 visits had been completed.
Figure 1. Flowchart of Students Included in Analysis.
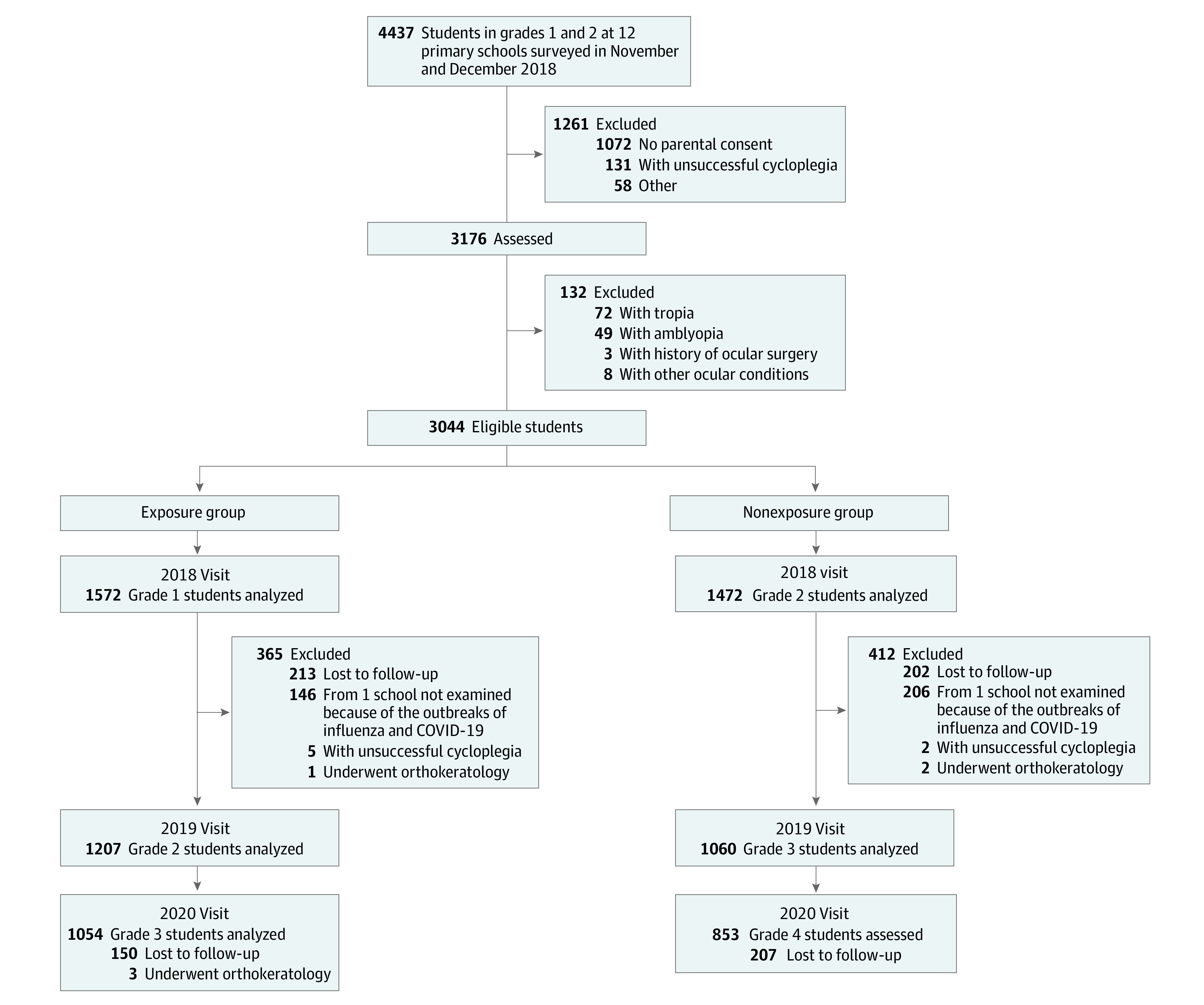
Participants were classified into 2 groups: the exposure group included 1572 students in grade 1 in November and December 2018 who were assessed from grade 2 (November and December 2019) to grade 3 (November and December 2020) during the COVID-19 pandemic, and the nonexposure group included 1472 students in grade 2 in November and December 2018 who were assessed from grade 2 (November and December 2018) to grade 3 (November and December 2019) prior to the pandemic period (Figure 1). Data for the exposure group, who experienced the COVID-19 pandemic during the period from grade 2 to grade 3, were analyzed and compared with the data for the nonexposure group who were in grade 2 to grade 3 prior to the pandemic. Students with unsuccessful cycloplegic refraction or who reported receiving orthokeratology treatment at the follow-up visits were removed from analysis.
Measurements
Field examinations were performed in each school on weekdays during the school day. All ocular examinations were conducted using standardized protocols by a group of trained ophthalmologists and optometrists (Y.H., F.Z., Z.L., Z.F., X.T.). Equipment was calibrated at the beginning of each examination session.
At each visit, uncorrected visual acuity was evaluated using the Early Treatment Diabetic Retinopathy Study chart with tumbling E optotypes (Precision Vision). The cover-uncover test was performed at both near and distance to identify tropia. Slitlamp and direct ophthalmoscopy were used to detect abnormalities in the anterior and posterior segments. AL was measured by noncontact partial-coherence laser interferometry (IOLMaster 500; Zeiss).
Cycloplegic autorefraction was performed using a desktop autorefractor (KR8800; Topcon Corp). Cycloplegia was induced by using 3 drops of 1% cyclopentolate, instilled 5 minutes apart. Refractive measurement was taken after complete cycloplegia (absence of light reflex and a dilated pupil at least 6 mm in diameter). For children with uncorrected visual acuity worse than 20/20 in either eye, cycloplegic subjective refraction was also performed and best-corrected visual acuity was determined.
Definitions
SER was calculated as spherical power +1/2 cylindrical power using data obtained from the cycloplegic autorefraction. Myopia was defined as SER of −0.50 D or less, emmetropia was defined as SER greater than −0.50 D and less than +2.00 D, and hyperopia was defined as SER of +2.00 D or greater. Specifically, children with emmetropia and SER greater than −0.50 D and less than or equal to +0.50 D (lower than the age-normal) were identified to estimate the future development of myopia,6 and children with myopia and with SER less than −1.80 D (lower than the age-specific fifth population centile) were identified to estimate the future development of high myopia.7,8
Data collected at 2 consecutive visits in grade 2 and grade 3 (November and December 2019 and November and December 2020 visits for the exposure group and November and December 2018 and November and December 2019 visits for the nonexposure group) were used for the longitudinal analysis. The incidence of myopia was calculated as the proportion of students with myopia who did not have myopia at the previous visit. Five refractive categories were defined as follows:
Students with hyperopia at both visits.
Students who developed hyperopia and demonstrated emmetropia at the second visit.
Students with emmetropia at both visits.
Students without myopia at the first visit (SER greater than −0.50 D) and with myopia at the second visit.
Students with myopia at both visits.
Statistical Analysis
Statistical analysis was performed using Stata version 15.0 (StataCorp). For all analyses, data from the right eyes were used because of high correlation between the right and left eyes using pairwise Pearson correlation (r, 0.93 for SER and 0.97 for AL in the grade 2 measurement; P < .001). Descriptive statistics were performed. Means with SDs and numbers with percentages were reported. For comparisons, t test or χ2 test was applied as appropriate to examine differences between the nonexposure and exposure groups, and paired t test was used to evaluate annual changes within the nonexposure group or within the exposure group. Two-tailed P values were used and there was no adjustment to P values for multiple analyses. A P value <.01 was considered statistically significant.
Results
A flowchart of the students included in the analysis is shown in Figure 1. A total of 2679 students (mean [SD] age, 7.76 [0.32] years; 1422 [53.1%] male) were available for analysis. Among them, 1207 were in the exposure group examined in November and December 2019 and 1472 were in the nonexposure group examined in November and December 2018. After 1 year, 2121 of the 2679 grade 2 students (79.2%) were reexamined. Among them, 5 reported receiving orthokeratology treatment and 2 reported unsuccessful cycloplegic refraction, leaving 2114 grade 3 students (1054 from the exposure group examined in November and December 2020 and 1060 from the nonexposure group examined in November and December 2019) eligible for analysis. Demographic characteristics of the included students are in the eTable in the Supplement. There was no sex difference between the exposure group and nonexposure group, and the mean (SD) age of the nonexposure group was 0.05 (95% CI, 0.03-0.08) to 0.08 (95% CI, 0.06-0.11) years greater than that of the exposure group.
Table 1 demonstrates the mean SER, AL, and prevalence of refractive errors in grade 2 students in November and December 2018 (nonexposure group) and November and December 2019 (exposure group). SER and prevalence of myopia were not different between the 2 groups. The mean AL was 0.11 mm (95% CI, 0.05-0.16) shorter in the exposure group.
Table 1. Spherical Equivalent Refraction, Axial Length, and Prevalence of Refractive Errors in Grade 2 Students in November and December 2018 (Nonexposure Group) and November and December 2019 (Exposure Group).
| Refraction-related parameter | Mean (SD) | Difference (95% CI) | P value | |
|---|---|---|---|---|
| Nonexposure group (n = 1472) | Exposure group (n = 1207) | |||
| SER, D | 0.82 (1.06) | 0.86 (0.94) | 0.03 (−0.04 to 0.11) | .41 |
| AL, mm | 23.03 (0.75) | 22.92 (0.74) | −0.11 (−0.16 to −0.05) | <.001 |
| Prevalence, No. (%) | .74 | |||
| Myopia | 115 (7.8) | 85 (7.0) | −0.8 (−2.8 to 1.2) | |
| Emmetropia | 1262 (85.7) | 1041 (86.3) | 0.5 (−2.1 to 3.2) | |
| Hyperopia | 95 (6.5) | 81 (6.7) | 0.3 (−1.6 to 2.1) | |
Abbreviations: AL, axial length; SER, spherical equivalent refraction.
From grade 2 to grade 3, students in the exposure group experienced 0.36 D (95% CI, 0.32-0.41; P < .001) more myopic shift of SER and 0.08 mm (95% CI, 0.06-0.10; P < .001) greater AL elongation than those in the nonexposure group. Incidence of myopia was 7.9% (95% CI, 5.1-10.6; P < .001) higher in the exposure group than in the nonexposure group (Table 2). Consequently, the mean SER in grade 3 students in the exposure group was 0.35 D (95% CI, 0.25-0.45) more myopic than in the nonexposure group. The AL was not different between the exposure and nonexposure groups (Table 3), as opposed to longer AL in the nonexposure group in grade 2 students (Table 1). Prevalence of myopia in grade 3 in the exposure group (219 of 1054 students [20.8%]) was 7.5% (95% CI, 4.3-10.7) higher than in the nonexposure group (141 of 1060 students [13.3%]) (Table 3).
Table 2. Change in Spherical Equivalent Refraction, Axial Length Elongation, and Myopia Incidence From Grade 2 to Grade 3 During the Periods From November and December 2018 to November and December 2019 (Nonexposure Group) and November and December 2019 to November and December 2020 (Exposure Group) .
| Parameter associated with myopia development | Mean (SD) | Difference (95% CI) | P value | |
|---|---|---|---|---|
| Nonexposure group (n = 1060) | Exposure group (n = 1054) | |||
| Change in SER, D | –0.31 (0.46)a | –0.67 (0.56)a | –0.36 (–0.41 to –0.32) | <.001 |
| Change in AL, mm | 0.22 (0.21)a | 0.31 (0.24)a | 0.08 (0.06 to 0.10) | <.001 |
| Myopia incidence, No./total No. (%) | 74/992 (7.5) | 151/986 (15.3) | 7.9 (5.1 to 10.6) | <.001 |
Abbreviations: AL, axial length; SER, spherical equivalent refraction.
P < .001 using paired t test.
Table 3. Spherical Equivalent Refraction, Axial Length, and Distribution of Refractive Errors in Grade 3 Students in November and December 2019 (Nonexposure Group) and November and December 2020 (Exposure Group) .
| Refraction-related parameter | No. (%) | Difference (95% CI) | P value | |
|---|---|---|---|---|
| Nonexposure group (n = 1060) | Exposure group (n = 1054) | |||
| SER, D, mean (SD) | 0.55 (1.16) | 0.20 (1.15) | −0.35 (−0.45 to −0.25) | <.001 |
| AL, mm, mean (SD) | 23.25 (0.78) | 23.23 (0.79) | −0.02 (−0.08 to 0.05) | .64 |
| Prevalence | <.001 | |||
| Myopia | 141 (13.3) | 219 (20.8) | 7.5 (4.3 to 10.7) | |
| Emmetropia | 880 (83.0) | 809 (76.7) | −6.3 (−9.7 to −2.9) | |
| Hyperopia | 39 (3.7) | 26 (2.5) | −1.2 (−2.7 to 0.3) | |
| Proportion | ||||
| Individuals without myopia, SE >−0.50 and ≤+0.50 D, No./total No. (%) | 286/919 (31.1) | 409/835 (49.0) | 17.9 (13.3 to 22.4) | <.001 |
| Total population, SE <−1.80 D | 38 (3.58) | 57 (5.41) | 1.8 (0.1 to 3.6) | .04 |
Abbreviations: AL, axial length; SER, spherical equivalent refraction.
In November and December 2020, 409 of 835 students without myopia in grade 3 (49.0%) had SER greater than −0.50 D and less than or equal to +0.50 D. The percentage of students with SER greater than −0.50 D and less than or equal to +0.50 D in November and December 2020 was 17.9% (95% CI, 13.3-22.4) higher than in November and December 2019 (Table 3). The proportion of grade 3 students with myopia more severe than −1.80 D was 5.4% (57 of 1054) in November and December 2020, while that in November and December 2019 was 3.6% (38 of 1060) (Table 3).
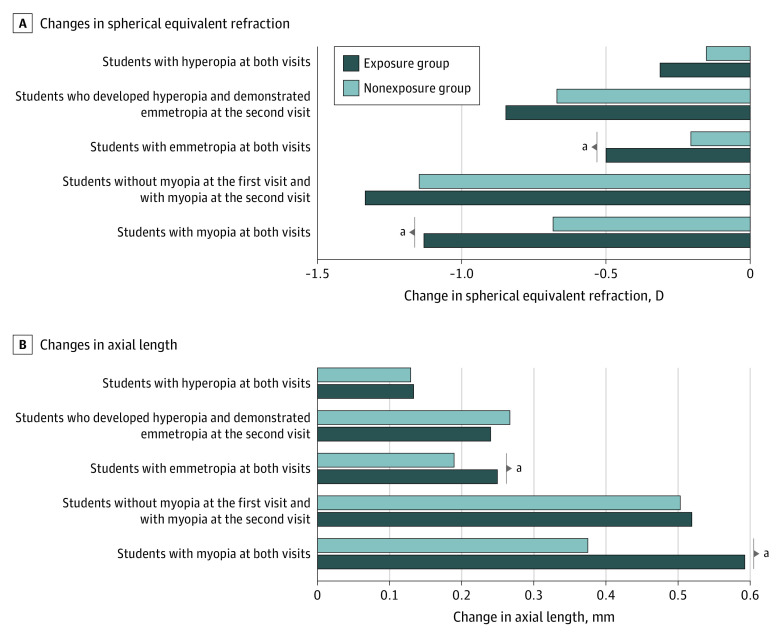
Figure 2 displays the changes in SER and AL from grade 2 to grade 3 in children in different refractive categories. Increased myopic shift of SER and AL elongation during the period from November and December 2019 to November and December 2020 were observed in students with emmetropia at both visits and those with myopia at both visits. While in students with hyperopia at both visits, students who developed hyperopia and demonstrated emmetropia at the second visit, and students without myopia at the first visit and with myopia at the second visit, changes in SER and AL were not different between the periods from November and December 2018 to November and December 2019 and November and December 2019 to November and December 2020.
Figure 2. Changes in Spherical Equivalent Refraction and Axial Length From Grade 2 to Grade 3 in Different Refractive Categories in Students in the Nonexposure Group (November and December 2018 to 2019) and Exposure Group (November and December 2019 to 2020).
aP < .001.
Discussion
In this study, we reported changes in the development of myopia from grade 2 to grade 3 during the COVID-19 outbreak period in China. Compared with the period from November and December 2018 to November and December 2019, SER increased 2-fold toward myopia during the period from November and December 2019 to November and December 2020. AL elongation sped up about 1.4-fold, and the incidence of myopia doubled. Corresponding to the accelerated progression, cross-sectionally, we found a 0.35-D myopic shift in SER in grade 3 students from November and December 2019 to November and December 2020. The shift was comparable with the noncycloplegic data reported in Wang et al.5 The prevalence of myopia in grade 3 in November and December 2020 increased by 7.5%, matching findings from a study in Taiwan9 that showed changes in the prevalence of myopia (defined as SER of −0.25 D or less) in grade 3 during a 6-year period (from 42.7% in 2010 to 50.0% in 2016).
While it is evident that the development of myopia accelerated in young Chinese schoolchildren during the COVID-19 outbreak, some may argue that the acceleration would fade after the spread of the pandemic was under control. In our study sample, nearly half of the children without myopia in grade 3 in November and December 2020 demonstrated SER greater than −0.50 D and less than or equal to +0.50 D, compared with the proportion of approximately 30% in November and December 2019. Because these children are deemed to be at risk of developing myopia,6 we are concerned that the incidence of myopia may remain high over the next few years. Moreover, behavior changes, including reduced time outdoors and increased digital learning, may persist beyond the period of the pandemic,2 heightening the risk of a prolonged acceleration in the progression of myopia.
Given the strong association between early-onset myopia and development of high myopia,10,11 the doubled myopia incidence found in the children in this study might arouse concern regarding future increases in incident high myopia. In our preliminary analysis of the proportion of at-risk children in grade 3, a relative increase of around 50% was found in November and December 2020 compared with November and December 2019 (5.4% vs 3.6%). This indicates that environmental changes during the COVID-19 outbreak, which had an impact on the development of myopia in young schoolchildren in this study, might also worsen the burdens on the health care system for myopia control and on future high myopia.
We observed that a myopic shift (eg, more negative SER) in refractive parameters during the COVID-19 pandemic was only observed in students in the exposure group who had emmetropia at both examinations or who had myopia at their first examination, while in students who initially had hyperopia, differences in development of refractive parameters between the exposure and nonexposure groups were not observed. Previous epidemiological studies have demonstrated an association between gene-environment interaction and myopia.12,13,14 Factoring in similar environmental risk factors for all children during the pandemic outbreak period, we speculate that the differential effect of the environmental change is conditional on individual genetic predisposition.
This study found that, although environmental changes during the COVID-19 outbreak period substantially increased incident myopia in the study population, the amount of SER and AL change among children with incident myopia (ie, students without myopia at the first visit and with myopia at the second visit) were not affected. Previous studies reported that the maximum changes in refraction and AL were demonstrated just 1 year before the onset of myopia.15,16 Combining this evidence, we speculate that during this phase of disease development, changes in SER and AL might have achieved their maximum values and adding on environmental risks would not promote further change.
Limitations
This study had limitations. The study only examined changes in children from grade 2 to grade 3. Because most instances of myopia develop after children enter primary school,17 it would be more informative if data on children of other grades were evaluated. However, results from Wang et al5 indicate that age-specific refractive changes in response to environmental changes during the COVID-19 pandemic were similar among young schoolchildren, and older children appeared to be insensitive to the alteration. Therefore the current study provided longitudinal data on cycloplegic refraction and axial elongation for younger schoolchildren.
This study did not collect data on ocular biometric parameters, including corneal curvature, anterior chamber depth, and lens thickness. Thus, changes in the development of these ocular components could not be investigated. Because the development of myopia in schoolchildren is mostly owing to excessive axial elongation,15,18 we inferred with caution that the environmental changes during the pandemic outbreak period would barely alter the development of ocular components except for axial elongation. Moreover, we were unable to evaluate detailed environmental changes during the pandemic outbreak period, limiting the interpretation of the results of the study.
Conclusions
In this study, the development of myopia accelerated in young Chinese schoolchildren during the outbreak of COVID-19. This acceleration resulted in a doubled myopic shift of SER from grade 2 to grade 3 as well as a doubled incidence of myopia. The proportion of children without myopia at risk of developing myopia increased significantly in grade 3 in November and December 2020. The findings reported in this study need to be validated and generalized. The long-term impact of environmental changes during the COVID-19 outbreak period warrants further investigations with longer observation.
eTable. Characteristics of the study groups in grade 2 and grade 3
References
- 1.Wang G, Zhang Y, Zhao J, Zhang J, Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020;395(10228):945-947. doi: 10.1016/S0140-6736(20)30547-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wong CW, Tsai A, Jonas JB, et al. Digital screen time during the COVID-19 pandemic: risk for a further myopia boom? Am J Ophthalmol. 2021;223:333-337. doi: 10.1016/j.ajo.2020.07.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Navel V, Beze S, Dutheil F. COVID-19, sweat, tears… and myopia? Clin Exp Optom. 2020;103(4):555. doi: 10.1111/cxo.13086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pellegrini M, Bernabei F, Scorcia V, Giannaccare G. May home confinement during the COVID-19 outbreak worsen the global burden of myopia? Graefes Arch Clin Exp Ophthalmol. 2020;258(9):2069-2070. doi: 10.1007/s00417-020-04728-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang J, Li Y, Musch DC, et al. Progression of myopia in school-aged children after COVID-19 home confinement. JAMA Ophthalmol. 2021;139(3):293-300. doi: 10.1001/jamaophthalmol.2020.6239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gifford KL, Richdale K, Kang P, et al. IMI—clinical management guidelines report. Invest Ophthalmol Vis Sci. 2019;60(3):M184-M203. doi: 10.1167/iovs.18-25977 [DOI] [PubMed] [Google Scholar]
- 7.Chen Y, Zhang J, Morgan IG, He M. Identifying children at risk of high myopia using population centile curves of refraction. PLoS One. 2016;11(12):e0167642. doi: 10.1371/journal.pone.0167642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang X, Chen YX, Zeng JW, He MG. From evidence to clinical practice: myopia control among children in refraction clinics. Article in Chinese. Zhonghua Yan Ke Za Zhi. 2019;55(2):89-92. doi: 10.3760/cma.j.issn.0412-4081.2019.02.003 [DOI] [PubMed] [Google Scholar]
- 9.Tsai TH, Liu YL, Ma IH, et al. Evolution of the prevalence of myopia among Taiwanese schoolchildren: a review of survey data from 1983 through 2017. Ophthalmology. 2021;128(2):290-301. doi: 10.1016/j.ophtha.2020.07.017 [DOI] [PubMed] [Google Scholar]
- 10.Hu Y, Ding X, Guo X, Chen Y, Zhang J, He M. Association of age at myopia onset with risk of high myopia in adulthood in a 12-year follow-up of a Chinese cohort. JAMA Ophthalmol. 2020;138(11):1129-1134. doi: 10.1001/jamaophthalmol.2020.3451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chua SY, Sabanayagam C, Cheung YB, et al. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children. Ophthalmic Physiol Opt. 2016;36(4):388-394. doi: 10.1111/opo.12305 [DOI] [PubMed] [Google Scholar]
- 12.Enthoven CA, Tideman JWL, Polling JR, et al. Interaction between lifestyle and genetic susceptibility in myopia: the Generation R study. Eur J Epidemiol. 2019;34(8):777-784. doi: 10.1007/s10654-019-00512-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Verhoeven VJ, Buitendijk GH, Rivadeneira F, et al. ; Consortium for Refractive Error and Myopia (CREAM) . Education influences the role of genetics in myopia. Eur J Epidemiol. 2013;28(12):973-980. doi: 10.1007/s10654-013-9856-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fan Q, Verhoeven VJ, Wojciechowski R, et al. ; Consortium for Refractive Error and Myopia . Meta-analysis of gene-environment-wide association scans accounting for education level identifies additional loci for refractive error. Nat Commun. 2016;7:11008. doi: 10.1038/ncomms11008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xiang F, He M, Morgan IG. Annual changes in refractive errors and ocular components before and after the onset of myopia in Chinese children. Ophthalmology. 2012;119(7):1478-1484. doi: 10.1016/j.ophtha.2012.01.017 [DOI] [PubMed] [Google Scholar]
- 16.Mutti DO, Hayes JR, Mitchell GL, et al. ; CLEERE Study Group . Refractive error, axial length, and relative peripheral refractive error before and after the onset of myopia. Invest Ophthalmol Vis Sci. 2007;48(6):2510-2519. doi: 10.1167/iovs.06-0562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Matsumura H, Hirai H. Prevalence of myopia and refractive changes in students from 3 to 17 years of age. Surv Ophthalmol. 1999;44(suppl 1):S109-S115. doi: 10.1016/S0039-6257(99)00094-6 [DOI] [PubMed] [Google Scholar]
- 18.Zadnik K, Manny RE, Yu JA, et al. ; Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) Study Group . Ocular component data in schoolchildren as a function of age and gender. Optom Vis Sci. 2003;80(3):226-236. doi: 10.1097/00006324-200303000-00012 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Characteristics of the study groups in grade 2 and grade 3